Research Article - Diabetes Management (2016) Volume 6, Issue 6
Taking a Moment to Pay Respects to People with Type-2 Diabetes
- Corresponding Author:
- Puziah Y
Deputy Dean, School of Nursing
KPJ Healthcare University college
Negeri Sembilan, Malayasia
E-mail: puziah@kpjuc.edu.my/puziahy@gmail.com
Abstract
Living with diabetes is not simple. Beyond those like eating healthy food, keeping active and taking medication, often ignored is a struggle on emotion, spiritual and psychological. Numerous studies suggests for the best way of managing people with diabetes is through holistic or functional approach. They need support to success, which involve a patient-centred collaborative approach to promote self-care activities, education and empowerment. However, to date, initiative to support people with type-2 diabetes and healthcare professionals to achieve those have largely been segregated which results in delayed process of adaptations and engagement of self-care. Hence, this study attempts to explore the process undertaken by people with type-2 diabetes engaging in and adaptingself-management behaviour from the nursing perspective. This is part of a larger study in developing a support system strategy to assist vulnerable population of people with type-2 diabetes in self-management adherence. Views from health professionals and family members also considered. The research study used qualitative methods of reflective and personal diaries, individual interviews, focus group and longitudinal observations. Thirty individual were repeatedly interviewed over two yearsin various setting, within a central region of Malaysia from June 2013 to December 2015. Opportunity to spend time over nine months with six people with type-2 diabetes provide in-depth understanding of this study in making constant comparison and triangulation. Rich data were electronically recorded and transcribed verbatim. Data generation and analysis occurred concurrently, which enabled the identification of emerging themes and issues from earlier data to guide future study in topic areas. There are four major themes emerged; Denial Associated Behaviour, Uncertainty and Unpredictable, Engagement and Disengagement, Self-Efficacy & Coping Strategies.
Keywords
type 2 diabetesprimary care;adherence behaviour;self-care;daily living of diabetes;diabetic support
Introduction
Self-care of type-2 diabetes is an important part in diabetes management. This is because most of the care practices are carried out by individuals in their homes [1-4]. This situation make them vulnerable to both positive and negative influence that may affects their decision about self-care; social networking; interaction with health care providers, families and society. Each of these factors will eventually become as an influencer or barrier to self-management behaviour [5-8].
Facilitators and barriers to self-management behaviour have been described extensively by many scholars. Factors associated with successful self-managementperformance involves; gender high social position, social support, high selfefficacy, and good psychological status [9-16]. Other factors also reported having less selfmanagement performance such as minority ethnic groups, and in a vulnerable financial position, comorbidities, low self-efficacy and living in high social responsibility demands [17-25]. To date, there are a huge amounts of research related to factors affecting selfmanagement performance, but the pattern of behaviour development in the face of dealing with those challenges on day-to-day basis was not properly documented.
Learning to perform self-management activities themselves and to practice these behaviours in daily life in the face of other responsibilities is psychologically complex and burdensome to most people [26]. However, people differ in their judgment, and so as the ability to deal effectively with the demands of diabetes selfmanagement [27]. Subgroups of patients with diabetes are more psychologically vulnerable than others and need special attention [28]. This experience can negatively affect the wellbeing and ability to function of the person. Because of this complexity, healthcare providers need to have not only re-teach skills, but the most important is a good understanding of the psychosocial impact of diabetes on daily living and behavioural studies to improve people’s ability to cope.
This study is to highlight the impact of diabetes and psychosocial needs of people with diabetes and their families. It is part of a larger study with the intention to empower people with type-2 diabetes to effectively self-managing their disease. The goal is to provide participants with knowledge and skills in handling selfmanagement tasks themselves. These findings informthe future research in developing strategy for a support system by integrating behavioural and emotional component in self-management education program for people with type-2 diabetes.
The discussion in this study lies on the assumption that life modification of people with type-2 diabetes is critical, and they need supports throughout the process and at different levels of self-management adjustments. Lifestyle modification is not easy to achieve and maintain [29-32]. Thereby, distress related to diabetes management seemsto be a norm in everyday life that includes; fear of hypoglycaemia and longterm complications [33-35]. This condition can last fora year after diagnosis manifesting itself emotions such as anger, fear, and disappointment [36-38]. This is the reason for the development of clinical depression is more common in diabetes than in the general population [39]. However, various types of cognitive strategies and behavioural approaches have proven effective in helping patients to cope with the demands of diabetes self-management and the conditions related to stress [40-45]. The role of health care professionals in this regard is essential. It is their obligations to provide support based on the principles of transparency, trustworthy, and not to make assumptions about whothe people are,instead of what they need or need to appreciate, or what motivates them.
▪ Definition of self-care from the nursing perspective
The term self-care and self-management are used interchangeably by scholars from various disciplines. In nursing, the concept of self-care is considered as a process of maintaining health through certain practices that promote health and maintain well-being [46]. Everyone involved in some form of self-care in daily routine such as brushing teeth, food choices etc. but when someone gets sick, disease management become a priority while at the same time, needs for selfcare remain.
The concept of self-care is relatively more significant to people with chronic diseases such as diabetes. Engage in self-care make people active participants in their own care. Self-care is unique to an individual, in which, the number of activities that sound reasonable to one person may not suitable to the other. These justifies for the need of a middle range theory in this field [47]. Middle range theories reflect the views of reality associated with a phenomenon and a limited number of variables. The middle range theory of self-care described by Riegel et al. consists of three key concepts; self-care maintenance, self-care monitoring and self-care management [48].
▪ Self-care maintenance
Self-care maintenance refers to behaviour by an individual to improve well-being, maintain health or to maintain physical and emotional stability. This behaviour is mostly associated with lifestyle modifications, medical regimen, keeping active and handles daily pressures. Self- care maintenance would be benefited to a person from reflecting on their expanding behaviour consistently, fully commitment and evaluatecontinuously to assess the effectiveness. Thereby, adherence behaviour is an essential component in self-care maintenance.
▪ Self-care monitoring
Self-monitoring is common to all people. In diabetes, self-monitoring of blood sugar helps to achieve physical and emotional stability. Three criteria necessary to monitor the effective self-care are clinically significant changes made over time, the presence of reliable tools to detect the change, and finally the response should be measurable. People with chronic illnesses who are competent in self-care monitoring can deliver better information to healthcare professionals through discussion and care recommendations. In other word, self-care monitoring is the relationship between self-care maintenance and self-care management.
▪ Self-care management
Self-care management involves an evaluation of changes in physical and emotional signs and symptoms to determine if action is needed. These changes may be affected by the disease or living environment. An effective person in self-care comprehends the meaning of such changes and capable to make good decision in options for a course of his/her actions. Another important point about self-care management is a self-modification related to the treatment may need to consult the health care provider through therapeutic interactions.
▪ Underlying principles of self-care
Decision making
The basic process that makes self-care practices are complex is the need for effective decisions making. As well noted, self-managing in diabetes involve cognitive decision making in response to the symptoms of a disease. While, the basis for effective decision making on the other hand, requires a person to use an analytical and systematic methods to weight the evidence before making selection for a course of actions in selfcare management [49]. Unfortunately, it is come to realize that patients rarely use such methods, a rational decision making process, and they rarely generate and compare options in systematic fashion. A better description of the process used by patients in self-care is naturalistic decision making. It reflects the automatic, impulsive, contextual decision that people make in complex real-life situations [50].
Reflection
Reflection or contemplation is related to knowledge acquisition and both are essential in self-care. People with poor knowledge and lacking in an in-depth understanding of the rationale for self-care may perform insufficiently [51]. Unfortunately, there are many people performing self-care activities without knowing the reasons behind it. Some of them even dutifully monitor their blood sugar without knowing what to do with that information. Reflection in a structured and targeted education may increase their performance in self-care and for this case; it can be promoted through situation based discussion [52].
Another issue observed among diabetes, is about those who possessed the knowledge and reflective but chosen not to adhere to self-care. This phenomenon often referred to in the literature as reasoned decision making [53], intelligent non-adherence [54], or self-regulation [55]. Little known on the ethical approaches to interact with this group of people and after all, we must respect for their autonomy and freedom to choose. One example of evidence-based approach to handling these challenging situations known as motivational interviewing [56]. The ideal characteristic of a person with diabetes is purposive, reflective, sufficient, and reasoned self-care [57]. They are well informed about the self-care needed for their diabetes condition. They perform self-care with understanding and making sense with the data they gather and make good decision about what to do when the abnormal symptoms arises. To reach a state of reflective, knowledgeable and sufficient in selfcare, a person must be motivated and having received the targeted education from healthcare professionals or have successfully seeking information and contemplating their options.
▪ Support of health professionals team
Support initiative for people living with diabetes and healthcare professional in this country has been largely segregated. No overarching coordination between both patients and healthcare professional; and efforts to recognize the potential mutual reinforcement is still vague. The role of patient-healthcare professional relationships in this sense to provide a critical juncture for exchange of information, and decision making for diabetes in the community [58].
Health professionals can provide support on lifestyle modification and health outcomes through development of skills and confidence [59]. The main goal is to prepare patients to engage with the medical regimen, maintain a role in life and manage negative emotions such as fear and depression [60]. Other sources of information for self-management support is include the use of significant technological advances to facilitate the implementation and delivery of self-management within healthcare setting [61-65]. However, the important issue arises on the respond of people with diabetes in the community in the usage of such technologies.
Meanwhile, the interaction and communication between professional and patients often seen as interaction between an unequal position, and conflicts of expectation in self-care [66]. Certain aspect of this consultation can influence or impede the patient’s behaviour and wellbeing. People with diabetes in the community are in vulnerable state. Ongoing interactions, can help and support them to get back on tract, thus the sharing of information and action now are crucial [67]. Delays and stresses caused by lack of communication, trusts and poor services can result in delayed process of adaptations and engagement of self-care. These extra pressures and risks on the person and family, overtime can lead to non-adherence behaviour to self-care.
Hence, this study explored the process undertaken by people with type-2 diabetes engaging in and adapting self-management behaviour among vulnerable population in the community setting. This is part of a larger study in developing support system strategies to assist for their success in selfmanagement. Views from health professionals and family members also considered.
Material and Methods
▪ Grounded theory
This research study applies the constructivist grounded theory; a modified version of the Strauss and Corbin grounded theory approach through interpretivisms and symbolic interactionism reflecting the basic beliefs of constructionism as a paradigm of inquiry [48]. Through this approach, the theoretical sensitivity is enhanced using literature review as an additional source of data. Followed by data coding, analysis maps, concepts and discourse analysis with categorization and sub-categorization. The aim is to discover the concepts attributed to the relevant generating theory and the understanding of how professionals, people with diabetes and their partner or family members engaged with selfmanagement activities.
▪ Sampling in grounded theory
This research was undertaken in a central region of Malaysia where access was given to a Public Community Health Centre, Diabetes Counselling Unit and the Primary Care Team at one of the tertiary hospitals who care for people with progressive type-2 diabetes on a referral basis. The keypersons from healthcare professionals from public institutions were chosen first to seek their perspective for the relevance of the proposed research. The Diabetes Educator at an outpatient clinic within the community primary care centre and diabetic counselling unit selected people who comes for regular check-up and fulfilled the inclusion criteria to be included in this study for the interview. As for longitudinal observation, purposive sampling was used. Older than 18 years old, Malays and/ or English speaking and diagnosed with type-2 diabetes was considered and informed about the study. Agreed participants gave verbal informed consents before the interview (Table 1).
| Research participant | Employment | Age | Gender | First recognised symptoms | Year of diagnosis | Age at diagnosis |
|---|---|---|---|---|---|---|
| DM1 | Project Consultant | 53years | Male | 2008 | 2010 | 47years |
| DM2 | Admins Executive | 34years | Female | - | 2007 | 24years |
| DM3 | Lecturer | 43years | Female | 1997 | 2003 | 30years |
| DM4 | Laboratory | 53years | Female | - | 2000 | 37years |
| Supervisor | ||||||
| DM5 | Executive | 34years | Male | 2009 | 2010 | 28years |
| DM6 | Retired Teacher | 56years | Male | - | 2006 | 46years |
Table 1. Actual sample of people with Type-2 diabetes participated in longitudinal observation.
▪ Data collection
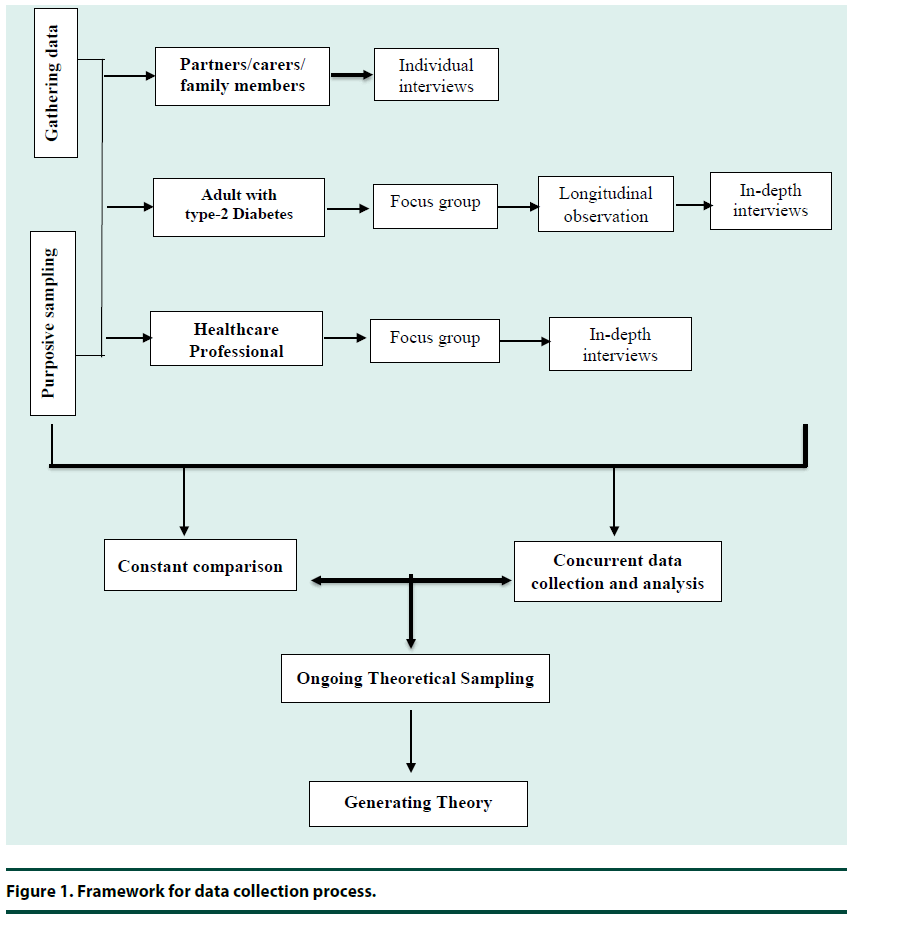
Data collection involved three stages. First stage was with the health professionals to seek perspective of the usefulness of the proposed research to get good grounding in the local service provision for diabetes. Second, conduct interviews with people with diabetes in the community. Then, the researcher spends time with people having type-2 diabetes at workplace and meet on monthly basis over nine to tenmonth period. Data was collected using focus group, semi structured interviews, longitudinal observations, personal and reflective diary (Figure 1). Minimum of two years of diagnosis with type-2 diabetes, and concerning their perceptions of self-management in the context of diabetes service delivery received. Through the data analysis, these methodologies interplayed and complimented each other to support the creation of considerable theory. Constant comparisons began as soon as the first items of data was collected and continued until saturation point was reached.
▪ Ethical consideration
This study has been conducted in accordance to Guidelines of Research Ethic of KPJ Healthcare University College for the entire researcher. Approval obtained is for collection of data in the community. Focus group interviews were conducted as part of the agenda of one Community Health Program which organized in collaboration with the local community leaders. The local leader also helps to invite people with diabetes to attend the health talk and consented for their participation in focus group interviews. Individuals were informed about confidentiality status and voluntarily basis of participation during the briefing prior to the interview. As for participation for longitudinal observation, all participants were invited to join the Diabetes Support Group formed by the researcher that meeting on monthly basis. The participant was informed about the aim and rationale of conducting the study to protect participants interest, trust and to ensure for high ethical standards of this study.
Results
▪ Demographic
Participants demographic are listed in Table 1. There were thirty (30) participants recruited for the interviews. Average age of participants was 55.0 years; range of 40-70 years old with ten males (33.3%) and the rest are female (66.7%) (Table 1).
▪ Themes
There were five (5) themes emerged through inductive analysis and generating selfmanagement issues from study population. Each category will be discussed separately; denial associated behaviour, uncertainty and unpredictability, moral engagement and self efficacy and coping strategies. All themes are tabulated below Tables 2-4.
| Demographic | Men (n=10) | Women (n=20) | Total (n=30) |
|---|---|---|---|
| Marital status (no. of participants) | |||
| Single/never married | 0 | 0 | 0 |
| Married | 5 | 10 | 15 |
| Separated/Divorced | 1 | 2 | 3 |
| Widowed | 4 | 8 | 12 |
| Education (no. of participants) | |||
| Less than primary education | 0 | 3 | 3 |
| Lower secondary school | 0 | 5 | 5 |
| Higher secondary school | 5 | 8 | 13 |
| Completed college or university college | 3 | 3 | 6 |
| Graduate /professional degree | 2 | 1 | 3 |
| Employment (no. of participants) | |||
| Part time/Self-employment | 4 | 5 | 9 |
| Unemployed/fulltime housewife | 0 | 6 | 6 |
| Retired | 3 | 5 | 8 |
| Fulltime working | 3 | 4 | 7 |
| Length of diabetes (no. of participants) | |||
| Less than a year (newly diagnosed) | 2 | 3 | 5 |
| >1year – 3years | 1 | 5 | 6 |
| >3years – 5years | 2 | 4 | 6 |
| >5years – 7years | 1 | 3 | 4 |
| >7years – 10 years | 2 | 2 | 4 |
| > 10 years | 2 | 3 | 5 |
| Type of current treatments (no. of participants) | |||
| Oral hypoglycaemic agent | 7 | 15 | 22 |
| Insulin injection | 0 | 1 | 1 |
| Combination of both (oral & insulin injection) | 3 | 4 | 7 |
Table 2. Demographic characteristic of participants involved in interviews.
| Subthemes | Major themes |
|---|---|
| •Denial and Complacency | Denial Associated Behaviour |
| •Dependency on Medical Personnel | |
| •Confidence on Healthcare Services | |
| •Role Conflicts & Rapport with Healthcare Team | |
| Subthemes | Major themes |
| Uncertainty &Inconsistency Experience | Uncertainty and Unpredictability |
| Unpredictable Outcomes | |
| Subthemes | Major themes |
| •Culture Belief & Moral Engagement towards Self-Care | Engagement andDisengagement |
| •Autonomy and Control Over Support |
Table 3. Major themes of self-management behaviour pattern.
| Variables of the Theory of Planned Behaviour |
Description | Perception of Self-Management Adherence |
|---|---|---|
| Attitudes towards behaviour (Behaviour Belief) | Favourable or unfavourable evaluation of the behaviour | Understanding the concepts of self-care management, personal experience of independence and adaptation process, self-control, quality of life, self-identity and autonomy. Re-establishing a role and the value of lives (Cognitive Domain) |
| Subjective Norm (Normative Beliefs) | Perceived social pressure to perform/ or not performed the behaviour |
Psychosocial expectations of adaptation of functional. Psychological and social changes (Affective Domain) |
| Perceived Behaviour Control (Control Beliefs) | Perceived capability to perform the behaviour | Demonstrating self-coping and self-control through self-confidence
Locus of control (Internal and External) |
Table 4. Theory of planned behaviour of self-management and adherence behaviour.
▪ Denial associated behaviour
Denial can be a way of escapism of behaviour or suppressing the seriousness of something that is affecting oneself, such as a serious disease like diabetes that has no cure or active treatment [68]. Participants in this study have two common defence identified that is denial and disobey or disavowal. Denial was reported by focus group participants as at the early stage of diagnosis which dragged them to more than years till at least five years. As on observation during consultation at physician clinic, denial commonly reflects on patient’s rejection towards the treatment change, from oral tablet to insulin injection. Further interview revealed that they reject the changes of treatment modebecause they think the disease is progressive and getting more critical.
“…It is hard for me to accept it actually...I think there must be a mistake…” (Figure 1)
“. . the doctor said…the drugs just to prevent myself from getting it…” (Figure 2)
“…well…I am perfectly find…that’s why, I don’t see the need for me to take the insulin.” (Observed participant-4)
On the other hand, disavowal means that a person adopts dual thinking as the way they manage themselves and deal with the disease and their prognosis. In this study, people often appear to have a rational discussion with professionals about their future, but at the same time remain with a set of beliefs that appear irrational, as the way to minimize the impact.
They also often make up story that is more lucrative than what happened to them and move between their diagnosis and minimize their own version of events depending on what they are experiencing at the time. Majority of participants in this study has some level of disavowal in terms of questioning about the blood investigation results which confirmed the diagnosis, and claimed there could be mistakenly interpreted.
“I know…I shouldn’t have done that (bad eating habits) but it just cannot be resisted…”
“...I must take snacks while doing work…otherwise I cannot do my work...”
▪ Uncertainty and unpredictability
Dealing with uncertainty and unpredictability related to the disease progress and self-care activities affects most people in this study with various threats and challenges throughout their journey.
“…I used to be like…whenever I feel like eating my favourite desserts…I cooked and served them to my friends…and I just feel satisfied watching them enjoying it…”
“…before I used to depend on my daughter in law so much…but when I think back…she also has her own commitment…”
However, at one point of these uncertainty situations, it has turned some of those participants into opportunities for them to make a change in behaviour as they started to praise for future hopes and the good life.
“. Well…I did that [the change] …because I am tired of getting sick…after all, life has to go on…”
They go through these processes and getting life back into control through coping mechanisms and embrace self-management. A hope in life may be associated with optimisms and positivisms that reflect in behaviour. Participants also recognizes the importance to engage in selfmanagement behaviours can improve their selfcontrol, quality of life and well-being.
▪ Engagement and disengagement
Shame and guilt are uncomfortable emotions and that make people use various strategies to prevent these feelings. For some, the sense of shame and guilt for poor behavior can lead to the development of positive character, warmth mature, generativity and integrity [69]. This scenario is observed as ‘a hidden phenomenon’ in an environment for people with diabetes in this study. It affects them directly and indirectly with the development and use of moral disengagement for just to ensure that their adherence behaviour will be ‘seen’ by others. In particular is to fulfil their healthcare professional’s expectation, thus they doing those in the act of self-protecting from sarcastic comments on their failure.
“…the only time I worked very hard is before going to see my doctor…like one week before, I started dieting strictly…desperately…to bring down my sugar level…well..maybe it sound ‘cheating’…but I have no choice…”
Moral disengagement was not identified as a focus within middle range concepts during the review of literature in this study raising the question about the impact of moral disengagement on long term adherence and behaviour change. Although moral disengagement has been identified as a significant barrier to behaviour change it was not being appropriately addressed in research.
▪ Patients autonomy
Autonomy can be translated into a group of related terms; individual liberty, privacy, freedom of choice, self-governance, self-regulation and moral independence [70]. Personal autonomy as the personal rule of the self, including decision making and other activities by the individual, that is free from both external interference and personal limitations [71]. Participants in this study frequently expressed their feelings about having constraints in life on making decision for them and showed concerns about their values and culture.
“…yes, diabetes disturbed me especially diet… because taking sugar don’t really matter with me… but most important is the rice…for me living without rice…will make my body very weak…Figure 2-P8
“…I think…the most and foremost, they need to explain clearly what we should do, how can we manage better rather than nagging at us like a ‘policeman’…Figure 2-P4
“….and flexibility…. always motivate us…like say to me ‘It’s ok, once a while you can eat that favorite food but just in small amount...” (Figure 2)
“…well, I was humiliated in front of everybody in the room for doing it incorrectly…” (P4-Intv)
Health professional must respect patient’s autonomy, by at least acknowledging their right to hold views, make choices, and to take actions based on personal values and beliefs. Information and involvement of health professional is at the heart of patient-centred approach.
▪ Dependency and role conflicts of health professionals
In the participants’ eyes, health professionals are deemed looked as an expert who is knowledgeable, well trained and have the power to cure, caring, able to relieve their pain and discomfort. Through this power and by the virtue of their knowledge based and expertise, health professionals are given a trust, authority and control of their patients. In this sense, when they are unwell and having problem with selfcare and health; they want help and support of health professionals to get them back on tract, thereby their sharing of information and action to them is crucial.
“…it is not fare asking us to do all those pricking …. especially at home…I am just a housewife…… anything happens, we suffer ourselves….” (FG2-P2)
However, most of the time, their attempts to get further explanation about the disease was confronted with the indifferent attitude of health professionals and thus, make them feeling disappointed and decided to keeping it for themselves.
“…. I did try to talk to the doctor…but somehow, I see them not really pay attention…and I taught … yeah…maybe they are busy…(FG2-P2)
“…normally, they just talk about our blood result… and that’s all…(FG2-P6)
“….at times, they did ask me what I eat and whether I do my exercise…in a very short conversation…” (FG2-P4)
“…I dare not to ask questions…because I see them busy writing…and sometimes talking over the phone…seriously…” (FG2-P3)
These delays and unnecessary stresses of people with type-2 diabetes can result in delayed process of adaptations and engagement of self-care due to the extra pressures and risks on the person and family.
▪ Self-efficacy and coping strategies
Self-esteem is a concept of personality which describes the extent to which we value ourselves. We need to have self-worth to promote that and it will be sought by embracing the challenges for success. Participants in this study showed some elevation in level of anxiety, depressions and other emotional reactions towards their unsuccessful efforts of self-care which altered their self-esteem and self-confidence.
“…I personally don’t like depending on people so much, that’s why now I really feel that I have made my life inconvenience to my son’s family especially my daughter in-law because she has to do extra work, besides cooking for the entire big family… now she has to prepare a different dish for me…” (FG2-P2)
Often participants feel a failure or a burden to others if they are no longer able to achieve what they once could, can demoralising to them.
“…but the problem is...after had all these constraints …my blood sugar still no change…I just couldn’t think of the reasons for that …. Something wrong somewhere…(FG2-P8)
In addition, the adjustment to self-care can also be influenced by other variables such as aspects of the individual personality, the availability of various types of support and their understanding and appraisal of their experience. However, participants in this study also found that the past life performance was to be the most significant overall predictor for either success or otherwise.
“…I wish to have someone for ‘being there’ for me when I have problem…like recently I was not feeling well…very weak and no appetite…. and I was just having a fear to decide anything …not even to take my insulin because once I had that before…and I was just ended up to be in the hospital…” (FG2-P4)
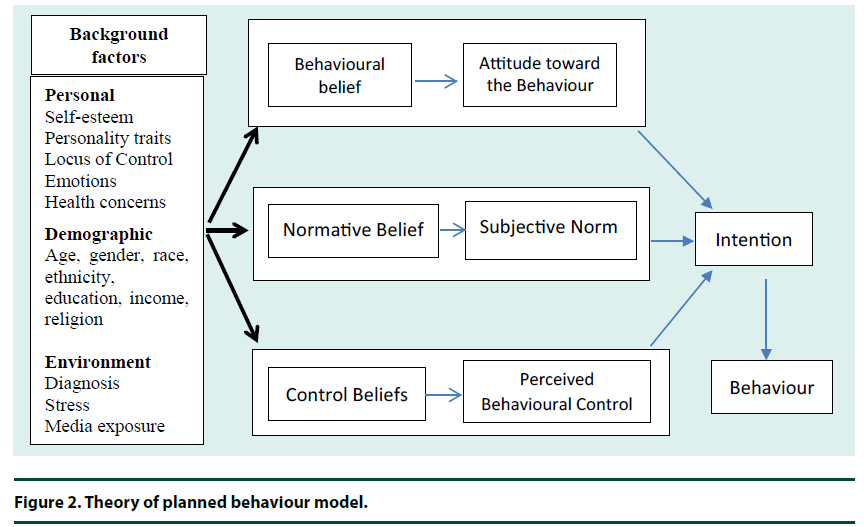
Identification and taking effort in developing self-strategies to cope and self- control are differed in levels and complexity in all participants in this study. However, most of them claimed to have an increasing in knowledge overtime and keeping updated with information about disease and care from various resources. According to Theory of Planned Behaviour by Ajzen, human action is influenced by three major variables of behavioural beliefs, normative beliefs and control beliefs (Figure 2). The application and relevance of this model to engage with selfmanagement and self- efficacy through planned behaviour has been set out in Table 2 under the variables of theory planned behaviour model.
Discussion
This study provides a base of knowledge and understanding for the concept of self -managements among people living with type- 2 diabetes, the meaning and interpretation of those within their psychosocial context. This exploratory research has shown that living with diabetes is an ongoing process and the meaning of those experiences may change alongside with the progress of the illness within the unpredictable daily life circumstances.
▪ The needs of patient’s empowerment as ‘self-manager’
It has been widely accepted that patient’s empowerment must begin with the patient acquiring information and therefore should be viewed as an outcome of the educational process. However, the level of empowerment among individual often affected by the environmental factors such as emotional status, spiritual, social efficacy, and cognitive living with the diabetes itself [72-75]. Many traditional diabetes selfmanagement education (DSME) has been overlooked of all these aspects in their curriculum. Finding of this research informs a future study which attempts to incorporate social support to help individuals develop the skills and selfawareness in the management of stress, coping, social support, goal setting, problem solving and motivation. Similarly, individuals with diabetes are also being educated on how to use the health care system and other community resources that can help them with their diabetes management.
To be a successful ‘self-manager’, a person with diabetes not only require coping strategy but also a personal skill such as self-leadership and good communication which consist of specific behavioural and cognitive strategies designed to positively influence personal effectiveness [76]. The concept of self-leadership is derived primarily from research and theory in two areas of psychology. The first, Social Cognitive Theory (SCT), views the adoption and change of human behaviour as a complex process with many parts. It recognizes that we influenced by the world in which we live [77]. SCT places importance on the capacity of a person to manage or control him/herself particularly when faced with difficult yet important tasks. This viewpoint serves as the primary basis for researcher to understand the interaction of people with diabetes and their psychosocial environmental SCT also recognizes the human ability to learn and experience tasks and events through vicarious and symbolic mechanisms–that is by observing others and by using imagination. Finally, SCT stresses the importance of our perceptions of our own effectiveness or potential to be effective.
▪ Partnership, support and networking with healthcare professionals
Majority of participants expressed concerns about their doubt on information and knowledge they received from healthcare professionals which they described as too technical for them to understand. Working with professionals usually seen as a partnership and reciprocity of information, knowledge and shared decision-making [78]. As a matter fact, healthcare professionals can also be a social network where people involved will feels the bonding as they part of the process. While at the same time, it should be careful to ensure that it do not become hierarchical, where there might make people involve with diabetes feelings vulnerable at times, then it became too difficult to be truly engage with too many people [79].
In respect to the professional power, it was expressed for the reasons of them not to asking further during their diabetic visits because they afraid to interrupt professionals work and fear of misunderstanding in their intentions. Despite those, they also raised concerns about differences in expectation of care consultations which causing some conflicts sometime. Therefore, they decided to seek help from others such as friends, family members or neighbours. These might be placing them at risks for decisions or suggestion that might be taken based on inadequate information and that the value of support from others again justified. While having said that, people with diabetes again were challenged in facing with challenges such as partners being ignored and taken a back seat, not knowing them or their condition. The development of personalised plan for people with diabetes will allow them interacting more meaningfully with health professionals and partner/family members to set out goals and targets which are related to coping with self-management tasks at home on daily basis [80-83]. This could set out their independence, self-management and coping strategies.
It is observed that most of the emphasis on self-management support strategies in this country was developed based on professionals personalised care plan, care pathways, and professional care records which were written by professionals and very limited are shared with the patients. The researcher proposes that real consideration should be given to a personal plan with support a development by professional to enhance the self-management and self-efficacy of people with type-2 diabetes. This plan would also be useful to families in setting out the boundaries and support that they can provide to the person with diabetes.
Conclusion
Finding of this study sought to contribute to the knowledge of based and understanding of the concepts of self-management behaviour in terms of reality, meaning and interpretation of people with type-2 diabetes in the progressive of their illness, the complexity of the self-management tasks and having those to living in the challenges psychosocial environment on day-to-day basis.
This research has demonstrated that living with diabetes is an ongoing process and that means, the experience of people might change alongside with the changes of their illness as it progresses and so as the circumstances that they are facing with throughout their life. The uncertainty of living with diabetes confront people with numerous treats and challenges in life. However, finding of this study revealed that people will reach ‘a turning point’ where they make a transformation of that uncertainty event into some opportunities of getting life back ‘on tracts’ through coping mechanisms and embraced self-management tasks. Healthcare professionals should be made aware of this important ‘turning point’ which can be taken the opportunity for them to use their medical power to influence people with diabetes to engage in self-management behaviour to improve their health and wellbeing.
Support strategy should be taking consideration on the potential personal barriers to selfmanagement such as lack of information resources, internet access, and social isolation, physical, cognitive and emotional barriers. Giving people time during consultation to discuss their coping, allow them to ask questions, provide feedback with respects; and focusing on health behaviour to set the target goal and plan for strategies to achieve those.
References
- Arsand E, Tatara N, Ostengen G, Hartvigsen G. Mobile-Phone-based Self-Management Tools for Type 2 Diabetes: The Few Touch Application.J. Diabetes. Sci. Technol. 4(2), 328–336 (2010).
- Adwan MA, Najjar YW. The relationship between demographic variables and diabetes self-management in diabetic patients in Amman city/Jordan. Glob. J. Health. Sci. 5(2), 213–220 (2013).
- Baker MK, Simpson K, Lloyd B, Bauman AE, Singh MAF. Behavioral strategies in diabetes prevention programs: A systematic review of randomized controlled trials. Diabetes. Res. and Clin. Practice. 91(1), 1–12(2011).
- Bandura A.Social cognitive theory of self-regulation.Organ. Behav. Hum. Decis. Process.50(2), 248-287 (1991).
- Bandura A. Social cognitive theory.Annals of Child Development. 6, 1–60(1989).
- Bandura A. Moral Disengagement in the Perpetration of Inhumanities. Pers Soc Psychol Rev. 3(3), 193–209(1999).
- Bandura A. Social Cognitive Theory. Saf. Sci. 6(C), 1–60(2009).
- Barik A, Mazumdar S, Chowdhury A, Rai RK. Physiological and behavioral risk factors of type 2 diabetes mellitus in rural India.BMJ. Open. Diab. Res. Care. 4(1), e000255(2016).
- Bayliss EA, Ellis JL, Steiner JF. Barriers to self-management and quality-of-life outcomes in seniors with multimorbidities. Ann. Fam. Med.5(5),395–402 (2007).
- Beebe CA, Schmitt S. Engaging patients in education for self-management in an accountable care environment. Clin.Diabetes. 29(3), 123–126(2011).
- Bertoldi AD, Kanavos P, França GVA etal. Epidemiology, management, complications and costs associated with type 2 diabetes in Brazil: a comprehensive literature review. Globalization and Health. 9, 62(2013).
- Bird D, Oldenburg B, Cassimatis M et al. Randomised controlled trial of an automated, interactive telephone intervention to improve type 2 diabetes self-management (Telephone-Linked Care Diabetes Project): study protocol. BMC. Pub. Health. 10(1), 599(2010).
- British Columbia Ministry of Health. Self-Management Support : A Health Care Intervention. (2011).
- Brown MT, Bussell JK. Medication Adherence: WHO Cares? Mayo. Clin Proc. 86(4), 304–314(2011).
- Browning C, Chapman A, Cowlishaw S et al. The Happy Life ClubTM study protocol: a cluster randomised controlled trial of a type 2 diabetes health coach intervention. BMC. Public Health. 11(1), 90(2011).
- Bunch MJ, MorrisonKE, Parkes MW, Venema HD.Promoting Health and Well-Being by Managing for Social – Ecological Resilience : the Potential of Integrating Ecohealth and Water Resources. Ecology and Society. 16(1), 18(2011).
- Cameron F. Standards of Medical Care in Diabetes-2016. Aust. Fam. Physician. 35(6), 386–390(2006).
- Carcone AI. A social ecological perspective on diabetes care: Supporting adolescents and caregivers. Dissertation Abstracts International Section A: Humanities and Social Sciences. 71(7–A), 2647(2011).
- Chas T, Sarah E. (2001) Personal Personal Models of Diabetes in Relation to Self-Care, Well-Being, and Glycemic Control.Diabetes Care.24(5), 828-833(2001).
- Chesla CA, Chun KM, Kwan CML.Cultural and family challenges to managing type 2diabetes in immigrant Chinese Americans. Diabetes Care. 32(10), 1812–1816(2009).
- Collinsworth AW, Vulimiri M, Schmidt KL, Snead Ca. Effectiveness of a community health worker-led diabetes self-management education program and implications for CHW involvement in care coordination strategies. Diabetes Educ. 39(6), 792–9(2013).
- Dhada B, Blackbeard D. Using Intervention Mapping to Develop a Child Diabetes Support Intervention. Procedia-Social and Behavioral Sciences. 113(0), 74–83(2014).
- El-Gayar FO, Timsina P, Eid W. MobileApplicationsforDiabetesSelf-Management: StatusandPotential. J. Diabetes Sci. Technol. 7(1), 247–262(2013).
- Fitzpatrick S L, Schumann KP, Hill-Briggs F.Problem solving interventions for diabetes self-management and control: A systematic review of the literature. Diabetes Res. Clin. Pract. 100(2), 145–161(2013).
- Forjuoh SN, Bolin JN, Jr, JCH et al. Behavioral and technological interventions targeting glycemic control in a racially/ethnically diverse population : a randomized controlled trial.BMC. Public Health.14, 71 (2014).
- Funnell MM, Anderson RM. Empowerment and Self-Management of Diabetes. Clin. Diabetes. 22(3), 123–127(2004).
- Funnell MM, Brown TL, Childs BP et al. National standards for diabetes self-management education. Diabetes Care. 34(2011).
- Gao J, Wang J, Zheng P et al. Effects of self-care, self-efficacy, social support on glycemic control in adults with type 2 diabetes. BMC. Fam. Pract. 14(1), 1090–1101(2013).
- Gonzalez JS, Safren SA, Cagliero E et al. Depression, self-care, and medication adherence in type 2 diabetes: Relationships across the full range of symptom severity. Diabetes Care. 30(9), 2222–2227(2007).
- Gucciardi E, Wang SCT, DeMelo M, Amaral L, Stewart DE.Characteristics of men and women with diabetes: Observations during patients’ initial visit to a diabetes education centre. Can. Fam. Physician. 54(2), 219–227(2008).
- Hartayu T, Izham MI M, Suryawati S. Improving of Type 2 Diabetic Patients’ Knowledge, Attitude and Practice towards Diabetes Self-care by Implementing Community-Based Interactive Approach-Diabetes Mellitus Strategy. BMC. Res. Notes. 5(1), 315(2012).
- Holman H, Lorig K.Patient self-management: a key to effectiveness and efficiency in care of chronic disease. Public Health Rep. 119(3), 239–243(2004).
- Jamsiah M, RS, NHI. Journal of Community Health 2010: Vol 16 Number 1 ORIGINAL ARTICLE. Journal of Community Health, 16(1), 60–68(2010). (http://journalarticle.ukm.my/270/1/1.pdf)
- Kaur G, Tee GH, Ariaratnam S, Krishnapillai AS,China K.Depression, anxiety and stress symptoms among diabetics in Malaysia: a cross sectional study in an urban primary care setting. BMC. Fami. Pract. 14(1), 69(2013).
- Khan AR, Al-Abdul Lateef ZN, Al Aithan MAet al.Factors contributing to non compliance among diabetics attending primary health centers in the Al Hasa district of Saudi Arabia.J. Fam. Comm. Med.19(1), 26–32(2012).
- Klein G. A naturalistic decision making perspective on studying intuitive decision making. J. Appl. Res. Mem. Cogn. 4(3), 164–168(2015).
- Lee HS. A Study on the Public-Private Partnership to Global Health Issues in Korea. Osong. Public Health Res. Perspect. 4(6), 308–315(2013).
- Lindenmeyer A, Whitlock S, Sturt J, Griffiths F. Patient engagement with a diabetes self-management intervention.Chronic. Illn. 6(4), 306-316(2010).
- Lipshitz R, Klein G, Orasanu J,Salas E. Taking stock of naturalistic decision making.J. Behav. Decis. Mak. 14(5), 331–352(2001).
- Liu S, BiA, FuD et al. Effectiveness of using group visit model to support diabetes patient self-management in rural communities of Shanghai: a randomized controlled trial.BMC. Public Health. 12, 1043(2012).
- Lo TO.Adherence to long-term therapies World Health Organization (2003).
- Lohman MC. A Survey of Factors Influencing the Engagement of Information Technology Professionals in Informal Learning Activities.ITLPJ. 25(1), 43–53(2007).
- Luo X, Liu T, Yuan Xet al. Factors influencing self-management in Chinese adults with type 2 diabetes: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health. 12(9), 11304–11327(2015).
- Madeleine A, John C, Michael R., Rebecca CJ, Kamila H. Culturally appropriate health education for people in ethnic minority groups with type 2 diabetes mellitus.Cochrane. Database Syst. Rev.(9) (2014).
- Markland D, Ryan RM, Tobin VJ, Rollnick S. Motivational Interviewing and Self–Determination Theory. J. Soc. Clin. Psychol. 24(6), 811–831. (2005).
- Mathew R, Gucciardi E, De Melo M, Barata P. Self-management experiences among men and women with type 2 diabetes mellitus: a qualitative analysis. BMC. Family Practice. 13(1), 122(2012).
- Mayberry LS, Osborn CY. Family support, medication adherence, and glycemic control among adults with type 2 diabetes. Diabetes Care. 35(6), 1239–1245(2012).
- Misono AS, Cutrona SL, Choudhry NK et al. Healthcare information technology interventions to improve cardiovascular and diabetes medication adherence. Am. J. Manag. Care. 6(12 Spec No.), SP82-P92 (2010).
- Nijland N, Van Gemert-Pijnen JEWC, Kelders SM, Brandenburg BJ, Seydel ER. Factors influencing the use of a web-based application for supporting the self-care of patients with type 2 diabetes: A longitudinal study. J. Med. Internet. Res. 13(3) (2011).
- Osherson D, Hall G. Theories of Reasoning and Decision-Making, 1–5(2008).
- Pal K, Eastwood SV, Michie S et al. Computer‐based diabetes self‐management interventions for adults with type 2 diabetes mellitus (Review). The Cochrane Library. 3. (2013).
- Pangan IK, Pangilinan M, Pangilinan R et al. Telenursing through SMS (short messaging service): it’s effect on knowledge and adherence. Int. J. Public Health. ResearchSpecial Issue, 115–120(2011).
- Parkin CG, Hinnen DA, Tetrick DL.Effective use of structured self-management of Blood glucose in type 2 diabetes: Lessons from the STeP study. Clin. Diabetes. 29(4), 131–138(2011).
- Patient Personal Self-Management Plan (2015).
- Pearson M, Mattke S, Shaw R.,Ridgely S. Patient self-management support programs: an evaluation. Agency for Healthcare Research and Quality (8) (Contract No. 282-00-0005) (2007).
- Pennel CL, McLeroy KR, Burdine JN, Matarrita-Cascante D, Wang J.Community Health Needs Assessment: Potential for Population Health Improvement. Popul. Health Manag.19(3), 178-186 (2016).
- Perdue D. (2011). Effect of diabetes management program on glycemic control and quality of life in adults. (May)(2011).
- Pimouguet C, Le Goff M, Thiébaut R, Dartigues JF, Helmer C. Effectiveness of disease-management programs for improving diabetes care: A meta-analysis. Cmaj. 183(2), E115-E127 (2011).
- Press D. Self-care management strategies among individuals living with type 2 diabetes mellitus : nursing interventions.Nurs. (Auckl). 3,99–105(2013).
- Rampal L, Loong YY, Azhar MZ, Sanjay R. Enhancing diabetic care in the community in Malaysia: Need for a paradigm shift.Malays.Jour. of Med. and Health Sciences. 6(1), 3-9 (2010).
- Ratanawongsa N, Bhandari VK, Handley M et al.Primary care provider perceptions of the effectiveness of two self-management support programs for vulnerable patients with diabetes. J. Diabetes Sci. Technol.6(1):116-124 (2012)
- Realf K, Dallosso H.Effectiveness of a diabetes education and self management programme (DESMOND) for people with newly diagnosed type 2 diabetes mellitus : three year follow-up of a cluster randomised controlled trial in primary care. BMJ. 344:e2333, 1–12(2012).
- Ridgely MS (n.d.). Patient Self-Management Support Programs: An Evaluation. 8 (2014).
- Simmons D. Personal Barriers to Diabetes Care: Is It Me, Them, or Us?Preface. Diabetes Spectr. 14(1), 10–12(2001).
- Singh H, Cinnirella M, Bradley C. Support systems for and barriers to diabetes management in South Asians and Whites in the UK : qualitative study of patients ’ perspectives.BMJ. Open.2(6), e001459(2012).
- Smith M, Liehr P. Disciplinary Perspectives Linked to Middle Range Theory. Mid. Range Theory for Nursing. 1–11(2013).
- Sonsona JB. Factors Influencing Diabetes Self-Management of Filipino Americans with Type 2 Diabetes Mellitus : A Holistic Approach. Walden University.(2014).
- Inzucchi SE, Bergenstal RM, Buse JB et al.Management of hyperglycaemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD).Diabetologia.55(6), 1577–1596(2012).
- Tabatabaei-Malazy O, Peimani M, Heshmat R, Pajouhi M. Status of diabetes care in elderly diabetic patients of a developing country. ijdld. 10, 1-8(2011).
- ÖztürkA, Tarsuslu S, Yümin ET, Sertel M, Yümin M. The relationship between physical, functional capacity and quality of life (QoL) among elderly people with a chronic disease.Arch. Gerontol. Geriatr.53(3), 278–283(2011).
- Taylor M. The nurse-patient relationship. Senior Nurse. 13(5), 14–18(1993).
- Therapies P, Group W. Psychosocial Therapies in Diabetes Report of the Psychosocial Therapies Working Group (2001).
- Tomlin A, Sinclair A. The influence of cognition on self-management of type 2 diabetes in older people. Psychol. Res. Behav. Manag. 9, 7–20(2016).
- Tripp-reimer T, Choi E, Kelley S, Janet C. Cultural Barriers to Care: Inverting the Problem.Diabetes Spectr.14(1), 13–22(2010).
- Van Houtum L, Rijken M, Heijmans M, Groenewegen P. Self-management support needs of patients with chronic illness: Do needs for support differ according to the course of illness? Patient Educ. Couns. 93(3), 626–632(2013).
- van Olmen J, Ku GM, van Pelt M et al. The effectiveness of text messages support for diabetes self-management: protocol of the TEXT4DSM study in the democratic Republic of Congo, Cambodia and the Philippines. BMC. Public Health. 13(1), 423(2013).
- Vest BM, Kahn LS, Danzo A et al.Diabetes self-management in a low-income population: impacts of social support and relationships with the health care system. Chronic. Illn. 9(2), 145–155(2013).
- Visram S, Clarke C, White M. Making and maintaining lifestyle changes with the support of a lay health advisor: Longitudinal qualitative study of health trainer services in northern England. PLoS. ONE. 9(5), (2014).
- Von KorffM, Katon WJ, Lin EHB et al. Functional outcomes of multi-condition collaborative care and successful ageing: results of randomised trial. Bmj. 343, d6612–d6612 (2011).
- Weeks CE. Factors Influencing Self-Care Behaviour of African American Adults with Type 2 Diabetes.University of North Carolina. 1–44(2011).
- Williams GC, Freedman ZR, Deci EL.Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care. 21(10), 1644–1651(1998).
- Williams L.Overcome Barriers To Self-Care. 37(3), 32–38(2012).
- Williams S. Personality and self-leadership. Human Resource Management Review. (1997).