Case Report - Imaging in Medicine (2018) Volume 10, Issue 4
Peritoneal pseudotumoral actinomycosis: A case report
Rim Ouji*, Nazek Achour, Ines Kasraoui, Ons Ghdes & Najla Mnif
Charles Nicolle Hospital, Tunisia
Abstract
Abdominal actinomycosis is an uncommon abdominal disease caused by Actinomyces species. It may appear as an abdominal mass and it has a tendency to infiltrate adjacent tissues this is why it is often mistaken for a malignant tumor. We report a case of a man who consulted our institution for abdominal pain and a palpable right upper quadrant mass. Computerized tomography (CT) scan showed intra-peritoneal tissue mass with irregular contours that invades the left colon and infiltrates the abdominal oblique muscles. The biopsy under colonoscopy could not eliminate a malignant tumor. A scanner-guided biopsy confirmed the diagnosis of actinomycosis. The sample revealed the presence of voluminous clumps of rounded basophilic germs, filamentous in appearance. High dose IV penicillin therapy was given with complete resolution of symptoms and a complete disappearance of the colonic wall thickening as well as the invasion of the abdominal wall in the CT.
Keywords
Actinomycosis ▪ intra-abdominal infection ▪ abdominal pain
Introduction
Actinomycosis is a suppurative bacterial infection caused by Actinomyces species. The majority of infections in humans are related to Actinomyces israelii [1-4]. Abdomen is the third body site for the infection of actinomycosis (20%). If the circumstance of discovery is an abdominal mass, the local lesion needs to be differentiated from abdominal malignant neoplasia [2,3]. The clinical and radiologic findings of actinomycosis are variable. Diagnosis preoperatively is rarely made due to variable clinical presentations and confusion often with tumor origin. The majority of cases are diagnosed after surgical intervention with resection of the lesion and histological examination [5].
Case presentation
A 61-years-old man, without medical or surgical history, was admitted complaining of left abdominal pain for three months without bowel dysfunction. Physical examination showed a good general condition and no fever. Abdominal exam objectified a large tinder mass of the left upper quadrant fixed to the abdominal paw.
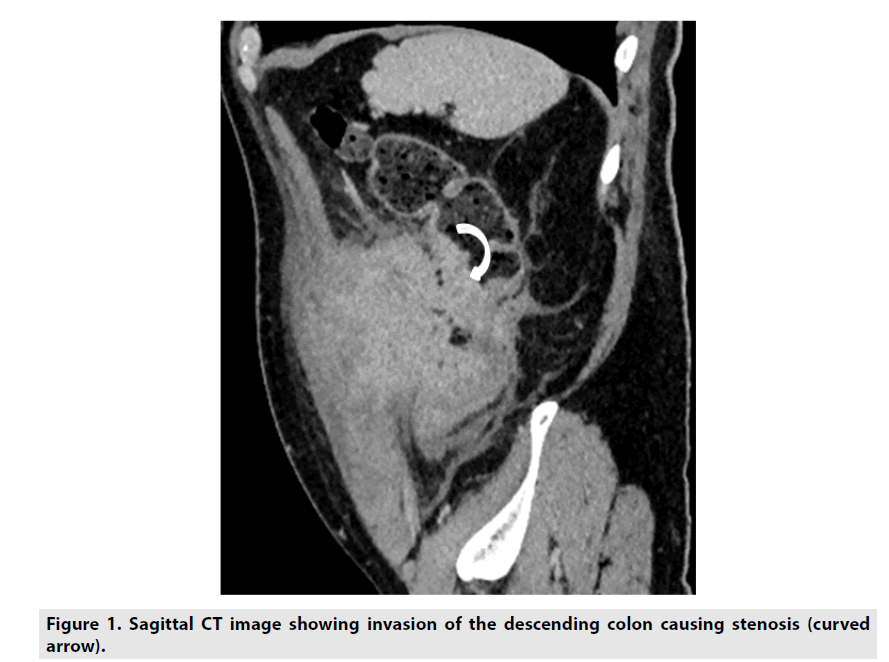
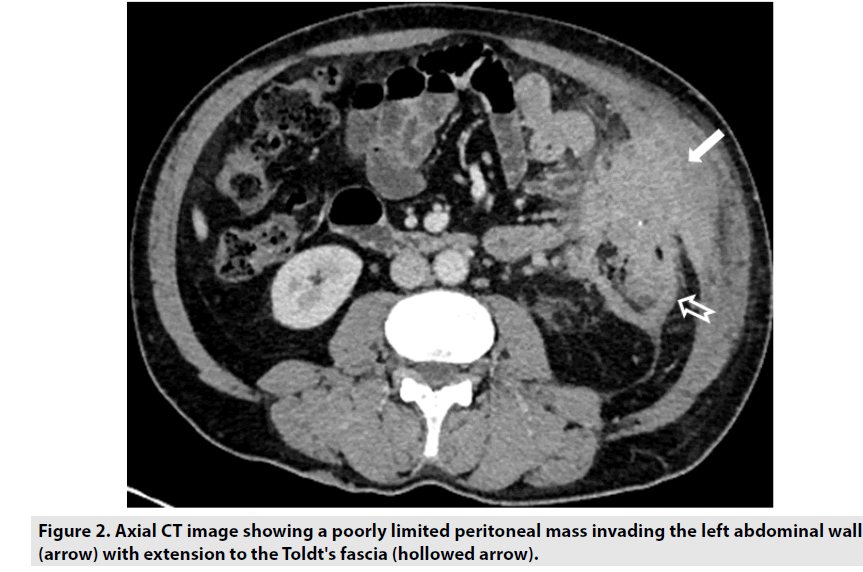
Laboratory examination revealed white blood cell count (WBC) 8350. Protein-C reactive levels were 114. CT scans with contrast enhancement of the abdomen and pelvis demonstrated intraperitoneal tissue mass with irregular contours, measuring 57 × 51 mm. This mass invaded the left colon (FIGURE 1) and infiltrates the abdominal oblique muscles. It continued with the Toldt's fascia which was thickened (FIGURE 2).
Figure 1. Sagittal CT image showing invasion of the descending colon causing stenosis (curved arrow).
Colonoscopy was performed and showed tow sigmoidian diverticulum, and congestive buds in the left colon, of firm consistency without the hardness of the neoplastic processes, and the presence of an impassable stenosis.
The biopsy done during the colonoscopy revealed edematous changes in the colonic mucosa without histological evidence of malignancy.
CT-guided biopsy of the parietal involvement was done. The sample showed the presence of voluminous clumps of rounded basophilic germs, filamentous in appearance, evoking actinomycotic grains. The final diagnosis was peritoneal pseudotumoral actinomycosis.
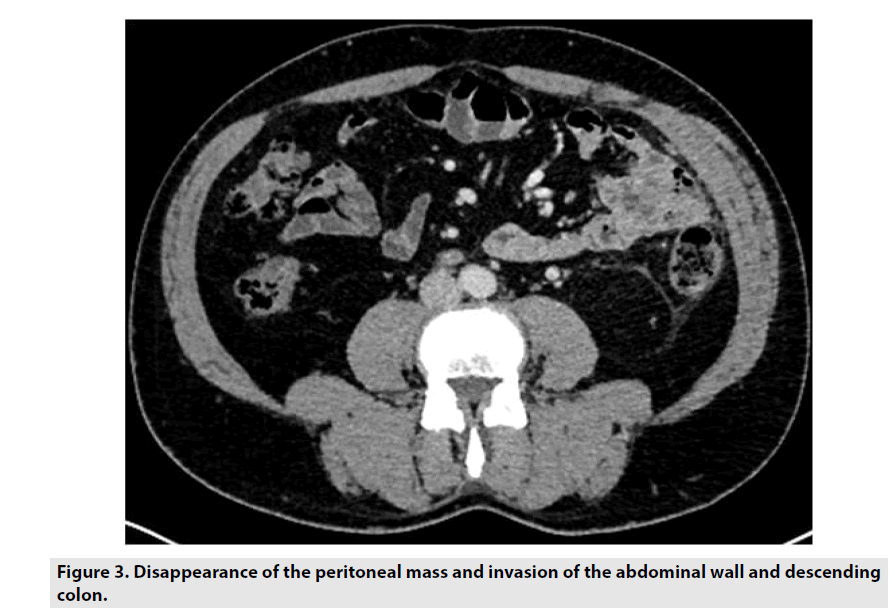
Penicillin G was started. The evolution has been marked by a significant clinical improvement. CT scan after five months of treatment showed a complete disappearance of the colonic wall thickening as well as the invasion of the abdominal wall (FIGURE 3).
Discussion
Actinomycosis is a suppurative disease produced by saprophyte organisms that normally colonize the oral cavity, gastrointestinal tract and female genital tract. It's caused by Actinomyces species. They are Gram-positive non-sporing, filamentous, anaerobic bacteria [6]. In human several Actinomyces species could be pathogenic; Actinomycoces israelli is the most common pathogenic species. The organisms have a low virulence potential and infection occurs when the mucosal barrier is broken, leading to abcess formation or a mass lesion [5,7,8].
On average, the abdominopelvic localization presents 20% of cases of patients with actinomycosis [3]. Abdominal actinomycosis usually occurs after the disruption of the intestinal mucosal integrity caused by different abdominal affection such as appendicitis, bowel perforation, colonic diverticulitis, foreign bodies or surgery of the gut [1,3,5,9].
Various abdominal organs may be involved in abdominopelvic actinomycosis and include most frequently the gastrointestinal tract and ovaries [9]. The portions of the gastrointestinal tract commonly affected are the appendix and ileocecal valve area (65%) [10]. The left side of the colon is rarely reported to be affected [11].
In case of colonic involvement, the colonoscopy is not very contributive for the positive diagnosis as the disease has an extra-mucosal origin [3]. CT scan of patients with abdominopelvic actinomycosis is useful to suggest the diagnosis and to determinate the anatomic location of this disease. It is also helpful for monitoring the effectiveness of treatment and for follow-up.
The most observed CT sign is a solid mass with tissue enhancement. It is surrounded by an inflammatory infiltration that invades the fascia and the abdominal wall [2,5,12]. When bowel is involved, the common CT finding is concentric wall thickening.
The invasive nature of the mass can mimic a malignant tumor. Often the infiltration of the peritoneum is localized and the disease process does not appear to spread into the whole peritoneal cavity. Ascite and lymphadenopathy are rarely associated with abdominal actinomycosis [3,9].
CT-guided fine needle aspiration helps to confirm the diagnostic. It is also used for therapeutic purposes in case of large abscess. The diagnosis is based on microbiological or histological examination which isolate Actinomyces species in pus, or tissue biopsy. Gram staining reveals a gram positive bacteria with filamentous branching and sulphur granules [13]. High dose intravenous penicillin injection followed by orally administered penicillin for at least 6 to 12 months is the treatment of choice [7].
Conclusion
Abdominal actinomycosis is to be considered in the differential diagnosis of an abdominal mass. The most important CT feature for the correct diagnosis is a large infiltrative mass adjacent to the involved bowel mimicking cancer.
Conflict of interest
No potential conflict of interest relevant to this article was reported.
References
- Ridha A, Oguejiofor N, Abayechi AS et al. Intra-Abdominal Actinomycosis Mimicking Malignant Abdominal Disease. Case. Rep. Infect. Dis. 2017, 1-4 (2017).
- Montori G, Allegri A, Merigo G et al. Intra-abdominal actinomycosis, the great mime: case report and literature review. Emerg. Med. Health. Care. 3, 1-5 (2015).
- Heo SH, Shin SS, Kim JW et al. Imaging of Actinomycosis in Various Organs: A Comprehensive Review. Radio Graphics. 34, 19-33 (2014).
- Yegüez JF, Martinez SA, Sands LR et al. Pelvic actinomycosis presenting as malignant large bowel obstruction: a case report and a review of the literature. Am. Surg. 66, 85-90 (2000).
- Sung HY, Lee IS, Kim SI et al. Clinical Features of Abdominal Actinomycosis: A 15-year Experience of A Single Institute. J. Korean. Med. Sci. 6, 932-937 (2011).
- Garner JP, Macdonald M, Kumar PK. Abdominal actinomycosis. Int. J. Surg. 5, 441-448 (2007).
- Smego JRA, Foglia G. Actinomycosis. Clin. Infect. Dis. 26, 1255-1261 (1998).
- Sumer Y, Yilmaz B, Emre B et al. Abdominal mass secondary to actinomyces infection: An unusual presentation and its treatment. J. Postgrad. Med. 50, 115 (2004).
- Lee IJ, Ha HK, Park CM et al. Abdominopelvic actinomycosis involving the gastrointestinal tract: CT features. Radiology. 220, 76-80 (2001).
- Cintron JR, Del PA, Duarte B et al. Abdominal actinomycosis. Dis. Colon. Rectum. 39, 105-108 (1996).
- Privitera A. Actinomycosis of the sigmoid colon: A case report. World. J. Gastrointest. Surg. 1, 62 (2009).
- Triantopoulou C, Molen AV, Es ACV et al. Abdominopelvic actinomycosis: spectrum of imaging findings and common mimickers. Acta. Radiol. Short. Rep. 3, 1-5 (2014).
- Valour F, Sénéchal A, Dupieux C et al. Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect. Drug. Resist. 7, 183-297 (2014).