Review Article - Imaging in Medicine (2012) Volume 4, Issue 2
PET/CT application in pediatric oncology
Leilei Yuan, Nan Zhang, Chunlin Li & Jigang Yang*Department of Nuclear Medicine, Beijing Friendship Hospital of Capital Medical University, 95 Yong An Road, Xi Cheng District, Beijing 100050, China
- Corresponding Author:
- Jigang Yang
Department of Nuclear Medicine
Beijing Friendship Hospital of Capital Medical University
95 Yong An Road, Xi Cheng District, Beijing 100050, China
E-mail: nmyangjigang@yahoo.com.cn
Abstract
Radionuclide functional imaging has become a central part of pediatric oncological practice. There have been a number of major advances in imaging technology in recent years. PET/CT is becoming an important imaging method in evaluating many pediatric malignancies, such as lymphomas, soft‑tissue tumors and sarcomas. PET/CT may provide information that is not detected by conventional imaging. During PET/CT application in pediatric patients, physicians should have the knowledge of the technical issues, pediatric anatomy and physiology that is different from adult patients. In this review, we describe the technical issues in pediatric PET/CT scan, false negative and positive cause in pediatric PET/CT images, and the value of PET/CT in pediatric oncology.
Keywords
oncology ▪ pediatric ▪ PET/CT
Background
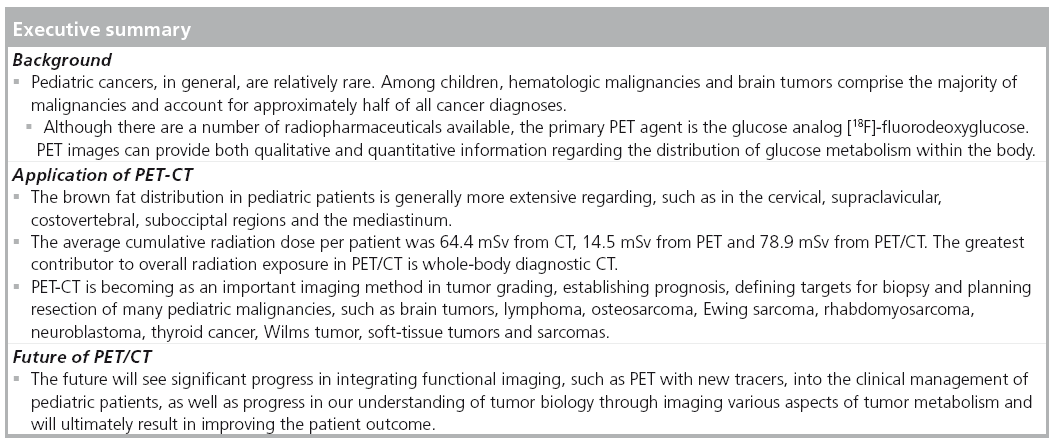
Pediatric cancers, in general, are relatively rare. Among children, the hematologic malignancies (leukemias and lymphomas) and brain tumors comprise the majority of malignancies and account for approximately half of all cancer diagnoses. While rare in adults, CNS tumor is the most common solid tumor in childhood, accounting for 21.2% of all cancers, and is the leading cause of cancer death in children [1]. Childhood brain tumors are different from those in adults in epidemiology, histologic features, and responses to treatment [1]. Although the outcome for children with brain tumors is poor, survival rates are better than in adults with similar tumors [1]. The 5-year survival for children with CNS tumors is reported to be as high as 74%. Sarcomas, malignancies that arise from mesenchymal cells, which normally mature into skeletal muscle, smooth muscle, fat, fibrous tissue, bone or cartilage, represent less than 6% of all childhood cancers. In children, the most common sarcomas are the primary bone tumors – osteosarcoma and Ewing sarcoma – and rhabdomyosarcoma, a tumor that may arise from any tissue except bone [2,3].
PET is a minimally invasive imaging technique in which a tracer amount of a radiopharmaceutical that is labeled with a positron emitter is injected into a patient and the resulting distribution imaged to map a physiological/biochemical process in the body. Although there are a number of radiopharmaceuticals available, the primary PET agent is the glucose analog [18F]-f luorodeoxyglucose (FDG). The PET images can provide both qualitative and quantitative information about the distribution of glucose metabolism within the body [4]. With respect to glucose uptake, many malignant cells are hypermetabolic and so many tumors can be located as areas of increased FDG accumulation on FDG-PET scans. This results in good sensitivity for malignant lesions [5]. PET with 3´-deoxy-3´-[18F]-fluorothymidine (FLT) can image cellular proliferation in cancers. FLT uptake has been shown to correlate with proliferation, such as the Ki-67 score, in many malignant cancers. FLT-PET may, therefore, be a good imaging tracer for evaluating tumor aggressiveness, predicting outcome, planning therapy and or monitoring therapy response. FLT-PET has shown greater specificity for cancer than FDG-PET because infection or inflammation can cause false-positive FDG uptake. However, the disadvantage of FLT is lower overall uptake and higher background activity in liver and bone marrow; FLT-PET should not be considered a potential replacement for staging. Instead, FLT-PET should be considered a powerful supplement to FDG-PET, providing additional diagnostic specificity and important biological information that could be useful in predicting prognosis, planning treatment and monitoring response. This technology could have exciting implications in oncology, including the possibility of assessing tumor grade and aggressiveness without the use of biopsy. This article will review the application of PET and CT in pediatric oncology [6].
Pediatric patient preparation
In FDG-PET/CT body imaging, pediatric patients should fast for 4 h before administration of FDG. Plasma glucose should be tested before the study. However, in contrast to adult patients, elevated fasting glucose levels are very uncommon in pediatric patients [7]. If the patient is too young to hold still and cooperate with imaging, sedation will be needed. When sedation is given, it is administered immediately before imaging. Oral intake is restricted for up to 8 h before sedation. Patients should not engage in strenuous exercise for 48 h before the PET/CT scan. Patients also lie still during the period from FDG injection until imaging is started to avoid uptake in skeletal muscle. Patients should void their bowels immediately before imaging.
A study by Hany et al. PET/CT demonstrated that symmetrical FDG uptake in the shoulder, neck and thoracic spine region is probably related to uptake in adipose tissue, especially in underweight patients. Prior to FDG-PET/CT, brown adipose tissue was believed to completely involute during infancy [8]. The intensity of cold stress seems to determine which regions of brown adipose tissue are activated. FDG uptake first appears in posterior cervical and supraclavicular regions, then costovertebral regions. With the greatest levels of cold stress, activity appears in the subocciptal regions and mediastinum [9]. However, brown fat distribution in the pediatric patient is generally more extensive. Many sites of brown fat uptake occur in areas that are rich in lymph nodes. This is a particular problem in children and adolescents with lymphoma as lymph nodes that are frequently involved in lymphoma are found in very close proximity to sites where brown adipose tissue activation occurs; this is particularly true in the posterior cervical, supraclavicular and mediastinum. Two methods have been used to successfully block cold stimulation of brown adipose tissue. The first and simplest method is to warm the patient and avoid cold stimulation. Patients can be asked to dress warmly. Patients can then be held in a warm room or warmed with preheated blankets for 30–60 min before FDG injection [10]. The second method is to pharmacologically block FDG uptake in brown adipose tissue. These drugs, such as diazepam, opiate, fentanyl and the b-blocker propranolol, can block transmission of cold receptor impulses through the hypothalamus and abolish postoperative shivering.
Radiation dosimetry
Typical doses of FDG used for PET imaging are of the order of 5–10 MBq/kg. This gives a usual range in the pediatric population of the order of 37–750 MBq. The contentious issue with respect to radiation dose is the value of the dose coefficient. The International Commission on Radiological Protection assigns a value of approximately 0.025 mSv/MBq. This means that the maximum effective dose to children who undergo PET scanning with FDG is between 0.925 and 18.75 mSv. Gelfand et al. have examined dosimetry for both PET and CT [11]. They reported that the radiation dose from their protocols for a CT of chest, abdomen and pelvis to be of the order of 10–16 mSv, while for PET scanning at a dose of 5.2 MBq/kg the estimated dose is 6 mSv for an average 5 year old and 8.6 mSv for an average 16 year old. When this is compared with the radiation dose of typical CT scans of chest, abdomen and pelvis, FDG PET scan doses are substantially less. For centers that undertake whole-body dual modality FDG PET/CT examinations, the effective dose per PET/CT exam is similar to the combined doses of CT and FDG done separately (at about 25 mSv) [12]. Chawla et al. also reported that the average effective dose was 20.3 mSv for CT (range: 2.7–54.2), 4.6 mSv for PET (range: 0.4–7.7) and 24.8 mSv for PET/CT (range: 6.2–60.7). The average cumulative radiation dose per patient was 64.4 mSv from CT (range: 2.7–326), 14.5 mSv from PET (range: 2.8–73) and 78.9 mSv from PET/CT (range: 6.2–399) [13]. The greatest contributor to overall radiation exposure in PET/CT is whole-body diagnostic CT. It is widely recognized that the radiation dose can be decreased significantly by decreasing the tube current (mA) value of a CT scan. PET/CT should be applied judiciously with particular emphasis on the risk, benefit and cumulative radiation dose to children [13]. Design of imaging protocols must take into account not only the usual protocol design considerations of PET and CT, but also artifact prevention in the combined PET/CT study and minimization of absorbed radiation dose in children and adolescents who are imaged. Beyer et al. has discussed similar questions in adult patients [14]. In adults, the PET/CT scan scope is from the base of the brain to the upper thighs. In children and adolescents, metastases to bone occur in a large number of malignant tumors. The metastases are often located in the long bones, occurring most frequently in the metaphyses. Imaging from the base of the brain to the ankles should be performed routinely in many pediatric malignancies, particularly those prone to bone metastases, such as neuroblastoma and sarcomas. The average length of a whole-body PET/CT is about 120 cm, which depend on the height of the patient.
Brain tumors
Gliomas make up over one half of all childhood brain tumors. According to the WHO classification, there are three main types of gliomas based on their histologic features: astrocytomas, oligodendrogliomas and mixed oligoastrocytomas. Analysis of the most malignant region of the tumors establishes grading: low grade or WHO grades I and II, and high grade or WHO grades III (anaplastic tumor) and IV (glioblastoma). In children, low-grade (grade I and II tumors) tumors are the most common type of glioma [15]. Metastasis from systemic tumors to the brain through hematogenous spread is uncommon in childhood. The top three most common childhood cancers that metastasize to the brain are melanoma (13.6%), germ cell tumors (13.5%), and osteosarcoma (6.5%) [16].
Clinical application of PET imaging in brain tumors has demonstrated that it is helpful in tumor grading, establishing prognosis, defining targets for biopsy, and planning resection. PET imaging may also be an effective method to distinguish recurrent tumors from treatment-induced changes. Malignant brain tumors, like many other soft-tissue tumors, show increased glucose metabolism, which is shown on FDG-PET scans. FDG-PET imaging of the brain presents unique challenges because of the high background glucose metabolism of normal gray matter structures compared with other organs. In addition to FDG PET, amino acid PET seems particularly suited for imaging brain tumors [17]. PET uptake with FDG is generally high in high-grade tumors. It is well established that FDG uptake has prognostic value in that anaplastic transformation can be acquired based on high FDG accumulation in a previously known low-grade tumor [18]. Another new tumor imaging tracer is amino acid and amino acid analog-PET agents. The biggest advantage is that there is a high uptake in tumor lesions and low uptake in normal brain tissue [19,20]. FDOPA as an amino acid analog was shown to be taken up through the blood–brain barrier in normal brains by the neutral amino acid transporter. In the most detailed and comprehensive study published on FDOPA in brain tumors, FDOPA demonstrated excellent visualization of highand low-grade tumors [21]. When FDG-PET is used to distinguish recurrent tumor tissue from radiation necrosis after treatment, it is important to: evaluate lesion activity not by the absolute uptake value and not by the ratio to untreated surrounding normal tissue, but by whether it is higher than the expected background activity based on the uptake in the adjacent normal brain tissue; and to compare it with the MRI structural information. Chao et al. studied a series of 44 lesions that had received stereotactic radiosurgery treatment. They reported that the sensitivity of FDG-PET alone was of 65% in patients with metastases, but reached 86% when MRI and PET images were explained at the same time [22].
Lymphoma
Lymphoma includes two main groups: Hodgkin disease (HD) and non-Hodgkin lymphoma. Accurate diagnosis of involved sites is important as it has both prognostic and therapeutic implications. Imaging for initial staging of lymphomas and for follow-up has conventionally been with CT, bone scan, ultrasound, MRI and gallium scanning. Moog et al. compared the FDG PET and CT role in staging of patients aged 7–72 years with untreated lymphoma. Staging was upgraded in four patients on seven confirmed additional PET findings and downgraded in one patient on a false-positive CT finding [23]. Juweid et al. reported that FDG-PET has a number of advantages, such as that PET requires less time to complete compared with a gallium scan and there is a lower radiation dose with PET (an estimated average 9 mSv for FDG-PET vs 23 mSv for gallium). Considering the quality of images and the availability of fused PET/CT images, anatomical localization is also improved with PET relative to gallium scanning. In addition, through the use of standardized uptake values (SUVs), a quantitative treatment response can be obtained. Hoh et al. reported that whole-body PET may be an accurate and cost-effective method for staging malignant lymphomas. They investigated seven HD and 11 NHL patients for staging or restaging and compared the cost and staging outcome of PET to conventional imaging studies. PET was almost half the cost. Accurate staging was performed in 17 out of 18 patients with PET compared with 15 out of 18 patients with conventional imaging [24]. Overall, the evidence suggests that staging of lymphomas with PET over conventional imaging is more accurate, quicker, results in less radiation to the patient and is less expensive. PET can also be used to monitor response during therapy, detect residual disease, identify relapse and provide prognostic information [25]. Rini et al. reported that PET was superior to gallium scanning for evaluating children and young adults with newly diagnosed HD [26]. Mody et al. reported that PET is more useful than either anatomical imaging or gallium scanning, especially in the evaluation of residual or recurrent masses. While anatomic imaging may show a residual mass, PET is more accurate in identifying active disease [27]. While PET alone has been shown to have value in staging, treatment response and assessment of residual masses at the end of therapy, PET/CT similarly has been shown to improve the accuracy of reporting. Furth et al. evaluated 33 children with HD and showed image fusion improves the observers’ confidence in interpretation and has an impact on therapeutic management [28]. Moskowitz et al. reported that pre-autologous stem cell transplant (ASCT) FDG-PET response to salvage chemotherapy (SLT) predicts outcome. This Phase II study uses both pre-SLT prognostic factors and post-SLT FDG-PET response in a risk-adapted approach to improve partial free survival following high-dose radio-chemotherapy (HDT) and ASCT. At a median follow-up of 51 months, event-free survival analyzed by intent to treat as well as for transplanted patients is 70 and 79%, respectively. Patients transplanted with negative FDG-PET, pre-HDT/ASCT, after one or two SLT programs, had an EFS of >80 vs 28.6% for patients with a positive scan (p < 0.001). This prospective study provides evidence that the goal of SLT in patients with HL should be a negative FDG-PET scan prior to HDT/ASCT [29].
Osteosarcoma
Osteosarcoma is the most common bone tumor of children and young adults, and 80% of osteosarcomas present between the ages of 5 and 25 years. Primary osteosarcoma occurs predominately in the metaphyses of the long bones of the extremities, with less than a third occurring in other locations. Over half the cases of osteosarcoma are found to have metastases, at or soon after, diagnosis. The most common site of metastatic disease is lung. Less commonly, 10–20% of metastases are in bone, but lymph node metastatic disease is rare [30]. FDG-PET has been used in the initial evaluation and staging of osteosarcoma. FDG-PET and conventional imaging modalities were equally effective in the detection of primary tumors ( 100% accuracy). PET was superior to conventional imaging modalities concerning the correct detection of lymph node involvement (sensitivity, 95 vs 25%, respectively) and bone manifestations (90 vs 57% sensitivity, respectively), whereas CT was more reliable than FDG-PET in depicting lung metastases (100 vs 25%sensitivity, respectively). FDG avidity, as measured by average maximum SUVmax, is higher in osteosarcoma than in most other sarcomas [31]. Franzius et al. reported that low FDG uptake is associated with longer event-free and overall survival in children with osteosarcoma [32]. Soon after the introduction of FDG-PET into clinical use, it was used to identify metastatic lung lesions in patients with osteosarcoma. Early investigators reported that 18F-FDG-PET and single detector CT had a similar accuracy for finding lung metastases [33], but Franzius et al. demonstrated that spiral CT detected twice as many lung metastases as FDG-PET [34]. Because the spatial resolution of the current generation of PET scanners is 7–8 mm, FDG-PET had greater value in more than 10 mm lesions. Performance of FDG-PET appears to be similar for nodules measuring at least 1 cm in diameter and larger mass lesions. Hamada et al. reported that in post-therapy, presurgical scan, the SUVmax is the strongest predictor of histopathological response to neoadjuvant chemotherapy. The standard imaging method for bone metastases in malignancies is the technetium methylene diphosphonate scan. Walter et al. compared the value of FDG-PET/CT and bone scan in the diagnosis of bone metastasis from sarcomas. Of these, 21 patients (72%) had bone sarcoma, whereas eight patients (28%) had soft-tissue sarcoma. The results showed that FDG PET/CT had an accuracy of 100%. Bone scan had accuracies of 90 and 82% demonstrated by patient-and case-based analysis. They concluded that 99mTc-MDP bone imaging did not provide an added diagnostic value for bone involvement over FDG-PET/CT [35].
Ewing sarcoma
Ewing sarcoma is a tumor of the skeleton and adjacent soft tissue, and is the second most frequent bone tumor of children and young adults [36]. Ewing tumors can occur anywhere in the body. Metastatic disease is common; approximately one quarter of patients have metastatic disease at diagnosis. Lung, bone and bone marrow are the most common sites of metastases [37]. The prognosis of Ewing tumors depends on the extent of disease and the use of appropriate therapy. The initial diagnosis of a Ewing tumor is typically made during assessment of symptoms with radiographs or MRI. For imaging the local primary disease site, the performance of 18F-FDG-PET is no better than conventional imaging, and tumor FDG avidity is not associated with prognosis in Ewing sarcoma [38]. Identification of sites of disease and localization of metastases affects staging and initial risk stratification, but is particularly important for Ewing sarcoma as all sites of disease receive local therapy. FDG-PET and whole-body MRI may have a role in identifying distant sites of disease. Although both FDG-PET and whole-body MRI can identify soft-tissue disease, neither is ideal for identifying lung metastases [34]. For identification of skeletal disease, both MRI and FDGPET are more sensitive than bone scan [39], but FDG-PET is more sensitive than whole body MRI [40]. Volker et al. reported that FDG-PET was 91% accurate, whereas conventional imaging was only 47% accurate in locating sites of distant disease, and FDG-PET findings led to changes in local control of chemotherapy in approximately half of the patients [31]. For Ewing sarcoma, MRI typically has been used for assessment of the response of local disease. MRI still relies on size criteria and contrast enhancement, although enhancement is somewhat related to size, not viability [41]. The ability to assess metabolic activity should allow FDG-PET to better assess response to therapy [42]
Rhabdomyosarcoma
Rhabdomyosarcoma is the most common malignant soft-tissue tumor affecting children and accounts for 4–8% cases of cancer in children younger than 15 years [43]. There are many histologic subtypes of rhabdomyosarcoma [44] and, in children, more than 70% of cases are the embryonal subtype while approximately one-fifth of cases are the alveolar subtype; other subtypes are rare. Volker et al. studied 12 rhabdomyosarcoma subjects. They reported that FDG-PET and conventional imaging performed equally in imaging the primary tumor, but FDG-PET was better than conventional imaging for identifying lymph node involvement [31]. McCarville et al. studied 28 subjects with childhood rhabdomyosarcoma and reported that FDG-PET/CT was sensitive for lymph node disease when used for initial staging [45]. These findings suggest that, in the management of rhabdomyosarcoma, two roles for FDG-PET are earlier identification of lymph node disease and excluding disease at sites of ambiguous findings on conventional imaging. FDG-PET can also be useful to detect widespread bone marrow involvement [46]. Very little has been reported regarding the use of FDG-PET or FDG-PET/CT in assessing the response of rhabdomyosarcoma to therapy.
Neuroblastoma
Conventionally, meta-iodobenzylguanidine (MIBG) has been the radiopharmaceutical used in the evaluation of neuroblastoma. MIBG can be labeled with iodine-131 or iodine-123. This norepinephrine analog requires the presence of a Type 1 catecholamine transport system [47]. Both neuroblastoma and pheochromocytoma usually, but not always, contain this transport system. MIBG has a reported sensitivity of greater than 85% for detecting neuroblastoma and it is useful for the detection of distant metastatic disease missed by anatomic imaging, including the evaluation of active bone marrow disease. It also allows for the differentiation of viable tumor tissue from treatment-related scar, which is not well assessed by CT or MRI [48]. FDG is not dependent on Type 1 catecholamine uptake and may be taken up in neuroblastomas that fail to accumulate MIBG as illustrated in the following case reports. Shulkin et al. reported the potential usefulness of PET in MIBG-negative neuroblastoma [49]. Kushner et al. studied the use of PET in monitoring disease status in patients with neuroblastoma. They reported that PET was useful in identifying disease in soft tissue as PET failed to identify only two MIBG-negative abdominal masses in 36 evaluations of 22 patients. PET and MIBG both showed more skeletal lesions than bone scans. However, PET was not helpful in identifying cranial lesions or marrow involvement because of physiologic uptake in the brain and marrow [50,51].
Thyroid cancer
Approximately 30% of endocrine neoplasms in children arise from the thyroid gland. The usual management is to surgically resect the thyroid and to ablate any residual gland and other sites of disease with radioactive iodine. Iodine-131 can also be used diagnostically to look for metastatic disease. Except in patients who express antithyroglobulin antibodies, biochemical measurements of thyroglobulin levels are likely to be the most sensitive way of detecting recurrent disease. Management is now moving towards imaging to look for metastatic disease when biomarkers suggest the presence of recurrence. Studies indicate that, in most cases, iodine-131 scanning has a higher sensitivity than FDG-PET. The opposite, however, is the case when the tumor dedifferentiates and loses the potential to concentrate iodine [52]. Such a dedifferentiated lesion is more likely to require surgery or other noniodine radiopharmaceuticals, as it will not concentrate enough iodine-131 for a therapeutic response. Up to 20% of these tumors may lose iodine avidity. FDGPET scanning may change clinical management in some of these cases. In an adult population, Hooft et al. reported that 115 had lesions on PET scans suspicious for recurrence. Of these, 90% were confirmed as true recurrences that had not been found by other imaging techniques. It appears that PET could have a role to play in the investigation of thyroid carcinoma [53].
Wilms tumor
Most Wilms tumors are solitary lesions, but up to 7% involve both kidneys, and up to 12% arise multifocally within one kidney. Experience with FDG-PET in Wilms tumor is limited, but reports indicate that the tumors are FDG avid. Shulkin et al. reported FDG-PET scanning is useful for the management of patients with Wilms tumors [54]. Misch et al. reported that PET is no more informative than traditional imaging in initial staging, particularly because the sensitivity of FDG-PET for the lung is limited and this is a common metastatic site for Wilms tumors [55].
Conclusion & future perspective
Combined FDG-PET/CT is being used more frequently in the diagnosis, tumor grading, establishing prognosis and ongoing surveillance of children with cancer. We should be familiar with its specific roles in individual tumor types. The future will see significant progress in integrating functional imaging, such as PET, into the clinical management of pediatric patients with cancer, as well as in our understanding of tumor biology through imaging various aspects of tumor metabolism, and ultimately in improving the patient outcome.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
- Packer RJ. Brain tumors in children. Arch. Neurol. 56, 421–425 (1999).
- Stein-Wexler R. Pediatric soft tissue sarcomas. Semin. Ultrasound CT MR 32, 470–488 (2011).
- Walter F, Federman N, Apichairuk W et al. (18)F-fluorodeoxyglucose uptake of bone and soft tissue sarcomas in pediatric patients. Pediatr. Hematol. Oncol. 28, 579–587 (2011).
- Gatenby RA, Gillies RJ. Why do cancers have high aerobic glycolysis? Nat. Rev. Cancer 4, 891–899 (2004).
- Rohren EM, Turkington TG, Coleman RE. Clinical applications of PET in oncology. Radiology 231, 305–332 (2004).
- Salskov A, Tammisetti VS, Grierson J, Vesselle H. FLT measuring tumor cell proliferation in vivo with positron emission tomography and 3´-deoxy-3´-[18F] fluorothymidine. Semin. Nucl. Med. 37, 429–439 (2007).
- Beaulieu S, Kinahan P, Tseng J et al. SUV varies with time after injection in (18)F-FDG PET of breast cancer: characterization and method to adjust for time differences. J. Nucl. Med. 44, 1044–1050 (2003).
- Hany TF, Gharehpapagh E, Kamel EM, Buck A, Himms-Hagen J, von Schulthess GK. Brown adipose tissue: a factor to consider in symmetrical tracer uptake in the neck and upper chest region. Eur. J. Nucl. Med. Mol. Imaging 29, 1393–1398 (2002).
- Gelfand MJ, O’Hara SM, Curtwright LA, Maclean JR. Pre-medication to block [(18)F] FDG uptake in the brown adipose tissue of pediatric and adolescent patients. Pediatr. Radiol. 35, 984–990 (2005).
- Zukotynski KA, Fahey FH, Laffin S et al. Constant ambient temperature of 24 degrees C significantly reduces FDG uptake by brown adipose tissue in children scanned during the winter. Eur. J. Nucl. Med. Mol. Imaging 36, 602–606 (2009).
- Gelfand MJ, Lemen LC. PET/CT and SPECT/CT dosimetry in children: the challenge to the pediatric imager. Semin. Nucl. Med. 37, 391–398 (2007).
- Brix G, Lechel U, Glatting G et al. Radiation exposure of patients undergoing whole-body dual-modality 18F-FDG PET/CT examinations. J. Nucl. Med. 46, 608–613 (2005).
- Chawla SC, Federman N, Zhang D et al. Estimated cumulative radiation dose from PET/CT in children with malignancies: a 5 year retrospective review. Pediatr. Radiol. 40, 681–686 (2010).
- Beyer T, Antoch G, Muller S et al. Acquisition protocol considerations for combined PET/CT imaging. J. Nucl. Med. 45(Suppl. 1), S25–S35 (2004).
- Schmandt SM, Packer RJ, Vezina LG, Jane J. Spontaneous regression of low-grade astrocytomas in childhood. Pediatr. Neurosurg. 32, 132–136 (2000).
- Curless RG, Toledano SR, Ragheb J, Cleveland WW, Falcone S. Hematogenous brain metastasis in children. Pediatr. Neurol. 26, 219–221 (2002).
- Poussaint TY, Phillips PC, Vajapeyam S et al. The neuroimaging center of the pediatric brain tumor consortium-collaborative neuroimaging in pediatric brain tumor research: a work in progress. Am. J. Neuroradiol. 28, 603–607 (2007).
- De Witte O, Levivier M, Violon P et al. Prognostic value positron emission tomography with [18F]fluoro-2-deoxy-Dglucose in the low-grade glioma. Neurosurgery 39, 470–476 Discussion 6–7 (1996).
- Ishiwata K, Kubota K, Murakami M et al. Re-evaluation of amino acid PET studies: can the protein synthesis rates in brain and tumor tissues be measured in vivo? J. Nucl. Med. 34, 1936–1943 (1993).
- Jager PL, Vaalburg W, Pruim J, de Vries EG, Langen KJ, Piers DA. Radiolabeled amino acids: basic aspects and clinical applications in oncology. J. Nucl. Med. 42, 432–445 (2001).
- Chen W, Silverman DH, Delaloye S et al. 18F-FDOPA PET imaging of brain tumors: comparison study with 18F-FDG PET and evaluation of diagnostic accuracy. J. Nucl. Med. 47, 904–911 (2006).
- Chao ST, Suh JH, Raja S, Lee SY, Barnett G. The sensitivity and specificity of FDG PET in distinguishing recurrent brain tumor from radionecrosis in patients treated with stereotactic radiosurgery. Int. J. Cancer 96, 191–197 (2001).
- Moog F, Bangerter M, Diederichs CG et al. Lymphoma: role of whole-body 2-deoxy-2- [F-18]fluoro-D-glucose (FDG) PET in nodal staging. Radiology 203, 795–800 (1997).
- Hoh CK, Glaspy J, Rosen P et al. Whole-body FDG-PET imaging for staging of Hodgkin’s disease and lymphoma. J. Nucl. Med. 38, 343–348 (1997).
- Rehm PK. Radionuclide evaluation of patients with lymphoma. Radiol. Clin. N. Am. 39, 957–978 (2001).
- Rini JN, Nunez R, Nichols K et al. Coincidence-detection FDG-PET versus gallium in children and young adults with newly diagnosed Hodgkin’s disease. Pediatr. Radiol. 35, 169–178 (2005).
- Mody RJ, Bui C, Hutchinson RJ, Frey KA, Shulkin BL. Comparison of (18)F flurodeoxyglucose PET with Ga-67 scintigraphy and conventional imaging modalities in pediatric lymphoma. Leuk. Lymphoma 48, 699–707 (2007).
- Furth C, Denecke T, Steffen I et al. Correlative imaging strategies implementing CT, MRI, and PET for staging of childhood Hodgkin disease. J. Pediatr. Hematol. Oncol. 28, 501–512 (2006).
- Moskowitz CH, Matasar MJ, Zelenetz AD et al. Normalization of pre-ASCT, FDG-PET imaging with second-line, non-cross resistant, chemotherapy programs improves event-free survival in patients with Hodgkin lymphoma. 119(7), 1665–1670 Blood (2011).
- Brenner W, Bohuslavizki KH, Eary JF. PET imaging of osteosarcoma. J. Nucl. Med. 44, 930–942 (2003).
- Volker T, Denecke T, Steffen I et al. Positron emission tomography for staging of pediatric sarcoma patients: results of a prospective multicenter trial. J. Clin. Oncol. 25, 5435–5441 (2007).
- Franzius C, Bielack S, Flege S, Sciuk J, Jurgens H, Schober O. Prognostic significance of (18) F-FDG and (99m)Tc-methylene diphosphonate uptake in primary osteosarcoma. J. Nucl. Med. 43, 1012–1017 (2002).
- Schulte M, Brecht-Krauss D, Werner M et al. Evaluation of neoadjuvant therapy response of osteogenic sarcoma using FDG PET. J. Nucl. Med. 40, 1637–1643 (1999).
- Franzius C, Daldrup-Link HE, Sciuk J et al. FDG-PET for detection of pulmonary metastases from malignant primary bone tumors: comparison with spiral CT. Ann. Oncol. 12, 479–486 (2001).
- Walter F, Czernin J, Hall T et al. Is there a need for dedicated bone imaging in addition to 18F-FDG PET/CT imaging in pediatric sarcoma patients? J. Pediatr. Hematol. Oncol. 34(2), 131–136 (2011).
- Furth C, Amthauer H, Denecke T, Ruf J, Henze G, Gutberlet M. Impact of whole-body MRI and FDG-PET on staging and assessment of therapy response in a patient with Ewing sarcoma. Pediatr. Blood Cancer 47, 607–611 (2006).
- Marec-Berard P, Philip T. Ewing sarcoma: the pediatrician’s point of view. Pediatr. Blood Cancer 42, 477–480 (2004).
- Hawkins DS, Schuetze SM, Butrynski JE et al. [18F]Fluorodeoxyglucose positron emission tomography predicts outcome for Ewing sarcoma family of tumors. J. Clin. Oncol. 23, 8828–8834 (2005).
- Mazumdar A, Siegel MJ, Narra V, Luchtman- Jones L. Whole-body fast inversion recovery MR imaging of small cell neoplasms in pediatric patients: a pilot study. Am. J. Roentgenol. 179, 1261–1266 (2002).
- Daldrup-Link HE, Franzius C, Link TM et al. Whole-body MR imaging for detection of bone metastases in children and young adults: comparison with skeletal scintigraphy and FDG PET. Am. J. Roentgenol. 177, 229–236 (2001).
- van der Woude HJ, Bloem JL, Hogendoorn PC. Preoperative evaluation and monitoring chemotherapy in patients with high-grade osteogenic and Ewing’s sarcoma: review of current imaging modalities. Skeletal Radiol. 27, 57–71 (1998).
- Franzius C, Sciuk J, Brinkschmidt C, Jurgens H, Schober O. Evaluation of chemotherapy response in primary bone tumors with F-18 FDG positron emission tomography compared with histologically assessed tumor necrosis. Clin. Nucl. Med. 25, 874–881 (2000).
- Raney RB, Anderson JR, Barr FG et al. Rhabdomyosarcoma and undifferentiated sarcoma in the first two decades of life: a selective review of intergroup rhabdomyosarcoma study group experience and rationale for Intergroup Rhabdomyosarcoma Study V. J. Pediatr. Hematol. Oncol. 23, 215–220 (2001).
- Wharam MD, Meza J, Anderson J et al. Failure pattern and factors predictive of local failure in rhabdomyosarcoma: a report of group III patients on the third Intergroup Rhabdomyosarcoma Study. J. Clin. Oncol. 22, 1902–1908 (2004).
- McCarville MB, Christie R, Daw NC, Spunt SL, Kaste SC. PET/CT in the evaluation of childhood sarcomas. Am. J. Roentgenol. 184, 1293–1304 (2005).
- Seshadri N, Wright P, Balan KK. Rhabdomyosarcoma with widespread bone marrow infiltration: beneficial management role of F-18 FDG PET. Clin. Nucl. Med. 32, 787–789 (2007).
- Shulkin BL, Shapiro B. Current concepts on the diagnostic use of MIBG in children. J. Nucl. Med. 39, 679–688 (1998).
- Portwine C, Marriott C, Barr RD. PET imaging for pediatric oncology: an assessment of the evidence. Pediatr. Blood Cancer 55, 1048–1061 (2010).
- Shulkin BL, Mitchell DS, Ungar DR et al. Neoplasms in a pediatric population: 2-[F-18]-fluoro-2-deoxy-D-glucose PET studies. Radiology 194, 495–500 (1995).
- Kushner BH, Yeung HW, Larson SM, Kramer K, Cheung NK. Extending positron emission tomography scan utility to high-risk neuroblastoma: fluorine-18 fluorodeoxyglucose positron emission tomography as sole imaging modality in follow-up of patients. J. Clin. Oncol. 19, 3397–3405 (2001).
- Murata Y, Kubota K, Yukihiro M, Ito K, Watanabe H, Shibuya H. Correlations between 18F-FDG uptake by bone marrow and hematological parameters: measurements by PET/CT. Nucl. Med. Biol. 33, 999–1004 (2006).
- AL-Nahhas A. Dedifferentiated thyroid carcinoma: the imaging role of 18F-FDG PET and non-iodine radiopharmaceuticals. Nucl. Med. Commun. 25(9), 891–895 (2004).
- Hooft L, Hoekstra OS, Deville W et al. Diagnostic accuracy of 18F-fluorodeoxyglucose positron emission tomography in the follow-up of papillary or follicular thyroid cancer. J. Clin. Endocrinol. Metab. 86, 3779–3786 (2001).
- Shulkin BL, Chang E, Strouse PJ, Bloom DA, Hutchinson RJ. PET FDG studies of Wilms tumors. J. Pediatr. Hematol. Oncol. 19, 334–338 (1997).
- Misch D, Steffen IG, Schonberger S et al. Use of positron emission tomography for staging, preoperative response assessment and posttherapeutic evaluation in children with Wilms tumour. Eur. J. Nucl. Med. Mol. Imaging 35, 1642–1650 (2008).


