Research Article - Diabetes Management (2017) Volume 7, Issue 5
Prevalence of controlled and uncontrolled diabetes mellitus and associated factors of controlled diabetes among diabetic adults in the hohoe municipality of Ghana
- *Corresponding Author:
- Kweku M
Department of Epidemiology and Biostatistics
School of Public Health
University of Health and Allied Sciences
Ho, Ghana
E-mail: ebeyang@yahoo.gh
Abstract
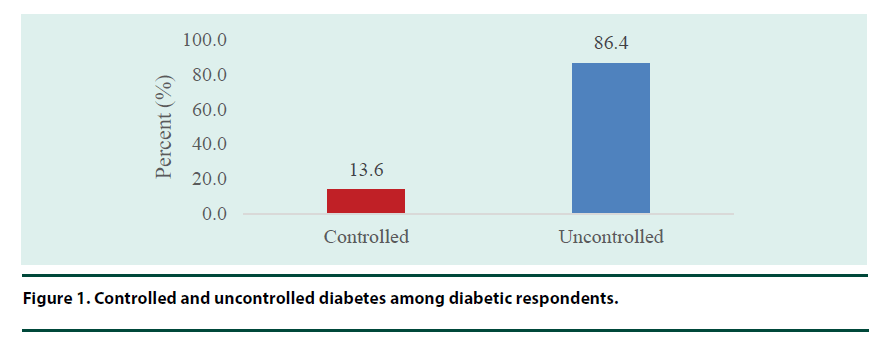
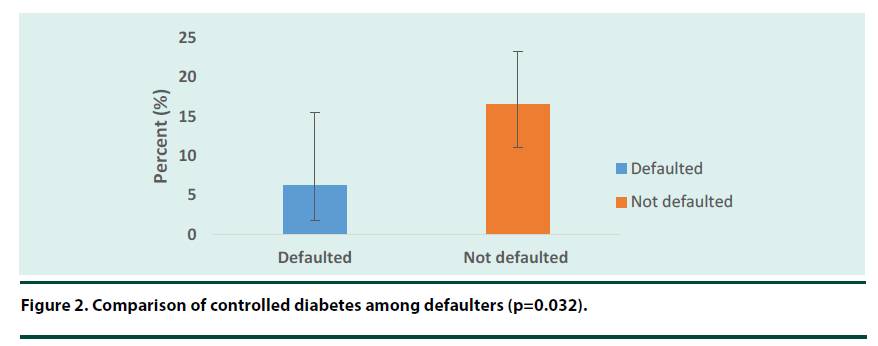
Background: When diabetes is uncontrolled, it has dire consequences on the health and well-being. Diabetes of all types can lead to numerous long-term complications in many parts of the body and can increase the overall risk of dying prematurely. Methods: A hospital-based cross-sectional survey that involved adults aged 18 years and above with diabetes and were attending the diabetic clinic at the Hohoe Municipal hospital in May and June 2017. Pre-tested semi-structured questionnaires were used to collect data. Blood Pressure, Blood glucose level and information on the last visit to the clinic were extracted from the diabetes card. Means were compared using t-test. Chi-square was used to determine the associations between type 2 diabetes and socio-demographic characteristics. Binary logistic regression was used to determine the strength of the associations between type 2 diabetes and some lifestyle risk factors. A p-value less than 0.05 was considered statistically significant. Results: The prevalence of controlled type 2 diabetes was 13.6%, and 86.4% of diabetics could not control their blood glucose level. There was a significant association between age, occupation, hypertension status, defaulter rate and control of diabetes (χ2=6.65, p=0.038), (χ2=12.43, p=0.014), (χ2=4.07, p=0.044) and (χ2=3.98, p=0.046) respectively. Of the 63 respondents who defaulted, only 6.3% were able to control their blood glucose level as compared to 16.6% of the 131 respondents who did not default (p=0.032). Respondents who were civil servants were 84% times less likely to have their blood glucose controlled as compared to those who were unemployed (AOR=0.16, p=0.031). Respondents with high socioeconomic status were 5.55 times more likely to have their blood glucose controlled as compared to those with low socioeconomic status (AOR=5.55, p=0.010). Conclusion: Only fourteen out of 100 adults with diabetes were able to control their blood glucose level. Civil servants and defaulters were less likely to control their blood glucose level. Diabetics with high socioeconomic status were more likely to control their blood glucose level. Health workers at the diabetic clinic should intensify education and counselling of diabetics. Intensified public education on diabetes and its management should be provided by nutrition and health promotion officers in the Hohoe Municipality.
Keywords
diabetes mellitus adults, controlled, uncontrolled, hohoe municipality, Ghana
Abbreviations
WHO: World Health Organization, BP: Blood Pressure, FBG: Fasting Blood Glucose, DM: Diabetes Mellitus, DM 2: Diabetes Mellitus Type 2, HDL-C: High Density Lipoprotein Cholesterol, HMH: Hohoe Municipal Hospital, GHS: Ghana Health Service, ERC: Ethics Review Committee, GHS-ERC: Ghana Health Service-Ethics Review Committee, BP: Blood Pressure, MoH: Ministry of Health, JHS: Junior High school, SHS: Senior High School, SES: Socio-Economic Status, SPH: School of Public Health, UHAS: University of Health and Allied Sciences, BMI: Body Mass Index, WC: Waist Circumference, CHPS: Community-based Health Planning and Services
Introduction
Diabetes Mellitus (DM) is a serious, chronic disease that occurs either when the pancreas does not produce enough insulin (a hormone that regulates blood glucose) (Type 1 Diabetes), or when the body cannot effectively use the insulin it produces (Type 2 Diabetes) (DM2) leading to symptoms such as frequent urination, lethargy, excessive thirst and hunger [1].
Globally, an estimated 422 million adults were living with diabetes in 2014, compared to 108 million in 1980. The global prevalence (age-standardized) of diabetes has nearly doubled since 1980, rising from 4.7% to 8.5% in the adult population in 2014 [2]. In sub- Saharan Africa (SSA), the challenge posed by diabetes is even more overwhelming since diabetes will have to share scarce resources with infections and malnutrition [3]. By the year 2030, over 85% of the world’s diabetics will be living in the developing countries, affecting about 400 million people [4,5]. Diabetes caused 1.5 million deaths in 2012. Higher-than-optimal blood glucose caused an additional 2.2 million deaths, by increasing the risks of cardiovascular and other diseases. Forty-three percent of these 3.7 million deaths occur before the age of 70 years. The percentage of deaths attributable to diabetes that occurs prior to age 70 is higher in low and middle-income countries than in high-income countries. Over 80% of people with DM2 are overweight and obese [6]. Patients suffering from DM2 usually control their blood glucose by controlling their diet, carrying out regular exercises and possibly by taking drugs and or insulin injections [2,6].
Diabetes of all types can lead to numerous long-term complications in many parts of the body and can increase the overall risk of dying prematurely. Possible complications include heart attack, stroke, kidney failure, leg amputation, vision loss and neuropathy. Besides these complications, glaucoma and cataracts, foot problems, skin infections, infections in the urinary tract and the female genital tract and erection problems are also common in diabetics [2,7,8].
Studies have been conducted to determine the possible risk factors of uncontrolled diabetes among diabetics. A study conducted among diabetes patients in Pakistan revealed that 76% of them had a raised blood glucose level, which was labelled uncontrolled diabetes. Obesity, exercise, a family history of diabetes and hypertension were significantly increased in patients having blood glucose levels more than the reference range despite having regular medication [9]. Another study conducted in Vermont, Northern New York revealed that 57% of the diabetics were able to control the blood glucose level [10]. A study conducted in Ambo hospital, Ethiopia revealed that patients aged 41-50 years (p=0.038) and 61-70 years (p=.017) poorly managed their blood glucose levels compared to the other age groups. The study also found that Diabetics who had hyperlipidemia and peripheral neuropathy as comorbidities were 5 and 579 times more prone to having poor blood glucose control as compared to patients with no comorbidities (AOR=5, p=0.032) and (AOR=579, p=0.045) respectively [11].
A study conducted in Thiruchirappalli district revealed that adults with DM2 monitored their blood and urine glucose only when the complications arise. And this shows that they were under a poor control of blood glucose level, which gives rise to many complications which can be life threatening [12]. Another study conducted in the urban district of Karachi, Pakistan revealed that 38.9% had uncontrolled diabetes. Age <50 years, being diagnosed in a hospital, diabetes information from a doctor or nurse only, higher monthly treatment cost and higher consumption of tea were independently associated with uncontrolled diabetes among diabetics [13].
Females, long standing DM2, cigarette smoking, total hypercholesterolemia, elevated high-density lipoprotein cholesterol (HDL-C), high blood glucose and underweight were identified as independent risk factors of poorly controlled of blood glucose [14].
A study done in Almadinah diabetic center revealed that 76.4% of the diabetics could not control their blood glucose level. Respondents with poor blood glucose were significantly associated with a family history of diabetes, duration of DM2, diabetes management and complications [15]. A study conducted in Kerman, Iran revealed that only 31.7% of men and 26.0% of women had controlled the level of blood glucose. In that same study, results showed that long duration of disease and higher Waist Circumference (WC) were positively associated with uncontrolled diabetes status [16].
Even though there is a diabetic clinic at the Hohoe Municipal Hospital (HMH) and diabetics are undergoing counselling, management such as medication and insulin injections, advice on healthy eating, exercise and regular blood glucose testing, a recent study revealed that there is high uncontrolled blood glucose among diabetics. The current study assessed the prevalence of controlled and uncontrolled diabetes and associated factors influencing controlled diabetes among diabetic adults attending the diabetes clinic in Hohoe Municipality.
Materials and Methods
▪ Study area
Hohoe Municipality is one of the 25 administrative Districts/Municipalities in the Volta Region of Ghana. The Municipality has a total land surface area of 1,172 km square, which is 5.6% of the regional and 0.05% of the National land surface area. It is located at longitude 0 degrees 15 East and 0 degrees 45 East and latitude 6 degrees 45 North and 7 degrees 15 North and lies almost in the heart of the Volta Region. It shares boundary to the East with Togo, forming part of the International borders, on the Southeast by the Afadzato District, the Southwest with Kpando Municipal, on the Northeast with Jasikan District and on the Northwest with Biakoye District. According to the 2010 population census, the Municipality had a total population of 167,016 inhabitants, representing 7.9% of the total population of the Volta Region. The major ethnic groups in the Municipality are the Ewes, Lolobis, Sankrokofis and Likpes. Some economic activities engaged by the people in the Municipality include agriculture, petty trading, construction and the formal sector. There are 21 health facilities including a hospital located at Hohoe, 14 health centres and 7 community-based health planning and services (CHPS) compounds. The hospital has a 178-bed capacity, serving as the referral point for the health centres within and outside the Municipality. A diabetic clinic was established at the hospital in 2011 and provides services to patients twice a week.
▪ Study population
The study population was adults aged 18 years and above residing in the Hohoe Municipality.
▪ Inclusion criteria
Adults with diabetes, residing in the Hohoe Municipality, who were attending the diabetic clinic at the Hohoe Municipal hospital and consented to participate in the study were included.
▪ Exclusion criteria
Adults with diabetes but seriously ill, requiring hospital admission, attending the diabetic clinic for the first time; pregnant women; not residing in the Hohoe Municipality and did not consent to participate in the study were excluded.
▪ Study design
The study was a hospital-based crosssectional survey that involved adults aged 18 years and above, who were diabetics and were attending the diabetic clinic at the Hohoe Municipal hospital in May and June 2017. Pre-tested semi-structured questionnaires were used to collect data. Blood Pressure (BP), Blood glucose level results and information on the last visit to the clinic were extracted from the diabetes card.
▪ Sample size determination
The sample size required to be representative of the study population was calculated using a sample size calculation formula [17]. The reliability coefficient (z score) of 1.96 at 95% confidence level, the margin of error of 5% and a proportion of 21% [16] were entered into the formula to determine a minimum sample size of 211. Adjusting for a nonresponse rate of 4 % gives the total sample size of 219.44≈220.
▪ Sampling method
A simple random sampling technique was used in this study. A list of all diabetics who visited the hospital on each clinic day was created. Thus, simple random sampling (lottery) was used to select the required number of respondents on each day the researcher visited the clinic. Serial numbers were assigned to all the patients who had gathered at the clinic. The serial numbers were written on pieces of paper, which were neatly folded and placed in a bowl. One of the data collectors was blind folded and asked to pick the folded pieces of paper from the bowl repeatedly at random till the required number of diabetic patients was realized for each session. This procedure was repeated until all the 220 respondents were selected.
▪ Data collection
Data were collected with reference to the WHO STEPWISE approach for non-communicable disease surveillance (Diabetes Mellitus) on risk factors assessment with particular emphasis on step 3. STEP 1 was used to capture information associated with nutritional habit, sedentary lifestyle, socio-demographic characteristics and many others with the use of a questionnaire, which was administered through a face-to-face interview. STEP 2 was used to collect information on weight, height, waist-to-hip ratio, blood pressure level and BMI (this was carried out with the use of tools such as an electronic weighing scale, Stadiometer, tape measure and digital blood pressure monitor) including STEP 1. STEP 3 was used to collect finger-prick blood samples by the clinic staff, which were used to measure the level of fasting blood glucose using a digital Glucometer (OneTouch Ultra Easy blood glucose monitoring system, (LifeScan Johnson & Johnson company New Jersey- USA).
Anthropometric measurements
Heights of respondents were measured with a Stadiometer (SECA Leicester height measure with a fixed foot plate and movable headboard made in the United Kingdom) to the nearest 0.1 centimetres. Weight was measured with digital weighing scale (Bed and Bath room model BB-3018A manufactured by Conair Company based in the USA) with respondents dressed in light clothing to the nearest 0.1 kilogrammes. All anthropometric measurements were taken in triplicates and in accordance with the WHO standard anthropometry guidelines.
Measurement of Blood Pressure
Blood pressure (BP) of respondents was measured with the aid of a digital blood pressure monitor (Omron M2 Basic manufactured in India by Omron Company). Respondents were made to rest for at least 10 minutes before their BP was measured and this was done 3 times at 2 minutes intervals by clinic nurses.
Classifications of blood glucose and blood pressure
Classifications of blood glucose levels were done using the cut-off standard point of American Diabetes Association.
Fasting Blood Glucose Levels (FBS): Diabetes diagnosed at fasting blood glucose of ≥ 126 mg/dl or FBS <7.0 mmol/L. Fasting means not having anything to eat or drink (except water) for at least 8 hours before the test).
Classification of diabetes
Diabetes was classified based on the recommended cut-offs [2] as follows:
Normal (FBS <6.0 mmol/dl); Pre-diabetic (FBS=6.1-6.9 mmol/dl); Diabetic (FBS ≥ 7.0 mmol/dl).
Classification of hypertension
Hypertension was classified based on recommended cut-offs [2] as follows:
Normal (Systolic BP <120 and Diastolic BP <80 mmHg);
Pre-hypertension (Systolic BP=120-139 and/ or Diastolic BP=80-89 mmHg);
Hypertension- Stage I hypertension (Systolic BP=140-159 and/or Diastolic BP=90-99 mmHg) and Stage II hypertension (Systolic BP >160 and/or Diastolic BP >100 mmHg).
Data Management and Analysis
Data from the field were checked for completeness and accuracy and entered using EpiData version 3.1 statistical software and later exported to STATA version 14.1 for analysis. Descriptive statistics such as frequency distribution, proportion and percentages were used to describe qualitative variables. Chi-square was used to determine the associations between DM2 (dependent) and demographic characteristics and some life style risk factors (independent). Binary logistic regression was used to test the strength of the associations between the dependent and independent variable. A p-value less than 0.05 was considered statistically significant.
Ethical Issues
Before the commencement of the study, approval was obtained from the Ghana Health Service (GHS)/ Ministry of Health (MoH) Ethics Review Committee (ERC) MoH/GHS with approval number (GHS-ERC: 14/03/2017). Permission was sought from the Hohoe Municipal Hospital. A written informed consent was obtained from all respondents. In addition, respondents were informed that participation in the study was entirely voluntary and that they had the right to withdraw from the study and were assured that should they decide not to participate, it would not affect their future access to hospital services in any way.
Results
Table 1 shows a total of 220 adults aged 18 years and above with a mean age of 60.59 ± 11.8 years. The majority, 55.9% of the respondents were females. Most, 49.1% had Junior High school (JHS) level of education, and most, 35.9% were traders. More than half, 55% of the respondents were Married/ Co-habiting. The majority, 94.1% of the respondents were Christians and most, 51.8% had a low socioeconomic status.
| Variable | Frequency [N=220] | Percentage [%] |
|---|---|---|
| Mean age (in years) (SD) | 60.59 (11.8) | |
| Age group (years) | ||
| <50 | 35 | 15.9 |
| 50-59 | 48 | 21.8 |
| 60 and above | 137 | 62.3 |
| Sex | ||
| Male | 53 | 24.1 |
| Female | 167 | 75.9 |
| Educational level | ||
| No formal education | 24 | 10.9 |
| Primary | 21 | 9.6 |
| JHS | 108 | 49.1 |
| SHS | 31 | 14.0 |
| Tertiary | 36 | 16.4 |
| Occupation | ||
| Unemployed | 41 | 18.6 |
| Farmer | 42 | 19.1 |
| Trading | 79 | 35.9 |
| Artisan | 26 | 11.8 |
| Civil Servant | 32 | 14.6 |
| Marital Status | ||
| Single | 15 | 6.8 |
| Married/Co-habiting | 121 | 55.0 |
| Divorced | 26 | 11.8 |
| Widowed | 58 | 26.4 |
| Religion | ||
| Christian | 207 | 94.1 |
| Muslim | 13 | 5.9 |
| Socio-Economic Status | ||
| Low | 114 | 51.8 |
| High | 106 | 48.2 |
Table 1. Socio-demographic characteristics of respondents.
▪ Prevalence of controlled and uncontrolled diabetes
Figure 1 shows that only 30 (13.6 %) of the respondents had their blood sugar under control at the time of the survey. Of the 63 respondents who defaulted, only 6.3% were able to control their blood glucose level as compared to 16.6% of the 131 respondents who did not default (p=0.032 (Figure 2).
Figure 1. Controlled and uncontrolled diabetes among diabetic respondents.
Figure 2. Comparison of controlled diabetes among defaulters (p=0.032).
▪ Association between socio-demographic characteristics and Controlled diabetes
There was a significant association between age, occupation and controlled diabetes (χ2=6.65, p=0.038) and (χ2=12.43, p=0.014) respectively (Table 2). There was also a significant association between hypertension status, defaulter rate and controlled diabetes (χ2=4.07, p=0.044) and (χ2=3.98, p=0.046) respectively (Table 3).
| Variable | Controlled [30] |
Uncontrolled [190] |
Total [220] |
Chi-square | P-value |
|---|---|---|---|---|---|
| Age group (years) | |||||
| <50 | 2 (6.7) | 33 (17.4) | 35 (15.9) | ||
| 50-59 | 3 (10.0) | 45 (23.7) | 48 (21.8) | ||
| 60 and above | 25 (83.3) | 112 (58.9) | 137 (62.3) | 6.65 | 0.038 |
| Sex | |||||
| Male | 9 (30.0) | 44 (23.2) | 53 (24.1) | ||
| Female | 21 (70.0) | 146 (76.8) | 167 (75.9) | 0.66 | 0.415 |
| Educational level | |||||
| No formal education | 3 (10.0) | 21 (11.1) | 24 (10.9) | ||
| Primary | 3 (10.0) | 18 (9.4) | 21 (9.5) | ||
| JHS | 13 (43.4) | 95 (50.0) | 108 (49.1) | ||
| SHS | 4 (13.3) | 27 (14.2) | 31 (14.1) | ||
| Tertiary | 7 (23.3) | 29 (15.3) | 36 (16.4) | 1.31 | 0.859 |
| Occupation | |||||
| Unemployed | 10 (33.3) | 31 (16.3) | 41 (18.6) | ||
| Farmer | 10 (33.3) | 32 (16.9) | 42 (19.1) | ||
| Trading | 6 (20.0) | 73 (38.4) | 79 (35.9) | ||
| Artisan | 2 (6.7) | 24 (12.6) | 26 (11.8) | ||
| Civil Servant | 2 (6.7) | 30 (15.8) | 32 (14.6) | 12.43 | 0.014 |
| Marital Status | |||||
| Single | 1 (3.3) | 14 (7.4) | 15 (6.8) | ||
| Married/Co-habiting | 16 (53.3) | 105 (55.3) | 121 (55.0) | ||
| Divorced | 4 (13.3) | 22 (11.6) | 26 (11.8) | ||
| Widowed | 9 (30.1) | 49 (25.7) | 58 (26.4) | 0.88 | 0.831 |
| Religion | |||||
| Christian | 29 (96.7) | 178 (93.7) | 207 (94.1) | ||
| Muslim | 1 (3.3) | 12 (6.3) | 13 (5.9) | 0.41 | 0.520 |
| Socio-Economic Status | |||||
| Low | 11 (36.7) | 103 (54.2) | 114 (51.8) | ||
| High | 19 (63.3) | 87 (45.8) | 106 (48.2) | 3.19 | 0.074 |
Table 2. Association between socio-demographic characteristics and controlled diabetes.
| Variable | Controlled [30] |
Uncontrolled [190] |
Total [220] |
Chi-square | P-value |
|---|---|---|---|---|---|
| Smoking status | |||||
| Never smoke | 28 (93.3) | 184 (96.8) | 212 (96.4) | ||
| Current smoker/ Ex-smoker | 2 (6.7) | 6 (3.2) | 8 (3.6) | 0.91 | 0.340 |
| Drinking Status | |||||
| Never drink | 20 (66.7) | 117 (61.6) | 137 (62.3) | ||
| Current drinker | 3 (10.0) | 24 (12.6) | 27 (12.3) | ||
| Ex-drinker | 7 (23.3) | 49 (25.8) | 56 (25.4) | 0.32 | 0.854 |
| Fruit intake per week | |||||
| None | 6 (20.0) | 22 (11.6) | 28 (12.7) | ||
| One day | 7 (23.3) | 44 (23.2) | 51 (23.2) | ||
| Two days | 8 (26.7) | 43 (22.6) | 51 (23.2) | ||
| Three days | 5 (16.7) | 36 (18.9) | 41 (18.6) | ||
| Four and above | 4 (13.3) | 45 (23.7) | 49 (22.3) | 2.94 | 0.567 |
| Vegetable intake per week | |||||
| One day | 1 (3.3) | 10 (5.3) | 11 (5.0) | ||
| Two days | 1 (3.3) | 16 (8.4) | 17 (7.7) | ||
| Three days | 5 (16.7) | 18 (9.5) | 23 (10.5) | ||
| Four and above | 23 (76.7) | 146 (76.8) | 169 (76.8) | 2.34 | 0.504 |
| Physical activity per week | |||||
| No physical activity | 4 (13.3) | 18 (9.5) | 22 (10.0) | ||
| One day | 9 (30.0) | 41 (21.6) | 50 (22.7) | ||
| Two days | 2 (6.7) | 25 (13.2) | 27 (12.3) | ||
| Three days | 2 (6.7) | 20 (10.5) | 22 (10.0) | ||
| Four days and more | 13 (43.3) | 86 (45.3) | 99 (45.0) | 2.49 | 0.646 |
| Body Mass Index | |||||
| Normal | 10 (33.3) | 76 (40.0) | 86 (39.1) | ||
| Overweight | 11 (36.7) | 54 (28.4) | 65 (29.5) | ||
| Obese | 9 (30.0) | 60 (31.6) | 69 (31.4) | 0.911 | 0.634 |
| Salt Intake | |||||
| Low | 7 (23.3) | 64 (33.6) | 71 (32.3) | ||
| Moderate | 22 (73.4) | 109 (57.4) | 131 (59.5) | ||
| High | 1 (3.3) | 17 (9.0) | 18 (8.2) | 2.96 | 0.227 |
| Family History of Diabetes | |||||
| No | 9 (30.0) | 79 (41.6) | 88 (40.0) | ||
| Yes | 21 (70.0) | 111 (58.4) | 132 (60.0) | 1.45 | 0.229 |
| Hypertensive Status | |||||
| Normal | 5 (16.7) | 67 (35.3) | 72 (32.7) | ||
| Hypertensive | 25 (83.3) | 123 (64.7) | 148 (67.3) | 4.07 | 0.044 |
| Drug availability | |||||
| No | 7 (23.3) | 72 (37.9) | 79 (35.9) | ||
| Yes | 23 (76.7) | 118 (62.1) | 141 (64.1) | 2.38 | 0.122 |
| Take Drug | |||||
| No | 5 (16.7) | 49 (25.8) | 54 (24.6) | ||
| Yes | 25 (83.3) | 141 (74.2) | 166 (75.4) | 1.16 | 0.281 |
| Financial Support | |||||
| No | 21 (70.0) | 119 (62.6) | 140 (63.6) | ||
| Yes | 9 (30.0) | 71 (37.4) | 80 (36.4) | 0.61 | 0.436 |
| Default | |||||
| No | 26 (86.7) | 131 (68.9) | 157 (71.4) | ||
| Yes | 4 (13.3) | 59 (31.1) | 63 (28.6) | 3.98 | 0.046 |
| Complications of diabetes | |||||
| No | 18 (60.0) | 130 (68.4) | 148 (67.3) | ||
| Yes | 12 (40.0) | 60 (31.6) | 72 (32.7) | 0.83 | 0.361 |
| Dietary Diversity | |||||
| Adequate Nutrient | 22 (73.3) | 144 (75.8) | 166 (75.4) | ||
| Inadequate Nutrient | 8 (26.7) | 46 (24.2) | 54 (24.6) | 0.08 | 0.771 |
| Knowledge on Signs | |||||
| High | 5 (16.7) | 38 (20.0) | 43 (19.6) | ||
| Low | 25 (83.3) | 152 (80.0) | 177 (80.4) | 0.18 | 0.669 |
| Knowledge on Complications | |||||
| High | 1 (3.3) | 9 (4.7) | 10 (4.6) | ||
| Low | 29 (96.7) | 181 (95.3) | 210 (95.4) | 0.12 | 0.732 |
Table 3. Association between lifestyles characteristics and controlled diabetes.
▪ Association between socio-demographic, life style characteristics and the odds of controlled diabetes
Table 4 shows a statistically significant association between occupation and control of diabetes. Traders and civil servants were 80% and 87% times less likely to have their blood glucose controlled as compared to those who were unemployed [AOR=0.20 (95% CI: 0.05, 0.89), p= 0.036] and [AOR=0.13 (95% CI: 0.22, 0.72), p=0.019] respectively. Respondents with a high socioeconomic status were 6.55 times more likely to have their blood glucose controlled as compared to those with a low socioeconomic status [AOR=6.55(95% CI: 1.66, 25.88), p=0.007]. Respondents with hypertension were 3.37 times more likely to have their blood glucose controlled as compared to those with a normal blood pressure [AOR=3.37 (95% CI: 1.08, 10.49), p=0.036. Even though not statistically significant, respondents who depended on other people for financial support and those who defaulted were 42% and 59% times less likely to have their blood glucose controlled as compared to those who were not depending on others and those who did not default [AOR=0.58 (95% CI: 0.22, 1.57), p=0.285] and [AOR=0.41 (95% CI: 0.12, 1.37), p=0.146] respectively.
| Variable | Controlled [n=30] |
Uncontrolled [n=190] |
Total [N=220] |
Chi-square (P-value) | COR (95% CI) P-value | AOR (95% CI) P-value |
|---|---|---|---|---|---|---|
| Age group (years) | ||||||
| <50 | 2 (6.7) | 33 (17.4) | 35 (15.9) | 6.65 (0.038) | ||
| 50-59 | 3 (10.0) | 45 (23.7) | 48 (21.8) | 1.1 (0.17, 6.96) 0.919 | ||
| 60 and above | 25 (83.3) | 112 (58.9) | 137 (62.3) | 3.68 (0.83, 16.36) 0.087 | ||
| Sex | ||||||
| Male | 9 (30.0) | 44 (23.2) | 53 (24.1) | 0.66 (0.415) | ||
| Female | 21 (70.0) | 146 (76.8) | 167 (75.9) | 0.70 (0.30, 1.64) 0.417 | ||
| Educational level | ||||||
| No formal education | 3 (10.0) | 21 (11.1) | 24 (10.9) | 1.31 (0.86) | ||
| Primary | 3 (10.0) | 18 (9.4) | 21 (9.5) | 1.16 ( 0.21, 6.51) 0.861 | 0.96 (0.14, 6.37) 0.962 | |
| JHS | 13 (43.4) | 95 (50.0) | 108 (49.1) | 0.96 (0.25, 3.66) 0.950 | 0.33 (0.06, 1.77) 0.196 | |
| SHS | 4 (13.3) | 27 (14.2) | 31 (14.1) | 1.04 (0.21, 5.14) 0.965 | 0.15 (0.02, 1.39) 0.095 | |
| Tertiary | 7 (23.3) | 29 (15.3) | 36 (16.4) | 1.69 (0.39, 7.30) 0.483 | 0.19 (0.02, 1.87) 0.156 | |
| Occupation | ||||||
| Unemployed | 10 (33.3) | 31 (16.3) | 41 (18.6) | 12.43 (0.014) | ||
| Farmer | 10 (33.3) | 32 (16.9) | 42 (19.1) | 0.96 (0.35, 2.65) 0.951 | 1.35 (0.39, 4.65) 0.635 | |
| Trading | 6 (20.0) | 73 (38.4) | 79 (35.9) | 0.25 (0.08, 0.76) 0.014 | 0.25 (0.06, 0.95) 0.042 | |
| Artisan | 2 (6.7) | 24 (12.6) | 26 (11.8) | 0.26 (0.05, 1.29) 0.099 | 0.21 (0.04, 1.31) 0.096 | |
| Civil Servant | 2 (6.7) | 30 (15.8) | 32 (14.6) | 0.21 (0.04, 1.02) 0.053 | 0.16 (0.03, 0.85) 0.031 | |
| Marital Status | ||||||
| Single | 1 (3.3) | 14 (7.4) | 15 (6.8) | 0.88(0.831) | ||
| Married/Co-habiting | 16 (53.3) | 105 (55.3) | 121 (55.0) | 2.13 (0.26, 17.34) 0.479 | ||
| Divorced | 4 (13.3) | 22 (11.6) | 26 (11.8) | 2.54 (0.25, 25.17) 0.424 | ||
| Widowed | 9 (30.1) | 49 (25.7) | 58 (26.4) | 2.57 (0.29, 22.06) 0.389 | ||
| Religion | ||||||
| Christian | 29 (96.7) | 178 (93.7) | 207 (94.1) | 0.41 (0.520) | ||
| Muslim | 1 (3.3) | 12 (6.3) | 13 (5.9) | 0.51 (0.06, 4.08) 0.527 | ||
| Socio-Economic Status (SES) | ||||||
| Low | 11 (36.7) | 103 (54.2) | 114 (51.8) | 3.19 (0.074) | ||
| High | 19 (63.3) | 87 (45.8) | 106 (48.2) | 2.04 (0.92, 4.53) 0.078 | 5.55 (1.49, 20.56) 0.010 | |
| Smoking status | ||||||
| Never smoke | 28 (93.3) | 184 (96.8) | 212 (96.4) | 0.91 (0.340) | ||
| Current smoker/ Ex-smoker | 2 (6.7) | 6 (3.2) | 8 (3.6) | 2.19 (0.42, 11.39) 0.351 | ||
| Drinking Status | ||||||
| Never drink | 20 (66.7) | 117 (61.6) | 137 (62.3) | 0.32 (0.854) | ||
| Current drinker | 3 (10.0) | 24 (12.6) | 27 (12.3) | 0.73 (0.20, 2.66) 0.635 | ||
| Ex-drinker | 7 (23.3) | 49 (25.8) | 56 (25.4) | 0.84 (0.33, 2.10) 0.703 | ||
| Fruit intake per week | ||||||
| None | 6 (20.0) | 22 (11.6) | 28 (12.7) | 2.94 (0.567) | ||
| One day | 7 (23.3) | 44 (23.2) | 51 (23.2) | 0.58 (0.17, 1.95) 0.380 | ||
| Two days | 8 (26.7) | 43 (22.6) | 51 (23.2) | 0.68 (0.21, 2.21) 0.542 | ||
| Three days | 5 (16.7) | 36 (18.9) | 41 (18.6) | 0.51 (0.13, 1.86) 0.309 | ||
| Four and above | 4 (13.3) | 45 (23.7) | 49 (22.3) | 0.33 (0.08, 1.27) 0.107 | ||
| Vegetable intake per week | ||||||
| One day | 1 (3.3) | 10 (5.3) | 11 (5.0) | 2.34 (0.504) | ||
| Two days | 1 (3.3) | 16 (8.4) | 17 (7.7) | 0.63 (0.05, 11.15) 0.749 | 1.59 (0.07, 35.77) 0.767 | |
| Three days | 5 (16.7) | 18 (9.5) | 23 (10.5) | 2.78 (0.28, 27.21) 0.380 | 7.89 (0.63, 99.72) 0.110 | |
| Four and above | 23 (76.7) | 146 (76.8) | 169 (76.8) | 1.57 (0.19, 12.89) 0.672 | 4.39 (0.43, 44.54) 0.211 | |
| Physical activity per week | ||||||
| No physical activity | 4 (13.3) | 18 (9.5) | 22 (10.0) | 2.49 (0.646) | ||
| One day | 9 (30.0) | 41 (21.6) | 50 (22.7) | 0.99 (0.26, 3.63) 0.985 | ||
| Two days | 2 (6.7) | 25 (13.2) | 27 (12.3) | 0.36 (0.05, 2.18) 0.267 | ||
| Three days | 2 (6.7) | 20 (10.5) | 22 (10.0) | 0.45 (0.07, 2.76) 0.388 | ||
| Four days and more | 13 (43.3) | 86 (45.3) | 99 (45.0) | 0.68 (0.19, 2.33) 0.539 | ||
| Body Mass Index (BMI) | ||||||
| Normal | 10 (33.3) | 76 (40.0) | 86 (39.1) | 0.911 (0.634) | ||
| Overweight | 11 (36.7) | 54 (28.4) | 65 (29.5) | 1.55 (0.61, 3.90) 0.354 | ||
| Obese | 9 (30.0) | 60 (31.6) | 69 (31.4) | 1.14 (0.43, 2.98) 0.790 | ||
| Salt Intake | ||||||
| Low | 7 (23.3) | 64 (33.6) | 71 (32.3) | 2.96 (0.227) | ||
| Moderate | 22 (73.4) | 109 (57.4) | 131 (59.5) | 0.18 (0.74, 4.56) 0.184 | ||
| High | 1 (3.3) | 17 (9.0) | 18 (8.2) | 0.54 (0.06, 4.67) 0.574 | ||
| Family History of Diabetes | ||||||
| No | 9 (30.0) | 79 (41.6) | 88 (40.0) | 1.45 (0.229) | ||
| Yes | 21 (70.0) | 111 (58.4) | 132 (60.0) | 1.67 (0.722, 3.82) 0.232 | ||
| Hypertension Status | ||||||
| Normal | 5 (16.7) | 67 (35.3) | 72 (32.7) | 4.07 (0.044) | ||
| Hypertensive | 25 (83.3) | 123 (64.7) | 148 (67.3) | 2.72 (0.99, 7.44) 0.051 | 2.47 (0.54, 7.23) 0.100 | |
| Drug availability | ||||||
| No | 7 (23.3) | 72 (37.9) | 79 (35.9) | 2.38 (0.122) | ||
| Yes | 23 (76.7) | 118 (62.1) | 141 (64.1) | 2.00 (0.82, 4.91) 0.128 | ||
| Take Drug | ||||||
| No | 5 (16.7) | 49 (25.8) | 54 (24.6) | 1.16 (0.281) | ||
| Yes | 25 (83.3) | 141 (74.2) | 166 (75.4) | 1.74 (0.63, 4.79) 0.285 | ||
| Financial Support | ||||||
| No | 21 (70.0) | 119 (62.6) | 140 (63.6) | 0.61 (0.436) | ||
| Yes | 9 (30.0) | 71 (37.4) | 80 (36.4) | 0.72 (0.31, 1.65) 0.437 | ||
| Default | ||||||
| No | 26 (86.7) | 131 (68.9) | 157 (71.4) | 3.98 (0.046) | ||
| Yes | 4 (13.3) | 59 (31.1) | 63 (28.6) | 0.34 (0.11, 1.02) 0.055 | ||
| Dietary Diversity | ||||||
| Adequate Nutrient | 22 (73.3) | 144 (75.8) | 166 (75.4) | 0.08 (0.771) | ||
| Inadequate Nutrient | 8 (26.7) | 46 (24.2) | 54 (24.6) | 1.14 (0.47, 2.73) 0.772 | 1.29 (0.48, 3.47) 0.611 | |
| Knowledge on Signs | ||||||
| High | 5 (16.7) | 38 (20.0) | 43 (19.6) | 0.18 (0.669) | ||
| Low | 25 (83.3) | 152 (80.0) | 177 (80.4) | 1.25 (0.44, 3.48) 0.669 | ||
| Knowledge on Complications | ||||||
| High | 1 (3.3) | 9 (4.7) | 10 (4.6) | 0.12 (0.732 | ||
| Low | 29 (96.7) | 181 (95.3) | 210 (95.4) | ) | 1.44 (0.18, 11.81) 0.733 | |
Table 4. Association between socio-demographic, life style characteristics and the odds of controlled diabetes.
Discussion
Diabetes of all types can lead to numerous long term complications in many parts of the body and reduces the life quality of the diabetic patient. This study assessed prevalence of controlled and uncontrolled diabetes and some risk factors associated with controlled diabetes among diabetic adults in the Hohoe Municipality. In this study, only 13.6% of the adults were able to control their blood glucose level. This was similar to a study conducted in Southern West Bank of Palestine. In that study, 16.1% of diabetics were able to control their blood glucose level [18]. On the contrary, findings from Vermont, Northern New York reported 57% prevalence of control diabetes [10].
In the current study, 86.4% were not able to control their blood glucose level. Even though our finding was high, similarly high levels of uncontrolled diabetes have been reported by other reporters elsewhere [9,15,19]. However, findings from studies conducted in an Urban District of Karachi, Pakistan were lower as compared to findings from the current study. They observed 50% [11] and 38.9% [13] prevalence of uncontrolled diabetes among adults who were diabetic. The differences in the prevalence of diabetes could be due to differences in care, attitudes and practices among diabetics, discrepancies or varied methods of education, treatment and counselling or differences in geographical location.
In the current study, there was a significant association between controlled diabetes and occupation. Civil servants were 84% times less likely to control their diabetes compared to those who were unemployed (AOR=0.16, p=0.031). Findings from a study conducted in China contrast with findings from the current study [20]. In the China study, those who were unemployed were unable to control their blood glucose level. Uncontrolled diabetes among civil servants in our study could be due to the busy working schedule with less time to eat a balanced meal, take medications and to also engage in active exercise.
Socioeconomic status (SES) and its constituent elements are accepted as being determinants of health [21]. In the current study, a high SES was a predictor of controlled diabetes among diabetics. Those with a high SES were 5.55 times more likely to control their diabetes as compared to those with a low SES (AOR=5.55, p=0.010). A study conducted in San Francisco reported that the blood glucose level among diabetic adults with a low SES lowered when they were given financial support [22]. Results from a study conducted in China [23] contradicts with the findings of the current study. The China results showed that diabetic patients with SES had a poor blood glucose control (p=0.0021). Controlled diabetes among those with high SES could be due to due to the fact that they were able to afford access to quality health care and referrals to a specialist, acquisition of diabetes-related knowledge, communication with providers, afford recommended medication and dietary regimens.
Even though it was not statistically significant a high consumption of vegetable among diabetics depicts healthy eating. Diabetics who consumed vegetables 3 days in a week and more than 4 days in a week were 7.89 and 4.39 times more likely to control their diabetes level in this current study (AOR=7.89, p=0.110) and (AOR=4.39, p=0.211) respectively. Healthy eating is associated with controlled diabetes [19]. The presence of vegetables in foods supplies vitamins, minerals and fibres instead of high calories. These vegetables tend to be rich in antioxidants and other phytochemicals, which inhibit the damaging reactions within the human body and have a beneficial effect on health [24]. Also, the lowered calories in food help in controlling the blood glucose. Hence, the consumption of vegetable helps in controlling diabetes.
▪ Limitations of the study
Limitations of this study included the fact that the study was done for only two months and the results may not reflect what happens throughout the year. Also, Information on diet may not be accurate because it was only collected from the respondents but not observed.
Conclusion and recommendations
Diabetes control was very low. Only 14 of the 100 diabetics could control their blood glucose level. Civil servants were less likely to control their blood glucose level. Those with a high SES were more likely to control their blood glucose level. Targeted interventions in the form of financial support to diabetics who are socially disadvantaged could improve their diabetes health care. Further studies are required to identify reasons for the poor DM control. Health workers at the diabetic clinic should intensify counselling of diabetics on diet and complications if blood glucose is not well controlled. Nutrition and health promotion officers should intensify education to the general public on diabetes and how to provide support to diabetics.
Authors’ Contributions
JF and MK conceived the study, JF, MK, SB, JO, WT, MA, WKA and RO did the data analysis and wrote the methods section. JF, MK, PP, SB, JO, WT and ET were responsible for the initial draft of the manuscript. All authors reviewed and approved the final version of the manuscript.
Acknowledgements
We are grateful to the staff of the School of Public Health (SPH) of University of Health and Allied Sciences (UHAS). We are also grateful to Dr Pius Mensah the hospital medical superintendent and the staff of the Hohoe Municipal Hospital diabetic clinic. We would like to thank the interviewers and the diabetics who participated in the study.
References
- Muktabhant B, Sanchaisuriya P, Sarakarn P et al. Use of glucometer and fasting blood glucose as screening tools for diabetes mellitus type 2 and glycated haemoglobin as a clinical reference in rural community primary care settings of a middle-income country. BMC Public Health. 12(1), 349 (2012).
- World Health Organization, Global report on Diabetes. Geneva: World Health Organization. 2016.
- Assah FK, Mbanya JC. Diabetes in Sub-Saharan Africa – Overview of a Looming Health Challenge. US Endocrinology. 5(1), 13−19 (2009).
- Wild S, Roglic G, Green A et al. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 27, 1047-1053 (2004).
- Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes. Res. Clin. Pract. 87, 4−14 (2010).
- World Health Organization Global report on Diabetes. Geneva: World Health Organization, 2009.
- Fowler MJ. Microvascular and macrovascular complications of diabetes. Clin. Diabetes 26, 77−82 (2008).
- Mattila TK, de Boer A. Influence of intensive versus conventional glucose control on microvascular and macrovascular complications in type 1 and 2 diabetes mellitus. Drugs. 70(17), 2229−2245 (2010).
- Memoona R, Nadeem I, Wajiha M. Factors Associated with Uncontrolled Type 2 Diabetes Mellitus. Journal of Islamabad Medical & Dental College (JIMDC). 4(2), 68−71 (2015).
- Strauss K, MacLean C, Troy A et al. Driving Distance as a Barrier to Glycemic Control in Diabetes. J GEN INTERN MED. 21, 378–380 (2006).
- Woldu MA, Wami CD, Lenjisa JL et al. Factors Associated with Poor Glycemic Control among Patients with Type 2 Diabetes Mellitus in Ambo Hospital, Ambo; Ethiopia. Endocrinol. Metab. Synd. 3, 143 (2014).
- Kavithal V, Ramadas VS. Prevalence of Diabetes and Associated Risk Factors among Selected Type 2 Diabetes. Inter. J. Sci. Res (IJSR). 3(11) (2014).
- Siddiqui FJ, Avan BI, Mahmud S et al. Uncontrolled diabetes mellitus: Prevalence and risk factors among people with type 2 diabetes mellitus in an Urban District of Karachi, Pakistan. Diabe. Res. Clin. Pra. 148−156 (2014).
- Dalvi S, Khanolkar M, Biswas M. Weight reduction and improved glycaemic control following oestrogen replacement: Individualising diabetes care in women. Pract. Dia. Inter. 27(5): 185−186 (2010).
- Almutairi MA, Said SM, Zainuddin H. Predictors of Poor Glycemic Control Among Type Two Diabetic Patients. Am. J. Med. Med. Sci. 3(2), 17−21 (2013).
- Yousefzadeh G, Shokoohi M, Najafipour H. Inadequate control of diabetes and metabolic indices among diabetic patients: A population based study from the Kerman Coronary Artery Disease Risk Study (KERCADRS). Int. J. Health. Policy. Manag. 4, 271–277 (2015).
- Degu G, Tessema F. Biostatistics for Health Science Students: lecture note series. The Carter Center 9EPHTI), Addis Ababa; January 2005
- Al-Halaweh AA, Davidovitch N, Almdalc TP et al. Prevalence of type 2 diabetes mellitus complications among Palestinians with T2DM. Diab. Met. Syndr: Clin. Res. Rev. 2017
- Chen CP, Peng YS, Weng HH et al. Health-promoting behavior is positively associated with diabetic control among type 2 diabetes patients. J. Nursing. 274−280 (2013).
- Zhang H, Xu W, Dahl AK et al. Relation of socioeconomic status to impaired fasting glucose and Type 2 diabetes: findings based on a large population-based cross-sectional study in Tianjin, China. Diabetes Medicine. 30(5), e157−e162 (2013).
- Rabi DM, Edwards AL, Southern DS et al. Association of socio-economic status with diabetes prevalence and utilization of diabetes care services. BMC Health. Serv. Res. 6, 124 (2006).
- Yew M, Quek HC, Khor HT, Shakoor SA. Relationship between Glycemic control and socioeconomic status in secondary diabetes care setting, San Francisco. The Endocrine Society 15–18 (2013).
- Tao X, Li J, Zhu X et al. Association between socioeconomic status and metabolic control and diabetes complications: a cross-sectional nationwide study in Chinese adults with type 2 diabetes mellitus. Cardio. Diabet. 15, 61 (2016).
- Asif M. The role of fruits, vegetables, and spices in diabetes. International Journal of Nutrition, Pharmacology, Neuro. Dise. 1(1) (2011).