Commentary - Diabetes Management (2017) Volume 7, Issue 2
Self-management of diabetes blood sugar as measured by HbA1c using "dental air force"
Abstract
Introduction
Some form of plaque removal by twigs and leaves has been around since 3000 BC. The modern toothbrush was first introduced in England in 1780.
Insulin resistance, a phenomenon that often starts out symptomless in childhood and closely associated with Body Mass Index (BMI) and a high carb diet, is the mismanagement of the limited resource of the pancreas. Once diagnosed as prediabetes, the patient’s condition later evolves with age into Type II diabetes resulting in the use of a standard accepted protocol to try to manage the disease. This protocol includes a dynamic self-management by the use of an oral medication (Metformin), parental insulin for blood sugar control, a well-controlled diet, proper exercise, and frequent blood testing. This protocol needs to be improved.
The objective of this commentary is to suggest an amendment to standard diabetes management in order to achieve higher positive predictable outcomes in the overwhelming population of diabetics while also achieving health care cost savings.
Inflammatory disease
Within recent decades, diabetes along with other systemic diseases such as periodontal disease, heart, liver and gastrointestinal diseases, Chronic Obstructive Pulmonary Disease (COPD), depression, dementia, Alzheimer’s, arthritis, osteoporosis, Peripheral Arterial Disease (PAD) and even some cancers has been characterized as an inflammatory disease.
Nowhere has more investigation been done on the association of periodontal inflammation with other diseases than with diabetes. Conversely many associations exist with diabetes and other inflammatory diseases, such as heart disease, PAD and periodontal disease.
Prior to 2017, diabetes was reported to contribute to between 3-4% of deaths in the United States. Current analysis of diabetics and death put that number closer to 12-19% [1].
Periodontal disease
Periodontal disease, once thought of as a local disease, is a systemic inflammatory disease characterized by biofilm. This biofilm consists of a rich microbial-organized community that has nutrients brought in and acidic waste removed through corridors intertwined in a matrix of organisms that are 100-300 cells thick-called plaque. The biofilm defies antimicrobial regimens due to the inaccessibility of the periodontal pocket during conventional home care (tooth brushing, flossing, oral irrigation and mouthwash) and the hydrophobic sticky glycoprotein and lipid buildup of matter making this home treatment ineffective. Stratification of the bacteria is assembled in relationship to aerotolerance and metabolism. Gram-negative cocci, rods and filaments quantities increase as more anaerobic bacteria are established [2]. As the biofilm thickens and becomes more mature, these anaerobic bacteria can live deeper within the biofilm to further protect them from the oxygen-rich environment within the oral cavity.
The etiology of periodontal disease and diabetes is multi factorial and bidirectional. The host response to the biofilm species ratio, the quantitative population of anaerobic bacterial periodontal pathogens and the endotoxin gingipains burden in a diabetic may be greater than in a non-diabetic. Bacterial gingipains are protease [3]. Porphyromonas gingivalis (Pg) is a major contributor to periodontitis and is strongly associated with peripheral systemic diseases. Pg is an organism in the periodontal pocket that creates a milieu of potential combinations of other pathogens that work together to create an environment vulnerable to these organisms entering the bloodstream.
The bacteria Pg, Aa, Fn, Pi are frequent components for many of the peripheral diseases in addition to diabetes. Pg gingipains degrade macrophage CD14, thus inhibiting activation of the leukocytes through the lipopolysaccharide receptor, and thereby allowing sustained colonization of Pg. Simply put it sabotages the immune system.
There is a confluence of events that occur with periodontal disease. The immune response is elicited by bacterial endotoxins resulting in a cascade of inflammatory cytokines such as IL-1 il-6 and tumor necrosis factor (TNF). The cytokines and chemokines increase adhesion and permeability thus wounding the endothelial cells of blood vessels throughout the entire circulatory system. Particularly important to diabetics is the inflammation in vessels in the pancreas, kidneys, heart, eyes, intestines and peripheral limb capillary beds. Blood pressure also increases due to the reduction of the vessel lumen causing circulation resistance [4].
Periodontal disease is the most prevalent disease on earth. About half of all adult humans have periodontal disease by the age of 35. An unprecedented 74% has the disease by age 65 [5].
It is a pandemic, systemic, vascular inflammatory disease that preys upon genetic predisposition and host response. It is highly influenced by home care management as is diabetes. The source of the debilitation in this and most other systemic diseases is chronic inflammation. Periodontitis is an insidious pandemic disease because of its communicability.
Periodontal disease is the low hanging fruit of chronic inflammation in all populations that is underdiagnosed by physicians. Management of periodontal disease is the most overlooked part of diabetes management protocol and consequentially becomes very costly to the quality of life-physically, financially and emotionally.
Traditional periodontal protocol
There is evidence that shows traditional professional periodontal treatment of deep cleaning and scaling of root surfaces helps lower hba1c by 0.4% predictably [6].
The problem is recidivism because the post-operative instruction after professional periodontal therapy is the standard regimen for home care which is flossing and brushing. It is the same standard that is recommended for its prevention which clearly has not worked and therefore the populations of tenacious pathogens inaccessible to both brushing and flossing quickly return to the pre diagnosis levels. Further destruction is inevitable and inflammatory host response progresses.
New periodontal protocol for diabetics
Diabetic physicians look to hunt down and reduce inflammation in the body that can cause insulin resistance and erratic blood sugar fluctuations. The mouth and its ever present source of chronic inflammation are rarely discussed or addressed in diabetic protocol. The dentist can identify the first signs of diabetes through diagnosing periodontal disease and being involved in the collaborative effort necessary for diabetes management [7].
It should be an obligation that diabetic management providers emphasize a new periodontal protocol for diabetes.
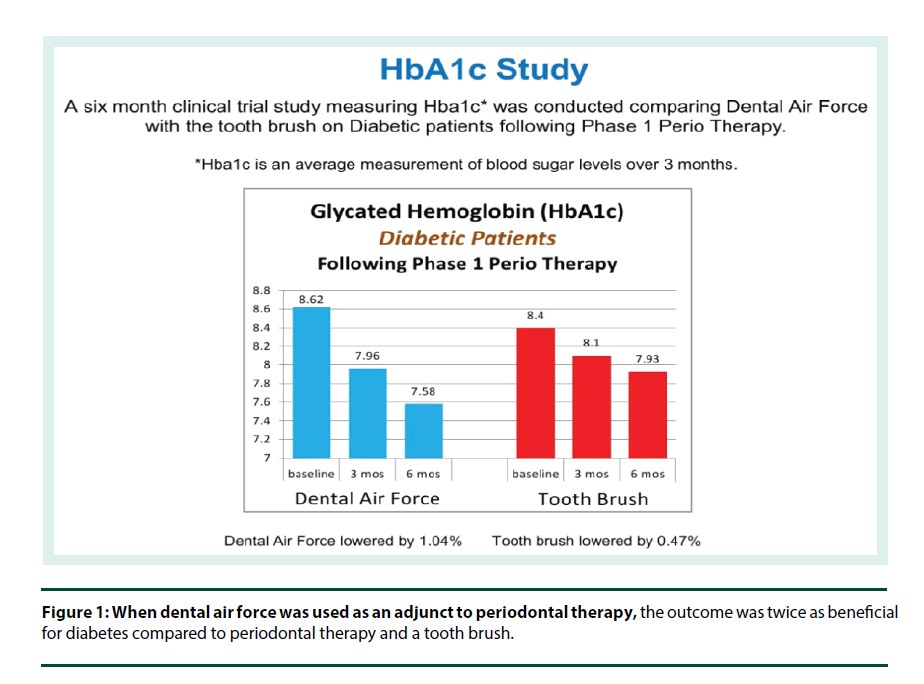
A new FDA approved medical device known as Dental Air Force has been designed to increase predictable diabetic outcome by treating oral inflammation. It has been shown to have a substantial impact on diabetic populations’ control of blood sugar as measured by HbA1c. In one independent six month study, using Dental Air Force as an adjunct to periodontal therapy, HbA1c in the diabetic population was lowered by 1.04% or over two times the average outcome of periodontal therapy alone (Figure 1) [8].
Figure 1: When dental air force was used as an adjunct to periodontal therapy, the outcome was twice as beneficial for diabetes compared to periodontal therapy and a tooth brush.
As a review, the British Medical Journal (BMJ) reported a 1% reduction in HbA1c levels gives the following reduction in combined diabetes-related endpoints [9]:
• 21% risk reduction for any endpoint related to diabetes.
• 21% risk reduction for deaths related to diabetes.
• 37% risk reduction in micro vascular complications.
• 14% risk reduction in myocardial infarction.
• 43% risk reduction in amputations.
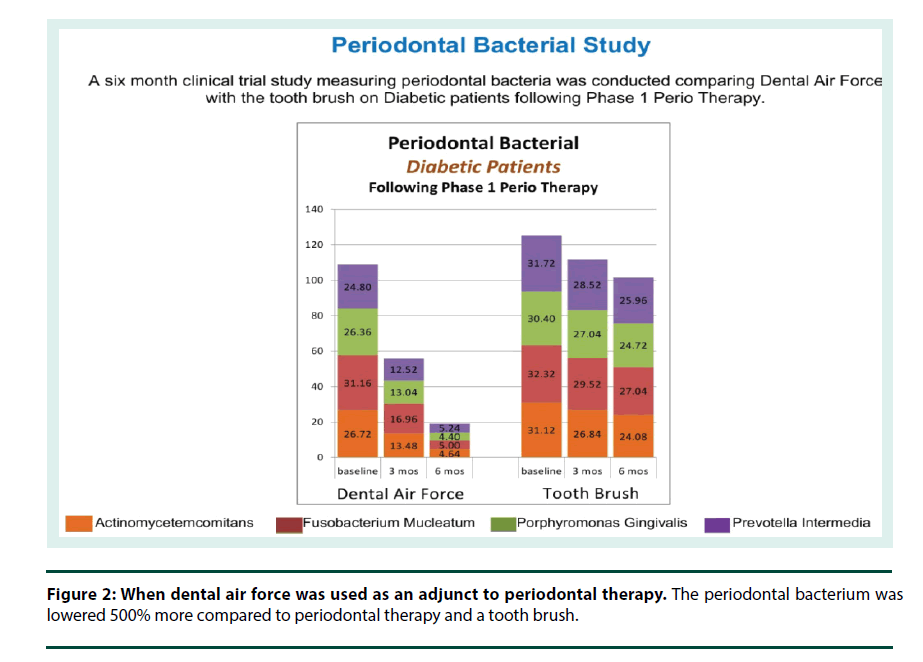
Dental Air Force is very promising to diabetics because it is the persistent daily reduction of the periodontal pathogen titers (versus only periodontal therapy) that was shown to continually drive down Pg, Aa, Fn, and Pi by 500% over the course of the study, unlike periodontal therapy followed by toothbrush maintenance (Figure 2) [10].
Home care in periodontal therapy, requires the ability to disrupt and remove biofilm. Dental Air Force is a powerful advancement and paradigm shift from tooth brushing and flossing by using a novel scientific approach in removing the bio-burden of periodontal pathogens below the gum line and in between teeth. It works to help stop the inflammation causing insulin resistance in the vast population of diabetics that harbor periodontal disease.
It uses a jet stream of air, water and sodium bicarbonate and can also deliver disinfectants and probiotics into the periodontal pocket. These combinations disrupt the biofilm bacterial quorum sensing and bombard the diseased sites with air creating an oxygenated environment where the gram negative anaerobic periodontal pathogens are seeking safe harbor. The use of this technology mitigates the growth and organization of the biofilm while shifting the population to a kinder aerobic species. It alters the population of pathogens in the previously inaccessible sites where the capillary bed is deep in the periodontal pocket-reducing the bio-burden and quelling the host response of chronic inflammation initiating wound and pocket depth reduction. Furthermore the use of encapsulated sodium bicarbonate in the dental cleaner infiltrate the interdental sites; dislodging and breaking through the sophisticated society of biofilm matrix creating disorder with a high pH shock-effect within its ecosystem.
Cost savings
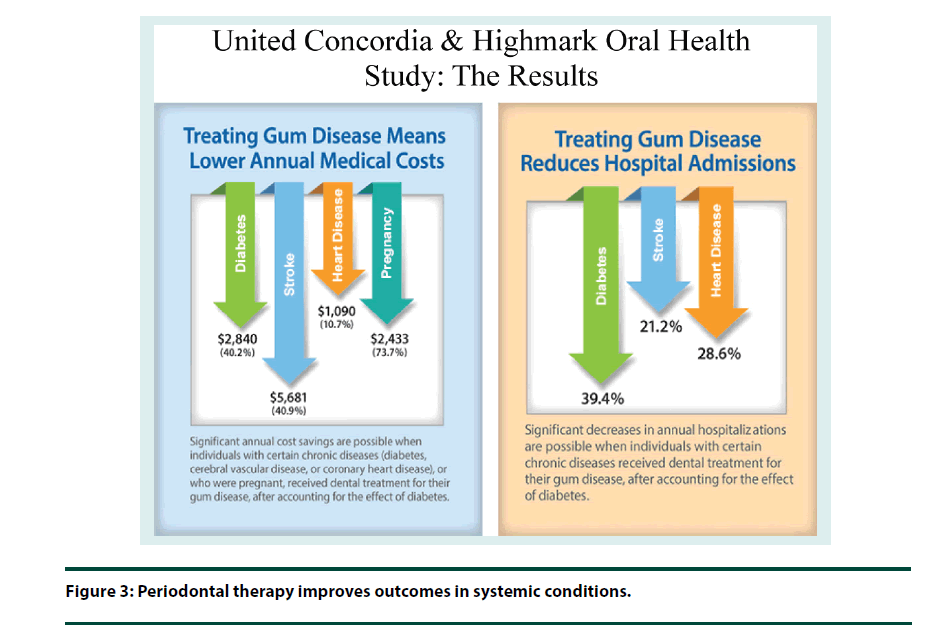
Dr. Marjorie Jeffcoat for United Concordia dental coverage company and Highmark medical insurance company published a study on the costs of periodontal disease related to three systemic diseases and pregnancy. The cost impact of periodontal disease is significant particularly to the diabetic population (Figure 3) [11]:
Annual Medical Costs Savings (savings every year):
• $2,840 for members with diabetes.
• $1,477 for diabetes outpatient drug costs.
• $5,681 for members with cerebral vascular disease (stroke).
• $1,090 for members with coronary artery disease (heart).
• $2,433 for women who were pregnant.
Annual Hospitalization Reductions (savings every year):
• 39.4% for members with diabetes.
• 21.2% for members with stroke.
• 28.6% for members with heart disease.
Incorporating Dental Air Force in the diabetic management protocol not only provides a dollar cost savings as the Jeffcoat study points out but there is no monetary value on ones kidneys, eyes, heart and limbs. In addition, the severity of diabetes has a social and productivity impact. It is believed that Dental Air Force would have a multiplying impact on Jeffcoat’s findings with regard to all aspects of quality of life.
Conclusion
Periodontal disease is prevalent among diabetic patients worldwide. Along with metformin, parental insulin, proper diet, exercise and blood sugar testing, periodontal chronic inflammation management using Dental Air Force should be prescribed for the long term self-management of diabetic patients.
It is with hope this new device is adopted as the adjunct to the new gold standard in diabetes management providing the patient a much better life as a diabetic as well as providing substantial health care costs savings over and above the present standard.
Much more research is needed in all aspects of health care to discover further benefits of the use of Dental Air Force as a medical device.
References
- Stokes A, Preston S. Deaths attributable to diabetes in the United States: Comparison of data sources and estimation approaches. PLoS. One. 12(1), e0170219 (2017).
- Marsh PD. Dental plaque as a biofilm and a microbial community–implications for health and disease. BMC. Oral. Health. 6(Supl. 1), S14 (2006).
- Imamura T. The role of gingipains in the pathogenesis of periodontal disease. J. Periodontol. 74(1), 111–118. (2003).
- Leong X, Ng C, Badiah B et al. Association between hypertension and periodontaldontitis: Possible mechanisms. Sci. World. J. 2014(2014), 1–11 (2014).
- https://www.perio.org/consumer/cdc-study.htm
- Teeuw WJ, Gerdes VE, Loos BG. Effect of periodontal treatment on glycaemic control of diabetic patients: a systematic review and meta-Analysis. Diabetes Care. 33(2), 421–427 (2010).
- Teeuw W, Kosho M, Poland D et al. Periodontitis as a possible early sign of diabetes mellitus. BMJ. Open. Diabetes. Res. Care. 5(1), e000326 (2017).
- Ameet M, Vinay V, Raju A et al. A clinical study on dental air force home dental cleaning system on adult chronic periodontitis patients and its assessment to C-reactive protein levels. Int. J. Exp. Dental. Sci. 1(1), 14–18 (2012).
- Stratton IM, Adler AI. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 321(1), 405–412 (2000).
- Shubhangi M, Ameet MM, Rajiv S. A clinical, laboratory and microbiological evaluation on efficacy of dental Air force home dental cleaning system on type 2 diabetic and nondiabetic adult chronic periodontitis patients: A 6-month clinical study. Int. J. Exp. Dental. Sci. 2(1), 1–8 (2013).
- Jeffcoat MK, Jeffcoat RL, Blum JJ et al. Impact of periodontal therapy on general health: evidence from insurance data for five systemic conditions. Am. J. Prev. Med. 47(2), 166–174 (2013).