Review Article - Pharmaceutical Bioprocessing (2017) Volume 5, Issue 4
Diabetes: pharmacological history and future management strategies
- *Corresponding Author:
- Jahangir MA
Department of Pharmaceutics
School of Pharmacy, Glocal University
Saharanpur, Uttar Pradesh, India
E-mail: asadullahpharma@gmail.com
Abstract
Diabetes a serious chronic disorder is one of the oldest diseases known to mankind. In spite of being known from a long time, the etiology of the disease is not clearly understood till date. With the growing cases of diabetes all around the world, new advancements are being made for the better understanding and management of the disease. The current review explores in terms of its historical perspective, the discovery of Insulin, Impairment of glucose level, its early treatments, present status of diabetes, the experiments in relation to diabetes, risk of hypoglycaemia, risk of mortality from diabetes including the neonate, adults and geriatrics and management of diabetes through rising technologies, pancreas transplantation, advanced diabetic treatments with self-care along with future perspective.
Introduction
Diabetes is a serious, chronic metabolic disorder which is primarily caused due to insufficient insulin production. However, insufficient use of insulin produced by the body is another major cause of the disease. Diabetes, being one of the important health problems is among one of the four priority non-communicable diseases targeted for action and a serious threat to population health. The prevalence of diabetes is steadily increasing everywhere, mostly in the middle-income countries of the world [1].
According to the International Diabetes Federation (IDF), an estimated 415 million people globally suffered from this condition in 2015. This number is expected to increase to 522 million by 2030 [2]. Diabetes Mellitus (DM) has serious complications which accounts for increased morbidity, disability, and mortality. DM stands among the oldest disease known to mankind. However, proper understanding of it pathogenesis has been known since ancient times, its treatments came to be known since the Middle Ages, and the elucidation of its pathogenesis occurred mainly in the 20th century [3]. DM is classified based on its etiology and clinical presentations. As such, there are two common types of DM viz; type 1 diabetes (T1D), and type 2 diabetes (T2D) [3].
T1D which is also known as insulin-dependent [4], juvenile or childhood-onset diabetes is characterized by insufficient insulin production in the body. Patients with T1D require regular administration of insulin to regulate the amount of glucose in their blood. The cause of T1D is still not well understood and it is currently an untreatable disease [5]. Its symptoms include excessive or frequent urination and thirst, constant hunger, vision changes, weight loss and fatigue. T1D results from complex interaction between genes and environmental factors; though no specific environmental risk factors have been shown to cause a significant number of cases. T1D occurs majorly in children and adolescents [1].
T2D which was formerly and very commonly known as non-insulin-dependent [6] or adult-onset diabetes results from the body’s ineffectiveness to use insulin. T2D diabetes accounts for the vast majority of people with diabetes around the world. Symptoms may be similar to those of T1D, but are often less marked or absent [7]. T2D may go undiagnosed for several years, until complications are prominent. For many years, type 2 diabetes was seen only in adults but now it has begun to develop in children. The risk of T2D is determined by interplay of genetic and metabolic factors. Family history of diabetes and previous gestational diabetes combine with older age, overweight and obesity, unhealthy diet, physical inactivity and smoking may increase its risk [1]. The diagnostic criteria for determining diabetes have evolved over the years. Currently, diabetes is diagnosed by a fasting glucose of 126 mg/dl or a random glucose of 200 mg/ dl. Biomarkers are biological molecules which can be exploited to diagnose subclinical disease before the development of clinical disease [8]. Various biomarkers are being studied for the early and better diagnosis of diabetes. Different diabetic biomarkers and the analytical methods which are used to diagnose diabetes are enlisted in the Table 1.
| Biomarker | Analytical Approach |
|---|---|
| C-Peptide | ELISA/RIA |
| Cholesteryl Ester Transfer Protein (CETP) | ELISA |
| Free Fatty Acids (FFA) | Immunoturbidimetric |
| Fructosamine | Immunoturbidimetric |
| Glucagon | RIA |
| Glutamate Decarboxylase-65 (GAD-65 ) Antibody | ELISA |
| HbA1c | Immunoturbidimetric/ HPLC |
| IA-2 Antibody | ELISA |
| Insulin Growth Factor (IGF-1) | ELISA |
| Microalbumin | Immunoturbidimetric |
| Proinsulin | ELISA |
Table 1. Biomarkers and analytical approaches for the early diagnosis of diabetes
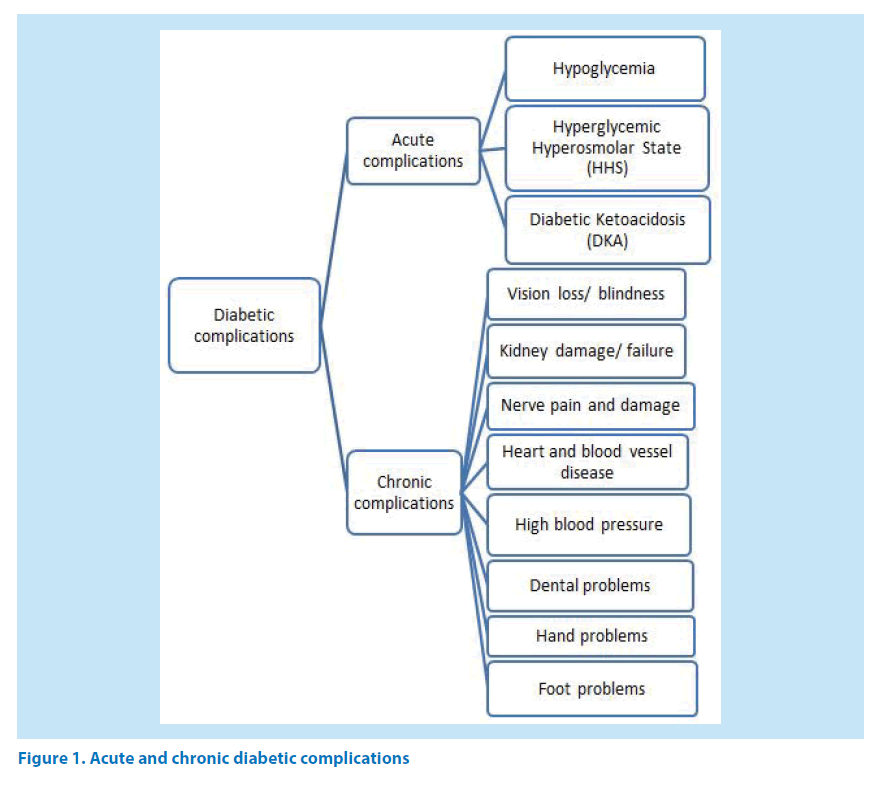
Being a metabolic disorder, diabetes directly or indirectly affects many organs and thus further complicates the situation. Diabetes mainly affects organs like kidney, heart, eyes, foot hand, teeth’s and nerves. Diabetic complications may be broadly classified into acute and chronic complications. Diabetic complications include retinopathy, nephropathy, neuropathy, cardiovascular, cerebrovascular diseases [3,8]. People with diabetes are at high risk for neovascular glaucoma [9]. Figure 1 enlists the complications that may arise due to diabetes.
Role of the pancreas
Role of the pancreas on the onset of diabetes was first described by Oskar Minkowski and Joseph Von Mering in the year 1889 [10]. They found that upon complete removal of the pancreas from dogs, the dogs exhibited all the signs and symptoms of diabetes and died shortly afterwards. Sir Edward Albert Sharpey-Schafer in the year 1910 suggested that in diabetes a single, specific chemical was missing which was normally produced by the pancreas. Later the name of this chemical was proposed to be insulin [1].
Insulin - the miraculous discovery
Many researchers were working to extract insulin in the early 19th century but the name of Banting and Best comes forward among the successful ones. Frederick Grant Banting and Charles Herbert Best in the year 1921 repeated the work of Von Mering and Minkowski but went a step further and showed that they could reverse the induced diabetes in dogs by giving them an extract from the pancreatic islets of Langerhans of healthy dogs. This was an important step in the elucidation of the endocrine role of pancreas in metabolism and existence of insulin. These scientists isolated insulin from bovine pancreases at the University of Toronto in Canada, thereby leading to the availability of an effective treatment of DM, with the first clinical patient being treated in 1922 [3].
Insulin is a polypeptide hormone produced in humans and other mammals by the β-cells of the islets of Langerhans within the pancreas. The islet cells form the endocrine part of pancreas, accounting for 2% of the total mass of the pancreas with beta cells constituting 60-80% of all the cells of islets of Langerhans [3].
The basic function of insulin [11] is to promote the synthesis of carbohydrates, proteins, lipids, and nucleic acids. The effects of insulin on carbohydrate metabolism is to stimulate the glucose transport across muscle and adipocyte cell membranes, inhibition of glycogenolysis [12], regulation of hepatic glycogen synthesis and gluconeogenesis.
The end result of these actions is a reduction in blood glucose concentration [13].
The production of insulin is directly proportional to the amount of carbohydrate consumed. The more sugar one consumes, the more insulin the body will have to produce, but, the tiny pancreatic beta cells were never designed to produce this level of insulin [14]. With a limited capacity to produce insulin, a capacity that is more than sufficient to last a lifetime under normal dietary conditions, the forced over-production of insulin will eventually exhaust that capacity and the cells will cease to operate [14].
However, the production of insulin does not always depend on blood glucose levels as insulin is stored in cells before its release. Insulin is also the major regulatory signal for glycogenesis in the hepatocytes and myocytes and its deficiency of Insulin has a vital role in all forms of diabetes [15]. It is the major hormone that helps muscle and fat cells to uptake glucose from the blood. Furthermore, Insulin also helps other body tissues to remove glucose from the blood for use as fuel, for conversion process into other needed molecules, or for storage [3].
Impairment of glucose level
Impaired glucose tolerance (IGT) and impaired fasting glycaemia (IFG) are intermediate conditions in the transition between normal blood glucose levels and diabetes (especially type 2), though the transition is not inevitable. People with IGT or IFG are at increased risk of heart attacks and strokes [16].
As per the National Cholesterol Education Plan (NCEP)-Adult Treatment Panel (ATP) III guidelines and American Diabetes Association (ADA), a study was conducted in Pondicherry, India to observe patterns and pre valences of dyslipidaemia and impaired glucose tolerance. In this study 1621 people were included and were divided into 5 groups based on their age. The lipid profile and blood glucose was estimated amongst this group of people. The result showed that 21.4% of the population had DM, 36.72% had high triglycerides, 39.72% had high cholesterol, 71.68% had high LDL-c and 78.65% had low HDL-C. These are some known risk factors for cardiovascular diseases and metabolic syndromes. Similar results have been noticed in studies conducted in many other countries [17].
Hypoglycaemia: insulin’s over effect
Hypoglycaemia is a clinical, physiologic condition that contributes to increased morbidity and mortality [18] in individuals with T1D and T2D. Hypoglycaemia results from the inability to raise the blood glucose (BG) level through endogenous or exogenous methods. The patients engaged in lifestyle modifications, like increased physical activity and dietary changes was observed with a reduced insulin dose by 10-20% [19]. Hypoglycemia has been found very common in clinical practices which occur during the treatment of DM [20].
The glycaemic control can be also improved by the psychological interventions which reduce diabetes distress and are proved to be more efficacious if they address an individual’s perception of personal control [21]. Also the emotional distress linked with adjusting to and living with diabetes is termed as diabetes distress. Higher levels of personal control are hypothesised for the better glycaemic control [22].
Neonatal hypoglycaemia
Neonatal hypoglycaemia is associated with maternal diabetes and preterm birth [23]. In an interesting study, racial differences were seen in neonatal hypoglycaemia. Out of the 66% spontaneous preterm births, 63% of the black neonates had experienced hypoglycaemia (blood glucose level < 40 mg/ dL), while only 22–30% of the other racial/ ethnic neonates did so [24]. Neonatal Hypoglycaemia is a significant factor in the overall neonatal mortality. Severe Neonatal Hypoglycaemia also leads to neurological damage, impaired cardiac performance, and incidence of seizers, mental retardation, personality disorders and muscle weakness [25]. Neonatal Hypoglycaemia is one of the leading causes of admission of neonates to the hospitals [26].
Hypoglycemia in women
Pregnancy in women with diabetes is mainly associated with an increased risk of perinatal mortality and obstetric complications. Rates of maternal morbidity and mortality are higher among women with diabetes. The death rate of pregnant women with T1D [27] is comparatively 109-times greater than women in the general population and 3.4 times higher than non-pregnant Type 1 diabetic women. Hypoglycaemic coma, traffic accidents and death due to severe hypoglycaemia in pregnancy may constitute problems. This can be treated in women with multiple insulin injections with fast-acting insulin at mealtimes and long-acting insulin 1-3 times daily [28].
Conventional therapeutic methods for the management of diabetes
Till date no cure has been found for diabetes; however, treatment modalities include change in lifestyle, treatment of obesity, oral anti-diabetic agents, and insulin sensitizers like metformin that reduces insulin resistance, is still considered as the first line medication especially for obese patients [29]. Glimepiride (GMD) can effectively control T2D by reducing the fasting and postprandial glucose levels, as well as glycosylated hemoglobin concentrations [30]. Other effective medications for the management of diabetes include non-sulfonylurea (Metformin), thiazolidinediones (Rosiglitazone, Pioglitazone), alpha glucosidase inhibitor (Acarbose, Miglitol), Meglitinides (Repaglinide, Nateglinide), Sodium-Glucose transporter-2 (SGLT- 2) (Canagliflozin, Empagliflozin, etc.), Sulfonylureas (Chlorpropamide, glimepiride, etc) and insulin (Insulin aspart, Insulin lispro, etc.) [2]. Conventional anti-diabetic medicines and their mechanism of actions are listed in Table 2. Apart from the conventional allopathic medicines, a number of herbal products have shown promising results for the management of diabetes.
| Class of hypoglycemic agent | Mechanism of Action | Drugs |
|---|---|---|
| Alpha-glucosidase inhibitors | Competitively and reversibly inhibits Alpha-glucosidase enzyme | Acarbose, Miglitol |
| Meglitinides | Stimulates the pancreas to release insulin in response to diet/meal | Repaglinide, Nateglinide |
| Non-sulfonylureas (biguanides) | Inhibits the amount of glucose produced by liver, increases insulin receptor binding, stimulates tissue uptake of glucose | Metformin |
| Sodium-Glucose transporter-2 (SGLT-2) | Lowers renal glucose threshold level, results in increased glucose excretion from urine | Canagliflozin, Empagliflozin, Dapagliflozin |
| Sulfonylureas | Stimulates the pancreas to release more insulin | Chlorpropamide, glimepiride, Glyburide, Glipizide, Tolazamide, Tolbutamide |
| Thiazolidinediones (glitazones) | Acts as agonists for peroxisome proliferator-activated receptors gamma (PPARgamma), acting as insulin sensitizer | Rosiglitazone, Pioglitazone |
| Insulin | Polypeptide hormone, regulates the amount of glucose in the blood | Insulin regular, Insulin aspart, Insulin lispro, Insulin isophane, Insulin regular, insulin glargine, Insulin detemir, Insulin zinc extended, insulin degludec |
Table 2. Conventional anti-diabetic drugs and their mechanism of action
Role of herbal compounds in controlling diabetes
Several herbal compounds such as Bitter Gourd (Momordica charantia), Bael (Aegle marmelos), Gurmar Leaves (Gymnema sylvestrae), Fenugreek (Trigonella foenum graecum), Turmeric (Curcuma longa), Onion (Allium cepa), Nayantatra (Vinca rosa), Neem (Azadirachtha indica), Garlic (Allium sativum), and Sagar gota (Ceasalpinia crista) play a key role in controlling diabetes [31]. Abdulazeez explored the benefits of strawberries by evaluating the efficacy of freeze dried strawberry powder (FSP) against the hyperlipidemia in alloxan induced diabetic rats. This study has found that the strawberries (polyphenolic antioxidant contents) not only beneficial for the treatment of cancer, infections, obesity, neurological and cardiovascular diseases but also has an effect on the control of hyperlipidemia during diabetes [32]. Hui et al. in their study extracted total flavonoids from the dried root of Pueraria lobata called Radix Puerariae by the chromatographic techniques and other isolation process. The effects of these isolated flavonoids were examined on blood glucose MDA in the alloxan diabetic mice. The serum glucose level was reduced in animals after the administration of Radix Puerariae flavonoids. These exhibited hypoglycemic effect, and helps in the reduction of lipid peroxidation [33].
Ahmed et al. used the phytochemical compounds of Malaysian propolis (natural product obtained from plant resins,) to determine the hypoglycaemic effect on diabetic rats. These phytochemical compounds were identified by using the gas chromatography-mass spectrometry (GC-MS) analysis [34]. Significant reduction in the fasting blood glucose level was seen in streptozotocin-induced diabetic female rats using these phytochemical compounds. Along with this, total food intake and body weight gain was also increased [35]. Li et al. demonstrated that hypoglycemic and hypolipidemic effects of tatary buckwheat (TBF) in induced type- 2 diabetic rats in combination of high-fat diet and streptozotocin injections. The following parameters were studied after 28 days of treatment; body weight, serum insulin, triglyceride (TG), fasting blood glucose (FBG), high-density lipoprotein-cholesterol (HDL-C), total cholesterol (TC) and low-density lipoprotein-cholesterol (LDL-C) levels. Oral Glucose Tolerance Test (OGTT) was performed. The results showed decreased fasting blood glucose and serum insulin levels with improvement in glucose intolerance. Furthermore, the TBF was found to be potent anti-diabetic agent in humans [36]. In a similar study of anti-diabetic activity of the plant leaves of Verbascum thapsus in alloxan induced diabetic rats, it was concluded that the whole plant extract of Verbascum thapsus (L) is having potent anti-diabetic activity on alloxan-induced diabetic rats and this justifies its use in ethanomedicine and can be exploited in the management of diabetes [37].
Chaudhury et al. in his review of literature compiled the beneficial effects of “Morin”. Morins are readily available from the extracts of natural resources like Almond (Prunus dulcis, syn. Prunus amygdalus), Guava (Psidium guajava L.), Old fustic (Chlorophora tinctoria or Maclura tinctoria), Osage orange (Maclura pomifera), Acridocarpus orientalis, Onion (Allium cepa), Apple (Malus pumila), Tea (Camellia sinensis) etc. Morin has shown strong potential in the treatment and management of Diabetes. It has also shown potential in treating or managing neurordegenrative disorders like Alzheimer and Parkinson’s disease, cardiovascular disorders like ischemia etc. Morin has also shows promising results as anti-bacterial, and anti-gout agents [38].
A study was conducted on pancreas of alloxan monohydrate-induced diabetic rats which were exposed to aqueous extract of ginger. This treatment was effective in decreasing the hyperglycemic and hyperlipidemic level in diabetic rats [39]. de la Fuente et al. in their study supplemented the animal models with zinc supplementation for diabetic injury liver and changes were examined by, histopathological assay [40], biochemical assay of serum, immuno-histochemical assay [41], radioimmunoassay [42] and Western blotting [43]. The diabetic liver injury found to be prevented by the zinc supplements [44]. Ekeanyanwu et al. aimed to measure the Vitamin C, Vitamin E and lipid peroxidation status in hypertensive and diabetic patients. These patients received Vitamin supplements, insulin and lipid lowering drug which has significantly reduced the lipid peroxidation which is commonly seen in diabetic patients [45]. In a recent study, Hou et al. has found that emodin (active ingredient of rhubarb) has anti-diabetic property. Emodin can actively reduce the blood glucose levels in T1D patients [46]. Gomphrena serrata has been found to be effective against diabetes [47]. Mirza et al. used Methanolic extract of Euphorbia neriifolia stem bark (MEEN) to study its effect on the blood glucose level serum and tissue lipids in streptozotocin diabetic rats. It was identified that MEEN has anti-hyperlipidaemic and antidiabetic effect and it significantly reduced the blood glucose level and tissue lipids [48].
Testing of haemoglobin level in diabetic patients
A regression analysis was conducted by Hompesch et al. on 75 diabetic patients. The result of this study showed that the levels of Fasting plasma sugar and glycosylated haemoglobin were not affected by the patient’s gender as these parameters did not show any significant difference between male and female diabetic patient [49].
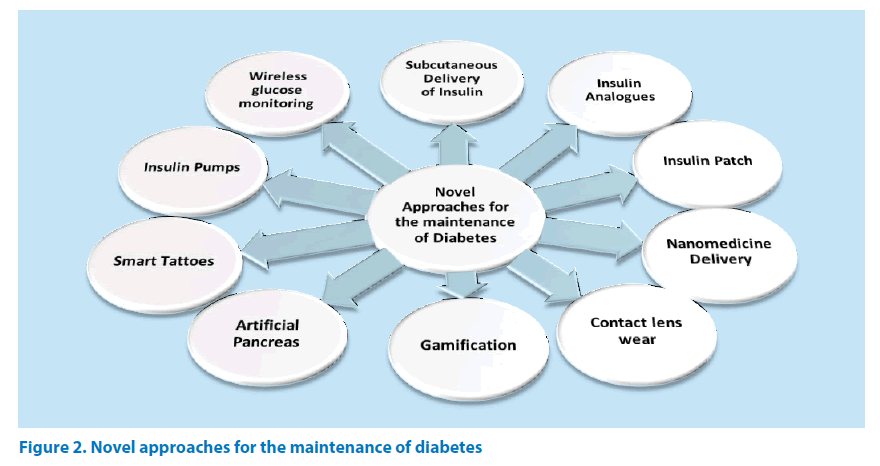
Novel approaches for the maintenance of diabetes
With the development of better scientific approach, researchers around the world are taking strides for better management of diabetes. Some of the recent advancements are briefly discussed in this following section (Figure 2).
Subcutaneous delivery of insulin
The rate of DM is increasing in population, and subcutaneous injection of insulin [50] has been established as an effective therapeutic strategy for reducing the complications associated with the disease. However, the pain after repeated injection is an important drawback. But now, there have been great improvements in injection techniques and devices, including the development of micro-needle and quantitative injection technologies, which can increase the accuracy of injection, decrease leakage of insulin to the skin surface, and can also reduce pain [51].
Insulin analogues
T1D is affecting pregnant women’s very often [52]. The inadequacy of glycemic control can complicate pregnancy and may even result in morbidity and mortality. The common fetal consequences are congenital malformations, recurrent miscarriages, growth anomalies and stillbirth. Maternal consequences are worsening of diabetes vascular complications, pre-eclampsia, eclampsia and increased likelihood of caesarian section. Hence, pregnancy needs to be carefully planned accompanied by experienced diabetologists, diabetes educators, and maternal-fetal medicine specialists. Several Insulin analogues have now been approved for use in pregnancies, facilitating insulin administration. Some patients choose insulin pump therapy. Glucose control is regulated through labor, and insulin requirements are also decreased to pre-pregnancy level after delivery [53].
Insulin Patch
This microneedle-patch device was developed by Yu and colleagues containing nanoparticles. It comprises of insulin; the enzyme glucose oxidase (glucose sensing enzyme) and a hypoxia responsive polymer. The polymer releases insulin without pain. This method is less-painful and more reliable. This technology helps people to deal with the diabetes condition more safely and in an effective way [54].
Nanomedicine delivery
Nanomedicine technology has shown potential in the management of diabetes in the recent time. Nanoparticles are assisting as contrasting agents in imaging which helps in early diagnosis of the disease. Glucose nanosensors are being implanted for more accurate and patient friendly tracking of blood glucose level. Nanotechnology approach is also being exploited for insulin delivery [55]. Apart from that, a number of oral anti-diabetic agents are being developed as nanoparticle system for targeted drug delivery, to decrease the frequency of administration and increase the patient compliance [56].
Contact lens wear
Diabetic patients are more susceptible to corneal erosions and blood vessel leakage, must wear contact lenses (made of hydrogel polymers). The diabetic patients have altered tear secretion and face structural and functional changes to the corneal epithelium, endothelium and nerves. This technology can become a viable mode of refractive correction for diabetic patients [57].
Gamification in self-management of diabetes
The use of videogames in the self-management of diabetes has gained popularity. The gamification and virtual environments has proved to increase the extrinsic motivation and it also provides positive reinforcement [58].
Artificial pancreas
To avoid post-operative complications, blood glucose is strictly controlled during the cardiovascular surgery. Blood glucose is continuously monitored using STG-55® artificial endocrine pancreas (Nikkiso Inc., Tokyo). Blood glucose concentrations do not increase during the cardiopulmonary bypass to lower body ischemia. However, they increase immediately after reperfusion followed by the lower body ischemia [59].
Insulin pumps technology for diabetes
Technology for diabetes management has developed in the recent decades. Such technological advances include- Continuous Subcutaneous Insulin Infusion (CSII), which is also known as Insulin Pumps, and Real-Time Continuous Glucose Monitoring System (RT-CGMS). This integration of CSII and RT-CGMS into a single device has proven to be effective in decreasing the incidences of hypoglycaemia in type 1 diabetic patients. This technology is known as hybrid system. This technology has automatic delivery of basal insulin therapy [60].
Pancreas transplantation
This advanced step in the field of science is associated with excellent glucose control than insulin. Patients with functional PTAs (Pancreas Transplantation) experience improved quality of life when compared to patients with failed grafts. Successful Pancreas Transplantation alone is also linked with the excellent Self-Identified Health Score [61].
Pancreas transplantation is majorly considered a therapeutic option in patients with complicated diabetes condition by the development of immunosuppressant. The survival rate is higher in the pancreatic transplant recipients. By the pancreatic transplantation sufficient beta cells are supplied. Despite the fact that there persist post-transplant complications such as retinopathy and neuropathy, pancreatic transplantation can be used to increase the survival rate [62].
In the patients who received pancreas transplants, the degree of diabetic retinopathy remains stable over time after transplantation. Early worsening of diabetic retinopathy could also occur in patients at risk [63].
Endocrine-metabolic abnormalities also occur after the long term follow up of transplantation of pancreas. For T1D, patients with pancreas transplantation require special care in regards to the metabolic deviations, infectious complications, and chronic rejection. The complex procedure of pancreatic transplantation is well associated with the surgical morbidity [64,65]. This can be negatively influenced by the side effects occurring from immunosuppressive agents, grafts failure and other infections, chronic rejection (50%) and recipient lifestyle after the transplantation [66].
Duodenal drainage via “button technique
Pancreas transplantation can be performed with the use of retroperitoneal placement of the pancreas transplant and duodenal drainage via the “button technique”. This can result in satisfactory function of both transplants (pancreas and kidney) [67].
Wireless blood glucose monitor
Sensor/Telemetry System and Model can be used for long-term monitoring of subcutaneous tissue glucose in people with diabetes. These sensors are generally based on a membrane containing immobilized glucose oxidase, electrodes and a telemetry system. This device is implanted for 180 days. Since, all diabetic therapies are based on glucose control so it requires glucose monitoring. This has facilitated a new era of management of the diabetes disease [68].
The key component of effective self-management of glycemic control is the accurate self-monitoring of blood glucose. For this purpose, wireless blood glucose meters are used extensively. This blood glucose meter comes in colour range indicator with wireless connectivity to mobiles. It works by connecting wirelessly with Diabetes Management Software [69].
Diabetes self-management by social media
A large number of population with diabetes is dealing their problems through the use of mobile phones, internet and social media for sharing their experience and supporting the self-management. It has been leading towards a new paradigm of hyper-connected Diabetes Digital Self-Management. The social media is empowering people with diabetes. This guidance has a stronger impact on patient health improvement and in improving patient’s health outcomes [70].
Smart Tattoos for glucose monitoring
New bio-sensing tattoo ink has been developed by the researchers to check diabetic sugar levels. These incredible colour changing tattoos monitors the blood sugar level of people with diabetes instantly. This glucose sensing ink works by reacting with sugar in the blood and changes its colour from blue to brown in case of high glucose level in the blood. The reverse can be achieved when the ink colour changes from brown to blue in low blood sugar. Unlike the needle pricking, this technique is a way ahead of pain and taking blood samples [71].
This smart tattoo still has few drawbacks such as specificity and sensitivity of the glucose sensor. These two factors must be maintained throughout the lifespan of the glucose sensor which can achieve by using the additive enzyme catalase. This enzyme helps in blocking the hydrogen peroxide from combining with glucose oxidase and allows the glucose sensor to retain its sensitivity and specificity [72].
Conclusion
Diabetes is a complex metabolic disease which mainly occurs due to either insufficient insulin production or insufficient use of insulin produced by the body. Although it is being one of the oldest diseases known to mankind, still it has no permanent cure. A number of researches are being carried out for the better understanding and management of the disease. It is a bit satisfying that mortality rate due to diabetes has significantly lessened over the years. In most of the cases the diagnosis of the disease is very late particularly in patients of younger age. Biomarkers are being investigated for early diagnosis and management of the disease. Currently, a number of conventional medicines are available in the market which are used either alone or in combination. The first line anti-diabetic agents for the management of diabetes include metformin. A part from that, other oral conventional anti-diabetic agents like Acarbose, Miglitol, Repaglinide, Nateglinide, Canagliflozin, Empagliflozin, Dapagliflozin are also used in combination therapy. Herbal medicine also provides promising evidence as potential anti-diabetic agents. Compounds from natural sources like morins, polyphenolic antioxidant contents from strawberry extracts, flavonoids extracted from the dried root of Pueraria lobata, resins from Malaysian propolis, aqueous extract of ginger etc. have shown promising results in managing diabetes in recent studies. However, more detailed data and clinical studies are required to further understand their potential as potent anti-diabetic agents. With the growing population suffering from diabetes all around the world, new medications as well as better techniques to deliver the drug must be developed. Modern technologies have made it possible to develop new approaches for better management of the disease. Novel approaches like subcutaneous delivery of insulin, insulin pumps, smart tattoes, insulin patches, artificial pancreas, nano-tragetted delivery system are being continuously studied for managing diabetes in a way which are more patient compliant. With the advancement of new technologies we expect a better quality of life of diabetic patients in the upcoming years.
References
- Global reports on diabetes- World Health Organization (2016).
- Jahangir MA, Imam SS, Kazmi I. Type 2 diabetes current and future medications: a short review. Int. J. Pharm. Pharmacol. 2017 (1), 101(2017).
- Piero MN, Nzaro GM, Njagi JM (2015) Diabetes mellitus-a devastating metabolic disorder. Asian. J. Biomed. Pharm. Sci. 5(40), 1 (2015).
- Marshall K, Martin H, Siarkowski Amer K. Exploring perceptions about insulin dependent diabetes mellitus in adolescent patients and peers. Comprehensive. Child. Adol. Nurs. 41(1), 25-41 (2017).
- Deshpande AD, Harris-Hayes M, Schootman M. Epidemiology of diabetes and diabetes-related complications. Phys. Ther. 88(11), 1254-1264 (2017).
- Koloverou E, Panagiotakos DB. Macronutrient composition and management of non-insulin-dependent diabetes mellitus (NIDDM): a new paradigm for individualized nutritional therapy in diabetes patients. Rev. Diab. Stud. 13(1), 6 (2016).
- Vera F, Zenuto RR, Antenucci CD. Decreased glucose tolerance but normal blood glucose levels in the field in the caviomorph rodent Ctenomys talarum: the role of stress and physical activity. Com. Biochem. Physiol. Mol. Int. Physiol. 151(2), 232-238 (2008).
- Sai YRKM, Dattatreya A, Anand SY et al. Biomarkers of internal origin and their significance in diabetes and diabetic complications. J. Diab. Metab. R1, 001 (2011).
- Opeyemi OT. Glaucoma: secrets of silent thief of vision - a review. Univ. J. Pharm. Res. 2(3), 26-30 (2017).
- Novak I, Solini A. P2X receptor-ion channels in the inflammatory response in adipose tissue and pancreas-potential triggers in onset of type 2 diabetes?. Curr. Opinion. Immunol. 52, 1-7 (2018).
- Jaganathan R, Ravindran R, Dhanasekaran S. Emerging role of adipocytokines in type 2 diabetes as mediators of insulin resistance and cardiovascular disease. Canadian. J. Diab.
- Morgan HE, Parmeggiani A. Regulation of glycogenolysis in muscle III. Control of muscle glycogen phosphorylase activity. J. Biol. Chem. 239(8), 2440-2445 (1964).
- Fischer MO, Gouëzel C, Fradin S et al. Assessment of changes in blood glucose concentration with intravascular microdialysis. J. Clin. Monitoring. Computing. 5, 1-8 (2018).
- Torii S, Kubota C, Saito N et al. The pseudophosphatase phogrin enables glucose-stimulated insulin signaling in pancreatic β-cells. J. Biol. Chem. jbc-RA 117 (2018).
- Zhao X, Lu Y, Wang F et al. High glucose reduces hepatic glycogenesis by suppression of microRNA‑152. Mol. Med. Rep. 10(4), 2073-2078 (2014).
- Yuan H, Li X, Wan G et al. Type 2 diabetes epidemic in East Asia: a 35-year systematic trend analysis. Oncotarget. 9(6), 6718 (2018).
- Basu S, Rani PU. Dyslipidaemia and impaired glucose levels in apparently healthy semi urban population in Pondicherry. Biomed. Res. 26(3), (2015).
- Kim JN, Runge W, Wells LJ et al. Effects of experimental diabetes on the offspring of the rat: fetal growth, birth weight, gestation period and fetal mortality. Diabetes. 9(5), 396-404 (1960).
- Kreider KE, Pereira K, Padilla BI. Practical approaches to diagnosing, treating and preventing hypoglycemia in diabetes. Diab. Ther. 8(6), 1427-1435 (2017).
- Martens P, Tits J. Approach to the patient with spontaneous hypoglycemia. Eur. J. Int. Med. 25(5), 415-421 (2014).
- Hagger V, Hendrieckx C, Cameron F et al. Diabetes distress is more strongly associated with HbA1c than depressive symptoms in adolescents with type 1 diabetes: Results from Diabetes MILES Youth-Australia. Ped. Diab.
- Martinez K, Lockhart S, Davies M et al. Diabetes distress, illness perceptions and glycaemic control in adults with type 2 diabetes. Psych. Health. Med. 23(2), 171-177 (2018).
- Bennett C, Fagan E, Chaharbakhshi E et al. Implementing a protocol using glucose gel to treat neonatal hypoglycemia. Nursing. Women. Health. 20(1), 64-74 (2016).
- James-Todd T, March MI, Seiglie J et al. Racial differences in neonatal hypoglycemia among very early preterm births. J. Perinatol. 5, 1 (2017).
- Stomnaroska O, Petkovska E, Jancevska S et al. Neonatal hypoglycemia: risk factors and outcomes. Prilozi. 38(1), 97-101 (2017).
- Bennett C, Fagan E, Chaharbakhshi E et al. Implementing a protocol using glucose gel to treat neonatal hypoglycemia. Nurs. Women. Health. 20(1), 64-74 (2016).
- Lin SF, Kuo CF, Chiou MJ et al. Maternal and fetal outcomes of pregnant women with type 1 diabetes, a national population study. Oncotarget. 8(46), 80679 (2017).
- Mathiesen ER. Insulin aspart in diabetic pregnancy: state of the art. Women. Health. 4(2), 119-124 (2008).
- Parthasarathi D, Gajendra C, Dattatreya A et al. Analysis of pharmacokinetic & pharmacodynamic models in oral and transdermal dosage forms. J. Bioequiv. Availab. 3, 268-276 (2011).
- Elsaied EH, Dawaba HM, Ibrahim EA, et al. Investigation of proniosomes gel as a promising carrier for transdermal delivery of Glimepiride. Univ. J. Pharm. Res. 1(2), 1-18 (2016).
- Adapa D, Sarangi TK. A review on diabetes mellitus: complications, management and treatment modalities. J. Med. Health. Sci. 4(3), (2015).
- Abdulazeez SS. Freeze dried strawberry powder ameliorates alloxan induced hyperlipidemia in diabetic rats. Biomed. Res. 26(1), (2015).
- Hui ZG, Zhou XW, Li RJ et al. Studies on the extraction process of total flavonoids in Radix puerariae and their hypoglycemic effect in mice. Biomed. Res. 26(1), (2015).
- Ahmed R, Tanvir EM, Hossen M et al. Antioxidant properties and cardioprotective mechanism of malaysian propolis in rats. Evid. Based. Complementary. Alternative. Med. (2017).
- Usman UZ, Bakar AB, Mohamed M. Phytochemical composition and activity against hyperglycaemia of Malaysian propolis in diabetic rats. Biomed. Res. 27(1), (2016).
- Li J, Gong F, Li F. Hypoglycemic and hypolipidemic effects of flavonoids from tatary buckwheat in type 2 diabetic rats. Biomed. Res. 27(1), (2016).
- Pothamsetty A, Janarthan M, Faheemuddin M et al. Evaluation of anti-diabetic activity of the plant leaves of verbascum thapsus in alloxan induced diabetic rats. Int. J. Pharm. Pharmacol. 1, 118 (2017).
- Choudhury A, Chakraborty I, Banerjee TS et al. Efficacy of morin as a potential therapeutic phytocomponent: insights into the mechanism of action. Health. Sci. 6(11), 175-194 (2017).
- Al-Qudah MM, Haddad MA, EL-Qudah JM. The effects of aqueous ginger extract on pancreas histology and on blood glucose in normal and alloxan monohydrate-induced diabetic rats. Biomed. Res. 27(2), (2016).
- de la Fuente RA, Cuadrado NM, Tafur C et al. Histopathological differences in patients with biopsy-proven non-alcoholic fatty liver disease with and without type 2 diabetes. Endocrinologia. Diab. Y. Nutricion. (2018).
- Omaña-Molina M, Sanchez-Rocha R, Hernandez-Martinez D et al. Type 2 diabetes mellitus BALB/c mice are more susceptible to granulomatous amoebic encephalitis: Immunohistochemical study. Exp. Parasitol. 183, 150-159 (2017).
- Murata T, Tsuzaki K, Nirengi S et al. Diagnostic accuracy of the anti‐glutamic acid decarboxylase antibody in type 1 diabetes mellitus: Comparison between radioimmunoassay and enzyme-linked immunosorbent assay. J. Diab. Inves. 8(4), 475-479 (479).
- Zuo Y. The role of adiponectin gene mediated by NF-κB signaling pathway in the pathogenesis of type 2 diabetes. Eur. Rev. Med. Pharmacol. Sci. 22(4), 1106-1112 (2018).
- Piao M, Liu Y, Yu T et al. Zinc supplementation ameliorates ER stress and autophagy in liver in a rat model of type 2 diabetes mellitus. Biomed. Res. 27(4), (2016).
- Ekeanyanwu RC, Ejiogu RN, Egbogu MC. Lipid peroxidation and non-enzymatic antioxidants status in hypertension in diabetic and non-diabetic patients in Nigeria: a comparative study. Biomed. Res. 27(1), (2016).
- Hou K, Chen C, Wang X et al. Effects of emodin on blood glucose and body weight in type 1 diabetic rats. Univ. J. Pharm. Res. 2(4), 11-14 (2017).
- Prasanth DSNBK, Prasanna MM, Priyanka M et al. Pharmacognostic evaluation of gomphrena serrata root. Univ. J. Pharm. Res. 2(4), 6-10 (2017).
- Mirza MS, Ali SA, Sanghvi I. Evaluation of methanolic extract of euphorbia neriifolia stem bark on blood sugar levels, serum and tissue lipids in a preclinical model. Univ. J. Pharm. Res. 2(3), 1-5 (2017).
- Khan HA, Sobki SH, Alhomida AS. Regression analysis for testing association between fasting blood sugar and glycated hemoglobin in diabetic patients. Biomed. Res. (2015).
- Hompesch M, Muchmore DB, Morrow L et al. Improved postprandial glycemic control in patients with type 2 diabetes from subcutaneous injection of insulin lispro with hyaluronidase. Diab. Tech. Ther. 14(3), 218-224 (2012).
- Guo X, Wang W. Challenges and recent advances in the subcutaneous delivery of insulin. Expert. Opinion. Drug. Delivery. 14(6), 727-734 (2017).
- Hieronymus L, Geil P. Women & diabetes. Pregnant and pumping. Great expectations. Diab. Self-management. 20(2), 104-106 (2003).
- Azar M, Lyons TJ. Management of pregnancy in women with type 1 diabetes. Minerva. Endocrinologica. 38(4), 339-349 (2013).
- Veiseh O, Langer R. Diabetes: A smart insulin patch. Nature. 524(7563), 39 (2015).
- Veiseh O, Tang BC, Whitehead KA et al. Managing diabetes with nanomedicine: challenges and opportunities. Nature. Rev. Drug. Disc. 14(1), 45 (2015).
- Jahangir MA, Khan R, Imam SS. Formulation of sitagliptin-loaded oral polymeric nano scaffold: process parameters evaluation and enhanced anti-diabetic performance. Artificial. Cell. Nanomed. Biotech. 8, 1-3 (2017).
- O'donnell C, Efron N. Diabetes and contact lens wear. Clin. Exp. Optometry. 95(3), 328-337 (2012).
- Theng YL, Lee JW, Patinadan PV et al. The use of videogames, gamification, and virtual environments in the self-management of diabetes: a systematic review of evidence. Games. Health. J. 4(5), 352-361 (2015).
- Kawahito K, Sato H, Kadosaki M et al. Spike in glucose levels after reperfusion during aortic surgery: assessment by continuous blood glucose monitoring using artificial endocrine pancreas. General. Thoracic. Cardiovasc. Surg. 29, 1-5 (2017).
- Apablaza P, Soto N, Codner E. From insulin pump and continuous glucose monitoring to the artificial pancreas. Revista. Medica. Chile. 145(5), 630-640 (2017).
- Scalea JR, Pettinato L, Fiscella B et al. Successful pancreas transplantation alone is associated with excellent self-identified health score and glucose control: A retrospective study from a high-volume center in the United States. Clin. Transplantation. 32(2), (2018).
- Choi JY, Jung JH, Shin S et al. Association between the pancreas transplantation and survival of patients with diabetes: A single center experience. PloS. One. 12(11), e0186827 (2017).
- Kim YJ, Shin S, Han DJ et al. Long-term effects of pancreas transplantation on diabetic retinopathy and incidence and predictive risk factors for early worsening. Transplantation. 102(1), e30-e38 (2013).
- Alharthi S, Adair M, Das C et al. Robot offers no advantages in roux-en-y gastric bypass: analysis of the NIS database. Int. J. Gen. Med. Surg. 1, 112 (2017).
- Garg A, Vaya RK, Chaturvedi H. Effect of herbal medicine “diabetocure” on clinical and biochemical parameters of diabetes. Int. J. Pharm. Pharmacol. 1, 120 (2017).
- Lauria MW, Ribeiro-Oliveira A. Diabetes and other endocrine-metabolic abnormalities in the long-term follow-up of pancreas transplantation. Clin. Diab. Endocrinol. 2(1), 14 (2016).
- Pinchuk A, Dmitriev I, Lazareva K et al. Retroperitoneal pancreas transplantation with the use of duodenal drainage via “button technique”: first clinical practice. In. Trans. Proc. 49(10), 2347-2351 (2017).
- Lucisano JY, Routh TL, Lin JT et al. Glucose monitoring in individuals with diabetes using a long-term implanted sensor/telemetry system and model. IEEE. Trans. Biomed. Engg. 64(9), 1982-1993 (2017).
- Katz LB, Grady M, Stewart L et al. Patient and healthcare professional satisfaction with a new, high accuracy blood glucose meter with color range indicator and wireless connectivity. Exp. Rev. Med. Dev. 13(7), 619-626 (2016).
- Fernández-Luque L, Mejova Y, Mayer MA et al. Panel: big data & social media for empowering patients with diabetes. Stud. Health. Tech. Informatics. 225, 607-609 (2016).
- Carciani C, Bagnaschino L. Tech couturism, an alternative showcase for new fashion designers. In: Handbook of research on global fashion management and merchandising. 305-345(2016).
- Kume EM. Smart tattoos: an innovation in continuous glucose monitoring (2012).