Review Article - Imaging in Medicine (2012) Volume 4, Issue 3
MR enterography in Crohn disease: a perspective on methodology, interpretation and utility
Diego R Martin1*, James Costello1, Bobby Kalb1, Cary Sauer2and Steve Goldschmid3
1Department of Medical Imaging, 1501 North Campbell Ave, PO Box 245067, Tucson, AZ, 85724-5067, USA
2Department of Pediatrics, Emory University, 2015 Uppergate Dr., Atlanta, GA, 30322, USA
3College of Medicine, University of Arizona, 1501 North Campbell Ave, PO Box 245035, Tucson, AZ, 85724, USA
- *Corresponding Author:
- Diego R Martin
Department of Medical Imaging
1501 North Campbell Ave, PO Box 245067 Tucson
AZ, 85724-5067, USA
Tel.: +1 520 626 1069
Fax: +1 520 626 1945
E-mail: dmartin@radiology.arizona.edu
Abstract
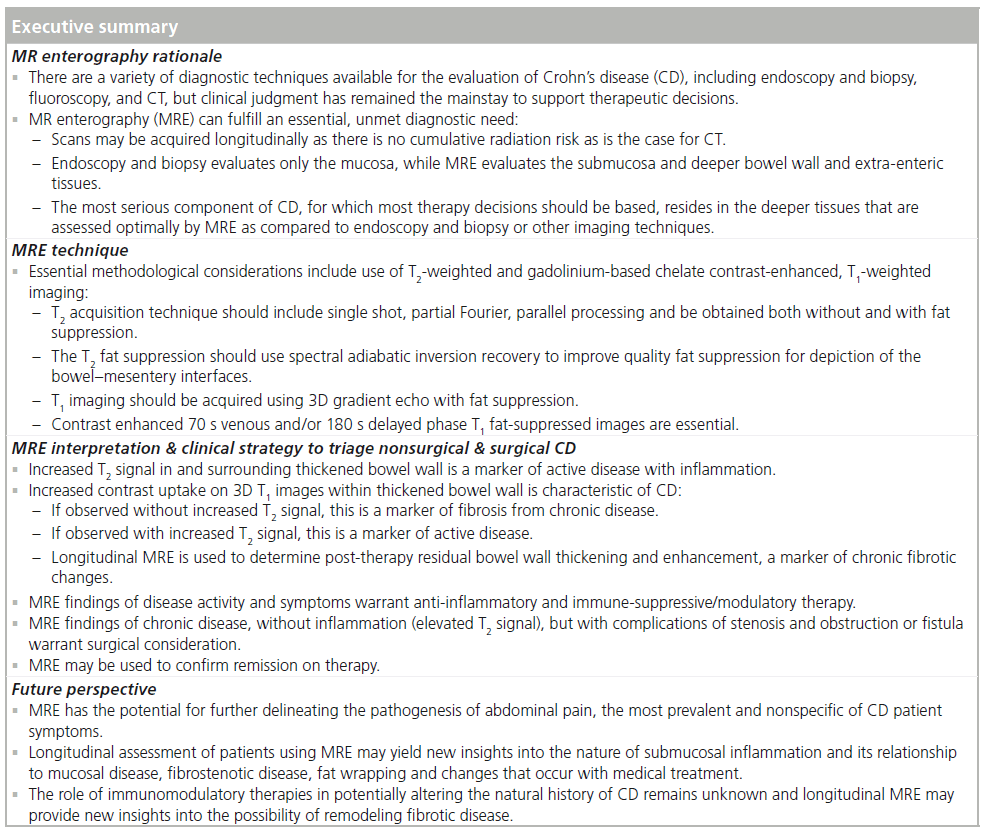
This article reviews MR enterography (MRE), contrasts MRE to other available tests and provides recommendations for optimal use of MRE in the clinical management of Crohn’s disease. A review of Crohn’s disease and diagnostic approaches is introduced. MRE is described from a historical perspective, and a technical approach with key essential elements vital to optimal diagnostic yield is described. MRE is contrasted to disease activity index, capsule and optical endoscopy, small bowel follow-through or enteroclysis, and CT enterography. Key patterns of findings on MRE in correlation with pathological relationships are summarized. Recommendations for clinical use of MRE are then provided, including how to use MRE to direct therapeutic management.
Keywords
adult Crohn’s disease; enteroclysis; magnetic resonance enterography; MR enterography; MRI; pediatric Crohn’s disease
Our overarching aim is to provide an understanding of the pathology–imaging correlation between MR enterography (MRE) and histology in Crohn’s disease (CD). The authors draw from their investigation on this topic to provide an analysis of the essential diagnostic methodology for MRE to be successful for routine clinical application. There is emphasis on simplified acquisition techniques and maximizing patient exam tolerance by minimizing the requirement for bowel preparation and shortening overall exam times. We provide a series of case presentations to elucidate these principles. Essential technical considerations are described in relation to the MRE sequences. These technical considerations are not yet widely appreciated, and the intent is to provoke more detailed consideration of the techniques employed by radiologists caring for patients with CD. Additional aims of this article include contrasting between the histological components of CD to which MRE is sensitive to detection but to which other imaging tests (fluoroscopy and CT) and endoscopy fail to distinguish. Finally, the unique contribution of MRE for CD evaluation will be highlighted. We will also provide guidelines on the use of MRE in current practice for the management of patients with suspected or known CD.
In this article we will emphasize that endoscopic tests and biopsies are sensitive to disease of the mucosa but do not evaluate inflammation or fibrosis within submucosa or deeper tissues. This is a significant limitation as the most important disease resides within the deeper tissues of the bowel wall. Considering the dynamic properties of the mucosa to repair injury, endoscopic techniques may not appreciate the full disease extent. We will discuss how MRE is sensitive to evaluating the deeper tissues, which are not adequately assessed endoscopically, and we will discuss the implications for CD management.
Background
There has been development of multiple diagnostic imaging methods in the evaluation of CD, yet there remains need for education and further validation of optimized utilization of the available imaging techniques, in conjunction with endoscopy and biopsy. General use of CT has increased markedly over the past 10 years, yet the optimal use of CT imaging in CD should be assessed in the context of balancing benefits against the risks of CT radiation-induced cancer [1–13]. Ultimately, the application of CT imaging must be judged against the more recently developed imaging techniques, namely MRE, which are devoid of damaging ionizing radiation.
Small bowel involvement of CD can be difficult to diagnose and to monitor. Endoscopy with biopsy is still generally viewed as a reference standard; however, very little of the small bowel is visualized, and these tests only evaluate the mucosa. Video capsule endoscopy (VCE) can visualize mucosal disease but is unable to provide tissue. Small bowel follow-through (SBFT) is relatively insensitive to mucosal disease, provides limited delineation of submucosal or deeper disease and requires use of ionizing radiation. Fluoroscopic enteroclysis, wherein contrast is administered into the duodenum with the use of a nasogastric tube, which can be cumbersome and uncomfortable for the patient. While fluoroscopic enteroclysis promises improved bowel distention and bowel wall morphologic imaging compared with SBFT, the technique is generally inconsistent and shares similar limitations as for SBFT.
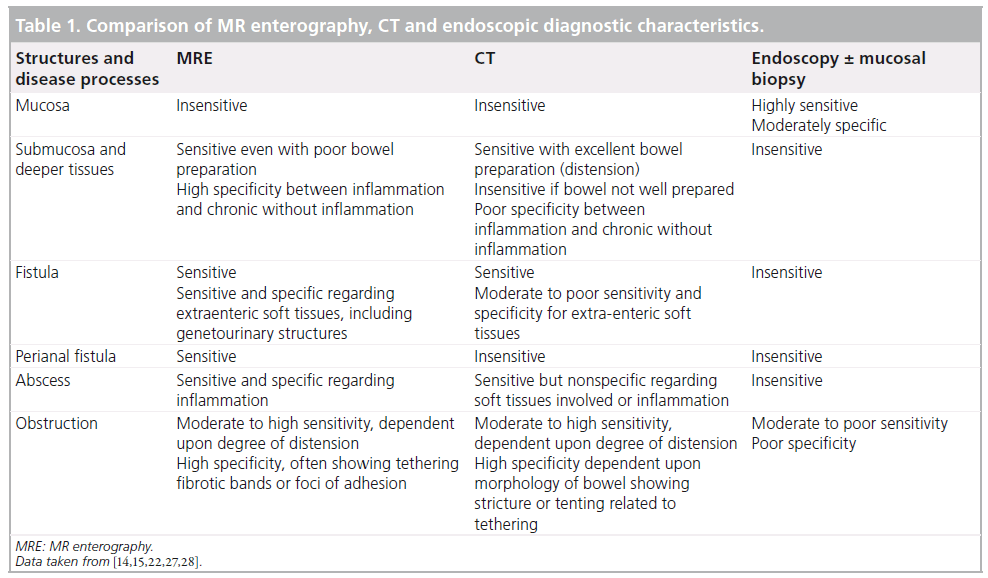
CD is a transmural disease in which submucosal inflammation is responsible for tissuedestructive and penetrating disease, fibrotic disease, strictures and fistulae. These disease processes are responsible for the most serious morbidities and contrast with disease restricted to the mucosa, which is not associated with such sequelae. Currently, CT enterography and MRE are the only two imaging modalities that enable visualization of submucosal tissues throughout the entire small bowel, but MRE does not expose patients to ionizing radiation (Table 1). In addition, MRE provides key technical and diagnostic advantages that favor this imaging modality for CD initial diagnosis and monitoring.
MRE technique: background
MRE findings can include acute inflammation and chronic disease without inflammation. Other MRE findings may include intra-abdominal complications such as fistulae, tethering (potentially the beginnings of a fistula), abscesses and fibrotic stricturing with associated proximal bowel distension. MRE uses different imaging sequences to acquire images with contrast characteristics generally described as T1-weighted (T1W; fluid dark, fat bright), or T2-weighted (T2W; fluid bright, fat bright). There are a variety of T1W and T2W sequences to select, but the most useful for bowel imaging include the 3D-gradient echo T1W and the single- shot T2W techniques [14,15]. T1W images are acquired after administration of gadoliniumbased contrast to selectively enhance diseased bowel wall. Since inflamed bowel and fat both produce high signal on T2W and gadoliniumenhanced T1W images, the naturally occurring fat surrounding bowel can interfere with visualizing disease. Fat-suppressed (FS) singleshot techniques are critical to improve disease complicity. If the adjacent fat is completely darkened by FS, the diseased bowel generates a high signal that becomes highly conspicuous. T1W gadolinium-enhanced FS and T2W single-shot images with and without FS are the foundation for diagnosing and characterizing CD. Regular T2W single-shot images depict bowel wall morphology. FS, single-shot T2W images, such as spectral presaturation attenuated inversion recovery (SPAIR), are critical for assessment of edema and inflammation related to active CD [14,15]. Various T2 FS techniques are widely used. Our experience has identified the frequency-selective SPAIR as the optimal technique with the ability to isolate water signal by employing selective fat inversion with a nonslice-selective adiabatic inversion that is insensitive to loss of mesenteric FS that would otherwise occur from bowel peristalsis using earlier slice-selective techniques [14].
MRE technique: historical perspective
Earlier work on MRE attempted to replicate the luminography of a SBFT or a small bowel enema exam. Much like the fluoroscopic studies, these MR counterparts achieved bowel distension by administering a large volume of fluid either by mouth (MRE) or by enteric tube (MR enteroclysis). Water-based methods of bowel distension detailed the bowel lumen as bright on T2W techniques and as dark on T1W techniques. T2W images were acquired rapidly, using single-shot, echo-train, spin echo images with thick 5–8 cm sections. In order to augment bowel distension, several techniques were employed to slow the absorption of water. Example methods included adding 2.5% mannitol, a nondigested carbohydrate, to increase the osmotic load and to slow water absorption in the jejunum. In an effort to improve visualization of the terminal ileum and the large bowel, rectal water enemas have been used. Studies have shown MR luminography with bowel distension is achievable by administering 1000–1200 ml of water-based contrast by mouth 20–30 min prior to the examination. This water-based contrast agent can be accompanied by metoclopramide or erythromycin dosed intravenously to promote gastric emptying [16,17].
MRE technique: the latest updates
Progressive experience over the past 10 years has led to the following conclusions and contrasts to both the early descriptions of MRE and to CT and fluoroscopy techniques (specific MRE sequence details are listed in [14,15]). By achieving significant improvements in the diagnostic quality of MRE sequence techniques, we have significantly relaxed the requirement for bowel lumen distention. These sequence techniques rely on T2W single-shot images coupled with SPAIR for optimal FS [14] and T1W contrast-enhanced imaging using latest generation 3D gradient echo (3D GRE) to improve contrast and edge sharpness. Of particular note, we have found that we do not require an enteroclysis level of distention [15].
Oral contrast or no added luminal contrast is sufficient in most patients. Routine water-based contrast agents used for CT are equally useful for MRE. Even if the patient is unwell and unable to take an oral agent, we proceed with the examination and find these studies similarly diagnostic in the setting of chronic/active CD. In comparison, CT and fluoroscopic techniques are usually nondiagnostic without an enteroclysis level of bowel distention. Even in lean patients, MRE remains diagnostically sensitive and generates ample bowel wall contrast. This technique contrasts with CT, which benefits progressively from increased levels of intraabdominal fat to separate bowel loops. While prior MRE studies have discussed potential benefits of rectal water enemas for visualization of terminal ileum CD, we have found that further improvements in the MRI techniques, including improvements in fat suppression and in 3D GRE, have reduced the need for colon water distension [15].
In summary, the benefits of a simplified MRE technique [15] include a faster exam, optimal patient comfort, improved compliance with the study and improved diagnostic yield. Simplification of oral contrast administration is achieved by using readily available and inexpensive CT oral contrast agents. By reducing the required degree of bowel lumen contrast distension, as compared to enteroclysis, and minimizing the need for rectal contrast, MRE becomes markedly more convenient for technologists and comfortable for patients. These are important developments and advantages, particularly when comparing to other diagnostic techniques and when considering the young age of most CD patients.
A summary of MRE findings in CD
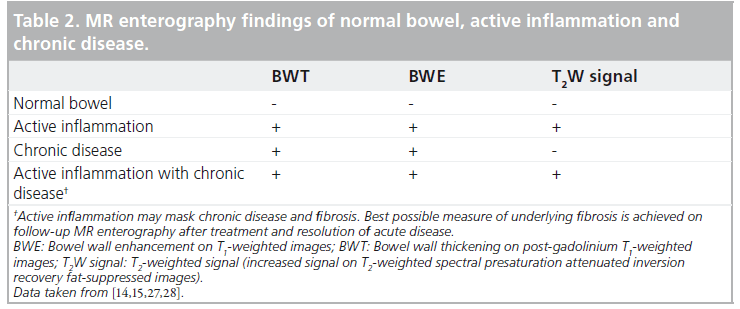
The features of CD shown by MRE are summarized in Table 2. On T1W images these findings include:
▪ Bowel wall thickening with increased enhancement in the delayed images;
▪ Stranding extending into the mesenteric border fat and increased size and number of vessels;
▪ Accordion-like compression and thickening of folds asymmetrically involving the mesenteric side of the small bowel having a tethered appearance;
▪ Reactive enlarged adjacent mesenteric nodes.
On T2W imaging common features of CD include:
▪ Bowel wall thickening with increased signal in and adjacent to the abnormal bowel (on FS images) showing active inflammation;
▪ Fluid accumulation in adjacent intraperitoneal and mesenteric spaces.
An interpretive approach to a thickened bowel wall segment is based on one of three key diagnostic characterizations of CD required for therapeutic decisions:
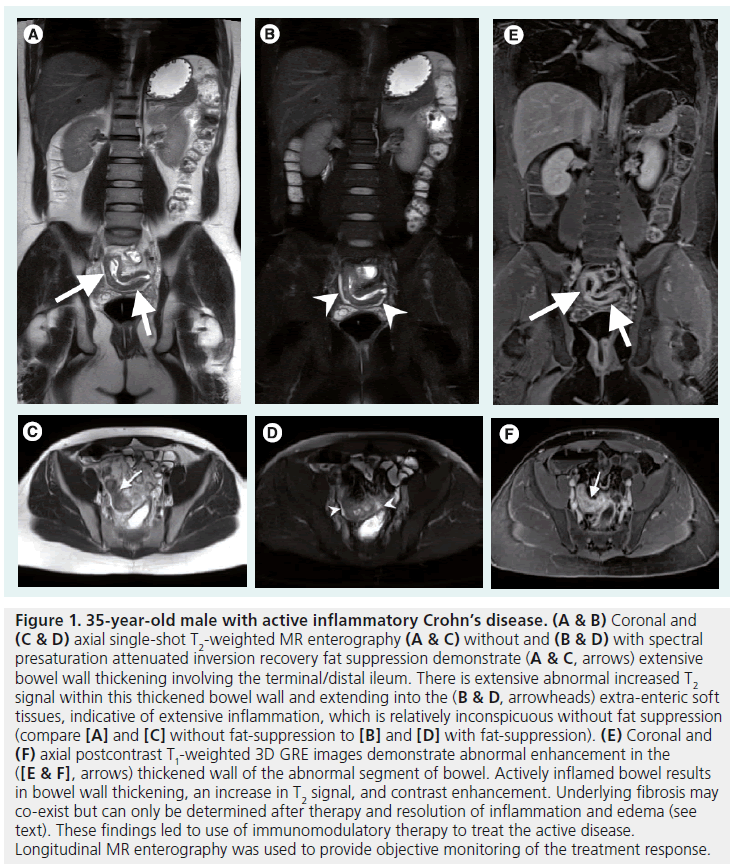
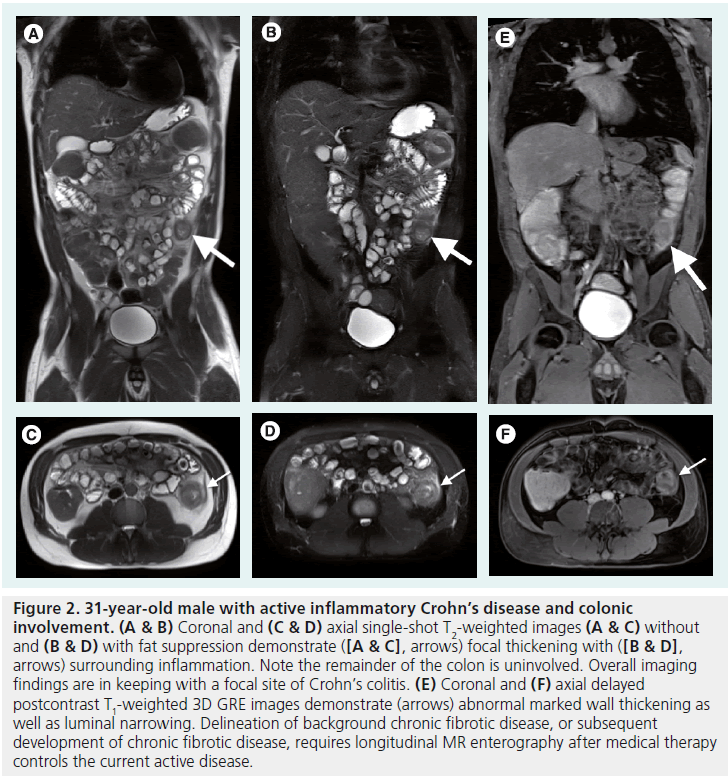
▪ Active inflammation: enhancement on postgadolinium T1W images coupled with bowel wall thickening in addition to high signal intensity on T2W-SPAIR FS images (Figures 1 & 2);
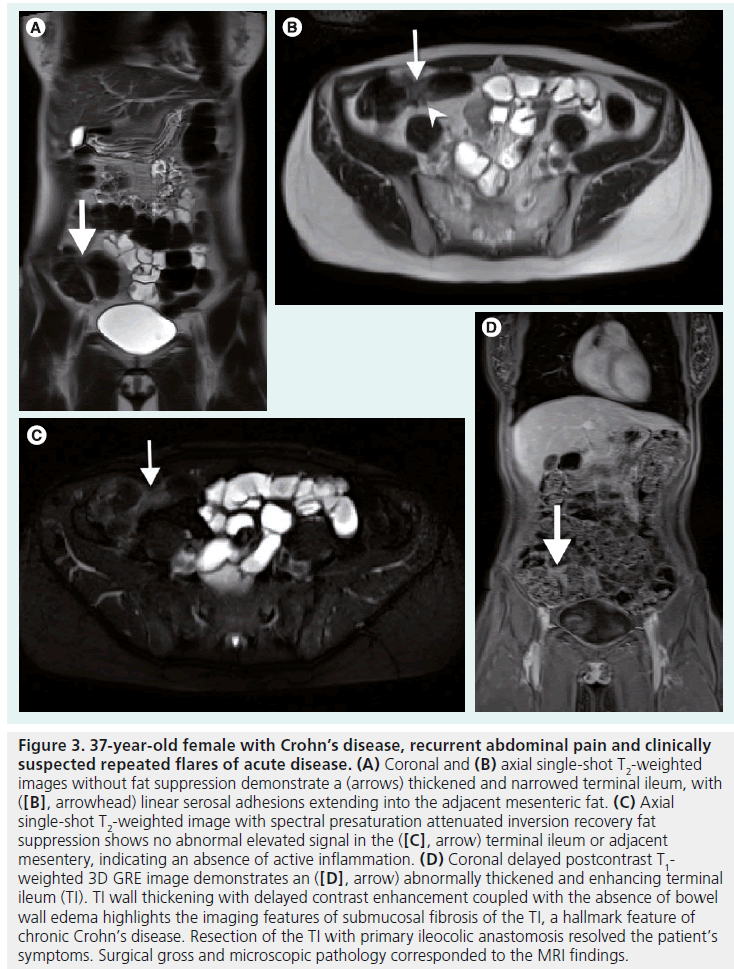
▪ Chronic disease without active inflammation: bowel wall thickening and enhancement on post-gadolinium T1W images coupled with bowel wall thickening in addition to low signal intensity on T2W-SPAIR FS images with possible stenosis and obstruction (Figure 3);
▪ Chronic disease with active inflammation: features that overlap with active inflammation with thickened bowel wall showing both increased T2 signal and retained contrast on T1W images. A symptomatic patient with these findings requires longitudinal repeated MRE scanning after therapy has been instituted to show the effect as measured by resolution of the elevated T2 signal. Findings of residual thickening and retained contrast are features of chronic disease [14,15].
Complicated CD is almost always a marker of a patient with relapsing and chronic disease, and the most common of these features can be shown on MRE, including:
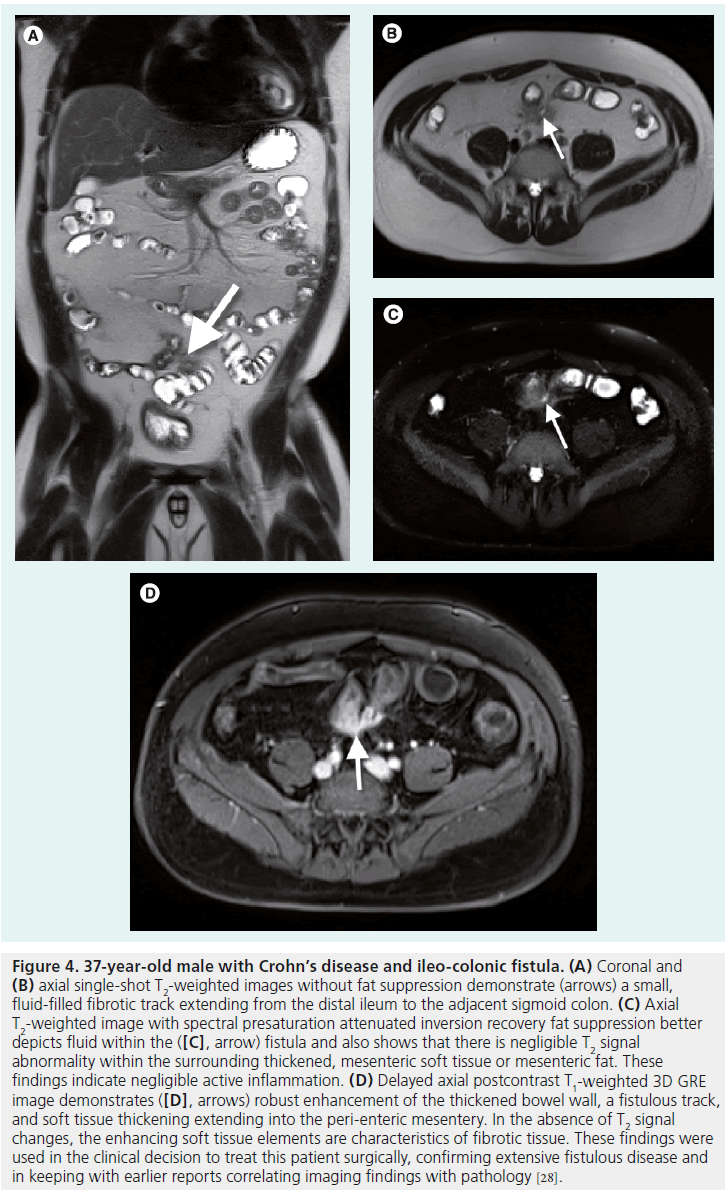
▪ Fistulae, tethering and strictures (Figure 4);
▪ Bowel obstruction;
▪ Extra-enteric collections, abscesses and perianal disease (Figure 5).
Identifying active inflammation is rarely an interpretive problem on MRE. One important aspect of MRE interpretation is that active inf lammation can mask underlying fibrosis related to chronic disease of the bowel wall (Table 2). The presence or absence of underlying fibrosis in this setting is of lesser immediate consequence as active inflammation requires treatment. In the setting of active inflammation, longitudinal MRE evaluation is implemented to confirm improvement of active inflammation and to then evaluate for the presence of unmasked chronic fibrotic disease. After therapy for active inflammation, the fibrotic burden can be assessed, and this information used for management decisions, including the role of surgery.
Clinical use of small bowel MRE
Currently, enteric disease activity is most frequently assessed with surgical technique, capsule endoscopy, and/or endoscopy, accompanied with tissue biopsy [18–21]. These techniques suffer from inherent limitations, such as the invasive nature of endoscopy or the restricted use of capsule endoscopy in clinical scenarios of bowel stenosis or obstruction. While these techniques demonstrate high fidelity in detecting mucosalonly disease, they lack the ability to detect the disease extent within the submucosa and the serosa–mesentery [22].
Several different MRE techniques have been employed for transmural evaluation of the small bowel. Some studies have solely relied on assessing the perfusion pattern of the bowel wall [23]. Other techniques have attempted to evaluate inflammatory activity by employing a multiparameter, MRE-based scoring system [24,25].
Figure 1. 35-year-old male with active inflammatory Crohn’s disease. (A & B) Coronal and (C & D) axial single-shot T2-weighted MR enterography (A & C) without and (B & D) with spectral presaturation attenuated inversion recovery fat suppression demonstrate (A & C, arrows) extensive bowel wall thickening involving the terminal/distal ileum. There is extensive abnormal increased T2 signal within this thickened bowel wall and extending into the (B & D, arrowheads) extra-enteric soft tissues, indicative of extensive inflammation, which is relatively inconspicuous without fat suppression (compare [A] and [C] without fat-suppression to [B] and [D] with fat-suppression). (E) Coronal and (F) axial postcontrast T1-weighted 3D GRE images demonstrate abnormal enhancement in the ([E & F], arrows) thickened wall of the abnormal segment of bowel. Actively inflamed bowel results in bowel wall thickening, an increase in T2 signal, and contrast enhancement. Underlying fibrosis may co-exist but can only be determined after therapy and resolution of inflammation and edema (see text). These findings led to use of immunomodulatory therapy to treat the active disease. Longitudinal MR enterography was used to provide objective monitoring of the treatment response.
These methods quantify several enteric parameters, such as bowel wall thickening, luminal narrowing and number of peri-intestinal lymph nodes. While very comprehensive, these techniques demand a significant time investment, which will ultimately limit their clinical application. In addition, these techniques require a unique sequencing of dynamic T1W imaging of the abdomen and pelvis to capture the perfusion pattern of the bowel in its entirety. This imaging requirement frequently leads to compromised imaging of the upper and/or lower field of view, particularly in larger patients. This may compromise both visualization of the entire bowel and also limit assessment of other soft tissues, particularly the liver. Technically, the T1W images are less robust and are susceptible to such technical complications as respiratory and bowel motion along with magnetic field distortions from surgical clips and bowel gas.
We propose a simpler imaging alternative using FS T2W, single-shot, fast spin-echo MRI [22]. This imaging technique demonstrates enhanced specificity for detecting inherent or surrounding bowel wall edema. When this T2W FS technique is coupled with late-vascular or interstitial phase contrast-enhanced, T1W imaging (180 s delayed), we can achieve a comprehensive evaluation of the bowel that discriminates between active inflammation versus quiescent and chronic disease (positive predictive value of 90%, negative predicitive value of 94%) (Figures 1–3) [26–28]. In addition, this combined technique can reliably evaluate for such complications of CD as abscesses or fistulae (Figures 4 & 5).
Figure 2. 31-year-old male with active inflammatory Crohn’s disease and colonic involvement. (A & B) Coronal and (C & D) axial single-shot T2-weighted images (A & C) without and (B & D) with fat suppression demonstrate ([A & C], arrows) focal thickening with ([B & D], arrows) surrounding inflammation. Note the remainder of the colon is uninvolved. Overall imaging findings are in keeping with a focal site of Crohn’s colitis. (E) Coronal and (F) axial delayed postcontrast T1-weighted 3D GRE images demonstrate (arrows) abnormal marked wall thickening as well as luminal narrowing. Delineation of background chronic fibrotic disease, or subsequent development of chronic fibrotic disease, requires longitudinal MR enterography after medical therapy controls the current active disease.
Active inflammation of the bowel wall correlates with the presence and extent of bowel wall edema. With this feature in mind, we can accurately distinguish between active inflammation and chronic fibrotic disease by detecting increased signal intensity on T2W FS imaging alongside contrast-enhanced T1W MRE. In 2008, we conducted a study where 81 patients with CD were diagnostically evaluated with CE interstitial phase (180 s delayed) T1W images, plus FS T2W imaging. Using edematous signal and bowel enhancing features as a reliable measure of disease activity, this imaging technique achieved a high degree of accuracy (T2 signal intensity changes with a specificity of 98%; gadolinium-enhanced T1 imaging with a sensitivity of 85%) as compared with conventional methods such as endoscopy, biopsy or surgical pathology [28]. With the addition of more advanced and technically more robust, high-quality, FS, single-shot, T2W imaging, MRE may detect disease activity with greater accuracy than demonstrated by prior MRE techniques [23,26,29–32].
MRE is sensitive to disease activity previously only detectable by surgical resection and otherwise inapparent to more conventional methods. A limitation of MRE is the apparent insensitivity to detecting early changes of CD restricted to the mucosa; however, when coupled with optical methods of mucosal evaluation (endoscopy, capsule endoscopy and biopsy), we possess a complete and comprehensive method to evaluate all stages and sequelae of disease activity [28].
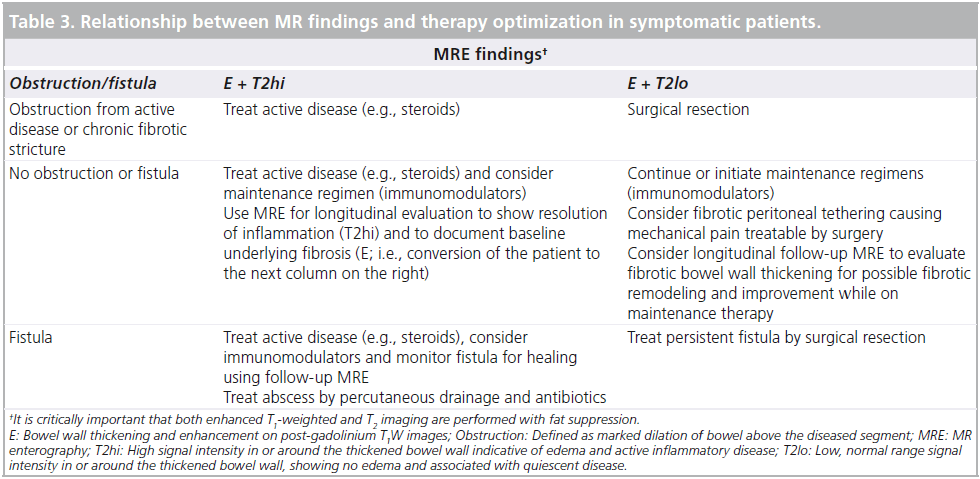
Another limitation of MRE is that this technology and expertise is not ubiquitous. For the pediatric population and for patients with claustrophobia, well-defined MRE imaging may require sedation prior to the exam. As with other MRI techniques, absolute contraindications include metallic fragments in the orbits and other relative limitations including claustrophobia or cardiac devices (uncommon in young CD patients). Despite these constraints, MRE promises an unparalleled measure of disease activity that can help direct the therapeutic decision pathway either towards surgical or medical management and for monitoring therapy longitudinally (Table 3). Furthermore, MRE can complement other diagnostic modalities, such as capsule endoscopy, by detecting procedural contraindications such as bowel stenosis or obstruction.
Figure 3. 37-year-old female with Crohn’s disease, recurrent abdominal pain and clinically suspected repeated flares of acute disease. (A) Coronal and (B) axial single-shot T2-weighted images without fat suppression demonstrate a (arrows) thickened and narrowed terminal ileum, with ([B], arrowhead) linear serosal adhesions extending into the adjacent mesenteric fat. (C) Axial single-shot T2-weighted image with spectral presaturation attenuated inversion recovery fat suppression shows no abnormal elevated signal in the ([C], arrow) terminal ileum or adjacent mesentery, indicating an absence of active inflammation. (D) Coronal delayed postcontrast T1- weighted 3D GRE image demonstrates an ([D], arrow) abnormally thickened and enhancing terminal ileum (TI). TI wall thickening with delayed contrast enhancement coupled with the absence of bowel wall edema highlights the imaging features of submucosal fibrosis of the TI, a hallmark feature of chronic Crohn’s disease. Resection of the TI with primary ileocolic anastomosis resolved the patient’s symptoms. Surgical gross and microscopic pathology corresponded to the MRI findings.
Comparison of MRE to disease activity index
CD activity measurements are predominantly subjective measurements. Examples include physician global assessment, Harvey-Bradshaw Index, Crohn’s Disease Activity Index (CDAI), and the Pediatric Crohn’s Disease Activity Index [33–35]. As expected, comparing MRE’s objective measures of disease inflammation to subjective measures of clinical activity resulted in conflicting data. Multiple studies have demonstrated no correlation between MRE findings and CDAI [20,36–38]. Meanwhile, other studies have demonstrated correlation between MRE and CDAI [23,39–41] and correlation between MRE and laboratory markers of inflammation (erythrocyte sedimentation rate/C-reactive protein test) [41–43]. Within the pediatric population, similar results were obtained. Some studies demonstrated a statistically significant correlation between disease on MRE and Pediatric Crohn’s Disease Activity Index [44,45], while others revealed no correlation [43]. When comparing CD activity measurements with direct optical assessment, similar conflicting results also emerged. Since subjective clinical activity measurements do not necessarily reflect mucosal findings, these studies demonstrated a discordance between inflammation on endoscopy and subjective activity index measurements.
Figure 4. 37-year-old male with Crohn’s disease and ileo-colonic fistula. (A) Coronal and (B) axial single-shot T2-weighted images without fat suppression demonstrate (arrows) a small, fluid-filled fibrotic track extending from the distal ileum to the adjacent sigmoid colon. (C) Axial T2-weighted image with spectral presaturation attenuated inversion recovery fat suppression better depicts fluid within the ([C], arrow) fistula and also shows that there is negligible T2 signal abnormality within the surrounding thickened, mesenteric soft tissue or mesenteric fat. These findings indicate negligible active inflammation. (D) Delayed axial postcontrast T1-weighted 3D GRE image demonstrates ([D], arrows) robust enhancement of the thickened bowel wall, a fistulous track, and soft tissue thickening extending into the peri-enteric mesentery. In the absence of T2 signal changes, the enhancing soft tissue elements are characteristics of fibrotic tissue. These findings were used in the clinical decision to treat this patient surgically, confirming extensive fistulous disease and in keeping with earlier reports correlating imaging findings with pathology [28].
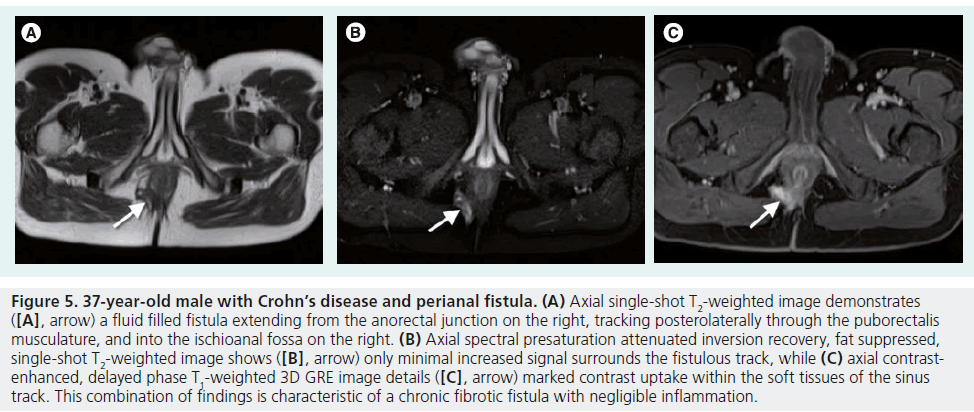
Figure 5. 37-year-old male with Crohn’s disease and perianal fistula. (A) Axial single-shot T2-weighted image demonstrates ([A], arrow) a fluid filled fistula extending from the anorectal junction on the right, tracking posterolaterally through the puborectalis musculature, and into the ischioanal fossa on the right. (B) Axial spectral presaturation attenuated inversion recovery, fat suppressed, single-shot T2-weighted image shows ([B], arrow) only minimal increased signal surrounds the fistulous track, while (C) axial contrastenhanced, delayed phase T1-weighted 3D GRE image details ([C], arrow) marked contrast uptake within the soft tissues of the sinus track. This combination of findings is characteristic of a chronic fibrotic fistula with negligible inflammation.
Comparison of MRE to VCE
VCE visualizes the mucosa throughout the entire small intestine with the use of a wireless video capsule. Three studies, all with approximately 20 patients each, have compared MRE to VCE for the detection of intestinal lesions. All three studies concluded that both MRE and VCE identified diseased small bowel; however, VCE was better at identifying small aphthous lesions and at recognizing a greater total number of lesions [31,46,47], reflecting our contention that MRE is insensitive to early, mild disease restricted to the mucosa [28].
Comparison of MRE to SBFT/conventional enteroclysis
Historically, SBFT has been recommended for the evaluation of both ulceration and strictures in CD. Gourtsoyiannis et al. published the largest study comparing MRE to SBFT in 52 CD patients. MRE and SBFT were in full agreement in revealing, localizing and estimating the length of bowel involved, and while MRE was poor at detecting superficial ulcers, it was very good at identifying deep ulcers and stenosis [39]. Multiple other studies have also suggested no difference between MRE and SBFT in the detection of active disease and stenosis [48–50]. Meanwhile, MRE shows transmural and deeper soft tissue pathologies that may be undetectable on SBFT [48]. With the current methods of optimized T1W and T2W imaging, MRE yields significant improvements over fluoroscopic techniques for overall detection of disease [14,15,28].
Comparison of MRE to CT scan
Concerns over radiation risks may lead to the underutilization of CT for the longitudinal management of CD [1]. There is a clinical need to provide for optimal use of cross-sectional imaging that is safer than CT imaging and provides at least the same diagnostic yield. MRE satisfies that need by providing a safe nonionizing technology that can be readily obtained without additive or long-term harm. When considering imaging options for the more radiationsensitive pediatric population, these features of MRE assume even greater importance [45,51,52].
In addition, evolving experience shows that MRE more accurately describes the submucosal pathology of transmural CD, including detection and quantification of inflammation, fibrotic disease and other intra-abdominal complications as compared to other diagnostics, including CT (Table 1). There is an accumulated body of evidence to show that a particular diagnostic strength of MRE over CT is the ability to differentiate inflammation from fibrosis within the submucosa of the bowel wall and within the peri-enteric tissues (Tables 1 & 2) [15,28,53,54]. MRE can show extra-intestinal disease, including bowel obstruction, abscesses, webs, tethering and fistulae. These disease processes may be visualized on MRE with less dependency on enteroclysis-level bowel distension as required for optimal CT imaging, an important technical advantage of MRE.
The advantages of a CT scan include availability and a slight cost differential. The overall cost–benefit is a key measure that remains as yet incompletely evaluated. Studies comparing MRE to CT for the evaluation of small bowel pathology have indicated similar sensitivities in one study [55], better sensitivity for CT in one study [56] and better sensitivity for MRE in a third study [54]. Finally, a meta-analysis of prospective studies concluded that there was no significant difference in diagnostic accuracy between MRE and CT [57]. As we discussed for SBFT, this array of results can be rationalized on the basis that these studies were performed without the advantages of current and more optimized MRE techniques and the latest generation MR systems.
Comparison of MRE to surgical resection specimens
The gold standard for evaluating MRE findings remains comparison to surgical specimens. Punwani et al. evaluated MRE prior to surgical resection in CD (seven fibrostenotic disease and 11 ileal disease unresponsive to treatment) [58]. Their results suggested that increased mural thickness (p < 0.001), high mural T2W signal intensity (p = 0.003) and a layered pattern of enhancement (p = 0.001) reflected histology features of small bowel inflammation in CD. The enhancement pattern of both fibrostenotic tissue and inflamed bowel demonstrated a nonhomogeneous, layered pattern. The authors acknowledged that this layered enhancement pattern might reflect acute inflammation superimposed upon chronic, fibrotic changes. They concluded that MRE images correlated with histological examination of surgical specimens and validated MRE findings against matched histology specimens [58].
Lawrance et al. evaluated MRE findings with surgical resection [59]. Using portal venous phase (60 s delayed), contrast-enhanced imaging, MRE findings were classified as no enhancement, mild hyperenhancement and mild thickening, mild hyperenhancement and marked thickening, and marked transmural hyperenhancement. All patients who had enhancement had mild to florid inflammation. Patients with mild or marked early small bowel enhancement demonstrated improvement to medical treatment, while those patients with mild bowel wall thickening and mild enhancement showed the overall best response to therapy. These results suggest that early phase contrast enhancement is an excellent marker for inflammation with presence and level of active disease correlating with surgical pathology [59].
Comparison of MRE to ultrasound
Ultrasound evaluation of the bowel is shown to have the capacity for demonstrating changes related to CD of the terminal ileum and for the evaluation of perianal disease [60]. Additional technical developments include use of microbubble enhancement. Limitations include the requirement for high level of operator expertise and the inability to explore all segments of small and large bowel systematically. Comparisons between ultrasound and MRE have been discussed with the conclusion that MRE is the most accurate method for evaluating disease activity [61].
Summary: recommendations for routine use of MRE in CD
Within a nonionizing exam, MRE can complement clinical management of CD and can provide a more complete picture of the extent of disease. The paired application of MRE with mucosal visualization and biopsy can lead to better management decisions and therapeutic options. MRE can provide a noninvasive longitudinal measure of disease activity and a measure of submucosal fibrosis. Specifically, MRE may be used in assessing CD as follows:
▪ Evaluation of extent of small bowel disease at diagnosis;
▪ Evaluation of disease burden in the symptomatic patient to direct therapeutic management;
▪ Evaluation for fibrostenotic disease, which may respond better to surgery than escalation of medical therapy;
▪ Confirmation of clinical remission and consideration for escalation of medical therapy if there is persistent submucosal disease despite clinical remission;
▪ Evaluation of intra-abdominal complications, including fistulae, tethering, stenosis and abscess;
▪ Evaluation of perianal disease.
Ultimately, MRE will help improve patient outcomes by assisting clinicians in how to direct the important therapeutic decisions of medical and surgical management.
Conclusion
MRE has evolved to produce reproducible high-quality examinations of the small and large bowel to a degree that significantly advances sensitivity and specificity for CD changes. Much of the published comparative literature on MRE is sufficiently old that it was not obtained using current optimized techniques, and this observation accounts for the large range of results. In our experience, CT does not match MRE for producing the soft-tissue contrast useful to reliably delineate between inflammation and chronic changes related to fibrosis. Both of these processes may look identical on CT. On MRE, T2 signal increases with inflammation and edema, a marker of active CD [28]. The use of single-shot T2 combined with fat-suppression employing the SPAIR technique is critically important to optimize sensitivity and specificity for active CD on MRE [14,15,28]. The majority of earlier publications either did not use FS T2 or did not use SPAIR. Other forms of FS, using simple inversion–recovery or chemical shift spoiling, will be either affected by higher noise, less uniform FS, or increased through-plane motion sensitivity to bowel peristalsis [14].
MRE will not detect mild, early disease isolated to the mucosa. This accounts for different results when comparing MRE with endoscopic biopsy and capsule techniques with their detailed evaluation of the mucosa. However, submucosal and deeper disease is often under-represented on endoscopic examinations while detected in exquisite detail by MRE [28].
Future perspective
Current MRE techniques have a vital application in the evaluation, management and investigation of patients with CD. The application of MRE is limited by a lag in the medical community’s familiarity with the optimal imaging techniques and diagnostic interpretation; there is need for continued education and an improved understanding of the relationship between specific MRE findings and associated histopathology.
A limitation of MRE remains the motion sensitivity of the 3D gradient echo T1W acquisitions. New gradient echo methods are being developed that are expected to transform our capacity to acquire these images from freely breathing patients. Such technology will favorably impact patients who require sedation, such as young pediatric subjects. There will also be benefits in reduction in image deterioration from bowel peristalsis.
We expect MRE will fundamentally change our approach to the management and first-line diagnosis of abdominal pain, the most prevalent and yet nonspecific symptom of CD. On the evaluation of disease etiology and therapy, we expect MRE to provide new insights into the relationship between submucosal disease and other related disease manifestations including fat wrapping (also known as creeping fat, i.e., mesenteric fat distorted by fibrotic retraction), mucosal alteration, bowel fibrostenosis and chronic changes of long-term medical therapy. The capacity for safe and noninvasive longitudinal evaluation of patients will facilitate more frequent diagnostic evaluations and allow clinicians to better orchestrate immunomodulatory therapy in the hope of altering the natural history of CD, the ultimate goal of therapeutic interventions. Interdisciplinary study of CD using advances in our understanding of MRE– pathology correlations may be expected to provide new insights into disease natural history and to better formulate medical and surgical interventions.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
Papers of special note have been highlighted as:
* of interest
* of considerable interest
- Brenner DJ, Hall EJ. Computed tomography – an increasing source of radiation exposure. N. Engl. J. Med. 357(22), 2277–2284 (2007).
- Fucic A, Brunborg G, Lasan R, Jezek D, Knudsen LE, Merlo DF. Genomic damage in children accidentally exposed to ionizing radiation: a review of the literature. Mutat. Res. 658(1–2), 111–123 (2008).
- Martin DR, Semelka RC. Health effects of ionising radiation from diagnostic CT. Lancet 367(9524), 1712–1714 (2006).
- Preston DL, Pierce DA, Shimizu Y et al. Effect of recent changes in atomic bomb survivor dosimetry on cancer mortality risk estimates. Radiat. Res. 162(4), 377–389 (2004).
- Preston DL, Ron E, Tokuoka S et al. Solid cancer incidence in atomic bomb survivors: 1958–1998. Radiat. Res. 168(1), 1–64 (2007).
- Preston DL, Shimizu Y, Pierce DA, Suyama A, Mabuchi K. Studies of mortality of atomic bomb survivors. Report 13: solid cancer and noncancer disease mortality: 1950–1997. Radiat. Res. 160(4), 381–407 (2003).
- Cardis E, Vrijheid M, Blettner M et al. The 15-Country Collaborative Study of Cancer Risk among Radiation Workers in the Nuclear Industry: estimates of radiationrelated cancer risks. Radiat. Res. 167(4), 396–416 (2007).
- Fazel R, Krumholz HM, Wang Y et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N. Engl. J. Med. 361(9), 849–857 (2009).
- Sodickson A, Baeyens PF, Andriole KP et al. Recurrent CT, cumulative radiation exposure, and associated radiation-induced cancer risks from CT of adults. Radiology 251(1), 175–184 (2009).
- Newnham E, Hawkes E, Surender A, James SL, Gearry R, Gibson PR. Quantifying exposure to diagnostic medical radiation in patients with inflammatory bowel disease: are we contributing to malignancy? Aliment. Pharmacol. Ther. 26(7), 1019–1024 (2007).
- Desmond AN, O’Regan K, Curran C et al. Crohn’s disease: factors associated with exposure to high levels of diagnostic radiation. Gut 57(11), 1524–1529 (2008).
- Palmer L, Herfarth H, Porter CQ, Fordham LA, Sandler RS, Kappelman MD. Diagnostic ionizing radiation exposure in a populationbased sample of children with inflammatory bowel diseases. Am. J. Gastroenterol. 104, 2816–2823 (2009).
- Patak MA, Mortele KJ, Ros PR. Multidetector row CT of the small bowel. Radiol. Clin. North Am. 43(6), 1063–1077 (2005).
- Lauenstein TC, Sharma P, Hughes T, Heberlein K, Tudorascu D, Martin DR. Evaluation of optimized inversion-recovery fat-suppression techniques for T2-weighted abdominal MR imaging. J. Magn. Reson. Imaging 27(6), 1448–1454 (2008). & Details the enhanced ability of the spectral adiabatic inversion recovery technique to provide augmented fat saturation and to furnish improved bowel wall delineation. Fat saturation helps to distinguish the high signal of edema from the elevated signal of fat. Overall, this technique improves our detection of inflammatory intra-abdominal processes, such as acute inflammation of active Crohn’s disease.
- Martin DR, Lauenstein T, Sitaraman SV. Utility of magnetic resonance imaging in small bowel Crohn’s disease. Gastroenterology 133(2), 385–390 (2007). & Details the updated protocol for the MR enterography (MRE) examination. This refined MRE technique relies upon 3D T1-weighted GRE with fat saturation and singleshot T2-weighted with fat saturation. The article describes the simplified eloquence of the technique, and the ability of the exam to be performed relatively quickly with an emphasis upon patient comfort and improved study compliance.
- Ajaj W, Lauenstein TC, Langhorst J et al. Small bowel hydro-MR imaging for optimized ileocecal distension in Crohn’s disease: should an additional rectal enema filling be performed? J. Magn. Reson. Imaging 22(1), 92–100 (2005).
- Narin B, Ajaj W, Gohde S et al. Combined small and large bowel MR imaging in patients with Crohn’s disease: a feasibility study. Eur. Radiol. 14(9), 1535–1542 (2004).
- Mary JY, Modigliani R. Development and validation of an endoscopic index of the severity for Crohn’s disease: a prospective multicentre study. Groupe d’Etudes Therapeutiques des Affections Inflammatoires du Tube Digestif (GETAID). Gut 30(7), 983–989 (1989).
- Mako EK, Mester AR, Tarjan Z, Karlinger K, Toth G. Enteroclysis and spiral CT examination in diagnosis and evaluation of small bowel Crohn’s disease. Eur. J. Radiol. 35(3), 168–175 (2000).
- Miao YM, Koh DM, Amin Z et al. Ultrasound and magnetic resonance imaging assessment of active bowel segments in Crohn’s disease. Clin. Radiol. 57(10), 913–918 (2002).
- Erber WF, Erber JA. Meta-analysis of the yield of capsule endoscopy in patients with Crohn’s disease. Am. J. Gastroenterol. 101(11), 2669 (2006).
- Udayasankar U, Lauenstein T, Burrow B, Sitaraman S, Rutherford R, Martin D. Evaluation of Crohn’s disease activity using MRI: correlation with T2 signal intensity on fat-suppressed single shot imaging. Presented at: International Society of Magnetic Resonance Medicine. Berlin, Germany, 19–25 May 2007.
- Florie J, Wasser MN, Arts-Cieslik K, Akkerman EM, Siersema PD, Stoker J. Dynamic contrast-enhanced MRI of the bowel wall for assessment of disease activity in Crohn’s disease. Am. J. Roentgenol. 186(5), 1384–1392 (2006).
- Rimola J, Rodriguez S, Garcia-Bosch O et al. Magnetic resonance for assessment of disease activity and severity in ileocolonic Crohn’s disease. Gut 58, 1113–1120 (2009).
- Ajaj WM, Lauenstein TC, Pelster G et al. Magnetic resonance colonography for the detection of inflammatory diseases of the large bowel: quantifying the inflammatory activity. Gut 54(2), 257–263 (2005).
- Maccioni F, Bruni A, Viscido A et al. MR imaging in patients with Crohn disease: value of T2- versus T1-weighted gadoliniumenhanced MR sequences with use of an oral superparamagnetic contrast agent. Radiology 238(2), 517–530 (2006).
- Martin DR, Danrad R, Herrmann K, Semelka RC, Hussain SM. Magnetic resonance imaging of the gastrointestinal tract. Top Magn. Reson. Imaging. 16(1), 77–98 (2005). & Details an early approach to a comprehensive MR examination of the gastrointestinal tract. The MR technique emphasizes the importance of T1-weighted GRE with fat saturation, single-shot T2-weighted with and without fat saturation, and balanced steady-state free precession imaging. The technique’s overall enhanced signal-to-noise ratio, rapid acquisition and motion insensitivity facilitates detection of inflammatory, infectious and neoplastic pathology.
- Udayasankar UK, Martin D, Lauenstein T et al. Role of spectral presaturation attenuated inversion-recovery fat-suppressed T2-weighted MR imaging in active inflammatory bowel disease. J. Magn. Reson. Imaging 28(5), 1133–1140 (2008). & Details the high accuracy of T2-weighted imaging with fat saturation to measure inflammation and acute disease activity as compared with endoscopy, biopsy and surgical pathology. In addition, the authors detail how MRE effectively evaluates the extent of submucosal disease. While MRE is insensitive to early changes of disease affecting the mucosa, coupling the MRE with either endoscopy, capsule endoscopy or biopsy promises a comprehensive and complete examination of inflammatory bowel pathology, targeting both mucosal and submucosal extent of disease.
- Shoenut JP, Semelka RC, Magro CM, Silverman R, Yaffe CS, Micflikier AB. Comparison of magnetic resonance imaging and endoscopy in distinguishing the type and severity of inflammatory bowel disease. J. Clin. Gastroenterol. 19(1), 31–35 (1994).
- Ochsenkuhn T, Herrmann K, Schoenberg SO, Reiser MF, Goke B, Sackmann M. Crohn disease of the small bowel proximal to the terminal ileum: detection by MR-enteroclysis. Scand. J. Gastroenterol. 39(10), 953–960 (2004).
- Albert JG, Martiny F, Krummenerl A et al. Diagnosis of small bowel Crohn’s disease: a prospective comparison of capsule endoscopy with magnetic resonance imaging and fluoroscopic enteroclysis. Gut 54(12), 1721–1727 (2005).
- Sempere GA, Martinez Sanjuan V, Medina Chulia E et al. MRI evaluation of inflammatory activity in Crohn’s disease. Am. J. Roentgenol. 184(6), 1829–1835 (2005).
- Best WR, Becktel JM, Singleton JW, Kern F Jr. Development of a Crohn’s disease activity index. National Cooperative Crohn’s Disease Study. Gastroenterology 70(3), 439–444 (1976).
- Harvey RF, Bradshaw JM. A simple index of Crohn’s-disease activity. Lancet 1(8167), 514 (1980).
- Hyams JS, Ferry GD, Mandel FS et al. Development and validation of a pediatric Crohn’s disease activity index. J. Pediatr. Gastroenterol. Nutr. 12(4), 439–447 (1991).
- Koh DM, Miao Y, Chinn RJ et al. MR imaging evaluation of the activity of Crohn’s disease. Am. J. Roentgenol. 177(6), 1325–1332 (2001).
- Martinez MJ, Ripolles T, Paredes JM, Blanc E, Marti-Bonmati L. Assessment of the extension and the inflammatory activity in Crohn’s disease: comparison of ultrasound and MRI. Abdom. Imaging 34(2), 141–148 (2009).
- Schunk K, Kern A, Oberholzer K et al. Hydro-MRI in Crohn’s disease: appraisal of disease activity. Invest. Radiol. 35(7), 431–437 (2000).
- Gourtsoyiannis N, Papanikolaou N, Grammatikakis J, Papamastorakis G, Prassopoulos P, Roussomoustakaki M. Assessment of Crohn’s disease activity in the small bowel with MR and conventional enteroclysis: preliminary results. Eur. Radiol. 14(6), 1017–1024 (2004). & Was performed with an older MRE technique. Even within these limitations, the study demonstrates the ability of MRE to at least equal the fidelity of small bowel follow-through for localizing and estimating the length and extent of bowel with ulcerations and strictures. Current MRE techniques utilize far more advanced dynamic contrast-enhanced GRE imaging and relatively motion insensitive single-shot T2-weighted imaging with fat saturation.
- Madsen SM, Thomsen HS, Munkholm P et al. Inflammatory bowel disease evaluated by low-field magnetic resonance imaging. Comparison with endoscopy, 99mTc- HMPAO leucocyte scintigraphy, conventional radiography and surgery. Scand. J. Gastroenterol. 37(3), 307–316 (2002).
- Del Vescovo R, Sansoni I, Caviglia R et al. Dynamic contrast enhanced magnetic resonance imaging of the terminal ileum: differentiation of activity of Crohn’s disease. Abdom. Imaging 33(4), 417–424 (2008).
- Maccioni F, Viscido A, Broglia L et al. Evaluation of Crohn disease activity with magnetic resonance imaging. Abdom. Imaging 25(3), 219–228 (2000).
- Alexopoulou E, Roma E, Loggitsi D et al. Magnetic resonance imaging of the small bowel in children with idiopathic inflammatory bowel disease: evaluation of disease activity. Pediatr. Radiol. 39(8), 791–797 (2009).
- Laghi A, Borrelli O, Paolantonio P et al. Contrast enhanced magnetic resonance imaging of the terminal ileum in children with Crohn’s disease. Gut 52(3), 393–397 (2003).
- Gee MS, Nimkin K, Hsu M et al. Original research: prospective evaluation of MR enterography as the primary imaging modality for pediatric Crohn’s disease assessment. Am. J. Roentgenol. 197, 224–231 (2011).
- Golder SK, Schreyer AG, Endlicher E et al. Comparison of capsule endoscopy and magnetic resonance (MR) enteroclysis in suspected small bowel disease. Int. J. Colorectal. Dis. 21(2), 97–104 (2006).
- Tillack C, Seiderer J, Brand S et al. Correlation of magnetic resonance enteroclysis (MRE) and wireless capsule endoscopy (CE) in the diagnosis of small bowel lesions in Crohn’s disease. Inflamm. Bowel Dis. 14(9), 1219–1228 (2008).
- Frokjaer JB, Larsen E, Steffensen E, Nielsen AH, Drewes AM. Magnetic resonance imaging of the small bowel in Crohn’s disease. Scand. J. Gastroenterol. 40(7), 832–842 (2005).
- Lee SS, Kim AY, Yang SK et al. Crohn disease of the small bowel: comparison of CT enterography, MR enterography, and small-bowel follow-through as diagnostic techniques. Radiology 251(3), 751–761 (2009).
- Masselli G, Casciani E, Polettini E, Gualdi G. Comparison of MR enteroclysis with MR enterography and conventional enteroclysis in patients with Crohn’s disease. Eur. Radiol. 18(3), 438–447 (2008).
- Darge K, Anupindi SA, Jaramillo D. MR imaging of the abdomen and pelvis in infants, children, and adolescents. Radiology 261(1), 12–29 (2011).
- Anupindi SA, Ayyala R, Kelsen J, Mamula P, Applegate KE. Imaging of inflammatory bowel disease in children. In: Evidence Based Imaging: Improving the Quality of Imaging in Patient Care. Medina LS, Blackmore CC, Applegate KE (Eds). Springer, Tarporley, UK, 571–591 (2011).
- Quencer K, Nimkin K, Kenudson MM, Gee M. MR-E vs CT-E in the detection and accuracy of characterizing active and chronic inflammation in pediatric Crohns disease. Presented at: RSNA 2011. 97th Scientific Assembly and Annual Meeting. Chicago, IL, USA, 27 November–2 December 2011.
- Low RN, Francis IR, Politoske D, Bennett M. Crohn’s disease evaluation: comparison of contrast-enhanced MR imaging and single-phase helical CT scanning. J. Magn. Reson. Imaging 11(2), 127–135 (2000).
- Siddiki HA, Fidler JL, Fletcher JG et al. Prospective comparison of state-of-the-art MR enterography and CT enterography in small-bowel Crohn’s disease. Am. J. Roentgenol. 193(1), 113–121 (2009).
- Schmidt S, Lepori D, Meuwly JY et al. Prospective comparison of MR enteroclysis with multidetector spiral-CT enteroclysis: interobserver agreement and sensitivity by means of ‘sign-by-sign’ correlation. Eur. Radiol. 13(6), 1303–1311 (2003).
- Horsthuis K, Bipat S, Bennink RJ, Stoker J. Inflammatory bowel disease diagnosed with US, MR, scintigraphy, and CT: meta-analysis of prospective studies. Radiology 247(1), 64–79 (2008).
- Punwani S, Rodriguez-Justo M, Bainbridge A et al. Mural inflammation in Crohn disease: location-matched histologic validation of MR imaging features. Radiology 252(3), 712–720 (2009). & Details the ability of current MRE techniques to estimate disease pathology comparable to histology of surgical specimens. For submucosal disease, MRE imaging provides complete evaluation of disease extent. MRE is only limited in evaluation of early disease confined to the mucosa.
- Lawrance IC, Welman CJ, Shipman P, Murray K. Correlation of MRI-determined small bowel Crohn’s disease categories with medical response and surgical pathology. World J. Gastroenterol. 15(27), 3367–3375 (2009).
- Wilson SR, Burns PN. Microbubbleenhanced US in body imaging: what role? Radiology 257(1), 24–39 (2010).
- Malagò R, D’Onofrio M, Mantovani W. Contrast-enhanced ultrasonography (CEUS) vs. MRI of the small bowel in the evaluation of Crohn’s disease activity. Radiol. Med. 117(2), 268–281 (2012).