Research Article - International Journal of Clinical Rheumatology (2020) Volume 15, Issue 3
Frequency and outcomes of venous thrombus embolism in hospitalized patients with Behçet's disease
- Corresponding Author:
- Christopher G. Gibson
Department of Internal Medicine
Fairfield Medical Center, Lancaster, Ohio, USA
E-mail: drcgibson@fmchealth.org
Abstract
Background: Behçet’s Disease (BD) is a multisystem vasculitis characterized by skin-mucosa lesions, ocular, musculoskeletal, gastrointestinal, neurologic, and major vessel involvement. The objective of this present study was to investigate BD in the inpatient setting and the associated risk of contracting venous thrombus embolism. Methods: We utilized the Healthcare Cost and Utilization Project’s National Inpatient Sample (NIS) database. The NIS is the largest inpatient care database in the United States, containing demographic and clinical information from approximately 8 million hospital stays from about 1000 hospitals sampled to approximate a 20% stratified sample of U.S. community hospitals. The 2016 NIS sample utilized ICD-10-CM/PCS diagnostic and procedure codes. Results: The 2016 NIS analysis was performed using 7,135,090 discharge summaries, of which 622 were "case" summaries associated with the ICD-10 code for Behçet's disease (M352). Case discharge summaries were also associated with a slightly longer hospital stay 5.6 days compared to 4.7 days. The percentage of VTE-related ICD codes was 2.8 times higher in case compared to control summaries (P = 4.4e-35). Overall, approximately 1 in 5 case summaries (19.45%) was linked to a VTErelated ICD code, compared to only 6.85% of control summaries. These trends were consistent in analyses performed for each sex separately. Case-male summaries were more frequently associated with VTE-related codes (28.19%) compared to case-female summaries (15.7%). Conclusion: Our study illustrates the association of BD and VTE-related ICD events.
Keywords
Behçet’s disease • epidemiology • inflammation • deep vein thrombosis • pulmonary embolism
Introduction
Behçet’s Disease (BD) is a multisystem inflammatory disease with an obscure etiology and origin. Hulusi Behçet, a Turkish dermatologist, was the first to describe what classically became known as the triad of oral ulcers, genital lesions, and recurrent eye inflammation. Vascular disease develops in up to 40% of the patients with BD with venous involvement occurring more commonly than arterial disease [1], and is seen mostly in the Mediterranean Basin, the Middle East, and the Far East [2]. The frequency is less common in Western Europe and the United States [2]. The age of usual onset of the disease is in the third decade, and its course is characterized by exacerbations and remissions with the etiopathogenesis still unknown [3]. Studies have shown that both genders are affected equally, but often with young men experiencing a more severe course [2]. There is no specific serological test available, and as such, the diagnosis is based on several criteria, the most widely used being those of the International Group Study on BD [4]. Because of the diversity of blood vessels that it affects, manifestations of BD may occur at many sites throughout the body, however, the disease has a predilection for certain organs and tissues. In the respiratory system, for example, the main features of pulmonary involvement in BD include arterial and venous thrombosis, pulmonary artery aneurysms, pulmonary infarction, recurrent pneumonia and pleurisy [5]. BD has also been shown to involve the gastrointestinal system. The most involved regions of the gastrointestinal tract are the ileocecal region and the colon [6,7]. The liver, pancreas, and spleen are rarely involved. The symptoms associated with these extra-oral manifestations of BD are abdominal pain, nausea, vomiting, diarrhea with or without blood, and constipation [6,7]. BD is known to cause an immune-inflammatory state yet there is a paucity of literature that demonstrates an increased risk of Venous Thromboembolism (VTE), i.e. Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE) [1].
DVT, is the most common type of venous thrombosis, especially in the lower extremities compared to the upper extremities [8]. Lower Extremity DVT (LEDVT) makes up 60-80% of all vascular lesions [8,9]. It is often found in patients that the LEDVT often occurs within the first few years of disease onset [9]. Vascular involvement tends to undergo a relapsing and remitting course, with a relapse rate of 38.4% at 5 years in a retrospective cohort [10].
The management of LEDVT in patients with recurrent episodes mainly consists of immunosuppressive agents such as Azathioprine and corticosteroids [8-10]. Depending on the hospital location, some hospitals will routinely use additional anticoagulants as part of their protocol when treating patients with BD [7-10]. Our aim in this study was to utilize a large database to demonstrate the frequency of VTE in hospitalized patients with known Behçet’s disease compared to the general population within the United States.
Methods
We utilized the Healthcare Cost and Utilization Project (HCUP) and the National Inpatient Sample (NIS) database. The NIS is the largest inpatient care database in the United States, containing demographic and clinical information from approximately 8 million hospital stays from about 1000 hospitals sampled to approximate a 20% stratified sample of U.S. community hospitals [3]. In this sample, hospitals are divided into strata based on U.S. region, urban/rural location, teaching status, bed size, and ownership. Sampling probabilities are proportional to the number of hospitals in each stratum. No unique patient identifiers are contained in the NIS. Information available for each hospitalization includes general hospital characteristics as well as patient information such as age, gender, race, quartile of median income based on patient ZIP code, and diagnostic and procedure codes form the International Classification of Diseases (ICD).
The 2016 NIS sample utilized ICD-10-CM/PCS diagnostic and procedure codes. To identify “case” discharge summaries associated with BD, we utilized the M352 diagnostic code. To identify a collection of VTEassociated diagnostic codes, we searched using the terms “embolism”, “embolic”, “thrombosis”, “postthrombotic”, “thrombophlebitis”, and “budd-chiari syndrome.” This identified a set of 472 ICD-10 diagnostic codes that we designated as VTE-related. The presence or absence of any VTE-related code with a discharge summary was our primary (binary) endpoint. Further sub-analyses were performed using binary variables corresponding to specific VTE-related codes identified during the analysis. A chi-squared test was used to test for an association between discharge summaries with VTE-related codes and BD. The strength of association was quantified in terms of risk ratios, frequency of VTE-related codes in case discharge summaries or frequency of VTE-related codes in control discharge summaries.
Results
The 2016 NIS analysis was performed using 7,135,090 discharge summaries, of which 622 were "case" summaries associated with the ICD-10 code for BD (M352) (Table 1). The average age of patients was 46.8 years of age compared to control discharge summaries of 55.6 years. Of the patients diagnosed with BD, 69.6% were female patients vs 56.7% of men. The patients with Behçet’s disease had an average hospital stay of 5.6 days and an average total charge of $57K.
Table 1. Comparison of discharge summaries from patients with Behçet’s disease (case) and patient’s without Behçet’s disease (control).
| Control | Case (Behçet’s) | |
|---|---|---|
| No. discharges | 7134468 | 622 |
| Age (SD) | 55.6 (22.1) | 46.8 (17.1) |
| Length of Stay (SD) | 4.7 (6.9) | 5.6 (7.5) |
| Total Charges (SD) | $47,018 (90687.5) | $57,415.3 (113116.2) |
| No. male (%) | 3085882 (43.3%) | 188 (30.2%) |
| No. female (%) | 4044397 (56.7%) | 433 (69.6%) |
| White (%) | 4425407 (62%) | 425 (68.3%) |
| Black (%) | 1029224 (14.4%) | 83 (13.3%) |
| Other race (%) | 1312760 (18.4%) | 80 (12.9%) |
| Lowest income quartile (%) | 2152763 (30.2%) | 137 (22%) |
| Highest income quartile (%) | 1399796 (19.6%) | 152 (24.4%) |
The table shows average values with standard deviation or the absolute number and percentage of discharge summaries. The analysis was performed using the 2016 NIS sample.
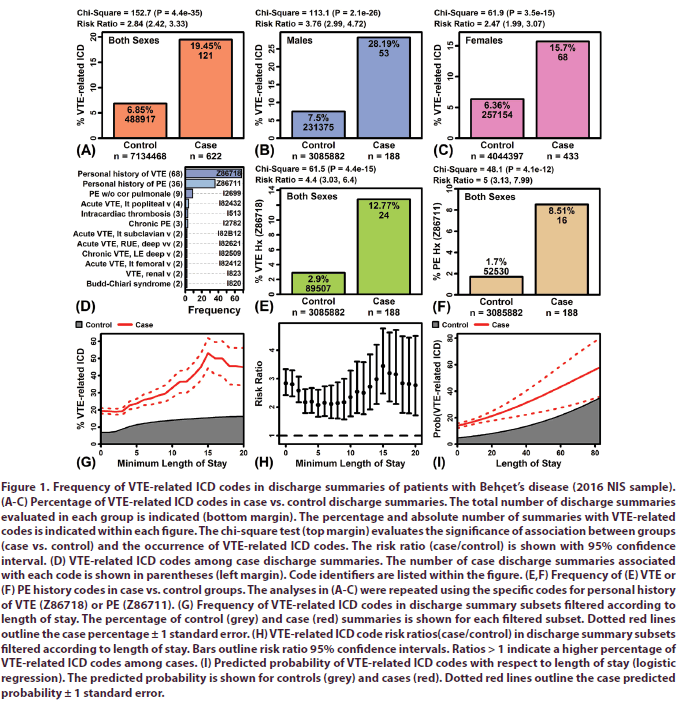
The percentage of VTE-related ICD codes was 2.8 times higher in case compared to control summaries (P = 4.4e-35; Figure 1A). Overall, approximately 1 in 5 case summaries (19.45%) was linked to a VTE-related ICD code, compared to only 6.85% of control summaries (Figure 1A). These trends were consistent in analyses performed for each sex separately (Figures 1B and 1C). Notably, however, case-male summaries were more frequently associated with VTE-related codes (28.19%) compared to case-female summaries (15.7%) (Figures 1B and 1C).
Figure 1: Frequency of VTE-related ICD codes in discharge summaries of patients with Behçet’s disease (2016 NIS sample). (A-C) Percentage of VTE-related ICD codes in case vs. control discharge summaries. The total number of discharge summaries evaluated in each group is indicated (bottom margin). The percentage and absolute number of summaries with VTE-related codes is indicated within each figure. The chi-square test (top margin) evaluates the significance of association between groups (case vs. control) and the occurrence of VTE-related ICD codes. The risk ratio (case/control) is shown with 95% confidence interval. (D) VTE-related ICD codes among case discharge summaries. The number of case discharge summaries associated with each code is shown in parentheses (left margin). Code identifiers are listed within the figure. (E,F) Frequency of (E) VTE or (F) PE history codes in case vs. control groups. The analyses in (A-C) were repeated using the specific codes for personal history of VTE (Z86718) or PE (Z86711). (G) Frequency of VTE-related ICD codes in discharge summary subsets filtered according to length of stay. The percentage of control (grey) and case (red) summaries is shown for each filtered subset. Dotted red lines outline the case percentage ± 1 standard error. (H) VTE-related ICD code risk ratios(case/control) in discharge summary subsets filtered according to length of stay. Bars outline risk ratio 95% confidence intervals. Ratios > 1 indicate a higher percentage of VTE-related ICD codes among cases. (I) Predicted probability of VTE-related ICD codes with respect to length of stay (logistic regression). The predicted probability is shown for controls (grey) and cases (red). Dotted red lines outline the case predicted probability ± 1 standard error.
The VTE-related ICD codes most commonly associated with case discharge summaries included a personal history of VTE (Z86718), personal history of PE (Z86711), and PE without cor pulmonale (I2699) (Figure 1D). Overall, 104 case discharge summaries were linked to ICD codes associated with personal history of VTE or PE (i.e., Z86718 and Z86711). The prior analyses were repeated using these two codes specifically, rather than the more heterogeneous group of VTE-related codes. This revealed similar trends, with 4-5 times greater frequency of these codes among cases compared to control discharge summaries (Figures 1E and 1F).
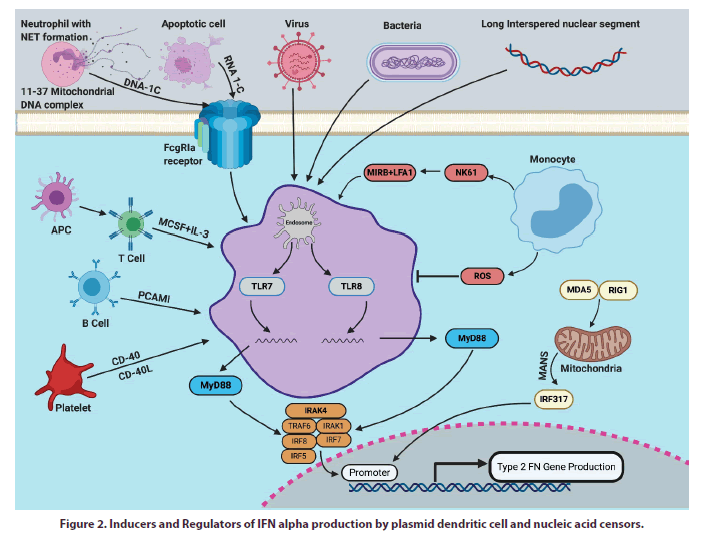
• The percentage of VTE-related ICD codes was higher in discharge summaries associated with longer hospital stays (Figure 1G). This trend was observed in both case and control summaries, although was slightly more prominent in case summaries (Figure 1G). Approximately 20% of all case summaries were linked to a VTE-related ICD code, but this percentage increased to 50% among summaries associated with a length of stay 15 days or longer (Figure 1G). Consistent with this, the risk ratio (case/control) for VTE-related codes was slightly higher considering only summaries with a length of stay greater than 15 days (Figure 1H). Predicted probability of VTE, generated from logistic regression models with sex and age as covariates, was also increased in discharge summaries associated with longer length of stay (Figures 1I and 2) [11-14].
Discussion
BD is an inflammatory condition that can affect multiple organ systems including involvement of the blood vessels causing vasculitis. Thromboembolic complications have been a significant contributor to the morbidity and mortality of BD (24). The purpose of our study was to examine the hospitalized patients with known BD and compare the rates of VTE to the general population within the United States. Previous studies have typically been limited to countries were the disease is more endemic [3,4].
The strengths of this study are the larger sample size, and a potentially more diverse patient population than previous studies. Sampling size was also proportional to the different stratums in the NIS and HCUP. However, limitations of this study are the retrospective nature of the study which included only patients who have been hospitalized [15-24].
Gender predilection for BD has not been established. A review article studied the male to female ratio (M/F) of BD in 33 countries. Male predominance was noted in 19 countries, female predominance in 7 countries, and equal distribution in 6 countries [25]. Our study also demonstrated a higher incidence of BD among women in the United States than men. This is consistent with the observations reported in a previous study by Calamia KT et al. [2]. However, further epidemiological research is needed to determine if there is a female predominance for BD in the United States.
Personal history of DVT and personal history of PE were the most frequent ICD codes. Our study shows that the rate of thrombus formation is elevated in patients with BD within the population of the United States. This is consistent previous studies that have shown BD have been associated with DVTs and more rarely pulmonary embolisms [26,27]. The hospitalized men with BD had higher rates of VTE than females and the control group. This confirms what has been established in prior studies with men having a high risk of vascular involvement in BD [3,26].
Conclusion
We also found that BD patients with a VTE associated ICD code had with prolonged length of hospital stay. Further investigation is needed to determine if people with BD are more likely to develop a thrombus during a hospital stay or if a VTE ICD code on admission is associated with a longer hospital stay. In conclusion, our study illustrates the association of BD and VTE-related ICD events.
Confidentiality and records
Any identifying information was removed, the Office of Human Research Protections for Mount Carmel Health System and the Institutional Review Board approved of this paper.
Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- HCUP Databases. Healthcare Cost and Utilization Project (HCUP). 2015-2016. Agency for Healthcare Research and Quality, Rockville, MD.
- Calamia KT, Wilson FC, Icen M et al. Epidemiology and clinical characteristics of Behçet's disease in the US: a population-based study. Arthritis. Rheum. 61(5), 600–604 (2009).
- Düzgün N, Ateş A, Aydintuğ OT et al. Characteristics of vascular involvement in Behçet's disease. Scandinavian Journal of Rheumatology. 35(1), 65–68 (2006).
- Aline T, Noël A, El-Rassi B et al. Vascular manifestations of Behçet's disease. Joint. Bone. Spine. 70(5), 384–389 (2003).
- Erkan F, Gul A, Tasali E. Pulmonary manifestations in Behcet's disease, Thorax. 56(7), 572–578 (2001).
- Baş Y, Güney G, Uzbay P et al. Colon perforation and Budd-Chiari syndrome in Behçet's disease. Am. J. Case. Rep. 16, 262–267 (2015).
- Bayraktar Y, Ozaslan E, Van Thiel DH. Gastrointestinal manifestations of Behcet's disease. J. Clin. Gastroenterol. 30(2), 144–154 (2000).
- Tascilar K, Melikoglu M, Ugurlu S et al. Vascular involvement in Behcet’s syndrome: a retrospective analysis of associations and the time course. Rheumatology. 53(11), 2018–2022 (2014).
- Desbois AC, Wechsler B, Resche-Rigon M et al. Immunosuppressants reduce venous thrombosis relapse in Behcet’s disease. Arthritis. Rheum. 64(8), 2753–2760 (2012).
- Alibaz-Oner F, Karadeniz A, Ylmaz S et al. Behc¸et disease with vascular involvement: effects of different therapeutic regimens on the incidence of new relapses. Medicine. 94(6), e494 (2015).
- Seyahi E, Yazici H. To anticoagulate or not to anticoagulated vascular thrombosis in Behçet’s syndrome: an enduring question. Clin. Exp. Rheumatol. 34(1 Suppl 95), S3–S4 (2016).
- Merashli M, Ster IC, Ames PR. Subclinical atherosclerosis in Behcet’s disease: a systematic review and meta-analysis. Semin. Arthritis. Rheum. 45(4), 502–510 (2016).
- Sacre K, Ducrocq G, Hernigou A et al. Unusual cardiovascular events in Behçet’s disease. Clin. Exp. Rheumatol. 28(Suppl. 60), S82e5 (2010).
- Desbois AC, Wechsler B, Resche-Rigon M et al. Immunosuppressants reduce venous thrombosis relapse in Behçet’s disease. Arthritis. Rheum. 64(8), 2753–2760 (2012).
- Yazici H, Tuzun Y, Pazarli H et al. Influence of age of onset and patient’s sex on the prevalence and severity of manifestations of Behcet’s syndrome. Ann. Rheum. Dis. 43(6), 783–789 (1984).
- Hatemi G, Melikoglu M, Tunc R et al. Apremilast for Behçet’s syndrome-a phase 2, placebo-controlled study. N. Engl. J. Med. 372(16), 1510–1518 (2015).
- Yazici H, Ugurlu S, Seyahi E. Behçet syndrome: is it one condition? Clin. Rev. Allergy. Immunol. 43(3), 275–280 (2012).
- Ko GY, Byun JY, Cho BG et al. The vascular manifestations of Behçet’s disease: angiographic and CT findings. Br. J. Radiol. 73(876), 1270–1274 (2000).
- de Jesus H, Rosa M, Queiroz MV. Vascular involvement in Behcet’s disease. An analysis of twelve cases. Clin. Rheumatol. 16(2), 220–221 (1997).
- Kural-Seyahi E, Fresko I, Seyahi N. The long-term mortality and morbidity of Behc¸ et syndrome: a 2-decade outcome survey of 387 patients followed at a dedicated center. Medicine. 82(1), 60–76 (2003).
- Seyahi E, Memisoglu E, Hamuryudan V et al. Coronary atherosclerosis in Behcet’s syndrome: a pilot study using electron-beam computed tomography. Rheumatology. 43(11), 1448–1450 (2004).
- Caliskan M, Gullu H, Yilmaz S et al. Cardiovascular prognostic value of vascular involvement in Behcet’s disease. Int. J. Cardiol. 125(3), 428-430 (2007).
- Tascilar K, Melikoglu M, Ugurlu S et al. Vascular involvement in Behçet’s syndrome: a retrospective analysis of associations and the time course. Rheumatology (Oxford). 53(11), 2018–2022 (2014).
- Gaffo AL. Thrombosis in vasculitis. Best. Pract. Res. Clin. Rheumatol. 27(1), 57–67 (2013).
- Davatchi F, Chams-Davatchi C, Shams H et al. Behcet's disease: epidemiology, clinical manifestations, and diagnosis. Expert. Rev. Clin. Immunol. 13(1), 57e65 (2017).
- Houman MH, Ben Ghorbel I, Khiari Ben Salah I et al. Deep vein thrombosis in Behçet's disease. Clin. Exp. Rheumatol. 19(5 Suppl 24), S48–S50 (2001).
- Hammami S, Addad F, Kaoubaa N et al. Embolie pulmonaire et maladie de Behçet [Pulmonary embolism and Behçet's disease]. Arch. Mal. Coeur. Vaiss. 99(9), 786–790 (2006).