Review Article - Imaging in Medicine (2009) Volume 1, Issue 2
How have developments in molecular imaging techniques furthered schizophrenia research?
Judy L Thompson1†, Nina Urban1 & Anissa Abi-Dargham1,21Department of Psychiatry, Columbia University and New York State Psychiatric Institute, 1051 Riverside Drive, Unit 31, New York, NY 10032, USA
2Deparment of Radiology, Columbia University/NYSPI, New York, NY, USA
- Corresponding Author:
- Judy L Thompson
Department of Psychiatry
Columbia University and New York State Psychiatric Institute
1051 Riverside Drive, Unit 31, New York, NY 10032, USA
Tel: +1 212 543 5505
Fax: +1 212 568 6171
E-mail: jt2358@columbia.edu
Abstract
Keywords
antipsychotic ▪ dopamine ▪ GABA ▪ glutamate ▪ occupancy ▪ PET ▪ schizophrenia ▪ serotonin ▪ SPECT
Schizophrenia is a chronic and severe mental illness that can have devastating consequences for those affected by it. Its characteristic symptoms tend to emerge in late adolescence or early adulthood [1] and include positive, or psychotic, symptoms (delusions, hallucinations and disorganization), negative symptoms (e.g., flat affect, poverty of speech, reduced motivation and social withdrawal) and cognitive dysfunction (e.g., attention, memory and executive functioning deficits) [2,3]. Although variable across patients, the course of this disorder is typically characterized by episodes of psychotic-symptom exacerbation or relapse, alternating with periods of partial remission [4]. Most individuals who develop schizophrenia experience a prodromal period lasting months to years during which nonspecific and attenuated positive symptoms emerge before the appearance of full-blown psychotic symptoms [5].
Over the past several decades, developments in in vivo neuroimaging techniques, including both structural and functional methodologies, have led to dramatic advances in the identification of brain abnormalities associated with schizophrenia. These findings have contributed to our knowledge of the brain regions, circuitry and neurotransmitters involved and thus have importantly informed our understanding of the pathophysiology of this disorder [6–8]. The aim of this article is to review the major findings related to the application of molecular or neurochemical imaging techniques that have advanced schizophrenia research. This review will focus specifically on neuroreceptor imaging using SPECT and PET.
Prior to the advent of SPECT and PET, postmortem studies were the primary means by which to investigate potential neurochemical system abnormalities in schizophrenia. Although postmortem work has contributed substantially to the understanding of the neurobiology of schizophrenia [9], such research is often limited owing to potential confounding effects of premortem antipsychotic medication exposure and the advanced age of its subjects, and of course cannot allow for the in vivo examination of molecular brain functions. The introduction of PET and SPECT techniques allowed, for the first time, the relatively direct examination of neurotransmitter functioning in the brains of living patients, including those who had never been exposed to antipsychotic medication. Since this time, neuroreceptor imaging in schizophrenia has been used in two ways: to study the pathophysiology of the illness, and to advance the understanding of the mechanisms of action of antipsychotic agents and inform the development of new treatments. After presenting a brief overview of neuroreceptor imaging methodology, we review findings from both types of investigation, with a particular focus on studies that have advanced our understanding of schizophrenia pathophysiology.
Brief overview of key concepts in neuroreceptor imaging
Molecular imaging techniques allow for the assessment of neurotransmitter receptor availability or expression, as well as neurotransmitter synthesis and release. This is achieved through the use of a radioactive tracer or ligand that is injected into a vein, crosses the blood–brain barrier and selectively binds to, or follows the metabolic pathway of, the molecular target of interest, such as a specific neuroreceptor or transporter. The measurement of radioactivity by the PET or SPECT scanner yields information regarding the accumulation of ligand throughout the brain; however, in addition to reflecting the radioligand that is specifically bound to the target receptor, the measured activity is also due to the radioligand that is nonspecifically bound (e.g., to nonreceptor proteins) and unbound or free [10]. Model-based methods are used to derive quantitative information concerning specific radioligand binding from the time course of activity measured in the brain regions of interest, a reference region and, for some methods, in arterial plasma [11,12].
Most in vivo molecular imaging studies use very small concentrations (a ‘tracer dose’) of the radioligand, both to avoid exposing subjects to pharmacological doses of the ligand and because of assumptions of the mathematical models used to quantify receptor parameters [11]. Thus, unlike in vitro methods, receptor density (Bmax) and affinity for a given ligand (1/KD) cannot be measured independently in vivo in humans with tracer-dose studies owing to the exposure to high doses of ligand required for such measures [13]. What can be obtained, however, is a measure that is equivalent to the product of receptor density and affinity (Bmax/KD); this measure was introduced by Mintun et al. and is called binding potential (BP) [13]. BP refers to the ratio of the concentration of specifically bound radioligand to a reference concentration of radioligand at equilibrium and thus provides quantitative information regarding binding to the receptor of interest. The reference concentrations of radioligand that comprise the denominators of the various BP measures used include the free plasma concentration (BPF), the total plasma concentration (BPP) and the nondisplaceable (i.e., the nonspecifically bound and free) concentration in brain tissue (BPND). Owing to experimental design and methodological issues, the most commonly reported measure is BPND. The reader is referred to [11,12] for indepth reviews of these measures and related methodological considerations, and to [10] for a discussion of nomenclature and other issues related to BP.
Another important consideration is the role of radioligand development in the advancement of in vivo molecular imaging for psychiatric disorders. The successful development of a suitable radioligand for a given target of interest is challenging, as the potential tracer must possess a number of very specific properties, such as favorable toxicology and optimal range of lipophilicity, receptor selectivity and affinity, and peripheral clearance [14]. Owing to these challenges, successful radioligand development has been a rate-limiting factor for new targets of investigation in neuroreceptor imaging. Currently, there are radioligands available for sites of the dopamine (DA) and serotonin systems, but relatively few for other systems for use in humans. For a discussion of instrumentation issues related to PET and SPECT, see [15,16].
Molecular imaging in schizophrenia: studies of pathophysiology
Dopamine
The hypothesis that DA dysfunction is involved in the pathophysiology of schizophrenia developed in the 1960s [17], and was supported indirectly by the observation that antipsychotic drugs are DA receptor antagonists [18], and that their clinical potency is strongly associated with their ability to block DA D2-like receptors [19,20]. It was further supported by work indicating that drugs that increase DA activity, such as amphetamine, can induce psychotic symptoms [21]. Such findings led to the initial formulation of the DA hypothesis of schizophrenia, which proposed that features of the illness result from excessive DA activity [17,22–24]. However, subsequent postmortem and cerebrospinal fluid studies of DA metabolites did not support a basal, homogeneous state of hyperdopaminergia in schizophrenia [25]. Furthermore, there was growing awareness that the enduring negative symptoms of schizophrenia are largely resistant to D2 receptor-blocking drugs, and observations that DA agonists can actually ameliorate the negative symptoms of the disorder in some patients [26,27]. In addition, neuropsychological, functional imaging and preclinical findings were converging to suggest that schizophrenia may be associated with deficient DA activity in cortical regions [25,28,29]. In an effort to reconcile these findings with the long-observed link between DA overactivity and psychotic symptoms, the initial DA hypothesis was reformulated [25,29]. Thus, the prevailing hypothesis is that schizophrenia is associated with both: hyperactivity of DA projections to subcortical regions, resulting in excessive stimulation of D2-like receptors and the psychotic symptoms of the illness; and deficient activity of DA projections to the prefrontal cortex (PFC) and the consequent hypostimulation of D1 receptors, which contribute to its negative and cognitive symptoms. Current views of the role of DA in schizophrenia, as summarized in a recent revision of the DA hypothesis by Howes and Kapur [30], emphasize the role of other systems (e.g., glutamate and GABA), as well as potential genetic and environmental risk factors (e.g., exposure to psychoactive drugs and/or early stress or trauma), in contributing to DA dysregulation. Thus, it is thought that striatal DA dysregulation, which results from multiple ‘hits’, is the final common pathway that leads to psychotic symptoms through a disturbance in the assignment of salience to stimuli [30].
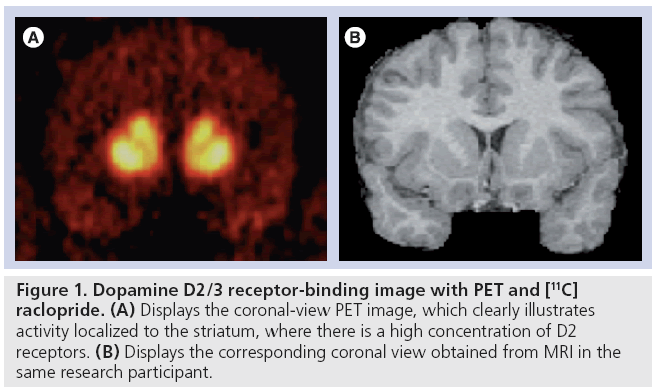
Neuroreceptor imaging techniques allow for a more direct examination of DA functioning in humans compared with previous methods (e.g., postmortem and metabolite studies) and, thus, have provided more definitive testing of the DA hypothesis of schizophrenia. Most research in this area has focused on the striatum, given that it receives extensive dopaminergic input from the midbrain and, unlike neocortical areas, has a rich supply of D2-like receptors [31], which are blocked by antipsychotic agents (Figure 1). There is also great interest in characterizing cortical DA functioning in schizophrenia, given hypotheses concerning its dysfunction in the illness. However, these efforts have been hampered to some degree by the low density of cortical DA receptors. To date, most neuroreceptor imaging studies of DA functioning in schizophrenia have used combined D2/D3 receptor radioligands. Similarly, imaging studies of D1-like receptors cannot as of yet distinguish between D1 and D5 receptors [32]. Thus, going forward, we will use ‘D2 receptors’ to refer to both D2 and D3 receptors, and ‘D1 receptors’ to refer to both D1 and D5 receptors, unless indicated otherwise.
Figure 1: Dopamine D2/3 receptor-binding image with PET and [11C] raclopride. (A) Displays the coronal-view PET image, which clearly illustrates activity localized to the striatum, where there is a high concentration of D2 receptors. (B) Displays the corresponding coronal view obtained from MRI in the same research participant.
Striatal DA functioning
D2 receptors
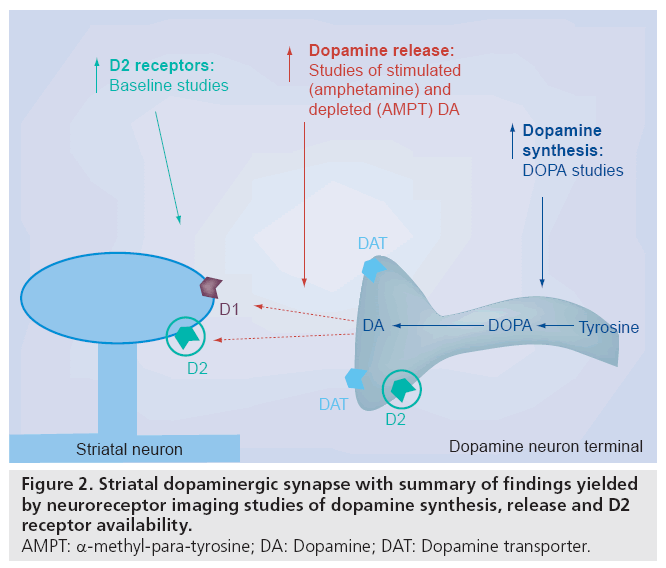
There are numerous PET and SPECT studies examining striatal D2 receptor availability or density in schizophrenia, both in previously treated and antipsychotic-naive patients. Such investigations have yielded mixed results. Some researchers observed a significant elevation in D2 receptor density in patients with schizophrenia compared with controls [33–35]; however, numerous studies found no statistically significant differences [27,36–42]. Given that numerous studies in this literature demonstrate a nonstatistically significant elevation in D2 receptors in patients compared with controls, some of the negative findings may be due to the small sample sizes and thus limited power that characterize many of these studies [43]. A meta-analysis of this literature that included 16 in vivo studies reported a modest but statistically significant increase in D2 receptors in untreated patients with schizophrenia compared with controls (effect size = 0.57; standard deviation = 0.78) (Figure 2) [43]. No clinical correlates of this elevation were reliably observed. Of note, group differences yielded by studies using butyrophenone radioligands had a significantly larger effect size than those observed with other radioligands (benzamides and lisuride). It is thought that such discrepant results obtained with different ligands may be due to differences in their susceptibility to being displaced from the receptor by endogenous DA combined with potentially increased endogenous DA in patients with schizophrenia compared with controls [43,44]. For a discussion of factors related to isotopes used, see [45].
A relatively recent PET study using [11C] raclopride found that D2 receptor availability was elevated in the caudate in unaffected monozygotic twins of patients with schizophrenia compared with control twins, but not in unaffected dizygotic twins; furthermore, the authors reported a negative association between D2 receptor density and performance on cognitive tasks (e.g., working memory and attention) that are considered sensitive to the genetic liability to the disorder [46]. Such results suggest that increased D2 receptor levels are associated with the genetic risk for schizophrenia.
Based on findings obtained with animal models [47,48], it has been hypothesized that the excessive stimulation of D2 receptors thought to underlie psychotic symptoms in schizophrenia may in part be due to an increase in the proportion of D2 receptors that are in the highaffinity (‘D2-high’), or functionally active, state [47–49]. However, most of the tracers available to probe D2 receptors in humans are antagonist ligands, and as such, cannot distinguish between the high- and low-affinity states of this receptor and, thus, cannot be used to address this hypothesis. The recently developed D2/3 ligand [11C]-(+)-PHNO is unique in that it is an agonist [50]; thus, it is thought to bind preferentially to D2 receptors when they are in their highaffinity state. Furthermore, this ligand displays a higher preference for the D3, compared with the D2, receptor [49,51]. Accordingly, it can be used to address hypotheses that previously could not be addressed in humans in vivo, including those regarding the D2-high state and the specific involvement of D3 in schizophrenia. Initial findings with this ligand in schizophrenia do not support the proposal that patients are characterized by a higher proportion of D2-high receptors or by increased D3 compared with controls, although the possible role of endogenous DA in masking such alterations cannot be ruled out by this study [49]. Therefore, additional work with this ligand, including possibly combining it with a DA depletion paradigm, is needed to more definitively address these questions.
D1 receptors
Neuroreceptor imaging studies of D1 receptor availability in unmedicated patients with schizophrenia have consistently found unaltered levels of striatal D1 in patients compared with controls [52–54]. Such results are consistent with those of most D1 postmortem studies of schizophrenia [55].
Amphetamine-induced DA release
Relatively recently, neuroreceptor imaging techniques have been developed that allow for the in vivo study of DA release or responsivity per se. These methods are based on the principle of competition between radioligand and endogenous neurotransmitter and provide a means for measuring dynamic fluctuations in intrasynaptic DA concentrations. When using a tracer that is displaceable from the DA receptor by endogenous DA, such as the D2 radioligand [11C]raclopride or [123I]IBZM, pharmacologically increasing intrasynaptic DA by means of a challenge, such as amphetamine, results in a reduction in radioligand BP; this decrease in BP provides an indirect measurement of pharmacologically stimulated DA release [56]. This paradigm has been validated by an abundant body of preclinical work [57]. For example, combined imaging and microdialysis studies with amphetamine in nonhuman primates have shown that the degree of reduction in radioligand BP is associated with the magnitude of increased extracellular DA following the challenge [57]. Of note, however, unresolved questions remain regarding the exact molecular mechanisms underlying the observed effects [57,58].
The three independent studies using this method have shown that amphetamine-induced striatal DA release is significantly greater in unmedicated patients with schizophrenia compared with controls (Figure 2) [27,36,37]. Moreover, Laruelle and colleagues [27,36,59] found that the transient amphetamine-induced exacerbation of positive symptoms observed in a subgroup of schizophrenia patients was associated with the degree of amphetamine-induced reduction in striatal [123I]IBZM BP. In addition, patients experiencing an acute phase of illness, including those at first episode who were antipsychotic naive, had a significantly greater degree of amphetamine-induced striatal DA release compared with those in remission. The remitted group did not differ significantly from controls on this index of DA release, although they were numerically higher than controls [59]. The findings of these studies marked an important advance in schizophrenia research, as they more directly than any prior results supported the proposal that excessive DA transmission at striatal D2 receptors is involved in the experiencing of psychotic symptoms. Furthermore, they more specifically indicated a role for a dysregulated, hyper-responsive subcortical DA system that fluctuates in its degree of dysregulation during different phases of the illness [56]. Since this time, Abi-Dargham and colleagues [60] have shown that as a group, patients with schizotypal personality disorder are also characterized by a larger reduction in striatal [123I]IBZM BP following amphetamine challenge compared with controls. The degree of amphetamine-induced [123I]IBZM displacement observed in schizotypal personality disorder was similar to that previously observed in remitted patients with schizophrenia but significantly lower than that seen in acutely ill schizophrenia patients [60]. Taken together, these results suggest that a more modest increase in DA release may characterize individuals at risk for psychosis, and that a larger degree of DA dysregulation characterizes those reaching the threshold of active psychosis.
Baseline DA release
Another imaging technique based on the principle of radioligand–neurotransmitter competition involves acutely depleting DA to ‘unmask’ DA receptors occupied by endogenous DA. The increase in radioligand BP observed after DA depletion indexes baseline occupancy of striatal D2 receptors by DA; thus, importantly, such measures provide information about baseline, or nonstimulated, DA release [61]. This interpretation of the results yielded by the DA depletion paradigm is supported by preclinical work [57]. However, as noted earlier, questions remain regarding the exact mechanisms underlying changes in radioligand BP following manipulations of synaptic DA levels [57].
In humans, this paradigm involves acutely depleting synaptic DA by orally administering the tyrosine hydroxylase inhibitor α‑methylpara- tyrosine (AMPT) over 48 h [62]. Using this technique with SPECT and the D2 radiotracer [123I]IBZM, Abi-Dargham and colleagues found that the increase in D2 receptor availability after acute DA depletion was significantly larger in patients with schizophrenia compared with controls, indicating increased occupancy of striatal D2 receptors by DA at baseline in schizophrenia [61]. Of note, all of the patients of this study were experiencing an episode of illness exacerbation. It was further noted that AMPT exposure led to a significant reduction in severity of positive symptoms among patients, and that higher occupancy of striatal D2 receptors by DA was significantly associated with a greater reduction in positive symptoms after 6 weeks of antipsychotic treatment [61]. Importantly, these results provided evidence that schizophrenia is characterized by excessive striatal D2 receptor stimulation by DA (Figure 2), and that the degree of this dysregulation is associated with the degree of therapeutic response to antipsychotic medication observed in patients. Of note, a small study involving antipsychotic-naive patients with schizophrenia who participated in both the amphetaminechallenge and DA-depletion paradigms indicated that indices of stimulated and baseline DA release are strongly associated in patients but not controls [63]. These results suggest that these measures are indexing the same pathological process in patients. They also highlight the variability in this DA transmission alteration across patients, which is an observation that informs our understanding of schizophrenia pathophysiology and may be important in the design of targeted treatment interventions [63].
Since the completion of these studies, advances in PET camera resolution and the development of methods to examine DA receptor parameters in the various subregions of the striatum have allowed researchers to probe aspects of DA transmission separately for the functional subdivisions of this heterogeneous structure [64,65]. Using these methods with PET and [11C]raclopride, it was found that patients with schizophrenia had a significantly larger increase in D2 receptor availability after DA depletion compared with controls in the associative striatum, but not in the limbic or sensorimotor striatal regions [66]. In particular, group differences were observed in the anterior (precommissural) dorsal caudate. This finding has challenged the notion that in schizophrenia, alterations in subcortical DA transmission are most prominently localized to the ventral, rather than dorsal, striatum and stimulated thinking regarding the potential role of the associative striatum in the illness [66]. This striatal region receives prominent input from the dorsolateral PFC (DLPFC), and is thought to play an important role in regulating the circuitry from various cortical regions that eventually projects back to the DLPFC; thus, these findings are consistent with hypotheses positing associations between cortical and subcortical abnormalities in the illness [66].
DA synthesis
Another important line of investigation for understanding DA dysfunction in schizophrenia has been the study of striatal DA synthesis and storage capacity through the assessment of DOPA decarboxylase activity. Using PET and either [b-11C]l-DOPA or [18F]DOPA, most [67–73] but not all [74,75] studies examining this index of DA synthesis capacity have found increased striatal DOPA uptake in patients with schizophrenia compared with controls. Of note, all investigations of patients experiencing an active psychotic episode at the time of scanning reported increased striatal DOPA uptake among patients [67,68,70]. Furthermore, one study reported an association between positive symptoms and [18F]DOPA uptake in the putamen [68,76]. Thus, overall, this body of work provides evidence that as a group, individuals with schizophrenia are characterized by elevated presynaptic DA synthesis/storage (Figure 2), and that this abnormality may be most evident in patients with active psychosis [76]. In addition, Meyer-Lindenberg and colleagues found that reduced activation in the DLPFC during an executive functioning task, as measured by PET with [15O]H2O, was associated with increased striatal DOPA uptake in patients but not controls [72], providing additional support for the relation between prefrontal dysfunction and potentiated striatal DA activity in the illness.
Howes and colleagues recently reported that striatal [18F]DOPA uptake was significantly increased among individuals experiencing prodromal symptoms of schizophrenia compared with controls, and that DOPA uptake correlated significantly with severity of prodromal symptoms [69]. Of note, these differences were observed in the associative, but not in the limbic or sensorimotor, striatum. Importantly, this study provides evidence that increased DA synthesis activity may occur before the full syndrome of schizophrenia emerges among those displaying prodromal symptoms of the illness. Furthermore, a recent study reported increased striatal [18F] DOPA uptake among nonpsychotic first-degree relatives of schizophrenia patients, suggesting that elevated presynaptic DA synthesis may be associated with the genetic vulnerability to the illness [77].
DA transporters
Dopamine transporters (DAT) are located on the presynaptic membrane of DA terminals and regulate phasic DA transmission at the synapse by rapidly removing DA from the synaptic cleft through reuptake [78]. Because striatal DAT are located exclusively on DA terminals, their measurement has been used to index the density of dopaminergic terminals or innervation into the striatum. Numerous studies have now examined striatal DAT density in antipsychoticnaive or -free patients with schizophrenia using either PET or SPECT and have failed to find significant differences between patients and controls [42,79–82]. These results, which are consistent with postmortem findings [83], suggest that the increased presynaptic striatal DA activity in schizophrenia indicated by other imaging parameters is not secondary to dysfunctional DAT or an elevation in the density of dopaminergic terminals. However, two studies using a dual-isotope SPECT technique with first-episode, antipsychotic-naive patients have reported a positive association between DAT and D2 receptor availability in patients but not controls [42,84]. Furthermore, using [99mTc] TRODAT-1 and SPECT, researchers recently observed a significant increase in DAT availability in a subgroup of patients with predominantly positive symptoms compared with controls [84]. Additional work is needed to confirm potential alterations of DAT availability in subgroups of patients, as well as to elucidate the underpinnings and functional consequences of these potential abnormalities.
Extrastriatal DA functioning
As noted earlier, numerous preclinical and clinical findings have suggested that schizophrenia is characterized by deficient DA transmission in cortical regions, such as the PFC, and that such dysfunction may contribute to the negative and cognitive symptoms of the disorder [28,29]. Thus, moving beyond the striatum and assessing DA functioning in the cortex is an important step in elucidating DA pathology in the illness.
D1 receptors
The D1 receptor is the most prevalent type of DA receptor in the neocortex [31] and thus characterizing its functioning, especially in the heavily implicated PFC, has been of great interest to schizophrenia researchers. The relatively recent development of suitable D1 PET radioligands has led to three published reports of D1 receptor availability in the PFC in schizophrenia. Using the PET radioligand [11C]SCH 23390, Okubo and colleagues reported a decrease in PFC D1 receptor availability in schizophrenia [54]; they also found that reduced D1 was significantly associated with more severe negative symptoms and cognitive impairment among patients. However, a second study with this radioligand failed to observe significant differences in PFC D1 between patients and controls [53].
Abi-Dargham and colleagues used the PET radioligand [11C]NNC 112 and found significantly elevated D1 in the DLPFC in patients compared with controls [52]. Furthermore, increased DLPFC D1 receptor availability was associated with poor working-memory performance among schizophrenia patients. Several factors may contribute to the discrepancies of these findings, including differences in clinical characteristics of the patient samples and aspects of PET methodology across studies [52]. Another complicating factor for this body of work is that recent research has confirmed that, in addition to D1, both of these radioligands bind to serotonergic 5‑HT2A receptors to a significant degree [85,86]. However, the finding across two studies [52,54] that alterations in radioligand BP was associated with impaired performance on tasks involving working memory in patients (specifically with decreased PFC [11C]SCH 23390 BP by Okubo et al. and increased PFC [11C]NNC 112 BP by Abi-Dargham et al.) suggests that these alterations may somehow reflect the same underlying DA deficit.
In an effort to understand the discrepant results yielded by the two radioligands, Guo et al. examined the effect of DA depletion on in vivo binding in rodents and found that subchronic, but not acute, DA depletion was associated with increased [11C]NNC 112 binding in the PFC and striatum [87], a change potentially reflecting an upregulation of D1 receptors in the face of sustained reductions in DA [87,88]. Subchronic DA depletion resulted in a decrease in [11C]SCH 23390 binding in the striatum (but not PFC); it is thought that this paradoxical response may be related to receptor externalization effects on [11C] SCH 23390 binding [57,87]. Based on such findings, it is thought that the reduced DLPFC [11C] NNC 112 BP observed in schizophrenia by Abi- Dargham and colleagues may reflect a compensatory increase in D1 receptor expression secondary to ongoing mesocortical DA dysfunction in the illness that may not detectable by [11C]SCH 23390 [52,88]. It is clear, however, that additional research is needed to clarify these issues and to further elucidate potential D1 receptor alterations in schizophrenia.
D2 receptors
Until recently, the available D2 radioligands only allowed measurement of these receptors in the striatum, where they are present in rich supply. The development of a new generation of radioligands with higher affinity for D2, including [18F]fallypride, [11C]FLB 457 and [123I] epidepride, has allowed researchers to probe D2 receptors in other, low density, brain regions that are implicated in the pathophysiology of schizophrenia, including limbic and cortical regions. Several studies, using PET or SPECT, have now examined D2 receptor availability in extrastriatal regions among untreated or antipsychotic- naive patients with schizophrenia. The most consistent result to emerge at this point is the finding of decreased D2 receptor availability in the thalamus of patients compared with controls [89–92]; however, this has not been observed across all studies [93,94]. Decreased D2 among patients has also been observed in the anterior cingulate [89,95], temporal cortex [89,96] and midbrain [94]; again, however, these findings have not been consistently observed [90,91,93,95]. A recent [18F]fallypride PET study reported increased D2 in the substantia nigra among patients [90]. Of note, significant inverse associations have been found between severity of positive symptoms and D2 receptor availability in the thalamus [89,92] and anterior cingulate [95], whereas one group reported a positive association between positive symptoms and D2 in the temporal cortex [90]. Several studies have failed to find alterations in D2 in the frontal cortex [91,93,95], although one group reported a positive association between frontal cortex D2 BP and severity of positive symptoms among their male patients with schizophrenia [93]. It should be noted that differences in D2 receptor availability (as measured by BP) may reflect differences in receptor density and/or endogenous DA levels [97]. Similarly, as with the striatum, alterations in the level of endogenous DA in these regions among patients may mask actual differences in receptor numbers. Additional research is needed to resolve the discrepancies across this body of work.
DA release
Research has shown that human in vivo binding of both [18F]fallypride and [11C]FLB 457 is vulnerable to acute changes in synaptic DA [98–100]. This has expanded the study of DA release from the striatum to extrastriatal and cortical regions, a step that is critical to more directly testing long-held hypotheses regarding cortical DA dysfunction in schizophrenia. Studies using these paradigms in schizophrenia have not yet been published but are currently underway.
Summary of DA findings
Taken together, molecular imaging studies have provided robust support for the long-held hypothesis positing subcortical DA hyperactivity in schizophrenia. Importantly, these findings converge in pointing to a hyper-responsive subcortical DA system (Figure 2) that fluctuates in its degree of dysregulation across phases of the illness; furthermore, DA dysregulation appears to be present to some degree during the prodromal period of the illness, before threshold psychotic symptoms emerge. Results suggest that this increased presynaptic DA functioning may be particularly evident in the dorsal caudate of the anterior striatum. Although still indirect at this point, molecular imaging findings are also consistent with the hypothesis that schizophrenia is characterized by deficient DA activity at D1 receptors in the PFC, and that such abnormalities are related to the cognitive dysfunction associated with the illness. As noted, several molecular imaging studies have also provided support for the proposed link between cortical and subcortical DA dysfunction.
Serotonin
A role for serotonin (or 5‑hydroxytryptamine [5‑HT]) dysfunction in the pathophysiology of schizophrenia was first proposed based on the structural similarity of serotonin and the hallucinogenic drug lysergic acid diethylamide, as well as the apparent effects of lysergic acid diethylamide on serotonin activity [101,102]. In particular, activity at the 5‑HT2A receptor was implicated in the positive symptoms of the disorder [102,103]. Interest in potential serotonin alterations in the illness, especially at the 5‑HT2 receptor, was strengthened after the introduction of clozapine, a drug that was shown to have superior efficacy for patients with ‘treatment-resistant’ schizophrenia and that acts to potently block 5‑HT2A receptors, even more so than D2 [103]. Numerous postmortem studies have supported the proposal of serotonin abnormalities in schizophrenia. Specifically, this work suggests that schizophrenia may be associated with alterations in the 5‑HT1A and ‑2A receptors and serotonin transporter (SERT) [103–107]. Relatively recently, the development of suitable 5‑HT receptor radioligands has allowed researchers to examine these markers of serotonin functioning in medication-free patients in vivo.
5‑HT2A receptors
Several PET studies have now examined 5‑HT2A receptor availability in untreated patients with schizophrenia and, in general, they have failed to find the reductions in cortical 5‑HT2A density suggested by some postmortem research. Specifically, four PET studies (two using [18F]setoperone, one using [11C] NMSP and one using [18F]altanserin) found no significant differences between patients and controls in cortical 5‑HT2A [108–111], suggesting that the cortical 5‑HT2A alterations detected by postmortem work may be secondary to premortem medication exposure. However, in a small study with six antipsychotic-naive patients and the PET radioligand [18F]setoperone, Ngan et al. did observe a significant decrease in 5‑HT2A receptor availability in the frontal cortex [112]. A more recent study using [18F]altanserin with antipsychotic-naive patients failed to replicate this finding, but reported increased 5‑HT2A among patients in the caudate nucleus [108]; however, given the low density of 5‑HT2A receptors in this brain region, the ligand employed for the striatum, and number of patients in this study, these results are considered preliminary (as noted by the authors) and in need of replication. Overall, additional research is needed with larger samples and more sensitive radioligands to clarify whether schizophrenia is associated with altered 5‑HT2A receptor availability per se.
5‑HT1A receptors
One of the most consistent serotonin abnormalities in schizophrenia to be observed in postmortem work is an increase in 5‑HT1A receptors in frontal cortical regions, including the PFC; this alteration is thought to potentially reflect an upregulation of these receptors secondary to decreased cortical serotonergic functioning [103]. Three PET studies using the radioligand [11C]WAY 100635 have now examined this receptor in schizophrenia in vivo and produced conflicting results. Tauscher and colleagues compared antipsychotic-naive patients with schizophrenia to controls and found increased 5‑HT1A receptor availability in the temporal, but not prefrontal, cortex [113]. By contrast, Yasuno et al. observed a decrease in [11C]WAY BP in the amygdala among patients compared with controls [114]; furthermore, they found that decreased 5‑HT1A receptor availability was associated with more severe negative and depressive/ anxiety symptoms. More recently, Frankle et al. failed to detect any significant differences in 5‑HT1A receptor availability between patients with schizophrenia and controls across 12 brain regions examined [115]. Although not clear, the discrepancies in results across these PET studies may be due to clinical heterogeneity in the patient samples and/or differences in the PET methodologies used. The failure of these PET studies to detect 5‑HT1A alterations in the PFC, in contrast to postmortem work, may relate to the poorer resolution of PET. Current PET technology does not allow for the quantification of receptor characteristics within specific cortical layers, and some postmortem studies suggest more pronounced increases of 5‑HT1A in schizophrenia in superficial cortical layers [105,107]. It is clear that additional in vivo work is needed to clarify the potential role of altered serotonin transmission and 5‑HT1A in schizophrenia pathophysiology. For example, the application of agonist ligands for 5‑HT1A (e.g., the recently developed [11C] CUMI‑101 [116]) to schizophrenia research will likely prove useful in further examining indices of potential serotonin system alterations in the disorder, such as the proportion of 5‑HT1A receptors that are in the high-affinity state [116].
Serotonin transporters
Serotonin transporters are located on presynaptic serotonin terminals and are involved in regulating serotonin transmission by removing it from the synaptic cleft via reuptake back into the presynaptic membrane. As with DAT, their density can be used to index the density of serotonin terminals or fiber innervation into various brain regions. The first SERT radioligand available was the SPECT tracer [123I]b-CIT, which labels SERT in the midbrain [117]. Using this ligand, Laruelle and colleagues found that patients with schizophrenia did not differ from controls in midbrain SERT availability [118]. A limitation of this study is that the radioligand used did not allow for assessment of SERT outside the midbrain region. The recently developed PET radioligand [11C]DASB, which has been shown to be superior to the previously introduced PET tracer [11C]McN 5652 for imaging SERT [119], allows for the assessment of this protein in other brain areas, including limbic and striatal regions. Frankle and colleagues used this radioligand to compare SERT availability in medication-free patients and controls and found no significant differences across the ten brain regions examined [120]. One limitation of this study is that [11C]DASB does not allow quantification of SERT in neocortical regions, where, among other regions, SERT abnormalities have been implicated by postmortem research. Thus, additional work, including with radioligands that allow for assessment of neocortical SERT (e.g., [11C]AFM), is needed to clarify potential SERT abnormalities in schizophrenia.
GABA
Numerous postmortem findings have suggested that schizophrenia may be characterized by deficient GABAergic functioning in cortical and limbic regions [121–124]. In vivo investigation of potential GABAergic alterations in the illness with PET and SPECT has been significantly hampered, however, by the relative lack of suitable radioligands for various indices of GABAergic functioning. To date, the only marker that has been investigated is the benzodiazepine binding site of the GABAA receptor complex. Three studies have used SPECT and the radioligand [123I]iomazenil to compare benzodiazepine receptor density between patients with schizophrenia and controls, and two out of three found no significant group differences across the regions examined [125,126]. When normalizing regional [123I]iomazenil uptake values for total brain uptake, however, Verhoeff and colleagues observed a significant decrease in relative [123I]iomazenil uptake in the left precentral gyrus of the frontal cortex in patients compared with controls, suggesting a potential reduction in benzodiazepine receptor density in this region in patients [127]. A more recent study using PET and the benzodiazepine radioligand [11C]Ro15-4513, which has relatively higher affinity for a‑5-containing GABAA receptors, did not find any significant differences between patients and controls across the regions examined [128]. Three studies have reported associations between clinical symptom severity and their index of benzodiazepine receptor concentration [126,128,129]. However, such associations have not been observed across all investigations [125]. Overall, this work is inconclusive, although it suggests that the illness is not characterized by marked alterations of benzodiazepine receptor density. Advances in PET technology and methodology (e.g., to allow for the detection of highly localized alterations, such as in specific cortical layers) and the development of novel radioligands for additional GABA markers (e.g., specific subunits and the GABA binding site of the GABAA receptor complex) should contribute to efforts to elucidate GABAergic alterations in schizophrenia.
One recently developed PET technique that holds promise for advancing this research may allow for the in vivo measurement of GABA release. Taking advantage of the increase in affinity of GABAA benzodiazepine receptors for benzodiazepine ligands in the presence of increased GABA levels (the ‘GABA shift’), Frankle and colleagues measured the increase in [11C]flumazenil BP after elevating GABA levels through GABA transporter blockade with tiagabine [130]. This change is thought to index acute increases in GABA levels. As expected, this manipulation resulted in significant increases in [11C]flumazenil BP in cortical and limbic regions among healthy controls [130]. Thus, in future studies, this method may lead to important progress in understanding potential alterations in GABA release in schizophrenia.
Glutamate
Several lines of evidence strongly implicate abnormal glutamate functioning in schizophrenia [121,131,132]. Particularly compelling are findings suggesting that the disorder is characterized by reduced functioning at the N-methyl-d-aspartate (NMDA) receptor, a type of glutamate receptor. For example, antagonists of the NMDA receptor, such as phencyclidine (PCP) and ketamine, produce behavioral effects in healthy humans that closely resemble the positive, negative and cognitive symptoms of schizophrenia [133,134], and, in stabilized patients, induce a re-emergence of idiosyncratic schizophrenia symptoms [131,135,136]. It is thought that reduced functioning at the NMDA receptor may, through disinhibition, lead to excessive glutamate release and hyperactivity at non-NMDA glutamate receptors [124,132,137]. As is the case for GABAergic investigations, the direct in vivo study of glutamatergic functioning, and NMDA receptors more specifically, has been hampered by the lack of suitable radioligands. The development of tracers for the binding site of PCP and ketamine (the NMDA/ PCP binding site) has been complicated by its intrachannel location [138]. Initial findings with a potential SPECT probe for this binding site ([123I]CNS-1261) are consistent with the hypothesis of NMDA receptor dysfunction in the illness [139]. However, owing to methodological concerns related to this radioligand, additional work with a more established tracer is needed to investigate potential alterations at the NMDA receptor in schizophrenia.
Another means by which investigators have used neuroreceptor imaging to understand potential glutamatergic alterations in schizophrenia has been to examine the effects of NMDA receptor antagonism on indices of DA functioning. These findings are mixed, with some reports indicating that in healthy controls, administration of ketamine (an NMDA receptor antagonist) may result in a significant increase in synaptic DA in the striatum [134] and posterior cingulate [140]; however, Kegeles et al. did not detect such changes in the striatum [141,142]. However, Kegeles and colleagues did find that ketamine administration in healthy controls resulted in more than a twofold increase in amphetamine-induced DA release, as indexed by reductions in [123I]IBZM BP [141]. In addition, it has been reported that recreational ketamine users are characterized by a significant upregulation of D1 receptor availability in the DLPFC; based on animal work, it is thought that such an alteration could be secondary to sustained reductions in prefrontal DA [143]. These findings are consistent with hypotheses of schizophrenia that link both increased subcortical DA release and deficient prefrontal DA functioning to disruptions in glutamatergic transmission at the NMDA receptor [141,144].
Future perspective: directions of the field
Molecular neuroimaging has contributed substantially to our understanding of the pathophysiology of schizophrenia. As recent applications of this methodology continue to develop along with the suitable molecular probes, it is likely that it will play an increasingly larger role in this research. For example, the findings of Howes et al., reviewed earlier, demonstrate the utility of PET in identifying neurochemical alterations in individuals who are experiencing prodromal symptoms of schizophrenia but have not yet developed the full syndrome [69]. Future studies to replicate this work, examine additional correlates of such abnormalities (e.g., genetic polymorphisms and stress responsivity) and prospectively assess indices of DA functioning will provide important insights regarding the developmental pathology of the illness and factors that may interact with pre-onset DA pathology to further increase risk.
Another promising development is assessing patients with multiple neuroimaging modalities. This multimodal approach, as used by Meyer- Lindenberg and colleagues [72], uniquely allows researchers to test hypotheses across multiple levels of analysis in the same patients. For example, Schobel and colleagues recently used MRI to measure regional cerebral blood volume (CBV) and observed that CBV was increased in the CA1 subfield of the hippocampus in patients with schizophrenia [145]. These results suggest that patients are characterized by elevated basal metabolism in this brain region. Furthermore, they found that among patients displaying prodromal symptoms of the illness, those who later converted to full psychosis were characterized by increased CBV in this region of the hippocampus compared with those who did not, suggesting that this alteration may be predictive of progression to psychotic illness [145]. Future studies combining this methodology with PET to assess DA functioning will provide a powerful means to test models of pathophysiology derived from animal research linking abnormal excitation in the hippocampus to elevated DA activity [146].
As reviewed earlier, Abi-Dargham and colleagues observed that higher baseline occupancy of striatal D2 receptors by DA was associated with a positive therapeutic response to antipsychotic treatment [61]. In addition to informing our understanding of pathophysiology, such findings can provide crucial information for the development of treatment strategies that tailor therapy with regard to the pathology characterizing subgroups of patients rather than using the same approach for all individuals who meet criteria for this heterogeneous disorder. Further research using molecular imaging to identify separate phenotypes within the illness, and markers of prognosis and treatment response in particular, should prove invaluable for the development of a more personalized medicine approach in this field. Such strategies may be particularly powerful when combining multiple imaging modalities (e.g., to characterize DA functioning, CBV and volume changes), along with behavioral assessments, to identify subgroups of patients characterized by a specific set of pathophysiological and clinical features. As demonstrated by Bose and colleagues [147], the use of computerized pattern-recognition tools may prove useful to these efforts. Furthermore, continued molecular imaging research with individuals who are experiencing prodromal symptoms of schizophrenia should allow such strategies to be extended back to before full illness onset [7,147]. Given that only a subset of young people who meet current prodromal research criteria will transition to full psychotic illness (e.g., 35%) [148], these potential developments, which should aid in predicting who will convert to psychosis, have important implications for the diagnosis of ‘prodromal’ patients and the development of tailored treatment strategies based on level of risk and the trajectory of pathophysiology in efforts to slow or even prevent illness progression.
Molecular imaging in schizophrenia: studies of pharmacotherapy
The use of molecular imaging to assess the neuroreceptor occupancy produced by antipsychotic drugs and the clinical correlates of this occupancy has significantly advanced our understanding of the potential mechanisms of action of these agents. Molecular imaging findings have also pointed to promising targets for novel pharmacological agents. Below we provide a brief overview of some of the major findings to emerge from this line of research. For more detailed reviews, see [144,149–151].
Studies of current antipsychotic agents
Early research showed that all antipsychotic compounds blocked D2 receptors, and that their clinical potency was strongly associated with their ability to block D2 in vitro [19,20,152]. Thus, it was assumed that striatal D2 receptor blockade was a key factor in the mechanism of action of antipsychotic agents [153]. The development of neuroreceptor imaging and suitable D2-receptor probes for PET and SPECT allowed for the assessment of antipsychotic action at this site to be directly assessed with patients in vivo. This large body of work is consistent in confirming that clinical doses of antipsychotic drugs block striatal D2 receptors to a substantial degree [154–156]. This research has also demonstrated repeatedly that striatal D2 receptor occupancy over approximately 80% is likely to result in the emergence of extrapyramidal symptoms (EPS; which are motor side effects of antipsychotics) [156]. Less clear from this work is the minimum occupancy of D2 needed for a clinical response. Striatal D2 occupancy at therapeutic doses of ‘typical’ or first-generation antipsychotics is high (e.g., 70–89%) [156]. For example, research with the typical agent haloperidol has indicated that the likelihood of a therapeutic response increases significantly at striatal D2 occupancy levels greater than 65% [157]. In general, therapeutic doses of ‘atypical’, or second-generation antipsychotics tend to produce lower striatal D2 occupancy levels than those reported for typical agents, although D2 occupancy varies across these agents [144,158]. Neuroreceptor imaging studies have also revealed that among patients clinically treated with antipsychotics, ‘nonresponders’ are characterized by high D2-receptor occupancy that is similar to those who experience a positive therapeutic response, indicating that in a given patient, failure to respond is not necessarily due to inadequate drug levels or D2 occupancy [159,160]. This insight importantly contributed to the consensus that treating poorly responsive patients with ‘mega doses’ of antipsychotics was not helpful [161]. Furthermore, such findings suggest that nonresponders may differ from responders with regard to pathophysiology, a notion consistent with results reviewed earlier indicating that in unmedicated patients, higher baseline occupancy of striatal D2 receptors by DA was associated with a positive therapeutic response to antipsychotic treatment [61].
The first ‘atypical’ antipsychotic to be introduced was clozapine, which was approved for use in the USA in the late 1980s. This marked a significant advance in the treatment of schizophrenia, as clozapine was shown to be uniquely effective in treating those patients whose illness was considered refractory [162,163]. Furthermore, compared with typical agents, clozapine has a reduced risk of inducing EPS at clinically effective doses [164]. Neuroreceptor imaging studies have indicated that therapeutic doses of clozapine produce a modest striatal D2 occupancy of approximately 20–65% [156,165,166]. Such findings challenged the notion that high striatal D2 receptor blockade, with its concomitant risk for EPS, was required for a drug to be an effective antipsychotic. Furthermore, unlike typical agents, it was shown that clozapine antagonizes the 5‑HT2A receptor to a substantial degree [165,166].
The superior efficacy and unique profile of clozapine invigorated attempts to develop antipsychotic drugs that, like clozapine, were more efficacious than the conventional agents, but that did not share with clozapine the risk for agranulocyctosis [150]. Since this time, a whole host of second-generation antipsychotics have been introduced, including a number that were developed based on their high 5‑HT2A/D2 affinity ratio, such as risperidone, olanzapine, quetiapine and ziprasidone. All of the secondgeneration agents were considered atypical, based on their apparently lower risk of EPS when used at clinically effective doses. Of note, however, at this point none has proven to be as clinically effective as clozapine [167,168].
The action of clozapine at 5‑HT2 receptors led to hypotheses concerning the potentially important role of high 5‑HT2A/D2 receptor affinity ratio for a favorable therapeutic profile [169,170]. However, current findings do not support the notion that 5‑HT2A receptor blockade per se is important in producing antipsychotic effects. A recent meta-analysis of PET and SPECT studies failed to find a significant association between clinical efficacy and 5‑HT2A receptor blockade for atypical antipsychotics [171]. It has also been noted that the atypical agent amisulpride does not have affinity for 5‑HT2A, and the atypical aripiprazole has a high D2/5‑HT2A affinity ratio [144,150]. Furthermore, a trial with M‑100907, a highly selective 5‑HT2A antagonist, indicated that this compound is not effective as an antipsychotic [172]. In addition, research suggests that at least when D2 receptor occupancy is high, 5‑HT2A blockade may not confer protection against EPS [173,174]. However, based on present findings, it cannot be excluded that 5‑HT2A blockade is an important aspect for some antipsychotic agents, in particular with regard to potential synergistic effects when combined with D2 receptor antagonism [144].
It has also been hypothesized that the atypical profile of antipsychotics such as clozapine may be related to a greater selectivity for D2 receptors in areas innervated by mesolimbic, rather than nigrostriatal, DA projections [144]. The development of high-affinity radioligands has allowed researchers to examine whether atypical antipsychotics bind preferentially to D2 in limbic regions, such as the temporal cortex, compared with D2 in the striatum. This body of work has yielded mixed findings, with some, but not all, studies suggesting that atypicals produce higher blockade of D2 in the temporal cortex than in the striatum [149]. In a recent meta-analysis of PET and SPECT studies, Stone and colleagues found that both typical and atypical antipsychotics blocked D2 receptors in the temporal cortex to a high degree (~70–80%), whereas only typical agents produced high D2 blockade in the striatum (~74 vs 49% observed for atypicals) [171]. The authors found significant associations between clinically effective doses and D2 occupancy (indexed by the dose producing maximal D2 occupancy across subjects for each antipsychotic) for both the temporal cortex and striatum, with a higher correlation observed for the temporal cortex. Based on these findings, they concluded that D2 occupancy in both brain regions likely plays a role in antipsychotic action [171]. A recent investigation by Kegeles et al. of the novel antipsychotic agent aripiprazole likewise reported higher occupancy levels in extrastriatal than striatal regions; of note, however, the authors found that clinical improvement in positive symptoms was significantly associated with striatal, but not extrastriatal, occupancy [175]. Such findings are consistent with Agid et al. [176], who found among patients taking either risperidone or olanzapine that reductions in positive symptoms were related to striatal, but not extrastriatal, blockade. Of note, however, the sample sizes in which clinical responses were determined for both Kegeles et al. and Agid et al. were small. It is clear that additional research is needed to address questions regarding regional selectivity and therapeutic responses [171,175,176].
It is important to note that to date, most studies examining regional selectivity of D2 occupancy have assessed binding in the striatum as a whole. As discussed earlier, however, the striatum is heterogeneous with regard to function and structure. One study by Stone et al. [177] with SPECT and [123I]epidepride reported that the atypical agents risperidone and amisulpride produced greater D2 blockade in the head of the caudate (corresponding to part of the associative striatum) compared with the putamen (part of which comprises the sensorimotor striatum). However, in two studies with PET and [18F]fallypride, Kessler and colleagues found that atypical drugs (specifically olanzapine, clozapine and quetiapine) did not show differential D2 occupancy between the ventral striatum and putamen [178,179].
The most recently introduced antipsychotic, aripiprazole, is novel in that it is a partial agonist at D2 receptors [180]. Occupancy studies of this drug have confirmed its partial agonist properties by demonstrating striatal occupancy higher than 80% in the absence of EPS [181,182].
Future perspective: drug development
The introduction of the first antipsychotic drugs in the 1950s marked a revolution in the treatment of schizophrenia. However, given the side effects associated with the currently available antipsychotics, the lack of response to these drugs in some patients, and the fact that negative and cognitive symptoms of the illness are largely nonresponsive to these treatments, the development of novel and more efficacious agents is an active area of research [150].
Neuroreceptor imaging is playing an increasingly important role in drug development [7,149,151]. Direct assessments of potential compounds with PET can facilitate drug development by aiding in the screening of promising therapeutic agents and informing dose selection and scheduling [151]. In conjunction with the continued development of novel radioligands, neuroreceptor imaging also provides the means to further elucidate the mechanism of action of therapeutic compounds that have unique profiles (e.g., clozapine, lamotrigine and LY354740) in humans [7,144]. In addition, molecular imaging findings on the pathophysiology of schizophrenia aid in the identification of novel targets for therapeutic compounds (e.g., D1, NMDA and muscarinic receptors) [144,149,150].
Conclusion
The development of molecular imaging techniques allowed for the first time the relatively direct examination of molecular brain functioning in living patients. The application of these techniques to schizophrenia has led to substantial advances in our understanding of the neurochemical abnormalities that characterize the illness. For example, the development of techniques and radiotracers over the last two decades has allowed researchers to move beyond assessing striatal DA receptor density to examining indices of DA synthesis and release. In doing so, molecular imaging studies have provided support for long-held hypotheses concerning DA dysfunction in the illness that previously could not be directly assessed in vivo. Furthermore, the application of these techniques to individuals experiencing the prodromal symptoms of schizophrenia has provided evidence that measurable alterations in DA functioning occur before threshold psychotic symptoms emerge. As discussed earlier, such findings will likely play an important role in the development of targeted treatment and prevention strategies by contributing to the identification of subgroups of patients characterized by specific pathophysiological features. Continued efforts to characterize extrastriatal DA functioning, as well as potential neurochemical alterations in other systems, should serve to further elucidate the pathophysiology of the illness. Molecular imaging studies have also informed our understanding of the mechanisms of action of drugs used to treat this illness. In addition, by contributing to the identification of novel targets and providing a means for evaluating the action of therapeutic compounds, these techniques are playing an increasingly important role in novel drug development. The application of PET and SPECT to these efforts will continue to expand with the ongoing development of novel methodologies, molecular probes and higherresolution scanners.
Financial & competing interests disclosure
A Abi-Dargham has received grant funding from NIH, NARSAD and Glaxo-SmithKline, and has received compensation from BMS-Otsuka for consulting and speaking engagements. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
- Hafner H, Maurer K, Loffler W, Riecher-Rossler A: The influence of age and sex on the onset and early course of schizophrenia. Br. J. Psychiatry 162, 80–86 (1993).
- Arndt S, Andreasen NC, Flaum M, Miller D, Nopoulos P: A longitudinal study of symptom dimensions in schizophrenia. Prediction and patterns of change. Arch. Gen. Psychiatry 52(5), 352–360 (1995).
- Barch DM: Neuropsychological abnormalities in schizophrenia and major mood disorders: similarities and differences. Curr. Psychiatry Rep. 11(4), 313–319 (2009).
- Lewis DA, Lieberman JA: Catching up on schizophrenia: natural history and neurobiology. Neuron 28(2), 325–334 (2000).
- an der Heiden W, Hafner H: The epidemiology of onset and course of schizophrenia. Eur. Arch. Psychiatry Clin. Neurosci. 250, 292–303 (2000).
- Gur RE, Keshavan MS, Lawrie SM: Deconstructing psychosis with human brain imaging. Schizophr. Bull. 33(4), 921–931 (2007).
- McGuire P, Howes OD, Stone J, Fusar-Poli P: Functional neuroimaging in schizophrenia: diagnosis and drug discovery. Trends Pharmacol. Sci. 29(2), 91–98 (2008).
- Shenton ME, Dickey CC, Frumin M, McCarley RW: A review of MRI findings in schizophrenia. Schizophr. Res. 49(1–2), 1–52 (2001).
- Benes FM: Emerging principles of altered neural circuitry in schizophrenia. Brain Res. Rev. 31(2–3), 251–269 (2000).
- Innis RB, Cunningham VJ, Delforge J et al.: Consensus nomenclature for in vivo imaging of reversibly binding radioligands. J. Cereb. Blood Flow Metab. 27(9), 1533–1539 (2007).
- Slifstein M, Laruelle M: Models and methods for derivation of in vivo neuroreceptor parameters with PET and SPECT reversible radiotracers. Nucl. Med. Biol. 28(5), 595–608 (2001).
- Slifstein M, Frankle W, Laruelle M: Ligand tracer kinetics: theory and application. In: Nuclear Medicine in Psychiatry. Otte A, Audenaert K, Peremans K, Heeringen K, Dierckx R (Eds). Springer Verlag, Berlin and Heidelburg, Germany 75–93 (2004).
- Mintun MA, Raichle ME, Kilbourn MR, Wooten GF, Welch MJ: A quantitative model for the in vivo assessment of drug binding sites with positron emission tomography. Ann. Neurol. 15, 217–227 (1984).
- Laruelle M, Slifstein M, Huang Y: Relationships between radiotracer properties and image quality in molecular imaging of the brain with positron emission tomography. Mol. Imaging Biol. 5(6), 363–375 (2003).
- Spanoudaki VC, Ziegler SI: PET and SPECT instrumentation. Handb. Exp. Pharmacol. 185(Pt 1), 53–74 (2008).
- Townsend DW: Physical principles and technology of clinical PET imaging. Ann. Acad. Med. Singapore 33(2), 133–145 (2004).
- van Rossum JM: The significance of dopamine receptor blockade for the mechanism of action of neuroleptic drugs. Arch. Int. Pharmacodyn. Therapy 160, 492–494 (1966).
- Carlsson A, Lindqvist M: Effect of chlorpromazine or haloperidol on formation of 3‑methoxytyramine and normetanephrine in mouse brain. Acta Pharmacol. Toxicol. 20, 140–144 (1963).
- Creese I, Burt DR, Snyder SH: Dopamine receptor binding predicts clinical and pharmacological potencies of antischizophrenic drugs. Science 192, 481–483 (1976).
- Seeman P, Lee T, Chau-Wong M, Wong K: Antipsychotic drug doses and neuroleptic/ dopamine receptors. Nature 261(5562), 717–719 (1976).
- Angrist BM, Gershon S: The phenomenology of experimentally induced amphetamine psychosis – preliminary observation. Biol. Psychiatry 2, 95–107 (1970).
- Matthysse S: Dopamine and the pharmacology of schizophrenia: the state of the evidence. J. Psychiatr. Res. 11, 107–113 (1974).
- Angrist B, Rotrosen J, Gershon S: Commentary on: “Differential effects of amphetamine and neuroleptics on negative vs. positive symptoms in schizophrenia.” Psychopharmacology 72, 17–19 (1980). Psychopharmacology (Berl). 158(3), 219–221 (2001).
- Grace AA: Cortical regulation of subcortical systems and its possible relevance to schizophrenia. J. Neural. Transm. 91, 111–134 (1993).
- Davis KL, Kahn RS, Ko G, Davidson M: Dopamine in schizophrenia: a review and reconceptualization. Am. J. Psychiatry 148, 1474–1486 (1991).
- Angrist B, Peselow E, Rubinstein M, Corwin J, Rotrosen J: Partial improvement in negative schizophrenic symptoms after amphetamine. Psychopharmacology (Berl). 78(2), 128–130 (1982).
- Laruelle M, Abi-Dargham A, van Dyck CH et al.: Single photon emission computerized tomography imaging of amphetamineinduced dopamine release in drug-free schizophrenic subjects. Proc. Natl Acad. Sci. USA 93(17), 9235–9240 (1996).
- Finlay JM: Mesoprefrontal dopamine neurons and schizophrenia: role of developmental abnormalities. Schizophr. Bull. 27(3), 431–442 (2001).
- Weinberger DR: Implications of the normal brain development for the pathogenesis of schizophrenia. Arch. Gen. Psychiatry 44, 660–669 (1987).
- Howes OD, Kapur S: The dopamine hypothesis of schizophrenia: version III – the final common pathway. Schizophr. Bull. 35(3), 549–562 (2009).
- Hall H, Sedvall G, Magnusson O, Kopp J, Halldin C, Farde L: Distribution of D1‑ and D2‑dopamine receptors, and dopamine and its metabolites in the human brain. Neuropsychopharmacology 11, 245–256 (1994).
- Missale C, Nash SR, Robinson SW, Jaber M, Caron MG: Dopamine receptors: from structure to function. Physiol. Rev. 78(1), 189–225 (1998).
- Crawley JC, Owens DG, Crow TJ et al.: Dopamine D2 receptors in schizophrenia studied in vivo. Lancet 2(8500), 224–225 (1986).
- Tune L, Barta P, Wong D et al.: Striatal dopamine D2 receptor quantification and superior temporal gyrus: volume determination in 14 chronic schizophrenic subjects. Psychiatry Res. 67(2), 155–158 (1996).
- Wong DF, Wagner HN Jr, Tune LE et al.: Positron emission tomography reveals elevated D2 dopamine receptors in drug-naive schizophrenics. Science 234(4783), 1558–1563 (1986).
- Abi-Dargham A, Gil R, Krystal J et al.: Increased striatal dopamine transmission in schizophrenia: confirmation in a second cohort. Am. J. Psychiatry 155(6), 761–767 (1998).
- Breier A, Su TP, Saunders R et al.: Schizophrenia is associated with elevated amphetamine-induced synaptic dopamine concentrations: evidence from a novel positron emission tomography method. Proc. Natl Acad. Sci. USA 94(6), 2569–2574 (1997).
- Farde L, Wiesel FA, Stone-Elander S et al.: D2 dopamine receptors in neuroleptic-naive schizophrenic patients. A positron emission tomography study with [11C]raclopride. Arch. Gen. Psychiatry 47, 213–219 (1990).
- Hietala J, Syvälahti E, Vuorio K et al.: Striatal D2 receptor characteristics in neurolepticnaive schizophrenic patients studied with positron emission tomography. Arch. Gen. Psychiatry 51, 116–123 (1994).
- Martinot J-L, Peron-Magnan P, Huret J-D et al.: Striatal D2 dopaminergic receptors assessed with positron emission tomography and [76Br]bromospiperone in untreated patients. Am. J. Psychiatry 147, 346–350 (1990).
- Talvik M, Nordstrom AL, Okubo Y et al.: Dopamine D2 receptor binding in drug-naive patients with schizophrenia examined with raclopride-C11 and positron emission tomography. Psychiatr. Res. 148(2–3), 165–173 (2006).
- Yang YK, Yu L, Yeh TL, Chiu NT, Chen PS, Lee IH: Associated alterations of striatal dopamine D2/D3 receptor and transporter binding in drug-naive patients with schizophrenia: a dual-isotope SPECT study. Am. J. Psychiatry 161(8), 1496–1498 (2004).
- Weinberger DR, Laruelle M: Neurochemical and neuropharmachological imaging in schizophrenia. In: Neuropsychopharmacology – The Fifth Generation of Progress. Davis KL, Charney DS, Coyle JT, Nemeroff C (Eds). Lippincott, Williams & Wilkins, Philadelphia, PA, USA 833–855 (2002).
- Seeman P, Niznik HB, Guan H-C: Elevation of dopamine D2 receptors in schizophrenia is underestimated by radioactive raclopride. Arch. Gen. Psychiatry 47, 1170–1172 (1990).
- Catafau AM, Suarez M, Bullich S et al.: Within-subject comparison of striatal D2 receptor occupancy measurements using [123I] IBZM SPECT and [11C]Raclopride PET. Neuroimage 46(2), 447–458 (2009).
- Hirvonen J, van Erp TG, Huttunen J et al.: Increased caudate dopamine D2 receptor availability as a genetic marker for schizophrenia. Arch. Gen. Psychiatry 62(4), 371–378 (2005).
- King MV, Seeman P, Marsden CA, Fone KC: Increased dopamine D2High receptors in rats reared in social isolation. Synapse 63(6), 476–483 (2009).
- Seeman P, Weinshenker D, Quirion R et al.: Dopamine supersensitivity correlates with D2High states, implying many paths to psychosis. Proc. Natl Acad. Sci. USA 102(9), 3513–3518 (2005).
- Graff-Guerrero A, Mizrahi R, Agid O et al.: The dopamine D2 receptors in high-affinity state and D3 receptors in schizophrenia: a clinical [11C]-(+)-PHNO PET study. Neuropsychopharmacology 34(4), 1078–1086 (2009).
- Wilson AA, McCormick P, Kapur S et al.: Radiosynthesis and evaluation of [11C]-(+)-4- propyl-3,4,4a,5,6,10b-hexahydro-2Hnaphtho[ 1,2-b][1,4]oxazin-9-ol as a potential radiotracer for in vivo imaging of the dopamine D2 high-affinity state with positron emission tomography. J. Med. Chem. 48(12), 4153–4160 (2005).
- Narendran R, Slifstein M, Guillin O et al.: Dopamine (D2/3) receptor agonist positron emission tomography radiotracer [11C]-(+)-PHNO is a D3 receptor preferring agonist in vivo. Synapse 60(7), 485–495 (2006).
- Abi-Dargham A, Mawlawi O, Lombardo I et al.: Prefrontal dopamine D1 receptors and working memory in schizophrenia. J. Neurosci. 22(9), 3708–3719 (2002).
- Karlsson P, Farde L, Halldin C, Sedvall G: PET study of D1 dopamine receptor binding in neuroleptic-naive patients with schizophrenia. Am. J. Psychiatry 159(5), 761–767 (2002).
- Okubo Y, Suhara T, Suzuki K et al.: Decreased prefrontal dopamine D1 receptors in schizophrenia revealed by PET. Nature 385(6617), 634–636 (1997).
- Guillin O, Abi-Dargham A, Laruelle M: Neurobiology of dopamine in schizophrenia. Int. Rev. Neurobiol. 78, 1–39 (2007).
- Laruelle M, Abi-Dargham A: Dopamine as the wind of the psychotic fire: new evidence from brain imaging studies. J. Psychopharmacol. 13(4), 358–371 (1999).
- Laruelle M: Imaging synaptic neurotransmission with in vivo binding competition techniques: a critical review. J. Cereb. Blood Flow Metab., 20(3), 423–451 (2000).
- Ginovart N: Imaging the dopamine system with in vivo [11C]raclopride displacement studies: understanding the true mechanism. Mol. Imaging Biol. 7(1), 45–52 (2005).
- Laruelle M, Abi-Dargham A, Gil R, Kegeles L, Innis R: Increased dopamine transmission in schizophrenia: relationship to illness phases. Biol. Psychiatry 46(1), 56–72 (1999).
- Abi-Dargham A, Kegeles L, Zea-Ponce Y et al.: Striatal amphetamine-induced dopamine release in patients with schizotypal personality disorders studied by SPECT and [123I]IBZM. Biol. Psych. 55, 1001–1006 (2004).
- Abi-Dargham A, Rodenhiser J, Printz D et al.: Increased baseline occupancy of D2 receptors by dopamine in schizophrenia. Proc. Natl Acad. Sci. USA 97(14), 8104–8109 (2000).
- Laruelle M, D’Souza CD, Baldwin RM et al.: Imaging D2 receptor occupancy by endogenous dopamine in humans. Neuropsychopharmacology 17(3), 162–174 (1997).
- Abi-Dargham A, Giessen EV, Slifstein M, Kegeles LS, Laruelle M: Baseline and amphetamine-stimulated dopamine activity are related in drug-naive schizophrenic subjects. Biol. Psychiatry 65, 1091–1093 (2009).
- Martinez D, Slifstein M, Broft A et al.: Imaging human mesolimbic dopamine transmission with positron emission tomography. Part II: amphetamine-induced dopamine release in the functional subdivisions of the striatum. J. Cereb. Blood Flow Metab. 23(3), 285–300 (2003).
- Mawlawi O, Martinez D, Slifstein M et al.: Imaging human mesolimbic dopamine transmission with positron emission tomography: I. Accuracy and precision of D2 receptor parameter measurements in ventral striatum. J. Cereb. Blood Flow Metab. 21(9), 1034–1057 (2001).
- Kegeles LS, Abi-Dargham A, Frankle WG et al.: Increased synaptic dopamine in associative regions of the striatum in schizophrenia. Arch. Gen. Psychiatry (2009) (In Press).
- Hietala J, Syvalahti E, Vuorio K et al.: Presynaptic dopamine function in striatum of neuroleptic-naive schizophrenic patients. Lancet 346(8983), 1130–1131 (1995).
- Hietala J, Syvalahti E, Vilkman H et al.: Depressive symptoms and presynaptic dopamine function in neuroleptic-naive schizophrenia. Schizophr. Res. 35(1), 41–50 (1999).
- Howes OD, Montgomery AJ, Asselin MC et al.: Elevated striatal dopamine function linked to prodromal signs of schizophrenia. Arch. Gen. Psychiatry 66(1), 13–20 (2009). nn First study to report on striatal dopamine synthesis among individuals experiencing prodromal symptoms of schizophrenia.
- Lindstrom LH, Gefvert O, Hagberg G et al.: Increased dopamine synthesis rate in medial prefrontal cortex and striatum in schizophrenia indicated by l‑(b-11C) DOPA and PET. Biol. Psychiatry 46(5), 681–688 (1999).
- McGowan S, Lawrence AD, Sales T, Quested D, Grasby P: Presynaptic dopaminergic dysfunction in schizophrenia: a positron emission tomographic [18F] fluorodopa study. Arch. Gen. Psychiatry 61(2), 134–142 (2004).
- Meyer-Lindenberg A, Miletich RS, Kohn PD et al.: Reduced prefrontal activity predicts exaggerated striatal dopaminergic function in schizophrenia. Nat. Neurosci. 5(3), 267–271 (2002).
- Reith J, Benkelfat C, Sherwin A et al.: Elevated dopa decarboxylase activity in living brain of patients with psychosis. Proc. Natl Acad. Sci. USA 91(24), 11651–11654 (1994).
- Dao-Castellana MH, Paillere-Martinot ML, Hantraye P et al.: Presynaptic dopaminergic function in the striatum of schizophrenic patients. Schizophrenia Res. 23(2), 167–174 (1997).
- Elkashef AM, Doudet D, Bryant T, Cohen RM, Li SH, Wyatt RJ: 6-18F-DOPA PET study in patients with schizophrenia. Positron emission tomography. Psychiatr. Res. 100(1), 1–11 (2000).
- Howes OD, Montgomery AJ, Asselin MC, Murray RM, Grasby PM, McGuire PK: Molecular imaging studies of the striatal dopaminergic system in psychosis and predictions for the prodromal phase of psychosis. Br. J. Psychiatry Suppl. 51, S13–S18 (2007).
- Huttunen J, Heinimaa M, Svirskis T et al.: Striatal dopamine synthesis in first-degree relatives of patients with schizophrenia. Biol. Psychiatry 63(1), 114–117 (2008).
- Grace AA: Dopamine. In: Neuropsychopharmacology: The Fifth Generation of Progress. Davis KL, Charney DS, Coyle JT, Nemeroff C (Eds). Lippincott, Williams & Wilkins, Philadelphia, PA, USA 119–132 (2002).
- Hsiao MC, Lin KJ, Liu CY, Tzen KY, Yen TC: Dopamine transporter change in drug-naive schizophrenia: an imaging study with 99mTc-TRODAT‑1. Schizophr. Res. 65(1), 39–46 (2003).
- Laakso A, Vilkman H, Alakare B et al.: Striatal dopamine transporter binding in neuroleptic-naive patients with schizophrenia studied with positron emission tomography. Am. J. Psychiatry 157(2), 269–271 (2000).
- Lavalaye J, Linszen DH, Booij J et al.: Dopamine transporter density in young patients with schizophrenia assessed with 123FP-CIT SPECT. Schizophr. Res. 47(1), 59–67 (2001).
- Schmitt GJ, Frodl T, Dresel S et al.: Striatal dopamine transporter availability is associated with the productive psychotic state in first episode, drug-naive schizophrenic patients. Eur. Arch. Psychiatry Clin. Neurosci. 256(2), 115–121 (2006).
- Seeman P, Niznik HB: Dopamine receptors and transporters in Parkinson’s disease and schizophrenia. FASEB J. 4(10), 2737–2744 (1990).
- Schmitt GJ, la Fougere C, Dresel S et al.: Dual-isotope SPECT imaging of striatal dopamine: first episode, drug naive schizophrenic patients. Schizophr. Res. 101(1–3), 133–141 (2008).
- Ekelund J, Slifstein M, Narendran R et al.: In vivo DA D1 receptor selectivity of NNC 112 and SCH 23390. Mol. Imaging Biol. 9(3), 117–125 (2007).
- Slifstein M, Kegeles LS, Gonzales R et al.: [11C]NNC 112 selectivity for dopamine D1 and serotonin 5‑HT2A receptors: a PET study in healthy human subjects. J. Cereb. Blood Flow Metab. 27(10), 1733–1741 (2007).
- Guo N, Hwang DR, Lo ES, Huang YY, Laruelle M, Abi-Dargham A: Dopamine depletion and in vivo binding of PET D1 receptor radioligands: implications for imaging studies in schizophrenia. Neuropsychopharmacology 28(9), 1703–1711 (2003).
- Abi-Dargham A, Moore H: Prefrontal DA transmission at D1 receptors and the pathology of schizophrenia. Neuroscientist 9(5), 404–416 (2003).
- Buchsbaum MS, Christian BT, Lehrer DS et al.: D2/D3 dopamine receptor binding with [F‑18]fallypride in thalamus and cortex of patients with schizophrenia. Schizophr. Res. 85(1–3), 232–244 (2006).
- Kessler RM, Woodward ND, Riccardi P et al.: Dopamine D2 receptor levels in striatum, thalamus, substantia nigra, limbic regions, and cortex in schizophrenic subjects. Biol. Psychiatry 65(12), 1024–1031 (2009).
- Talvik M, Nordstrom AL, Olsson H, Halldin C, Farde L: Decreased thalamic D2/D3 receptor binding in drug-naive patients with schizophrenia: a PET study with [11C]FLB 457. Int. J. Neuropsychopharmacol. 6(4), 361–370 (2003).
- Yasuno F, Suhara T, Okubo Y et al.: Low dopamine D2 receptor binding in subregions of the thalamus in schizophrenia. Am. J. Psychiatry 161(6), 1016–1022 (2004).
- Glenthoj BY, Mackeprang T, Svarer C et al.: Frontal dopamine D2/3 receptor binding in drug-naive first-episode schizophrenic patients correlates with positive psychotic symptoms and gender. Biol. Psychiatry 60(6), 621–629 (2006).
- Tuppurainen H, Kuikka JT, Laakso MP, Viinamaki H, Husso M, Tiihonen J: Midbrain dopamine D2/3 receptor binding in schizophrenia. Eur. Arch. Psychiatry Clin. Neurosci. 256(6), 382–387 (2006).
- Suhara T, Okubo Y, Yasuno F et al.: Decreased dopamine D2 receptor binding in the anterior cingulate cortex in schizophrenia. Arch. Gen. Psychiatry 59(1), 25–30 (2002).
- Tuppurainen H, Kuikka J, Viinamaki H, Husso-Saastamoinen M, Bergstrom K, Tiihonen J: Extrastriatal dopamine D2/3 receptor density and distribution in drug-naive schizophrenic patients. Mol. Psychiatry 8(4), 453–455 (2003).
- Wong DF: In vivo imaging of D2 dopamine receptors in schizophrenia: the ups and downs of neuroimaging research. Arch. Gen. Psychiatry 59(1), 31–34 (2002).
- Montgomery AJ, Asselin MC, Farde L, Grasby PM: Measurement of methylphenidate-induced change in extrastriatal dopamine concentration using [11C]FLB 457 PET. J. Cereb. Blood Flow Metab. 27(2), 369–377 (2007).
- Narendran R, Frankle WG, Mason NS et al.: Positron emission tomography imaging of amphetamine-induced dopamine release in the human cortex: a comparative evaluation of the high affinity dopamine D2/3 radiotracers [11C]FLB 457 and [11C]fallypride. Synapse 63(6), 447–461 (2009).
- Riccardi P, Li R, Ansari MS et al.: Amphetamine-induced displacement of [18F] fallypride in striatum and extrastriatal regions in humans. Neuropsychopharmacology 31(5), 1016–1026 (2006).
- Woolley DW, Shaw E: A biochemical and pharmacological suggestion about certain mental disorders. Proc. Natl Acad. Sci. USA 40, 228–231 (1954).
- Aghajanian GK, Marek GJ: Serotonin model of schizophrenia: emerging role of glutamate mechanisms. Brain Res. Brain Res. Rev. 31(2–3), 302–312 (2000).
- Abi-Dargham A: Alterations of serotonin transmission in schizophrenia. Int. Rev. Neurobiol. 78, 133–164 (2007).
- Burnet PW, Eastwood SL, Harrison PJ: 5‑HT1A and 5‑HT2A receptor mRNAs and binding site densities are differentially altered in schizophrenia. Neuropsychopharmacology 15(5), 442–455 (1996).
- Gurevich EV, Joyce JN: Alterations in the cortical serotonergic system in schizophrenia: a postmortem study. Biol. Psychiatry 42(7), 529–545 (1997).
- Laruelle M, Abi-Dargham A, Casanova MF, Toti R, Weinberger DR, Kleinman JE: Selective abnormalities of prefrontal serotonergic receptors in schizophrenia: a postmortem study. Arch. Gen. Psychiatry 50, 810–818 (1993).
- Simpson MD, Lubman DI, Slater P, Deakin JF: Autoradiography with [3H]8‑OHDPAT reveals increases in 5‑HT1A receptors in ventral prefrontal cortex in schizophrenia. Biol. Psychiatry 39(11), 919–928 (1996).
- Erritzoe D, Rasmussen H, Kristiansen KT et al.: Cortical and subcortical 5‑HT2A receptor binding in neuroleptic-naive first-episode schizophrenic patients. Neuropsychopharmacology 33(10), 2435–2441 (2008).
- Lewis R, Kapur S, Jones C et al.: Serotonin 5‑HT2 receptors in schizophrenia: a PET study using [18F]setoperone in neurolepticnaive patients and normal subjects. Am. J. Psychiatry 156(1), 72–78 (1999).
- Okubo Y, Suhara T, Suzuki K et al.: Serotonin 5‑HT2 receptors in schizophrenic patients studied by positron emission tomography. Life Sci. 66(25), 2455–2464 (2000).
- Trichard C, Paillere-Martinot ML, Attar-Levy D, Blin J, Feline A, Martinot JL: No serotonin 5‑HT2A receptor density abnormality in the cortex of schizophrenic patients studied with PET. Schizophr. Res. 31(1), 13–17 (1998).
- Ngan ET, Yatham LN, Ruth TJ, Liddle PF: Decreased serotonin 2A receptor densities in neuroleptic-naive patients with schizophrenia: a PET study using [18F]setoperone. Am. J. Psychiatry 157(6), 1016–1018 (2000).
- Tauscher J, Kapur S, Verhoeff NP et al.: Brain serotonin 5‑HT1A receptor binding in schizophrenia measured by positron emission tomography and [11C]WAY-100635. Arch. Gen. Psychiatry 59(6), 514–520 (2002).
- Yasuno F, Suhara T, Ichimiya T, Takano A, Ando T, Okubo Y: Decreased 5‑HT1A receptor binding in amygdala of schizophrenia. Biol. Psychiatry 55(5), 439–444 (2004).
- Frankle WG, Lombardo I, Kegeles LS et al.: Serotonin 1A receptor availability in patients with schizophrenia and schizo-affective disorder: a positron emission tomography imaging study with [11C]WAY 100635. Psychopharmacology (Berl). 189(2), 155–164 (2006).
- Milak MS, Severance AJ, Ogden RT et al.: Modeling considerations for 11C‑CUMI‑101, an agonist radiotracer for imaging serotonin 1A receptor in vivo with PET. J. Nucl. Med. 49(4), 587–596 (2008).
- Laruelle M, Baldwin RM, Malison RT et al.: SPECT imaging of dopamine and serotonin transporters with [123I]b‑CIT: pharmacological characterization of brain uptake in nonhuman primates. Synapse 13, 295–309 (1993).
- Laruelle M, Abi-Dargham A, van Dyck C et al.: Dopamine and serotonin transporters in patients with schizophrenia: an imaging study with [123I]b‑CIT. Biol. Psychiatry 47(5), 371–379 (2000).
- Huang Y, Hwang DR, Narendran R et al.: Comparative evaluation in nonhuman primates of five PET radiotracers for imaging the serotonin transporters: [11C]McN 5652, [11C]ADAM, [11C]DASB, [11C]DAPA, and [11C]AFM. J. Cereb. Blood Flow Metab. 22(11), 1377–1398 (2002).
- Frankle WG, Narendran R, Huang Y et al.: Serotonin transporter availability in patients with schizophrenia: a positron emission tomography imaging study with [11C]DASB. Biol. Psychiatry 57(12), 1510–1516 (2005).
- Benes FM: Amygdalocortical circuitry in schizophrenia: from circuits to molecules. Neuropsychopharmacology (2009) (Epub ahead of print).
- Lewis DA: GABAergic local circuit neurons and prefrontal cortical dysfunction in schizophrenia. Brain Res. Rev. 31(2–3), 270–276 (2000).
- Lewis DA, Hashimoto T, Volk DW: Cortical inhibitory neurons and schizophrenia. Nat. Rev. Neurosci. 6(4), 312–324 (2005).
- Lisman JE, Coyle JT, Green RW et al.: Circuit-based framework for understanding neurotransmitter and risk gene interactions in schizophrenia. Trends Neurosci. 31(5), 234–242 (2008).
- Abi-Dargham A, Laruelle M, Krystal J et al.: No evidence of altered in vivo benzodiazepine receptor binding in schizophrenia. Neuropsychopharmacology 20(6), 650–661 (1999).
- Busatto GF, Pilowsky LS, Costa DC et al.: Correlation between reduced in vivo benzodiazepine receptor binding and severity of psychotic symptoms in schizophrenia. Am. J. Psychiatry 154(1), 56–63 (1997).
- Verhoeff NP, Soares JC, D’Souza CD et al.: [123I]Iomazenil SPECT benzodiazepine receptor imaging in schizophrenia. Psychiatr. Res. 91(3), 163–173 (1999).
- Asai Y, Takano A, Ito H et al.: GABAA/ benzodiazepine receptor binding in patients with schizophrenia using [11C]Ro15–4513, a radioligand with relatively high affinity for a5 subunit. Schizophr. Res. 99(1–3), 333–340 (2008).
- Schröder J, Bubeck B, Demisch S, Sauer H: Benzodiazepine receptor distribution and diazepam binding in schizophrenia: an exploratory study. Psychiat. Res. Neuroimaging 68(2–3), 125–131 (1997).
- Frankle WG, Cho RY, Narendran R et al.: Tiagabine increases [11C]flumazenil binding in cortical brain regions in healthy control subjects. Neuropsychopharmacology 34(3), 624–633 (2009).
- Goff DC, Coyle JT: The emerging role of glutamate in the pathophysiology and treatment of schizophrenia. Am. J. Psychiatry 158(9), 1367–1377 (2001).
- Moghaddam B, Jackson ME: Glutamatergic animal models of schizophrenia. Ann. NY Acad. Sci. 1003, 131–137 (2003).
- Adler CM, Malhotra AK, Elman I et al.: Comparison of ketamine-induced thought disorder in healthy volunteers and thought disorder in schizophrenia. Am. J. Psychiatry 156(10), 1646–1649 (1999).
- Vollenweider FX, Vontobel P, Oye I, Hell D, Leenders KL: Effects of S‑ketamine on striatal dopamine: a [11C]raclopride PET study of a model psychosis in humans. J. Psychiatr. Res. 34(1), 35–43 (2000).
- Malhotra AK, Pinals DA, Adler CM et al.: Ketamine-induced exacerbation of psychotic symptoms and cognitive impairment in neuroleptic-free schizophrenics. Neuropsychopharmacology 17(3), 141–150 (1997).
- Jentsch JD, Roth RH: The neuropsychopharmacology of phencyclidine: from NMDA receptor hypofunction to the dopamine hypothesis of schizophrenia. Neuropsychopharmacology 20(3), 201–225 (1999).
- Gaspar P, Bustamante M, Silva H, Aboitiz F: Molecular mechanisms underlying glutamatergic dysfunction in schizophrenia: therapeutic implications. J. Neurochem. 111(4), 891–900 (2009).
- Bressan RA, Pilowsky LS: Imaging the glutamatergic system in vivo – relevance to schizophrenia. Eur. J. Nucl. Med. 27(11), 1723–1731 (2000).
- Pilowsky LS, Bressan RA, Stone JM et al.: First in vivo evidence of an NMDA receptor deficit in medication-free schizophrenic patients. Mol. Psychiatry 11(2), 118–119 (2006).
- Aalto S, Ihalainen J, Hirvonen J et al.: Cortical glutamate–dopamine interaction and ketamine-induced psychotic symptoms in man. Psychopharmacology (Berl). 182(3), 375–383 (2005).
- Kegeles LS, Abi-Dargham A, Zea-Ponce Y et al.: Modulation of amphetamine-induced striatal dopamine release by ketamine in humans: implications for schizophrenia. Biol. Psychiatry 48(7), 627–640 (2000).
- Kegeles LS, Martinez D, Kochan LD et al.: NMDA antagonist effects on striatal dopamine release: positron emission tomography studies in humans. Synapse 43(1), 19–29 (2002).
- Narendran R, Frankle WG, Keefe R et al.: Altered prefrontal dopaminergic function in chronic recreational ketamine users. Am. J. Psychiatry 162(12), 2352–2359 (2005).
- Abi-Dargham A, Laruelle M: Mechanisms of action of second generation antipsychotic drugs in schizophrenia: insights from brain imaging studies. Eur. Psychiatry 20(1), 15–27 (2005).
- Schobel SA, Lewandowski NM, Corcoran CM et al.: Differential targeting of the CA1 subfield of the hippocampal formation by schizophrenia and related psychotic disorders. Arch. Gen. Psychiatry 66(9), 938–946 (2009).
- Lodge DJ, Grace AA: Aberrant hippocampal activity underlies the dopamine dysregulation in an animal model of schizophrenia. J. Neurosci. 27(42), 11424–11430 (2007).
- Bose SK, Turkheimer FE, Howes OD et al.: Classification of schizophrenic patients and healthy controls using [18F] fluorodopa PET imaging. Schizophr. Res. 106(2–3), 148–155 (2008).
- Cannon TD, Cadenhead K, Cornblatt B et al.: Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch. Gen. Psychiatry 65(1), 28–37 (2008).
- Frankle WG: Neuroreceptor imaging studies in schizophrenia. Harv. Rev. Psychiatry 15(5), 212–232 (2007).
- Stone JM, Pilowsky LS: Antipsychotic drug action: targets for drug discovery with neurochemical imaging. Expert Rev. Neurother. 6(1), 57–64 (2006).
- Talbot PS, Laruelle M: The role of in vivo molecular imaging with PET and SPECT in the elucidation of psychiatric drug action and new drug development. Eur. Neuropsychopharmacol. 12(6), 503–511 (2002).
- Peroutka SJ, Snyder SS: Relationship of neuroleptics drugs effects at brain dopamine, serotonin, d-adrenergic and histamine receptors to clinical potency. Am. J. Psychiatry 137, 1518–1522 (1980).
- Pilowsky LS: Probing targets for antipsychotic drug action with PET and SPET receptor imaging. Nucl. Med. Commun. 22(7), 829–833 (2001).
- Baron JC, Martinot JL, Cambon H et al.: Striatal dopamine receptor occupancy during and following withdrawal from neuroleptic treatment: correlative evaluation by positron emission tomography and plasma prolactin levels. Psychopharmacology 99(4), 463–472 (1989).
- Farde L, Wiesel FA, Nordström AL, Sedvall G: D1- and D2-dopamine receptor occupancy during treatment with conventional and atypical neuroleptics. Psychopharmacology 99, S28–S31 (1989).
- Farde L, Nordstrom AL, Wiesel FA, Pauli S, Halldin C, Sedvall G: Positron emission tomographic analysis of central D1 and D2 dopamine receptor occupancy in patients treated with classical neuroleptics and clozapine. Relation to extrapyramidal side effects. Arch. Gen. Psychiatry 49(7), 538–544 (1992).
- Kapur S, Zipursky R, Jones C, Remington G, Houle S: Relationship between dopamine D2 occupancy, clinical response, and side effects: a double-blind PET study of first-episode schizophrenia. Am. J. Psychiatry 157(4), 514–520 (2000).
- Frankle WG, Gil R, Hackett E et al.: Occupancy of dopamine D2 receptors by the atypical antipsychotic drugs risperidone and olanzapine: theoretical implications. Psychopharmacology (Berl). 175(4), 473–480 (2004).
- Pilowsky LS, Costa DC, Ell PJ, Murray RM, Verhoeff NP, Kerwin RW: Antipsychotic medication, D2 dopamine receptor blockade and clinical response: a 123I IBZM SPET (single photon emission tomography) study. Psychol. Med. 23(3), 791–797 (1993).
- Wolkin A, Barouche F, Wolf AP et al.: Dopamine blockade and clinical response: evidence for two biological subgroups of schizophrenia. Am. J. Psychiatry 146(7), 905–908 (1989).
- Jones HM, Pilowsky LS: Dopamine and antipsychotic drug action revisited. Br. J. Psychiatry 181, 271–275 (2002).
- Kane J, Honigfeld G, Singer J, Meltzer H: Clozapine for the treatment-resistant schizophrenic. A double-blind comparison with chlorpromazine. Arch. Gen. Psychiatry 45(9), 789–796 (1988).
- Kane JM, Marder SR, Schooler NR et al.: Clozapine and haloperidol in moderately refractory schizophrenia: a 6‑month randomized and double-blind comparison. Arch. Gen. Psychiatry 58(10), 965–972 (2001).
- Wahlbeck K, Cheine M, Essali A, Adams C: Evidence of clozapine’s effectiveness in schizophrenia: a systematic review and meta-analysis of randomized trials. Am. J. Psychiatry 156(7), 990–999 (1999).
- Kapur S, Zipursky RB, Remington G: Clinical and theoretical implications of 5‑HT2 and D2 receptor occupancy of clozapine, risperidone, and olanzapine in schizophrenia. Am. J. Psychiatry 156(2), 286–293 (1999).
- Nordstrom AL, Farde L, Nyberg S, Karlsson P, Halldin C, Sedvall G: D1, D2, and 5‑HT2 receptor occupancy in relation to clozapine serum concentration: a PET study of schizophrenic patients. Am. J. Psychiatry 152(10), 1444–1449 (1995).
- Carpenter WT, Buchanan RW: Lessons to take home from CATIE. Psychiatr. Serv. 59(5), 523–525 (2008).
- Swartz MS, Stroup TS, McEvoy JP et al.: What CATIE found: results from the schizophrenia trial. Psychiatr. Serv. 59(5), 500–506 (2008).
- Meltzer H: Clinical studies on the mechanism of action of clozapine: the dopamineserotonin hypothesis of schizophrenia. Psychopharmacology 99, S18–S27 (1989).
- Meltzer H, Matsubara S, Lee J: Classification of typical and atypical antipsychotic drugs on the basis of dopamine D-1, D-2, and serotonin2 pKi values. J. Pharmacol. Exp. Ther. 251, 238–246 (1989).
- Stone JM, Davis JM, Leucht S, Pilowsky LS: Cortical dopamine D2/D3 receptors are a common site of action for antipsychotic drugs – an original patient data meta-analysis of the SPECT and PET in vivo receptor imaging literature. Schizophr. Bull. 35(4), 789–797 (2009).
- 172 de Paulis T: M‑100907 (Aventis). Curr. Opin. Investig. Drugs 2(1), 123–132 (2001).
- Kapur S, Remington G, Zipursky RB, Wilson AA, Houle S: The D2 dopamine receptor occupancy of risperidone and its relationship to extrapyramidal symptoms: a PET study. Life Sci. 57(10), L103–L107 (1995).
- Kapur S, Roy P, Daskalakis J, Remington G, Zipursky R: Increased dopamine D2 receptor occupancy and elevated prolactin level associated with addition of haloperidol to clozapine. Am. J. Psychiatry 158(2), 311–314 (2001).
- Kegeles LS, Slifstein M, Frankle WG et al.: Dose-occupancy study of striatal and extrastriatal dopamine D2 receptors by aripiprazole in schizophrenia with PET and [18F]fallypride. Neuropsychopharmacology 33(13), 3111–3125 (2008).
- Agid O, Mamo D, Ginovart N et al.: Striatal vs extrastriatal dopamine D2 receptors in antipsychotic response – a double-blind PET study in schizophrenia. Neuropsychopharmacology 32(6), 1209–1215 (2007).
- Stone JM, Bressan RA, Erlandsson K, Ell PJ, Pilowsky LS: Non-uniform blockade of intrastriatal D2/D3 receptors by risperidone and amisulpride. Psychopharmacology (Berl). 180(4), 664–669 (2005).
- Kessler RM, Ansari MS, Riccardi P et al.: Occupancy of striatal and extrastriatal dopamine D2/D3 receptors by olanzapine and haloperidol. Neuropsychopharmacology 30(12), 2283–2289 (2005).
- Kessler RM, Ansari MS, Riccardi P et al.: Occupancy of striatal and extrastriatal dopamine D2 receptors by clozapine and quetiapine. Neuropsychopharmacology 31(9), 1991–2001 (2006).
- Bolonna AA, Kerwin RW: Partial agonism and schizophrenia. Br. J. Psychiatry 186, 7–10 (2005).
- Mamo D, Graff A, Mizrahi R, Shammi CM, Romeyer F, Kapur S: Differential effects of aripiprazole on D2, 5‑HT2, and 5‑HT1A receptor occupancy in patients with schizophrenia: a triple tracer PET study. Am. J. Psychiatry 164(9), 1411–1417 (2007).
- Yokoi F, Grunder G, Biziere K et al.: Dopamine D2 and D3 receptor occupancy in normal humans treated with the antipsychotic drug aripiprazole (OPC 14597): a study using positron emission tomography and [11C] raclopride. Neuropsychopharmacology 27(2), 248–259 (2002).
• Provides a clear overview of concepts and issues related to measuring specific radioligand binding with binding potential measures.
• Provides excellent review and discussion of the theory and application of tracer kinetic modeling.
• • Thoroughly reviews and critically examines findings and assumptions related to interpreting changes in radioligand binding potential following manipulations of synaptic dopamine levels.
• • Reports increased amphetamine-induced striatal dopamine release in schizophrenia, the magnitude of which differs between patients experiencing an acute episode and those in remission.
• • First study to report that schizophrenia is associated with increased occupancy of striatal D2 receptors by dopamine; the authors also found that among patients, higher occupancy of striatal D2 by dopamine is associated with greater reductions in positive symptoms following antipsychotic treatment.
• Reported that ketamine users are characterized by significant upregulation of D1 receptor availability in the dorsolateral prefrontal cortex; such findings contribute to our understanding of relations between chronic N-methyl-d-aspartate receptor antagonism and prefrontal cortex dopamine functioning in humans.
• Excellent review and discussion of results related to potential mechanisms of action of antipsychotics in the context of relevant pathophysiology findings.