Review Article - Imaging in Medicine (2016) Volume 8, Issue 1
The evidence supporting radiation safety methods- working towards zero operator exposure
Ryan Reeves* & Ehtisham MahmudDepartment of Cardiovascular Medicine, Sulpizio Cardiovascular Center, University of California, San Diego, CA
- Corresponding Author:
- Ryan Reeves
Department of Cardiovascular Medicine
Sulpizio Cardiovascular Center
University of California, San Diego, CA
Tel: 858-657-8030
E-mail: emahmud@ucsd.edu
Abstract
The evidence supporting radiation safety methods- working towards zero operator exposure
Keywords
radiation safety; interventional; fluoroscopy
Introduction
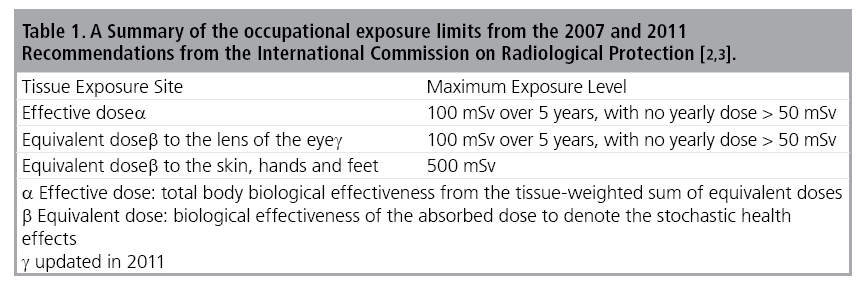
The potential dangers of fluoroscopy became evident with its initial use in research endeavors. Clarence Dally was a research assistant of Thomas Edison and focused his efforts on fluoroscopy. Years of exposure led to a myriad of medical problems that prompted his physician, Dr. Graves to comment, “Dally’s case has told science that the continuous exposure of any part of the human anatomy to the influence of the X rays is deadly to the part so exposed. Of course, it does not interfere with the use of the light for medical purposes when it is handled by experienced persons, but it is not a thing to be trifled with. Under proper care it is of great use” [1]. This continues to hold true today and the effects of chronic exposure to low dose radiation continue to unfold. The use of radiation guidance by interventional physicians results in relatively high levels of occupational exposure, the complete effects of which remain unknown. Occupational exposure limits have been set by the International Commission on Radiological Protection and are summarized in Table 1 [2,3]. Levels of exposure are affected by multiple factors beyond operator control and vary widely across different procedure types. With technological advancements, procedural complexity has increased across all interventional fields and is uniformly associated with increased radiation exposure [4-8]. Increased patient habitus is also a nonmodifiable factor resulting in higher radiation doses during procedures as varied as endovascular repair, joint injections, ureteroscopy and cardiac interventions [9-13]. The radial access site is gaining in popularity during coronary procedures due to lower access site bleeding compared to femoral access, but results in a measurable increased risk of radiation exposure [14]. Shorter operator height may also be a predictor of increased operator exposure [15]. A recent evaluation of the National Cardiovascular Data Registry identified operator and hospital factors as having a moderate impact on fluoroscopy time variation after controlling for patient and procedural characteristics [7].
Population aging is likely to continue as will the demand for interventional procedures. Therefore, determining the risks of performing x-ray guided procedures and optimizing the interventional suite for the personnel providing patient care should continue to accompany advances in imaging systems and interventional techniques.
Deleterious effects of operator radiation exposure
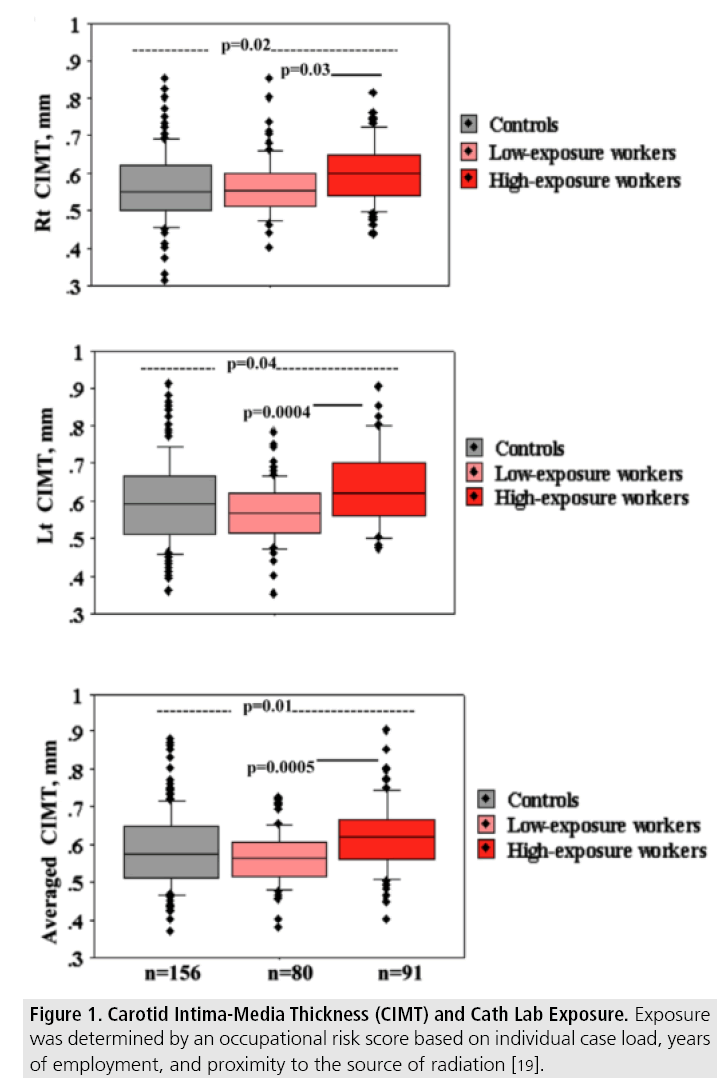
The effects of radiation exposure at the molecular level include DNA double-strand breaks and increased micronuclei [16,17]. A comparison of peripheral lymphocytes between clinical cardiologists and highvolume interventional cardiologists revealed significantly higher micronuclei values in the interventionalists [18]. By testing for high-risk alleles in DNA repair genes, an interactive effect was seen between chronic exposure, smoking, and the high-risk alleles in DNA damage [17]. In another recent study, subclinical effects were observed in high-exposure cath lab staff who had increased carotid intima-media thickness compared to low-exposure and unexposed contemporaries (Figure 1) [19]. Left-sided carotid intima-media thickness correlated with lifetime exposure, as did a biological marker of aging, leukocyte telomere length. In addition, morphologic abnormalities on nail bed capillaroscopy are associated with duration of exposure in interventional operators [20]. The risks of cataracts are another well-established complication of radiation exposure in multiple interventional disciplines [21-23]. Reports of predominantly left-sided brain cancer in highvolume interventional physicians question a causal relationship given standard operator positioning [24,25]. It would be nearly impossible to prove that the incidence of malignancy from chronic exposure to low dose radiation is higher than that of the general population, but statistical data suggest the risk is not negligible [26]. Further studies are required to completely determine causality and to strengthen the current body of evidence regarding the risk of biological effects in the interventional suite.
Figure 1: Carotid Intima-Media Thickness (CIMT) and Cath Lab Exposure. Exposure was determined by an occupational risk score based on individual case load, years of employment, and proximity to the source of radiation [19].
Methods to reduce operator radiation exposure
■Radiation safety training
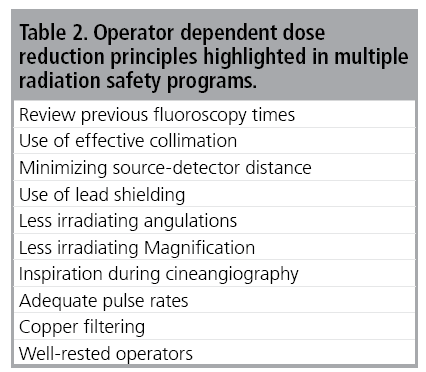
Operator awareness and training, barrier protection, imaging equipment, technique, and robotic assisted procedures have all been identified as targets to reduce radiation exposure. The fundamental principle of “as low as reasonably achievable” [ALARA] remains the cornerstone for limiting patient and staff exposure to ionizing radiation [27-32]. Focused training sessions for interventional staff and trainees are centered on the principle of ALARA and increase efficient use of imaging modalities and decrease markers of exposure without compromising patient care [33-37] (Table 2). The effects of training programs, including simulation center training, are enhanced over time and periodic review courses are of value in maintaining optimal operator awareness [38]. Despite the universally recognized importance of the ALARA principle and the strong evidence behind radiation safety training, a recent survey of cardiology fellows in training revealed that though 82% had undergone formal radiation safety training, only 52% regularly wore a dosimeter and 74% were unaware of the safe levels of radiation exposure [39]. A similar survey of vascular surgery residents also revealed that the ALARA principle is underutilized but is more prevalent in training programs that provided formal radiation safety training [40]. Standardized radiation safety training programs that highlight the ALARA principle and reinforce dose reduction methods are a foundation for operator safety.
■Radiation monitoring
Operator awareness is the foundation of radiation safety training and the ALARA principle. Periodic and real-time exposure monitoring enhance operator awareness and allow for operator adjustments to reduce radiation dose. Real-time monitoring devices that produce visual or auditory information regarding the level of operator exposure are available and have been shown to reduce patient and operator exposure [41,42]. Christopoulos et al. showed that a real-time monitoring device that provides auditory feedback has a major effect on operator behavior, reducing operator exposure without an effect on fluoroscopy time or patient exposure [42]. Therefore, by enhancing awareness with real-time feedback, behavior associated with shielding and distance may significantly reduce operator exposure.s Monthly monitoring may also alert individual operators or an entire interventional team to issues associated with radiation safety and the need for an investigation into the reasons for increased measurements. Practice modifications or systems maintenance may then be implemented to optimize operator protection.
■Barrier protection
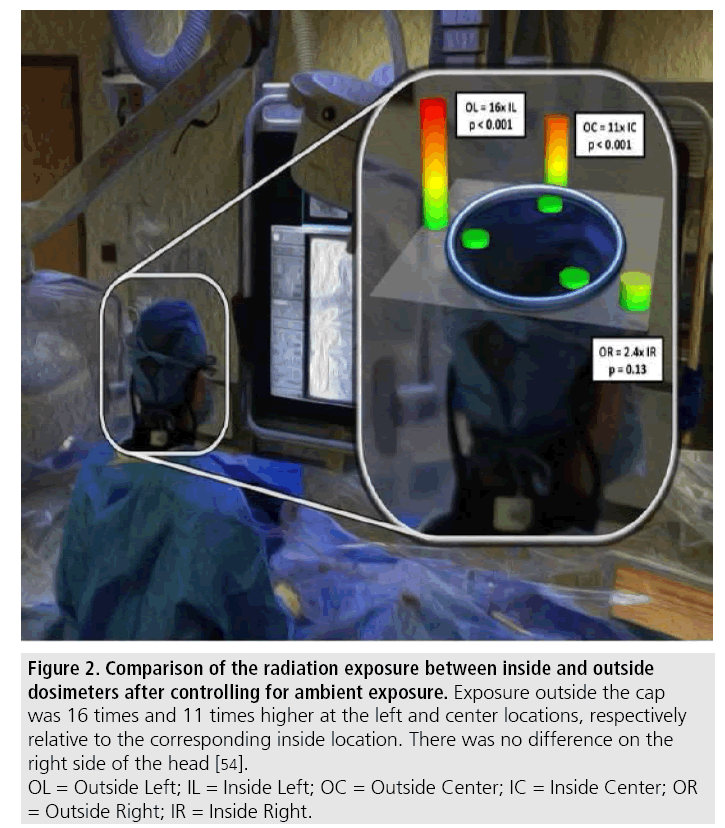
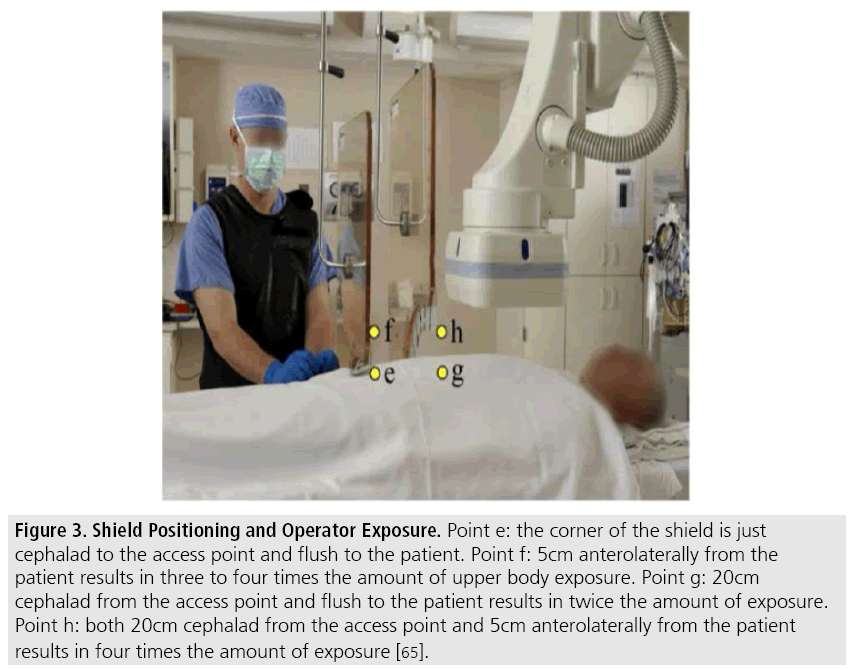
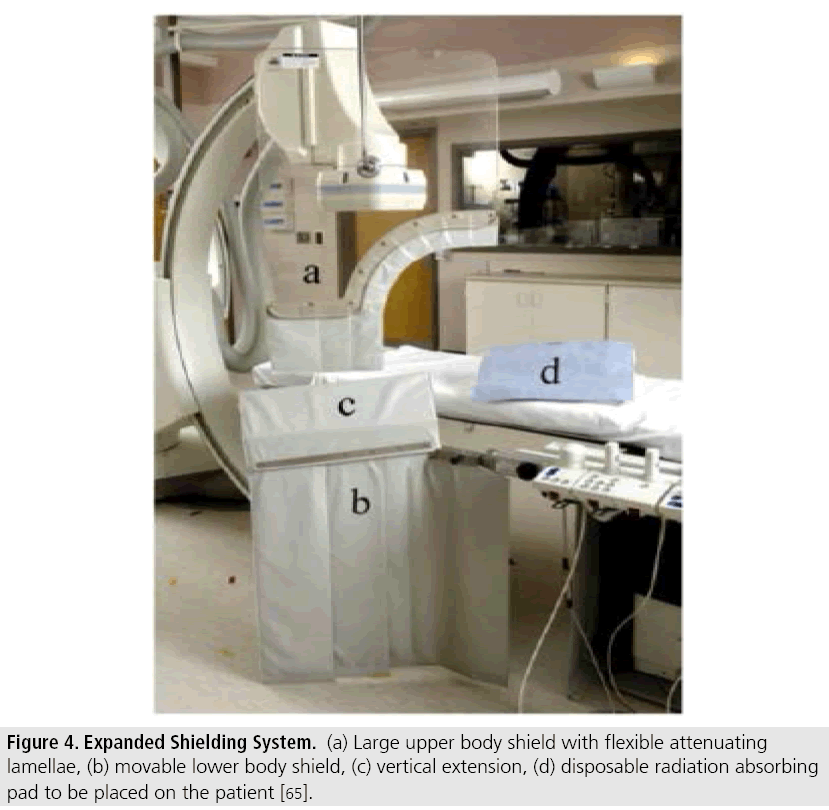
Barrier protection with lead aprons is nearly universal in interventional suites. The clinical effectiveness of lead aprons in attenuating operator exposure is well documented [43,44]. However, the prolonged use of relatively heavy aprons results in physical strain and potential cervical and lumbosacral spine issues. While difficult to demonstrate causality, self-reported orthopedic problems of leadwearing, invasive operators is high [45,46]. In a 2014 survey of members of the Society for Cardiovascular Angiography and Interventions, 49% reported at least one orthopedic injury, while 9.3% required a health-related period of absence [45]. Caseload and age were associated with orthopedic illnesses, which included cervical spine, lumbar spine, hip, knee, and ankle injuries. In a survey comparing multiple sub-specialties, lead apron use was associated with axial skeletal complaints [47]. Relatively light weight barriers that provide a level of protection similar to standard lead barriers have been produced by stacking two different attenuating materials to cover a broad energy range [48,49]. These materials have been fashioned into a myriad of protective barriers and further studies are needed to determine whether the incidence of orthopedic issues may be reduced with their routine use. Standard lead aprons do not provide protection to uncovered areas, namely the head and the extremities. Radiation exposure to the head is well documented and is affected by procedural complexity [8,50-52]. The concern for cranial exposure has led to an interest in developing a tolerable cap with attenuation capabilities. Leadbased protective caps provide cranial protection [53], however routine use has likely been limited due to poor tolerability. The Brain Radiation Exposure and Attenuation During Invasive Cardiac Procedures (BRAIN) study revealed that a light-weight, non-lead cap can reduce exposure across the cranium to near ambient levels [Figure 2] [54]. Other studies confirm the protective ability and tolerability of lightweight, non-lead caps [55- 57] and consideration should be given to routine cranial protection during radiation-guided procedures. Strong evidence exists for the protective ability of leaded-goggles, which should also be considered standard radiation safety equipment [23,58]. Given that the major source of radiation relevant to operator exposure is scatter from the patient, placing protective barriers on the patient has been investigated as a target for exposure reduction. The randomized use of a non-lead drape placed over the patient during 36 EVAR procedures resulted in a greater than 50% reduction in operator exposure [59]. Transcatheter aortic valve replacement is a novel procedure that is dependent on fluoroscopic guidance for optimal results. The placement of a non-lead drape over the patient resulted in a nearly 40% reduction in operator exposure [60]. Similarly, large relative and absolute reductions in operator exposure have been shown during vascular procedures with both femoral and radial access sites [56,61- 63]. Sensible use of room shielding can also have a significant effect on operator exposure. Ceiling suspended, transparent lead glass screens reduce normalized eye dose by a factor of 19 during cardiovascular procedures [64]. The most effective placement of room shielding is in between the source and the operator, with the operator as close as possible to the shield. This requires the operators to frequently adjust mobile shields to maintain and maximize protection. Proper positioning of the ceiling suspended shield results in significantly higher levels of protection. For example, if the shield is 20 cm cephalad from the femoral access point, the operator is exposed to twice the amount of scatter radiation relative to more optimal placement [65]. Moving the shield 5 cm from the patient’s body in addition to 20 cm cephalad from the access site, increases operator exposure by four-fold (Figure 3) [65]. Therefore, one major focus of the aforementioned training courses is reinforcement of the operator’s role in shield management [35,37]. Expanded shielding systems offer high levels of protection that decrease the interventional physician’s role in shield management (Figure 4). The use of a larger shield with flexible, protective lamellae attached to the base, in combination with a protective drape, resulted in a nearly 50% reduction in radiation exposure to staff and physicians [66]. Nearly complete operator isolation from radiation scatter has been demonstrated in a series of nonrandomized cases. Multiple shielding components with translucent sections create a complete attenuation barrier between the operator and the patient while access to catheterization equipment is permitted through flexible drapes. In the case series, operator exposure normalized to fluoroscopy time at various sites was barely detectable, and approached background levels [67]. Modifications of room shielding for non-vascular, fluoroscopic guided procedures have also been shown to reduce operator exposure. Non-lead attenuation drapes (n=50) and sham drapes (n=50) were secured to the image intensifier in a randomized fashion during endoscopic retrograde cholangiopancreatography demonstrating relative risk reduction of 90% for the physician and assisting nurse [68]. While standard-shielding systems may not provide equal or optimal protection for all access sites or complex procedures, these contemporary studies suggest that alternative barrier interventions may effectively be applied to provide increased levels of protection without negatively affecting the interventional procedures.
Figure 2: Comparison of the radiation exposure between inside and outside
dosimeters after controlling for ambient exposure. Exposure outside the cap
was 16 times and 11 times higher at the left and center locations, respectively
relative to the corresponding inside location. There was no difference on the
right side of the head [54].
OL = Outside Left; IL = Inside Left; OC = Outside Center; IC = Inside Center; OR
= Outside Right; IR = Inside Right.
Figure 3: Shield Positioning and Operator Exposure. Point e: the corner of the shield is just cephalad to the access point and flush to the patient. Point f: 5cm anterolaterally from the patient results in three to four times the amount of upper body exposure. Point g: 20cm cephalad from the access point and flush to the patient results in twice the amount of exposure. Point h: both 20cm cephalad from the access point and 5cm anterolaterally from the patient results in four times the amount of exposure [65].
■Imaging systems
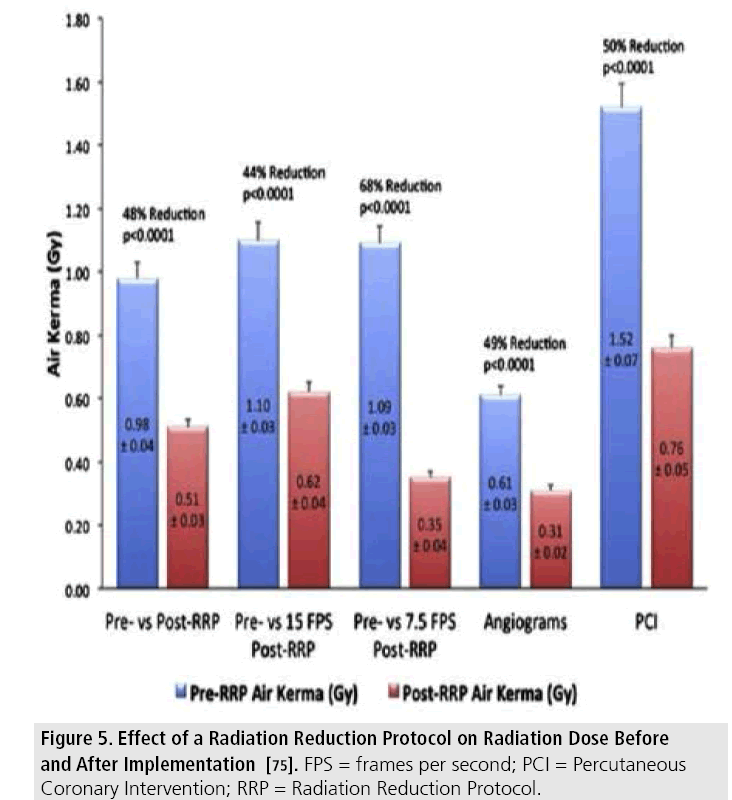
Focus has also been placed on imaging systems and software to reduce the exposure of interventional operators and staff. The availability and use of collimation allows for control of the size of the primary beam and therefore, the amount of scatter radiation. Like shielding, collimation requires operator awareness, has been a focus of radiation safety training courses, and results in exposure reduction within multiple interventional disciplines [33-35,69,70]. Alternative imaging modalities, such as ultrasound may be used to guide access and other components of interventional procedures. For example, the intermittent use of ultrasound reduces radiation dose during the creation of transjugular intrahepatic portosystemic shunts (TIPS) [71]. The combination of large detector systems and larger display monitors allows for adjusting magnification without a perceived degradation in image quality. With a large detector, the zoom setting may be reduced using less radiation dose to create a larger picture, but the region of interest will appear smaller. Larger, customizable monitors allow for a significant increase in image size, producing an image similar to a higher zoom setting on a standard monitor. Comparable quality on larger display monitors with reduced magnification and radiation dose has been demonstrated across a range of zoom setting and display sizes [72]. Simple technical upgrades on many different modern fluoroscopy machines may be performed that contribute to dose reduction. Many of these changes, such as alteration of the pulsed frame rate, may be activated and deactivated as needed at any point during interventional cases. This has been proven in TAVR and coronary procedures, where controlled comparisons of different frame rates resulted in reductions in radiation dose or operator exposure [73,74]. Current fluoroscopic systems can offer advanced imaging processing algorithms that allow for production of high quality final images from lower quality raw images. Enhanced processing allows for technical changes, including increased thickness of spectral filters, lower detector dose rate, and routine use of a lower fluoroscopic dose rate to be instituted without compromising final image quality or affecting the course of the interventional procedure. During diagnostic and therapeutic coronary procedures, radiation dose was decreased by 68% at 7.5 fps and 44% at 15 fps (Figure 5) [75]. Similar image quality with comparable fluoroscopic time, cine imaging, and contrast use with dose reduction protocol compared to standard protocols has been demonstrated [76]. Comparable improvements in dose reduction have also been demonstrated with dose reduction protocols during transarterial chemoembolization for hepatocellular carcinoma procedures [77], TIPS creation [78], and advanced aortic repair and revascularization interventions [10,79]. There is also potential for meaningful dose reduction after the implantation of iterative reconstruction techniques for CT guided procedures [80]. The development of feasible rotational angiography is another technical upgrade that may result in a decreased radiation dose. Rotation through various left-right and cranial-caudal angles during contrast injection produces a cineangiogram with different planar images for each frame of the imaging run. During coronary angiography, an entire coronary system may be imaged with one injection and cineangiogram. The evaluation of standard and rotational anonymized angiograms by three independent cardiologists resulted in high concordance of observer agreement across multiple levels of diagnostic interpretation [81]. Contrast use and patient radiation dose were nearly 40% and 60% lower, respectively.
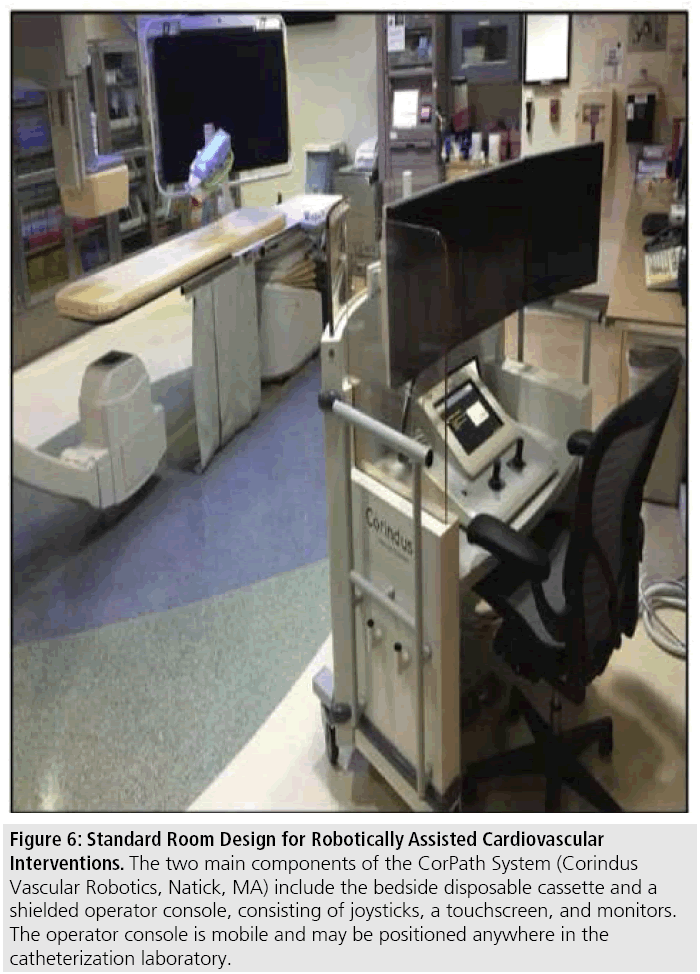
■Robotically assisted interventions
The safety and feasibility of robotically assisted PCI with the CorPath System (Corindus Vascular Robotics, Natick, MA) is described [83]. The bedside unit consists of a disposable cassette placed on a permanent robotic drive that is prepped into the field with a sterile plastic cover. The interventionalist commands the robotic drive by manipulating joysticks and a touch-screen console while sitting in a remote, shielded cockpit (Figure 6). Interventional guidewires may be rotated and advanced with qualitative joystick rotation and toggling or by selecting discrete distances and degrees of torque on the touch-screen. The balloon and stent catheters are manipulated in a similar fashion. In the PRECISE registry technical success without manual conversion was achieved in 162 of the 164 cases, with median operator radiation exposure reduction of 95.2% at the console compared to the traditional table-side operator position. This has been followed by successful reports of complex coronary and percutaneous peripheral arterial interventions given the potential for relatively high operator exposure levels [8,82-85]. Hypothetically, if the bedside operator is 1 meter from the scatter source and exposed to ‘X’ level of radiation, assuming a standard kVP and 0.5 mm lead apron, exposure to the thorax may be estimated at 0.013’X’. If the robotic operator is 3 meters from the source, the cockpit is exposed to 1/9‘X’ level of radiation. The transmission through a 2 mm lead shield around an interventional cockpit is estimated at 0.0007 of the afferent radiation level. Therefore exposure is a mere 0.00008’X’ to the robotic operator, or 163 fold lower than at the bedside position. By combining shielding and distance, the potential for operator exposure likely approaches ambient levels.
Figure 6: Standard Room Design for Robotically Assisted Cardiovascular Interventions. The two main components of the CorPath System (Corindus Vascular Robotics, Natick, MA) include the bedside disposable cassette and a shielded operator console, consisting of joysticks, a touchscreen, and monitors. The operator console is mobile and may be positioned anywhere in the catheterization laboratory.
Conclusion
Radiation safety and meaningful reduction of operator and patient exposure begins at operator awareness. Knowledge of the fundamentals of radiation allow for application of the ALARA principle. Radiation safety training and periodic updates provide reinforcement of these principles and preservation of meaningful gains. Ensuring optimal operation of imaging machines, including patient and table positioning, collimation, last-image hold, use of technical settings, and keen control of gantry angulation are integral methods in augmenting exposure reduction. Many modern imaging systems are equipped with technical upgrades and software algorithms that produce comparable images with less radiation output. Advances in shielding aprons and caps have resulted in lightweight protection that may provide tolerable cranial protection and have less of a long-term musculoskeletal impact on interventional operators. Exposure monitoring is also vital in adjusting individual practice and determining modifiable individual and system factors. Optimal room shielding and robotic assistance have the potential to allow operator exposure to be nearly negligible for certain procedures. Indeed, meaningful reduction in operator exposure may be accomplished without affecting patient care and may be of benefit by reducing patient exposure. We should continue to move forward in optimizing the interventional environment with a goal of operator exposure at near ambient levels without compromising procedural outcomes.
References
- “Edison Fears Hidden Perils of the X-Rays,” New York World, August 3, (1903).
- Wrixon AD. New ICRP recommendations. J. Radiol. Prot. 28, 161-168 (2008).
- International Commission on Radiological Protection. Statement on Tissue Reactions (2011).
- Stewart JK, Looney CB, Anderson-Evans CD. Percutaneous cryoablation of renal masses under CT fluoroscopy: radiation doses to the patient and interventionalist. Abdominal. imaging. 40, 2606-26012 (2015).
- Kocinaj D, Cioppa A, Ambrosini G et al. Radiation dose exposure during cardiac and peripheral arteries catheterisation. Int. J. Cardiol. 113, 283-284 (2006).
- Maccia C, Malchair F, Gobert I et al. Assessment of Local Dose Reference Values for Recanalization of Chronic Total Occlusions and Other Occlusions in a High-Volume Catheterization Center. Am. J. Cardiol. 116, 1179-1184 (2015).
- Fazel R, Curtis J, Wang Y et al. Determinants of fluoroscopy time for invasive coronary angiography and percutaneous coronary intervention: insights from the NCDR(®). Catheter. Cardiovasc. Interv. 82, 1091-1105 (2013).
- Ingwersen M, Drabik A, Kulka U et al. Physicians’ radiation exposure in the catheterization lab: does the type of procedure matter? JACC. Cardiovasc. Interv. 6, 1095-1102 (2013).
- Steinvil A, Aviram G, Konigstein M. Radiation dose of patients undergoing transcatheter aortic valve implantation: A comparison between edwards SAPIEN XT and medtronic corevalve aortic valve prostheses. Catheterization and Cardiovascular Interventions. (2013).
- de Ruiter QM, Moll FL, Gijsberts CM. AlluraClarity Radiation Dose-Reduction Technology in the Hybrid Operating Room During Endovascular Aneurysm Repair. Journal of endovascular therapy : an official journal of the International Society of Endovascular Specialists. 23, 130- 138 (2016).
- Cushman D, Flis A, Jensen B. The Effect of Body Mass Index on Fluoroscopic Time and Radiation Dose During Sacroiliac Joint Injections. PM & R : The journal of injury, function, and rehabilitation (2015).
- Shin RH, Cabrera FJ, Nguyen G. Radiation Dosimetry for Ureteroscopy Patients: A Phantom Study Comparing the Standard and Obese Patient Models. Journal of endourology / Endourological Society. 30, 57-62 (2016).
- Agarwal S, Parashar A, Bajaj NS. et al. Relationship of beam angulation and radiation exposure in the cardiac catheterization laboratory. JACC. Cardiovasc. Interv. 7, 558-566 (2014).
- Plourde G, Pancholy SB, Nolan J et al. Radiation exposure in relation to the arterial access site used for diagnostic coronary angiography and percutaneous coronary intervention: a systematic review and metaanalysis. Lancet. 386, 2192-2203 (2015).
- Rigatelli G, Panin S, Fiorrevanti R. Impact of Operators’ Height on Individual Radiation Exposure Measurements During Catheter- Based Cardiovascular Interventions. Journal of interventional cardiology. (2016).
- Kuefner MA, Brand M, Engert C et al. Radiation Induced DNA Double-Strand Breaks in Radiology. Rofo. 187, 872-878 (2015).
- Andreassi MG, Foffa I, Manfredi S et al. Genetic polymorphisms in XRCC1, OGG1, APE1 and XRCC3 DNA repair genes, ionizing radiation exposure and chromosomal DNA damage in interventional cardiologists. Mutation. research. 666, 57-63 (2009).
- Andreassi MG, Cioppa A, Botto N Somatic DNA damage in interventional cardiologists: a case-control study. FASEB journal : Official publication of the Federation of American Societies for Experimental Biology 19, 998-999 (2005).
- Andreassi MG, Piccaluga E, Gargani L. Subclinical carotid atherosclerosis and early vascular aging from long-term lowdose ionizing radiation exposure: a genetic, telomere, and vascular ultrasound study in cardiac catheterization laboratory staff. JACC Cardiovascular interventions. 8, 616-627 (2015).
- Wild P, Gauron C, Champion K. Effects of chronic low-dose exposure to ionizing radiation on physician microvascular structure revealed by nail fold capillaroscopy. Radiation and environmental biophysics (2015).
- Vano E, Fernandez JM, Resel LE et al. Staff lens doses in interventional urology. A comparison with interventional radiology, cardiology and vascular surgery values. Journal of radiological protection : Official journal of the Society for Radiological Protection. 36, 37-48 (2015).
- Jacob S, Boveda S, Bar O et al. Interventional cardiologists and risk of radiation-induced cataract: results of a French multicenter observational study. Int. J. Cardiol. 167, 1843- 1847 (2013).
- Seals KF, Lee EW, Cagnon CH et al. Radiation- Induced Cataractogenesis: A Critical Literature Review for the Interventional Radiologist. Cardiovascular and interventional radiology (2015).
- Roguin A, Goldstein J, Bar O. Brain tumours among interventional cardiologists: a cause for alarm? Report of four new cases from two cities and a review of the literature. EuroIntervention. 7, 1081-1086 (2012).
- Roguin A, Goldstein J, Bar O et al. Brain and neck tumors among physicians performing interventional procedures. Am. J. Cardiol. 111, 1368-1372 (2013).
- Venneri L, Rossi F, Botto N et al. Cancer risk from professional exposure in staff working in cardiac catheterization laboratory: insights from the National Research Council’s Biological Effects of Ionizing Radiation VII Report. Am. Heart. J. 157, 118-124 (2009).
- Durán A, Hian SK, Miller DL et al. Recommendations for occupational radiation protection in interventional cardiology. Catheterization and Cardiovascular Interventions. 82, 29-42 (2013).
- Heidbuchel H, Wittkampf FH, Vano E. Practical ways to reduce radiation dose for patients and staff during device implantations and electrophysiological procedures. Europace : European pacing, arrhythmias, and cardiac electrophysiology : journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 16, 946-964 (2014).
- Fazel R, Gerber TC, Balter S et al. Approaches to enhancing radiation safety in cardiovascular imaging: a scientific statement from the American Heart Association. Circulation.130: 1730-1748 (2014).
- Ketteler ER, Brown KR Radiation exposure in endovascular procedures. J. Vasc. Surg. 53, 35S-38S (2011).
- Amis ES Jr, Butler PF, Applegate KE et al. American College of Radiology white paper on radiation dose in medicine. J. Am. Coll. Radiol. 4, 272-284 (2007).
- Stecker MS, Balter S, Towbin RB et al. Guidelines for patient radiation dose management. J. Vasc. Interv. Radiol. 20, 263-273 (2009).
- Kuon E, Weitmann K, Hoffmann W et al. Efficacy of a minicourse in radiation-reducing techniques in invasive cardiology: a multicenter field study. JACC. Cardiovasc. Interv. 7, 382- 390 (2014).
- Georges JL, Livarek B, Gibault-Genty G. Reduction of radiation delivered to patients undergoing invasive coronary procedures. Effect of a programme for dose reduction based on radiation-protection training. Arch. Cardiovasc. Dis. 102, 821-827 (2009).
- Lakkireddy D, Nadzam G, Verma A Impact of a comprehensive safety program on radiation exposure during catheter ablation of atrial fibrillation:a prospective study. J Interv Card Electrophysiol. 24, 105-112 (2008).
- Gendelberg D, Hennrikus W, Slough J et al. A Radiation Safety Training Program Results in Reduced Radiation Exposure for Orthopaedic Residents Using the Mini C-arm. Clin. Orthop. Relat. Res. 474, 580-584 (2016).
- Weld LR, Nwoye UO, Knight RB. Safety, minimization, and awareness radiation training reduces fluoroscopy time during unilateral ureteroscopy.Urology. 84, 520-525 (2014).
- Kuon E, Weitmann K, Hoffmann W et al. Multicenter long-term validation of a minicourse in radiation-reducing techniques in the catheterization laboratory. Am J Cardiol. 115, 367-373 (2015).
- Kim C, Vasaiwala S, Haque F et al. Radiation safety among cardiology fellows. Am. J. Cardiol. 106, 125-128 (2010).
- Bordoli SJ, Carsten CG 3rd, Cull DL et al. Radiation safety education in vascular surgery training. J. Vasc. Surg. 59, 860-864 (2014).
- Heilmaier C, Kara L, Zuber N et al. Combined Use of a Patient Dose Monitoring System and a Real-Time Occupational Dose Monitoring System for Fluoroscopically Guided Interventions. J. Vasc. Interv. Radiol. (2015).
- Christopoulos G, Papayannis AC, Alomar M. Effect of a real-time radiation monitoring device on operator radiation exposure during cardiaccatheterization: the radiation reduction during cardiac catheterization using real-time monitoring study. Circulation. Cardiovascular. interventions. 7, 744-750 (2014).
- Kicken PJ, Bos AJ Effectiveness of lead aprons in vascular radiology: results of clinical measurements. Radiology. 197, 473-478 (1995).
- Mori H, Koshida K, Ishigamori O et al. Evaluation of the effectiveness of X-ray protective aprons in experimental and practical fields. Radiol. Phys. Technol. 7, 158-166 (2014).
- Klein LW, Tra Y, Garratt KN. Occupational health hazards of interventional cardiologists in the current decade. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac. Angiography.
- Interventions. 86, 913-924 (2015). 46. Moore B, vanSonnenberg E, Casola G et al. The relationship between back pain and lead apron use in radiologists. AJR. Am. J. Roentgenol. 158, 191-193 (1992).
- Ross AM, Segal J, Borenstein D. Prevalence of spinal disc disease among interventional cardiologists. Am. J. Cardiol. 79, 68-70 (1997).
- McCaffrey JP, Tessier F, Shen H. Radiation shielding materials and radiation scatter effects for interventional radiology (IR) physicians. Med. Phys. 39, 4537-4546 (2012).
- Kazempour M, Saeedimoghadam M, Shekoohi Shooli F et al. Assessment of the Radiation Attenuation Properties of Several Lead Free Composites by Monte Carlo Simulation. J. Biomed. Phys. Eng. 5, 67-76 (2015).
- Albayati MA, Kelly S, Gallagher D. Editor’s choice--Angulation of the Carm during complex endovascular aortic procedures increases radiationexposure to the head. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery 49, 396-402 (2015).
- Martin CJ. Personal dosimetry for interventional operators: when and how should monitoring be done? Br. J. Radiol. 84: 639-648 (2011).
- Butter C, Schau T, Meyhoefer J et al. Radiation Exposure of Patient and Physician during Implantation andUpgrade of Cardiac Resynchronization Devices. Pacing and Clinical Electrophysiology. (2010).
- Kuon E, Birkel J, Schmitt M et al. Radiation exposure benefit of a lead cap in invasive cardiology. Heart 89, 1205-1210 (2003).
- Reeves RR, Ang L, Bahadorani J. Invasive Cardiologists Are Exposed to Greater Left Sided Cranial Radiation: The BRAIN Study (Brain RadiationExposure and Attenuation During Invasive Cardiology Procedures). JACC Cardiovascular interventions. 8, 1197-1206 (2015).
- Uthoff H, Benenati MJ, Katzen BT Lightweight bilayer barium sulfatebismuth oxide composite thyroid collars for superior radiation protection influoroscopy-guided interventions: a prospective randomized controlled trial. Radiology. 270, 601-606 (2014).
- Alazzoni A, Gordon CL, Syed J Randomized Controlled Trial of Radiation Protection With a Patient Lead Shield and a Novel, Nonlead Surgical Cap forOperators Performing Coronary Angiography or Intervention.
- Circulation Cardiovascular interventions (2015). 57. Sans Merce M, Korchi AM, Kobzeva L et al. The value of protective head cap and glasses in neurointerventional radiology. J. Neurointerv Surg. (2015).
- Thornton RH, Dauer LT, Altamirano JP et al et al. (2010) Comparing strategies for operator eye protection in the interventional radiology suite. J. Vasc. Interv. Radiol. 21, 1703-1707 (2015).
- Kloeze C, Klompenhouwer EG, Brands PJ et al. Editor’s choice--Use of disposable radiationabsorbing surgicaldrapes results in significant dose reduction during EVAR procedures. European journal of vascular and endovascular surgery : the official journalf the European Society for Vascular Surgery. 47, 268-272 (2014).
- Sharma D, Ramsewak A, Manoharan G et al. Efficacy of RADPAD® protection drape in reducing radiation exposure to the primary operator during Transcatheter Aortic Valve Implantation (TAVI). Minerva. Cardioangiol. (2015).
- Lange HW, von Boetticher H. Reduction of operator radiation dose by a pelvic lead shield during cardiac catheterization by radial access: comparison with femoral access. JACC. Cardiovasc. Interv. 5, 445-449 (2012).
- Murphy JC, Darragh K, Walsh SJ et al. Efficacy of the RADPAD protective drape during real world complex percutaneous coronaryintervention procedures. The American journal of cardiology. 108, 1408-1410 (2011).
- Politi L, Biondi-Zoccai G, Nocetti L Reduction of scatter radiation during transradial percutaneous coronary angiography: a randomized trial using a lead-free radiation shield. Catheterization and cardiovascular interventions: official journal of the Society for Cardiac Angiography & Interventions. 79, 97- 102 (2012).
- Maeder M, Brunner-La Rocca HP, Wolber T. Impact of a lead glass screen on scatter radiation to eyes and hands in interventional cardiologists.Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions. 67, 18-23 (2006).
- Fetterly KA, Magnuson DJ, Tannahill GM et al. Effective use of radiation shields to minimize operator dose during invasive cardiology procedures. JACC Cardiovasc Interv. 4, 1133- 1139 (2011).
- Gilligan P, Lynch J, Eder H. Assessment of clinical occupational dose reduction effect of a new interventional cardiology shield for radial accesscombined with a scatter reducing drape. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography &Interventions. 86, 935- 940 (2015).
- Fattal P, Goldstein JA. A novel complete radiation protection system eliminates physician radiation exposure and leaded aprons. Catheterizationand cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions. 82, 11-16 (2013).
- Muniraj T, Aslanian HR, Laine L et al. A double-blind, randomized, sham-controlled trial of the effect of a radiation-attenuating drape on radiation exposure to endoscopy staff during ERCP. Am. J. Gastroenterol. 110, 690- 696 (2015).
- Chambers CE, Fetterly KA, Holzer R. et al. Radiation safety program for the cardiac catheterization laboratory. Catheter Cardiovasc Interv. 77, 546-556 (2011).
- Walters TE, Kistler PM, Morton JB et al. Impact of collimation on radiation exposure during interventional electrophysiology. Europace : European pacing, arrhythmias, and cardiac electrophysiology : journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 14, 1670-1673 (2012).
- Miraglia R, Maruzzelli L, Cortis K. Radiation Exposure in Transjugular Intrahepatic Portosystemic Shunt Creation. Cardiovascular andinterventional radiology (2015).
- Gailloud P. A large display is a powerful tool to reduce radiation exposure during single-plane fluoroscopically guided procedures. AJR Am J Roentgenol. 204, W483-485 (2015).
- Sharma D, Ramsewak A, O’Conaire S et al. (2015) Reducing radiation exposure during transcatheter aortic valve implantation (TAVI). Catheter Cardiovasc Interv. 85, 1256-1261.
- Abdelaal E, Plourde G, MacHaalany J et al. Effectiveness of low rate fluoroscopy at reducing operator and patient radiation dose during transradial coronary angiography and interventions. JACC Cardiovasc Interv. 7, 567- 574 (2014).
- Wassef AW, Hiebert B, Ravandi A et al. Radiation dose reduction in the cardiac catheterization laboratory utilizing a novel protocol. JACC Cardiovasc Interv. 7, 550-557 (2014).
- Bracken JA, Mauti M, Kim MS et al. A Radiation Dose Reduction Technology to Improve Patient Safety During CardiacCatheterization Interventions. Journal of interventional cardiology. 28, 493-497 (2015).
- Wen X, Jiang X, Li R, Zhang J, Yang P, Shen B, et al. (2015) Novel X-Ray Imaging Technology Allows Substantial Patient Radiation Reduction without Image Quality Impairment in Repetitive Transarterial Chemoembolization for Hepatocellular Carcinoma. Academic radiology 22: 1361-1367.
- Miraglia R, Maruzzelli L, Cortis K. Digital subtraction angiography during transjugular intrahepatic portosystemic shunt creation or revision: data on radiation exposure and image quality obtained using a standard and a lowdose acquisition protocol in a flat-panel detectorbased system. Abdominalimaging. 40, 1808- 1812 (2015).
- van den Haak RF, Hamans BC, Zuurmond K et al. Significant Radiation Dose Reduction in the Hybrid Operating Room Using aNovel X-ray Imaging Technology. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 50, 480-486 (2015).
- Chang DH, Hiss S, Mueller D et al. Radiation Dose Reduction in Computed Tomography- Guided Lung Interventions using an Iterative Reconstruction Technique. Rofo. 187, 906-914 (2015).
- Empen K, Kuon E, Hummel A, et al. Comparison of rotational with conventional coronary angiography. Am Heart J. 160, 552- 563 (2010).
- Bonatti J, Vetrovec G, Riga C et al. Robotic technology in cardiovascular medicine. Nat. Rev. Cardiol. 11, 266-275 (2014).
- Mahmud E, Schmid F, Kalmar P et al. RAPID (Robotic-Assisted Peripheral Intervention for peripheral arterialDisease) Study. Journal of the American College of Cardiology (2015).
- Duran C, Lumsden AB, Bismuth J. A randomized, controlled animal trial demonstrating the feasibility and safety of the Magellan endovascular roboticsystem. Annals of vascular surgery. 28, 470-478 (2014).
- Dominguez A, Reeves RR, Bahadorani J et al. TCT-148 Feasibility of Complex Robotic Percutaneous Coronary Intervention. Journal of the American College of Cardiology (2014).