Research Article - Imaging in Medicine (2016) Volume 8, Issue 4
Brain imaging assessment of associated abnormalities in patients with cavum septi pellucidi
Wassan A Khudhair Al-Saedi1 & Qays A Hassan Altimimy*2
1Department of Surgery, Al-Nahrain College of Medicine, University of Al-Nahrain, Baghdad, Iraq
2Department of Surgery, Al-kindy College of Medicine, Baghdad University, Baghdad, Iraq
- *Corresponding Author:
- Qays A Hassan Altimimy
Department of Surgery, Al-kindy
College of Medicine Baghdad University
Baghdad, Iraq
Tel.: 9647722604163
Email: qtimeme@yahoo.com
Abstract
Purpose: To assess the relation of cavum septi pellucidi (CSP) to other brain abnormalities and correlate this to its size and form of presentation.
Methods: We reviewed the neuroimaging studies of 1840 patients in our cross sectional study. A CSP was found in 85 (4.6%) of these patients. We graded CSP into three grades: I<1 cm3, II 1-2 cm3, III>2 cm3.
Results: Headache was the main presenting symptom in 44.7% of our patient’s sample. Patients less than 20 years old tend to have grade I CSP while grades II and III occurred more in patients older than 20. Sixty-seven percent of patients with grade I show no associated brain abnormality. There is no significant predominance of one sex over the other to have CSP.
Conclusion: Most of grade I patients show no other abnormality while most of patients with grades II and III show other abnormalities in their brain imaging.
Keywords
cavum septum pellucidum, brain imaging, MDCT, MRI.
Introduction
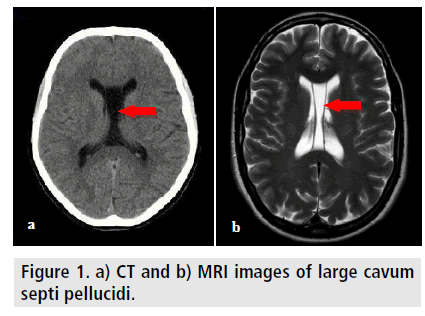
The cavum septi pellucidi (CSP) is the space between the two leaflets of the septum pellucidum. Examples of CSP can be seen in FIGURE 1 [see red arrows]. The septum pellucidum is a thin triangular translucent sheet of two laminae that extends from the anterior part of the body, the genu, and the rostrum of the corpus callosum to the superior surface of the fornix. During fetal development at approximately the twelfth week of gestation, a space forms between two laminae, which is the CSP. At approximately the twentieth week of gestation, the laminae start to close. This closure ends shortly after birth (3–6 months postnatally) in ninety per cent of cases [1]. Fusion of the CSP is attributed to rapid development of the hippocampus and corpus callosum. Incomplete fusion results in the persistence of a cavum, which, in turn, reflects possible neurodevelopmental anomalies of these midline structures [2].
CSP is sometimes called the fifth ventricle but this term seems to be inappropriate as there is no any direct communication with the ventricular system.
CSP has been loosely associated with schizophrenia, post-traumatic stress disorder, chronic brain trauma and antisocial personality disorder [3-5]. An absent CSP in antenatal imaging is a concerning feature and is associated with significant CNS anomalies [6]. However, for the majority of individuals, CSP produces no ill effects.
Multiple studies was held previously to evaluate the CSP and some of those studies consider it as a normal variant while the other consider it as a sign of midline brain developmental abnormality. The purpose of this study was to assess the relation of CSP to other brain abnormalities and correlate this to its size and form of presentation.
Materials and methods
Between May 2014 and May 2016, we reviewed 1840 brain imaging requested patients ranging in age from 3 months till 65 years. The study was done in a general hospital contain different departments and centers such as neurology, stroke, pediatric and epilepsy centers as well as outpatients clinics. Patients were presented with different signs and symptoms subjected them for brain magnetic resonance imaging (MRI) and multidetectors computed tomography (MDCT) imaging. A CSP was found in 85 (4.6%) of these patients; forty-one (48.2%) were female and forty-four (51.8%) were male. Each patient included in this study underwent a review of their request for brain imaging with their presenting symptoms and clinical data. The measurements are taken in three dimensions to measure the size of the CSP and according to the results, we graded CSP into three grades: I<1 cm3, II=1-2 cm3, III>2 cm3.
Modalities used for patient’s brain imaging evaluation were MRI and MDCT.
Regarding the MRI, all scans were performed on a General Electric 1.5 T scanner. The images were reformatted in the coronal plane, with 1 mm thickness and consisted of 128 contiguous slices. The axis for coronal slices was parallel to the axis of the brain stem. Coronal sequences extended from the tip of the frontal pole to the tip of the occipital pole.
Regarding CT scan, all scans were performed on a General Electric 64 slices MDCT scanner. Acquisition parameters were as follows: head scan FOV scan type: Helical, Rotation Time: 0.4 s, beam collimation (mm): 20 mm, 16 detector rows, pitch=0.531, speed=10.62 mm/ rotation, slice thickness=2.5 mm, interval=1.25 mm, Kv=120. Images reconstruction was done in two windows; brain soft tissue (WW=80, WL=25) and bone (WW=3000, WL=300). The patients head tilt so that a line connecting the lateral canthus of the eye and the external auditory canal is perpendicular to the CT table top. We used axial mode and angle the gantry when we cannot place the patient’s head within 15 degrees of the proper setup angle. These images were reconstructed in the coronal plane, with 0.6 mm thickness; the axis for coronal slices was parallel to the axis of the brainstem.
| Age group ( y) | Maleno (%) | Female no (%) |
Total no (%) |
|---|---|---|---|
| <5 | 21 (52.5) | 19 (47.5) | 40 (100.0) |
| 5-19 | 6 (33.3) | 12 (66.7) | 18 (100.0) |
| 20-39 | 5 (55.6) | 4 (44.4) | 9 (100.0) |
| >40 | 12 (66.7) | 6 (33.3) | 18 (100.0) |
| Total | 44 (51.8) | 41 (48.2) | 85 (100.0) |
P=0.250.
Table 1.Distribution of study sample according to sex and to age group.
Data management and statistical analysis were performed by using the statistical package for social sciences (SPSS) version 19 for Microsoft Windows. Statistical significance was indicated by a P value of less than 0.05.
Results
Males constitute 51.8% of our patient's sample while 48.2% of them were females, so in our sample male: female ratio was 1.07:1. This slight male predominance was noticed in all age groups that had been studied except in those young children and teenagers, i.e. 5-19 year old, but these findings were not significant (P=0.250) as seen in TABLE 1.
Headache comprise 44.7% of our patients sample presentation; it was the main presenting symptom in 94.4% of age group 5–19 year old and 77.8% of age group 20-40 year old, while delayed in milestones was the main presenting symptom in 42.4% of age group below 5 year old as seen in TABLE 2 in which the results were significant (P<0.001).
Our results show that the first presented symptom in both sex was headache (45.9%) with slight female predominance while the second was delayed in milestone (20.0%) with male predominance (P=0.750). Most of those patients who presenting with headaches state that the headache was chronic in nature and usually begin in the morning, peaked at noon and remitted in the afternoon and many of them diagnosed apparently as migraine.
| Symptoms or pathological abnormalities | <5 y no (%) |
5-19 y no (%) |
20-40 no (%) |
>40 no (%) |
Total no (%) |
|---|---|---|---|---|---|
| Headache | 3 (7.5) | 17 (94.4) | 7 (77.8) | 11 (61.1) | 38 (44.7) |
| Hydrocephalus | 8 (20.0) | 1 (5.6) | 0 (0.0) | 1 (5.6) | 10 (11.8) |
| Delay in milestone | 17 (42.5) | 0 (0.0) | 0 (0.0) | 2 (11.1) | 19 (22.4) |
| Fit | 9 (22.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 9 (10.6) |
| Tumor | 1 (2.5) | 0 (0.0) | 1 (11.1) | 2 (11.1) | 4 (4.7) |
| Others* | 2 (5.0) | 0 (0.0) | 1 (11.1) | 2 (11.1) | 5 (5.9) |
| Total | 40 (100.0) | 18 (100.0) | 9 (100.0) | 18 (100.0) | 85 (100.0) |
P<0.001 *others include gait disturbance, stroke, nausea and vomiting.
Table 2.Distribution of study sample according to age groups & symptoms or pathological abnormalities.
| Grade | <5 y no (%) | 5-19 y no (%) | 20-40 no (%) | >40 no (%) | Total no (%) |
|---|---|---|---|---|---|
| I | 33 (82.5) | 17 (94.4) | 6 (66.7) | 3 (16.7) | 59 (69.4) |
| II | 5 (12.5) | 1 (5.6) | 1 (11.1) | 12 (66.7) | 19 (22.4) |
| III | 2 (5.0) | 0 (0.0) | 2 (22.2) | 3 (16.7) | 7 (8.2) |
| Total | 40 (100.0) | 18 (100.0) | 9 (100.0) | 18 (100.0) | 85 (100.0) |
P<0.001
Table 3. Distribution of study sample according to age groups and CSP grades.
| CSP grades | ||||
|---|---|---|---|---|
| Symptoms or pathological abnormalities | Grade 1 no (%) |
Grade II no (%) |
Grade III no (%) |
Total no (%) |
| Headache | 23 (39.0) | 12 (63.2) | 3 (42.9) | 38 (44.7) |
| Hydrocephalus | 8 (13.6) | 1 (5.3) | 1 (14.3) | 10 (11.8) |
| Delay in milestone | 16 (27.1) | 2 (10.5) | 1 (14.3) | 19 (22.4) |
| Fit | 7 (11.9) | 2 (10.5) | 0 (0.0) | 9 (10.6) |
| Tumor | 2 (3.4) | 0 (0.0) | 2 (28.6) | 4 (4.7) |
| Others* | 3 (5.1) | 2 (10.5) | 0 (0.0) | 5 (5.9) |
| Total | 59 (100.0) | 19 (100.0) | 7 (100.0) | 85 (100.0) |
P=0.402 *others include gait disturbance, stroke, nausea and vomiting.
Table 4. Distribution of study sample according to CSP grades & symptoms or pathological abnormalities.
| CT & MRI brain findings | |||
|---|---|---|---|
| CSP Grade | Normal no (%) | Abnormal* no (%) | Total no (%) |
| I | 40 (67.8) | 19 (32.2) | 59 (100.0) |
| II | 8 (42.1) | 11 (57.9) | 19 (100.0) |
| III | 3 (42.8) | 4 (57.2) | 7 (100.0) |
| Total | 51 (60.0) | 34 (40.0) | 85 (100.0) |
Table 5. Distribution of study sample according to normality of brain imaging findings and CSP grades.
We found that 75.6% of the female patients presented with small size CSP (grade I) while large size CSP (grades II and III) tend to present more in males (P=0.405).
As in TABLE 3, our results show significant predominance of grade I CSP in patients less than 20 year old and grades II and III in patients more than 20 year old (P<0.001).
Our results show that there is not significant association between tumors (28.6%) as past presenting complain and grade III CSP. Most of grade II CSP patients presented with headache (63.2%) while only 39% of grade I CSP patients presented with headache as in TABLE 4 (P=0.402)
Although the results are not significant (P=0.087), 67.8% of patients with grade I CSP show no associated brain abnormality while 57.9% of patients with grade II & 57.2% of patients with grade III CSP show other associated abnormalities in their brain imaging as seen in TABLE 5.
Discussion
Multiple studies was held previously to evaluate the CSP and most of them concentrate on infants and few focus on the relation between its present and certain psychological disorders.
The reported incidence of CSP in brain CT is 5.5% in Great Britain, 1.24% in China and 0.93% in Taiwan [7]. In our study, the incidence of CSP was 4.6% and there was no significant predominance of one sex over the other to have it; however grade II and III tend to presented more in males than females.
In 1983, Akiyama et al publish that seventy one patients with CSP were found among 2722 patients who had received CT scanning at a mental hospital. In this study, the incidence of CSP was 2.6%, sex ratio was M:F 1.9:1.0 which are a results close to ours.
In Akiyama et al study [8], complications of epileptic attacks and mental retardation were 22.5% and 9.9% of the patients with CSP, respectively. Frequency of these complications was significantly higher, as compared with the patients without CSP. Bodensteiner et al. [9] in 1990 found that eight out of nine children studied showed observed abnormalities included cognitive impairment, seizures, hypoplasia of the corpus callosum, optic nerve hypoplasia, and growth failure. The incidence of intellectual dysfunction, the association with midline anomalies of the brain and growth failure all suggests that wide CSP may represent part of a spectrum of midline brain anomalies. Similar findings were noticed in 1998 by Guru Raj et al. [10] who detect fifty four consecutive cases of CSP amongst 1281 patients who underwent cranial CT scans; and their clinical and radiological features were studied. Recurrent seizures and developmental delay were the commonest presenting symptoms seen. Significant neurological deficits were present in 75.9% of these cases. Additional cerebral abnormalities were observed in the CT scan in 76% of cases, the commonest being cortical atrophy, cerebral infarction and hydrocephalus. Similarly in 2007, Kaciński et al. [11] reported that the majority of the children with CSP had also coexisting brain malformations diagnosed in MRI e.g. dysplasia septo-optica and agenesis of corpus callosum. Mental retardation was diagnosed in 1/3 children with different structural brain malformation but also in 11% of children with CSP as well. Comparatively our results shows that headache was the main presenting symptoms in all age groups and, although the results were not significant, 67.8% of patients with grade I CSP show no associated brain abnormality while 57.9% of patients with grades II & 57.2% of patients with grade III CSP show other associated abnormalities in their brain imaging.
In 1996, Shioiri et al [12] studied 113 patients with affective disorders (69 with bipolar disorder and 44 with major depression), 40 schizophrenic patients, and 92 control subjects by MRI. Significantly higher incidence of CSP (moderate to large) compared with the controls was found only in the schizophrenics. These findings are consistent with the hypothesis that neurodevelopment abnormality may be present in schizophrenia, and such an abnormality may also be present in some patients with bipolar disorder. Also in 1996, Nopoulos et al. [13] stated that CSP is a midline developmental anomaly shown to have increased incidence in patients with schizophrenia. In 2003, Kim et al. [14] noticed that CSP size in tuberous sclerosis (TS) children was significantly smaller than in normal control subjects, and it was inversely associated with attention-deficit/hyperactivity disorder (ADHD) symptom severity in the TS subjects. CSP size was not significantly associated with the comorbid diagnoses of obsessive-compulsive disorder (OCD) or ADHD. These results were replicated in the independent sample of adults with TS and their same-age control subjects. In 2004, Galarza et al. [3] published that thirty-two female patients with a diagnosis of residual schizophrenia and 19 female control subjects were studied through cerebral MRI. The prevalence of CSP was significantly higher in the patients with schizophrenia. No other significant associations with previously described morphological brain changes were found. As our study was held in a general hospital (not in a mental hospital), no schizophrenic patients were included.
Conclusion
Our study reviewed 1840 brain imaging requested patients and CSP was found in 85 (4.6%) of them. There is no significant predominance of one sex over the other to have CSP however grade II and III CSP tend to presented more in males than females. Headache was the main presenting symptom mainly in large CSP (grades II and III). Grade I CSP was noted more in patients less than 20 year old, some of them presented with developmental delay and seizures. Grades II and III CSP were more common in patients older than 20 year old, some of them presented with past history of tumors. Although the results are not significant but most of grade I CSP patients show no other abnormality while most of patients with grades II and III CSP show other abnormalities in their brain imaging.
Compliance with ethical standards
•Conflict of interest: The authors declare that they have no conflict of interest.
•Funding source: none.
•The ethical and scientific consideration: Approvals of the local ethical and scientific committees were obtained before study onset.
•Informed consent: The author declare that no patient data appears in this article.
References
- Clark DL, Boutros NN, Mendez MF. The brain and behavior: An introduction to behavioral neuroanatomy. Cambridge University Press. 3, 217-218 (2010).
- Raine A, Lee L, Yang Y, Colletti P. Neurodevelopmental marker for limbic maldevelopment in antisocial personality disorder and psychopath. Br J Psychiatry. 197, 186-192 (2010).
- Galarza M, Merlo AB, Ingratta A, et al. Cavum septum pellucidum and its increased prevalence in schizophrenia: A neuroembryological classification. J Neuropsychiatry Clin Neurosci. 16, 41-46 (2004).
- May FS, Chen QC, Gilbertson MW, et al. Cavum septum pellucidum in monozygotic twins discordant for combat exposure: relationship to posttraumatic stress disorder. Biol Psychiatry. 55, 656-658 (2004).
- Zhang L, Ravdin LD, Relkin N, et al. Increased diffusion in the brain of professional boxers: a preclinical sign of traumatic brain injury? AJNR Am J Neuroradiol. 24, 52-57 (2003).
- Winter TC, Kennedy AM, Byrne J et al. The cavum septi pellucidi: why is it important? J Ultrasound Med. 29, 427-444 (2010).
- Chen JJ, Chen CJ, Chang HF, et al. Prevalence of cavum septum pellucidum and/or cavum Vergae in brain computed tomographies of Taiwanese. Acta Neurol Taiwan. 2, 49-54(2014).
- Akiyama K, Sato M, Sora I, et al. A study of incidence and symptoms in 71 patients with cavum septi pellucidi. No To Shinkei. 35, 575-581(1983).
- Bodensteiner JB, Schaefer GB. Wide cavum septum pellucidum: a marker of disturbed brain development. Pediatr Neurol. 6, 391-394(1990).
- Guru Raj AK, Pratap RC, Jayakumar R, et al. Clinical features and associated radiological abnormalities in 54 patients with cavum septi pellucidi. Med J Malaysia. 53, 251-256 (1998).
- Kacinski M, Kubik A, Herman-Sucharska I, et al. MRI brain imaging data in children with cavum septi pellucidi and vergae. Przegl Lek. 64, 923-928 (2007).
- Shioiri T, Oshitani Y, Kato T, et al. Prevalence of cavum septum pellucidum detected by MRI in patients with bipolar disorder, major depression and schizophrenia. Psychol Med. 26, 431-434 (1996).
- Nopoulos P, Swayze V, Andreasen NC. Pattern of brain morphology in patients with schizophrenia and large cavum septi pellucid. J Neuropsychiatry Clin Neurosci. 8, 147-152 (1996).
- Kim KJ, Peterson BS. Cavum septi pellucidi in Tourette syndrome. Biol Psychiatry. 54, 76-85 (2003).