Review Article - Imaging in Medicine (2015) Volume 7, Issue 1
Stenting post-operative abdominal bleeding: the interventional radiologists point of view
Jean-pierre Tasu*Department of Imaging, University Hospital of Poitiers, Poitiers, France
- Corresponding Author:
- Jean-pierre Tasu
Department of Imaging
University Hospital of Poitiers
Poitiers, France
Tel: +33 05 49 44 44 44
E-mail: j.p.tasu@chu-poitiers.fr
Abstract
Post-operative bleeding following abdominal surgery remains rare. Although bleeding is usually controlled by symptomatic treatments, surgery or interventional radiology is sometimes necessary. This article reviews the main clinical features that must be recognized and focuses on the role of the radiologist in the management of this complication. This article is largely inspired by an extensive review already published in Diagn Interv Imaging 2015.
Keywords
Post-operative, surgery, CT, diagnosis, hemorrhage, embolization
What we have to know?
Digestive ulcer especially during a stay in intensive care (stress ulcer), rupture from direct arterial or venous trauma and delayed rupture from a previously existing pseudoaneurysm are the major causes of postoperative bleedings. Posthepatectomy hemorrhage has been classified by the International Study Group of Liver Surgery [1,2]. After hepatic transplantation, bleeding is a rare complication (9% of transplantations); most common causes are bleeding from a phrenic, an epigastric or an intercostal artery. In these 2 situations, the first-line treatment option should be endovascular but surgical treatment remains indicated for venous bleeding [3]. Post pancreatectomy hemorrhage has been classified by the International Study group of pancreatic surgery [4]. After pancreatic surgery, bleeding rate (from digestive anastomoses or damaged vascular structures) is estimated between 3.3% and 10%, all types of pancreatic surgery combined [5]. In 79% of cases, the onset is late, more than 24 hours after surgery; at mean 12 days after surgery. In 69% of cases, bleeding is due to intraluminal hemorrhage of digestive anastomoses [6]. The overall rate of postoperative hemorrhage following gastrointestinal surgery for cancer is approximately 0.9%, with a mortality of approximately 20% [7]. For patients following esophageal surgery, bleeding is the cause of postoperative mortality in 9%. The rate of hemorrhagic complications following gastrectomy is 0.9% [7], with a mortality rate of 20%. Ileocolic anastomoses are associated with hemorrhagic complications in 5 to 19% of cases, depending on the surgical technique. Only 1.4% is severe [8]. During colon surgery, perioperative bleeding is the cause of 9% of coelioscopic conversions to open surgery [9]. However the risk of bleeding is not greater with coelioscopy than with laparotomy [10]. In case of rectal surgery, the risk of bleeding is mainly perioperative (3% of presacral bleeding) [11]. Nephrectomy, especially partial nephrectomy, is associated with a higher rate (4.7%) of postoperative hemorrhage [3] (TABLE 1 and 2).
Role of diagnostic radiology
■Standard examination: computed tomography
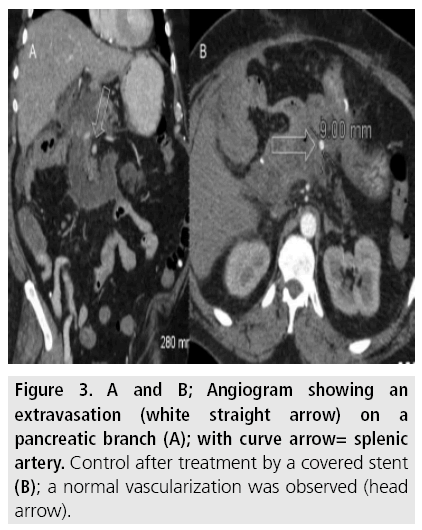
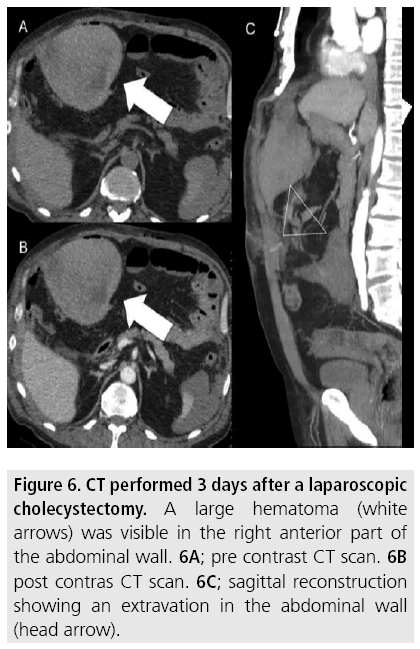
A diagnosis of bleeding should be suggested by shock or a decrease in haemoglobin and/or the presence of blood in the drain [12]. Multidetector computed tomography (MDCT) should be the first-line imaging test [13]. This examination should be performed with a non-enhanced sequence followed by a contrast enhanced arterial phase, a portal phase and sometimes by a delayed phase sequence. There are 4 basic lesions on MDCT [14]; A hemoperitoneum and a hemoretroperitoneum are characterized by the visualization of a spontaneously high-attenuation mass or effusion (more than 40 HU). A hematoma is seen as spontaneously high-attenuation round or oval shaped collection of blood. The sentinel clot sign describes the fact that clotted blood can be found close to the area of active bleeding. This sign is not always seen (FIGURE 3); for these 3 lesions, contrast material injection can mask the spontaneous high-attenuation and a pre contrast acquisition is needed to increase diagnosis performance. The Extravasation of contrast material, also called blush, is a sign of active bleeding. It can be detected on arterial phase images and is a sign of arterial extravasation, or on portal phase images, suggesting venous extravasation. Active bleeding of more than 1 cm in diameter or peritoneal extension, are signs of severe bleeding suggesting extensive extravasation.
The role of interventional radiologist
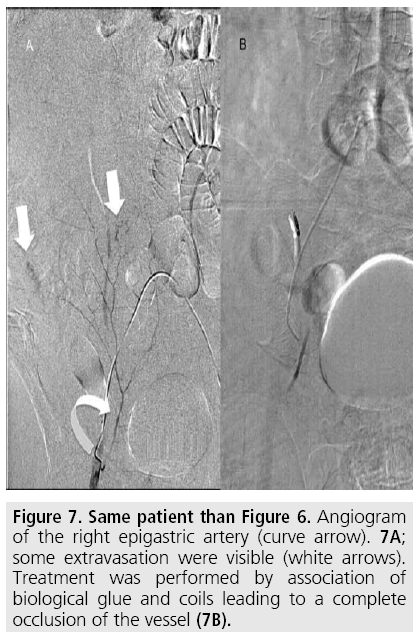
Technical Interventional radiology should be the first-line technique for the management of postoperative bleeding complications [15]. Indeed, additional surgery in the early postoperative period is associated with significant mortality, especially following hepatectomy or pancreatectomy [16]; in cases of hepatectomy, a second surgical intervention is associated to a mortality of approximately 9% within 6 hours after bleeding begins and 25% 6 hours of more after bleeding begins [17]. There are no large series in the literature; thus, there is no practical guideline on the choice of embolization material and techniques are based on the usual practices of the medical center and the operator’s experience. We can only provide some recommendations to avoid complications or unsuccessful procedures: A greater rate of necrosis (approximately 9%) is observed with glue, particularly pure, and small embolization particles. Thus this kind of material must be used with caution in case of distal or terminal vascularization. For non-terminal arteries, a sandwich technique (occlusion of the artery upstream and downstream of the extravasation) must be performed [18]. Embolization of the gastroduodenal artery has been shown to reduce the risk of re-bleeding in case of gastrointestinal bleeding that is not visible on arteriography (but has been confirmed by MDCT, endoscopy or based on clinical signs) [19]. The FIGURES 1 to 7 illustrate some cases including different clinical situations and different techniques of embolization.
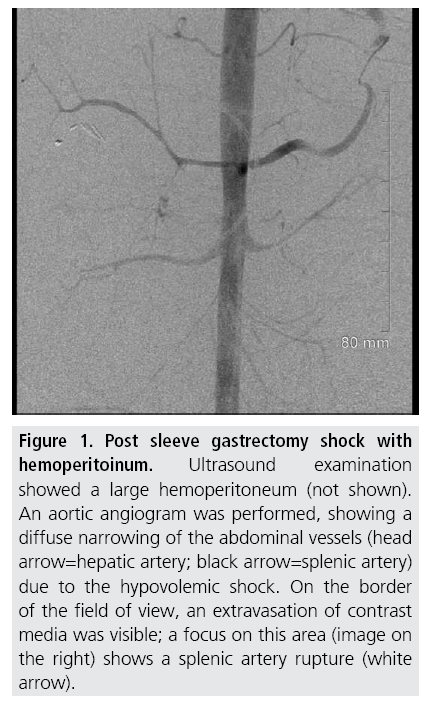
Figure 1: Post sleeve gastrectomy shock with hemoperitoinum. Ultrasound examination showed a large hemoperitoneum (not shown). An aortic angiogram was performed, showing a diffuse narrowing of the abdominal vessels (head arrow=hepatic artery; black arrow=splenic artery) due to the hypovolemic shock. On the border of the field of view, an extravasation of contrast media was visible; a focus on this area (image on the right) shows a splenic artery rupture (white arrow).
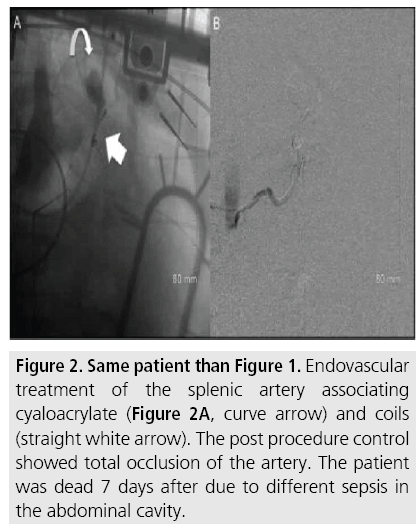
Figure 2: Same patient than Figure 1. Endovascular treatment of the splenic artery associating cyaloacrylate (Figure 2A, curve arrow) and coils (straight white arrow). The post procedure control showed total occlusion of the artery. The patient was dead 7 days after due to different sepsis in the abdominal cavity.
Figure 3: A and B; Angiogram showing an extravasation (white straight arrow) on a pancreatic branch (A); with curve arrow= splenic artery. Control after treatment by a covered stent (B); a normal vascularization was observed (head arrow).
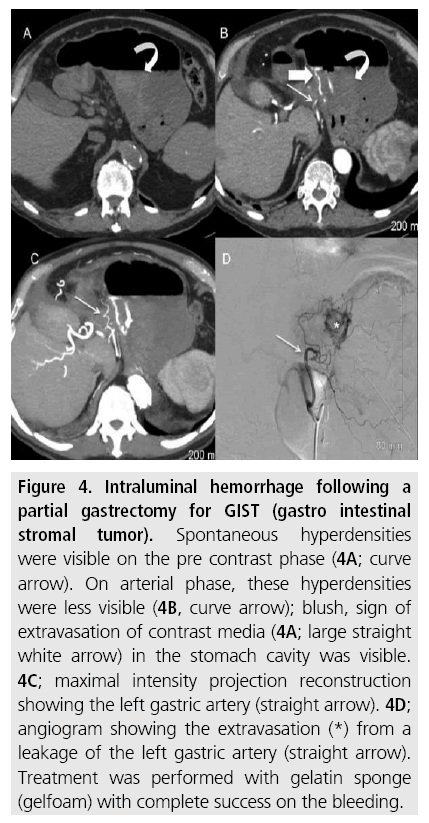
Figure 4: Intraluminal hemorrhage following a partial gastrectomy for GIST (gastro intestinal stromal tumor). Spontaneous hyperdensities were visible on the pre contrast phase (4A; curve arrow). On arterial phase, these hyperdensities were less visible (4B, curve arrow); blush, sign of extravasation of contrast media (4A; large straight white arrow) in the stomach cavity was visible. 4C; maximal intensity projection reconstruction showing the left gastric artery (straight arrow). 4D; angiogram showing the extravasation (*) from a leakage of the left gastric artery (straight arrow). Treatment was performed with gelatin sponge (gelfoam) with complete success on the bleeding.
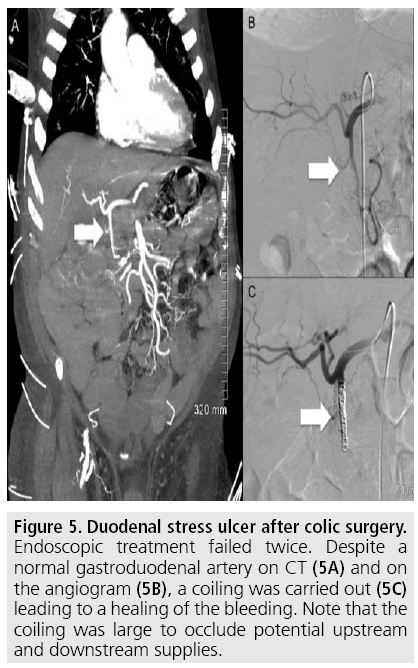
Figure 5: Duodenal stress ulcer after colic surgery. Endoscopic treatment failed twice. Despite a normal gastroduodenal artery on CT (5A) and on the angiogram (5B), a coiling was carried out (5C) leading to a healing of the bleeding. Note that the coiling was large to occlude potential upstream and downstream supplies.
Conclusion
Postoperative abdominal hemorrhage is a rare but potentially severe complication with a high mortality. MDCT must be performed in all cases to determine the location of bleeding. Interventional endovascular radiology should be proposed as the first-line treatment because it is associated with low mortality and morbidity compared to surgery.
References
- Tasu JP, Vesselle G, Herpe G et al. Postoperative abdominal bleeding. Diagn. Interv. Imaging. 96, 823-831 (2015).
- Rahbari NN, Garden OJ, Padbury R et al. Post-hepatectomy haemorrhage: a definition and grading by the International Study Group of Liver Surgery (ISGLS). 13, 528-535 (2011).
- Jung SW, Hwang S, Namgoong JM et al. Incidence and management of postoperative abdominal bleeding after liver transplantation. Transplant. Proc. 44, 765-768 (2012).
- Wente MN, Veit JA, Bassi C et al. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 142, 20- 25 (2007).
- Lefkowitz RJ. Identification of adenylate cyclase-coupled beta-adrenergic receptors with radiolabeled beta-adrenergic antagonists. Biochem. Pharmacol. 24, 1651-1658 (1975).
- Correa-Gallego C, Brennan MF, D’Angelica MI et al. Contemporary experience with postpancreatectomy hemorrhage: Results of 1,122 patients resected between 2006 and 2011. J. Am. Coll. Surg. 215, 616-621 (2012).
- Lermite E, Sommacale D, Piardi T et al. Complications after pancreatic resection: diagnosis, prevention and management. Clin. Res. Hepatol. Gastroenterol. 37, 230-239 (2013).
- Song W, Yuan Y, Peng J et al. The delayed massive hemorrhage after gastrectomy in patients with gastric cancer: characteristics, management opinions and risk factors. Eur. J. Surg. Oncol. 40, 1299-1306 (2014).
- Golda T, Zerpa C, Kreisler E et al. Incidence and management of anastomotic bleeding after ileocolic anastomosis. Colorectal. Dis. 15, 1301- 1308 (2013).
- Parnaby CN, Ramsay G, Macleod CS et al. Complications after laparoscopic and open subtotal colectomy for inflammatory colitis: a case-matched comparison. Colorectal. Dis. 15, 1399-1405 (2013).
- Nakamura A, Osonoi T, Terauchi Y. Relationship between urinary sodium excretion and pioglitazone-induced edema. J. Diabetes. Investig. 1, 208-211 (2010).
- Stein JM. The effect of adrenaline and of alphaand beta-adrenergic blocking agents on ATP concentration and on incorporation of 32Pi into ATP in rat fat cells. Biochem. Pharmacol. 24, 1659-1662 (1975).
- Chan AC, Poon JT, Fan JK et al. Impact of conversion on the long-term outcome in laparoscopic resection of colorectal cancer. Surg. Endosc. 22, 2625-2630 (2008).
- Pollard CW, Nivatvongs S, Rojanasakul A et al. Carcinoma of the rectum. Profiles of intraoperative and early postoperative complications. Dis. Colon Rectum. 37, 866-874 (1994).
- Lim C, Dokmak S, Farges O et al. Reoperation for post-hepatectomy hemorrhage: increased risk of mortality. Langenbecks. Arch. Surg. 399, 735-740 (2014).
- Romano S, Tortora G, Scaglione M et al. MDCT imaging of post interventional liver: A pictorial essay. Eur. J. Radiol. 53, 425-432 (2005).
- Anderson SW, Lucey BC, Rhea JT et al. 64 MDCT in multiple trauma patients: Imaging manifestations and clinical implications of active extravasation. Emerg. Radiol. 14, 151- 159 (2007).
- Li TF, Duan XH, Li Z, Ren JZ, Zhang K, et al. (2015) Endovascular embolization for managing anastomotic bleeding after stapled digestive tract anastomosis. Acta Radiol 56: 1368-1372.
- Tinto HR, Di Primio M, Tselikas L et al. Selective arterial embolization of lifethreatening renal hemorrhage in four patients after partial nephrectomy. Diagn. Interv. Imaging. 95: 601-609 (2014).