Research Article - Diabetes Management (2017) Volume 7, Issue 5
Economic burden of type 2 diabetes mellitus complications among patients in the eastern region of Ghana: A descriptive cross-sectional cost-of-illness study
- *Corresponding Author:
- Moses Kweku Sekyi Aikins
Department of Health Policy
Planning and Management
School of Public Health
College of Health Sciences
University of Ghana
Legon, Accra, Ghana
E-mail: mksaikins@ug.edu.gh
Abstract
Objective: To assess the economic burden associated with the management of type 2 diabetes with complications from patients of the Eastern Regional Hospital’s Diabetic Clinic of the Eastern Region of Ghana. Methods: The study is a descriptive cross sectional cost-of-illness study which was carried out in May, 2016 among 258 diabetes patients. Participants were selected by systematic random sampling and informed consent was signed. A pretested structured questionnaire was used for data collection. The data were entered into Epi-Info version 7 and analyzed using Microsoft Excel version 13 and STATA version 13. Kruskal-Wallis and Wilcoxon Rank Sum tests were used to determine statistical significance in cost difference. Total healthcare management cost was estimated and average cost determined. Intangible cost burden was analyzed using the 5-dimension Likert scale and the tertile descriptive statistics. Sensitivity analyses was conducted to test robustness of the cost estimates. Results: About 68% (n=175) of type 2 diabetes patients with complications were above 55 years. The estimated total healthcare management cost was US$9,980.62, with direct healthcare management cost constituting about 94%. The average healthcare management cost was US$38.68 (95% CI: 5.53-71.84). Patients on treatment for 5 years and above incurred significantly higher direct cost compared to those below 5 years, US$40.03 ± 40.71 (p<0.05). Patients incur moderate intangible cost burden. There was no statistically significant relationship between intangible cost burden and all the socio-demographic characteristics of patients. Conclusion: The findings suggest considerable economic burden associated with healthcare management of type 2 diabetes with complications, particularly in the elderly. The longer a patient stays with the disease, the significantly higher average direct cost incurred per month. Diabetes prevention strategies and, patient’s regular physical activities and proper dietary plan are highly recommended.
Keywords
type 2 diabetes, complications, economic burden, cost, Ghana
Introduction
Non-communicable diseases (NCDs) will become the leading cause of mortality worldwide by 2030 [1]. Non-communicable disease burden is now among the top five diseases which poses severe economic risk globally [2]. It leads to substantial economic losses in developing economies as a result of reduced productivity due to lost work hours, sub-optimal performance through physical and psychological problems, early retirement, reduced life expectancy and death [3,4]. Non-communicable diseases and for that matter diabetes contrary to popular view, disproportionally affect the poor who are most vulnerable to disease complications and mortality [5]. In Ghana, diabetes was among the top three NCD of Out-patient Department (OPD) cases, increasing from 39,789 in 2005 to 156,076 in 2010 [5].
Diabetes is a chronic, metabolic and progressive disease that affects the body’s ability to use the energy found in food. Uncontrolled diabetes over time causes hyperglycemia which leads to complications. The global prevalence of type 2 diabetes has risen substantially over the past few decades [6]. Complications associated with diabetes can be divided into micro vascular and macro vascular. Micro vascular complications occur due to damage to the small blood vessels whereas that of macro vascular occurs due to damage to larger blood vessels. Micro vascular complications involve damage to eyes (retinopathy) leading to blindness; kidneys (nephropathy) leading to renal failure; and nerves (neuropathy) leading to impotence. Macro vascular complications include cardiovascular such as heart attacks, strokes and severe foot disorders (foot ulcer) leading to amputation. The severe micro vascular and macro vascular complications due to diabetes mellitus has major implications for public health [7].
Diabetic neuropathy is one of the most common and problematic complication of diabetes mellitus which leads to severe morbidity, mortality, and a huge economic burden [7,8]. Most significant contribution to diabetes patients’ neuropathy morbidity is complications of the feet [9]. There is significantly long-term disability and premature mortality associated with foot ulceration and infection [10,11]. Other complications includes emotional distress [12], stroke [13], neural damage, foot ulcer, heart attack, kidney damage and blindness [6], and reduced life expectancy [14]. Furthermore, apart from these complications, the disease is often associated with certain comorbidities [15]. Diabetes, especially complicated diabetes is associated with great economic burden for patients, families, and society [16], these include direct, indirect and intangible costs [12,14,17- 19]. Diabetes patients with both micro vascular and macro vascular complications spend a total management cost of up to two-and-half times more compared to those without complications [20].
The cost-of-illness approach used in this study, measures costs associated with ill-health by categorizing into direct, indirect and intangible costs [21]. This approach has been used in numerous studies such as the estimation of outpatient care costs of type 2 diabetes mellitus [22]; estimation of cost of allergic rhinitis [23]; estimation of household costs of mental health care [24]; and estimation of the health facility cost of buruli ulcer wound treatment [25]. Reasonable number of studies have been conducted in developed countries on the cost of type 1 diabetes, however, studies on type 2 diabetes though prevalent are scarce. This study applied the cost-of-illness approach to estimate the economic burden of the management of type 2 diabetes among patients with complications receiving care in the Eastern region of Ghana.
Research design and methods
▪ Study design
This is a descriptive cross sectional cost-of-illness study, which was carried out May 2016 in the New Juaben Municipal of the Eastern Region of Ghana. The Municipality is one of the twenty six districts in the region, and has a population of 159,369 (about 52% female and 48% males) with a growth rate of 2.6% [26]. The regional capital is Koforidua which has the largest population. The economic activities in the municipality are agrobased (about 28%), industry (27%) and service (45%). There are various health facilities in the municipality. The Eastern Regional Hospital, the study site serves as a referral specialist hospital offering specialist medical and surgical care. One of the five major causes of Out-Patients- Department (OPD) attendance at the hospital was diabetes. The Eastern Regional Hospital’s Diabetic Clinic is the biggest in the region and caters for about 140 patients a week. Payment for health service delivery is both by insurance (national and private) and out-of-pocket. About 92% of diabetes patients were registered with the National Health Insurance Scheme [26].
▪ Study population
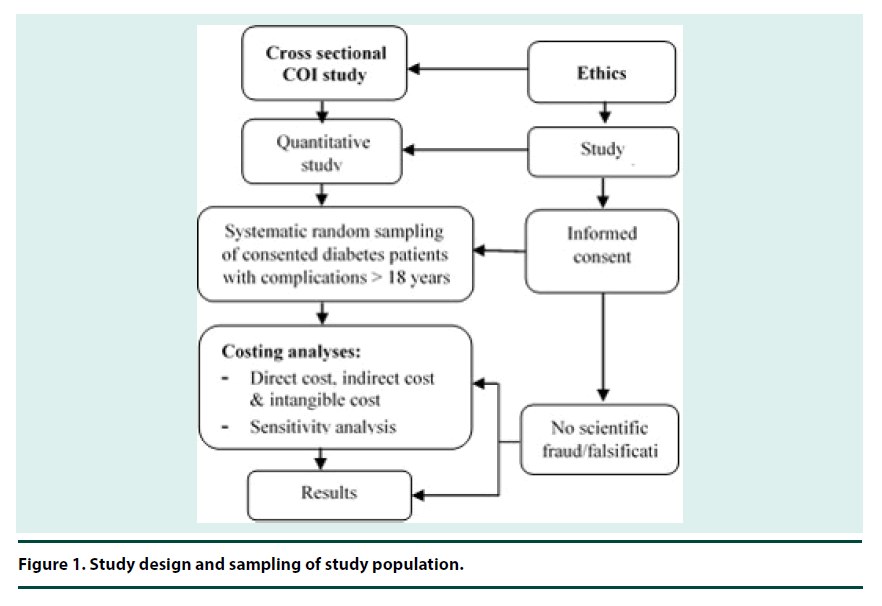
Patients with type 2 diabetes with complications were recruited using a systematic random sampling technique as shown in Figure 1. The hospital’s Diabetes Patients Register was used as the sampling frame with estimated registered diabetes patients of 560. Out of the master register, a list of type 2 diabetes patients with complications was compiled and their unique identification numbers were sorted in ascending order in Excel. The estimated study sample size was 258. The first patient was randomly selected, then subsequently, using an estimated sample interval of 2, all the other samples were selected.
The inclusion criteria were diabetes patients aged over 18 years with complications. The reason for the age threshold was to mitigate inclusion of unemployed patients. Thus, 258 diabetes patients with both micro vascular and macro vascular complications were sampled for the study.
▪ Data collection
Structured close-ended questionnaire was used for data collection. Data collected included demographics of type 2 diabetes patients with complications and costs (i.e., direct, indirect and intangible). Prior to data collection, Ethical approval was sought from the Ghana Health Service Ethics Review Committee (Ethical Approval–ID No: GHS-ERC: 13/12/15). Permissions were sought from the Eastern Regional Health Directorate, New Juaben Municipal Health Directorate and Eastern Regional Hospital Administration. Informed consent was obtained from sampled patients and they were assured of confidentiality and privacy before their participation in the study.
▪ Cost analysis
The data were entered into Epi-Info version 7. All cost analysis was carried out in Microsoft Excel version 13, and from the patient perspective. STATA version 13 was used to determine relationship between cost components and patients’ characteristics. Kruskal-Wallis and Wilcoxon Rank Sum tests were used to determine statistical significance in cost difference. P-value of less than 0.05 was considered significant. All the patient healthcare management cost estimates were costs incurred by patients within the month of the study. Table 1 provides details of the cost analyses. One-way and multi-way sensitivity analyses were carried out by varying critical costs components of the study (i.e., medications and wages) to test robustness of the cost estimates [27]. The cost of medicines and wages were varied by 3%. 5% and 7% similar to a study on household cost of seeking diabetes healthcare in Ghana [28]. Wage rate and medicine cost were selected due to uncertainty and variation in the cost data obtained.
| Cost type | Cost component | Cost Estimation Approach |
|---|---|---|
| Direct | Medical | Medicine: This was calculated by summing the cost incurred on drugs by patients. Consultation: This was calculated by summing the cost incurred on consultation and registration by patients. Diagnostics: This was calculated by summing the cost incurred on laboratory tests by patients. Other treatments cost: This was calculated by summing the cost incurred on other treatments by patients. Total medical cost: This was estimated by summing the cost incurred by patients on medical consultation, diagnostic test, other treatments and medication due to their diabetes disease. |
| Non-medical | Travel: This was calculated by summing the travel costs incurred by the patients when travelling to and from the hospital. Diet: This was calculated by summing the costs incurred by patients on food, drinks etc. Miscellaneous: This was calculated by summing other costs (e.g. phone calls made during treatment) incurred by the patients on other items due to the diabetes disease. Total non-medical cost: This was estimated by summing the cost incurred by patients on travel, diet and other miscellaneous costs due to their diabetes disease. |
|
| Total direct cost | This was the summation of the medical and non-medical costs. | |
| Indirect | Productivity losses due to health care seeking | Suhrcke et al’s human capital approach was used to estimate the productivity loses by patients [21]. This was sum of hours spent seeking healthcare by patient (travel, waiting and treatment times) |
| Other productivity losses | This was sum of total number of other productive work days lost to patients due to diabetes management activities other than healthcare seeking. | |
| Total indirect valuation | The total hours productivity losses (i.e., seeking health care and other productivity losses) was by multiplying by the average hourly earnings (i.e. US$2.05 per day). | |
| Total management cost | This was the summation of the total direct and total indirect costs. | |
| Intangible | Composite intangible cost | The composite intangible cost was obtained from responses to 5-dimension Likert scale questions in relation to physical pain, psychological pain, social relationship, functional limitation and quality of life. The aggregated score from the 5 dimensions were categorized into ‘low’ (13-30), ‘moderate’ (31-47) and ‘high’ (48-65) using the descriptive statistics tertile approach. Fisher’s exact test was conducted to determine association between intangible burden and patient sex and age. |
Table 1. Cost analysis of complicated type 2 diabetes healthcare management.
Results
The response rate was 100%. Table 2 shows that majority of the patients were aged 55 years or more with the mean age of 58 years (95% CI: 45-71). About 80% (n=207) of the patients were women, and 61% (n=158) had had primary school education. About 53% (n=137) of the patients were not married, and 52% (n=72) of them were employed, of which, 54% were traders. Seventy-one percent earned an average income of less than US$150.
| Item | Diabetes patients (N=258) | |
|---|---|---|
| N | % | |
| Age (years) | ||
| <35 | 14 | 5.5 |
| 35-44 | 15 | 5.8 |
| 45-55 | 54 | 20.9 |
| >55 | 175 | 67.8 |
| Sex | ||
| Men | 51 | 19.8 |
| Women | 207 | 80.2 |
| Educational level | ||
| No education | 49 | 19.0 |
| Primary | 158 | 61.2 |
| Secondary | 24 | 9.3 |
| Tertiary | 27 | 10.5 |
| Marital status | ||
| Married/living together | 121 | 46.9 |
| Not married | 137 | 53.1 |
| Employment status | ||
| Employed | 133 | 51.6 |
| Unemployed | 125 | 48.4 |
| Occupation1 | ||
| Trading | 72 | 54.1 |
| Farmer | 25 | 18.8 |
| Other | 36 | 27.1 |
| Average monthly income (from all sources)2 | ||
| ≤ US$150 | 183 | 70.9 |
| > US$150 | 75 | 29.1 |
| 1=Sample size of 133 2=US$1.00 equivalent to GHS3.90 (Bank of Ghana average monthly interbank exchange rate, June 2016) |
||
Table 2. Socio-demographic characteristics of study patients.
▪ Study diabetes patients’ health status and management
The mean number of years that study patients had been diagnosed with diabetes was 8 years (95% CI: 1-15). Majority of patients (80%) had their fasting blood sugar level above normal level of 6.1 mmol/dL with the mean fasting blood sugar level at 9.1 mmol/L (95% CI: 5.1-12.9). The studied patients had a wide-ranging complications, both micro vascular and macro vascular. Over 65% (n=169) of the patients had multiple complications (averagely 2 complications per patient). These included retinopathy, neuropathy, nephropathy, foot ulcer, dyslipidemia, skin condition, brain disorder, swollen/burning feet etc. Furthermore, more than two-third of the diabetics had hypertension (Tables 3 and 4).
| Complication | Diabetics (n=258) Number (%) | Drugs commonly used to manage type 2 diabetes and related complications |
|---|---|---|
| Microvascular | Insulin; Glibenclamide Tab; Metformin Tab; Pioglitazone Tab; Glimepiride; Acetylsalicylic Acid Tab; Losartan Tab; Nifedipine Tab; Amlodipine Tab; Lisinopril + Hydro Tab; Methylodopa Tab; Simvastatin; Spironolactone Tab; Erythromycin Tabs; Furosemide Tab; Atenolol; Amoxicillin Clavulanic acid; Cetinzine Tab; Bendroflume; Clotrimazole; Fluconazole; Miconazole; Cefuroxime; Mefedipin Tab; Tramadol; Allopurinol; Diazepan; Spironolactone tab; Clindemycin Caps; Omeprazole; Wartarin; Cuprofloxacin etc. | |
| Retinopathy | 124 (48.1) | |
| Neuropathy | 126 (48.8) | |
| Nephropathy | 8 (3.1) | |
| Macrovascular | ||
| Hypertension | 177 (68.6) | |
| Foot Ulcer | 13 (5.0) | |
| Brain Disorder | 31 (12.0) | |
| Dyslipidemia | 54 (21.0) | |
| Other conditions | ||
| Swollen/burning feet | 14 (5.4) | |
| Hearing impairment | 18 (7.0) | |
| Skin condition | 36 (14.0) | |
| Severe body pains | 10 (3.9) | |
Table 3. Complications of type 2 diabetics and drugs used.
| Number of Complication(s) | Diabetics (n=258) Number (%) |
Other conditions with type 2 diabetes |
|---|---|---|
| 1 | 89 (34.5) | Hypertension; Retinopathy; Neuropathy; Nephropathy; Foot Ulcer; Skin condition; Dyslipidemia; Swollen/burning feet; Severe body pains |
| 2 | 68 (26.4) | Hypertension; Retinopathy; Neuropathy; Nephropathy; Foot Ulcer; Skin condition; Brain disorder; Dyslipidemia; Hearing impairment; Swollen/burning feet |
| 3 | 58 (22.5) | Hypertension; Retinopathy; Neuropathy; Nephropathy; Foot Ulcer; Skin condition; Brain disorder; Dyslipidemia; Hearing impairment; Swollen/burning feet; Severe body pains |
| 4 | 29 (11.2) | Hypertension; Retinopathy; Neuropathy; Nephropathy; Foot Ulcer; Skin condition; Brain disorder; Dyslipidemia; Hearing impairment; Swollen/burning feet; Severe body pains |
| 5 | 10 (3.9) | Hypertension; Retinopathy; Neuropathy; Skin condition; Brain disorder; Dyslipidemia; Hearing impairment |
| 6 | 4 (1.6) | Hypertension; Dyslipidemia; Retinopathy; Neuropathy; Neuropathy; Skin condition; Brain disorder; Foot Ulcer |
| Average number of complications per patient= 2 | ||
Table 4. Multiple complications of type 2 diabetics.
The top ten most frequently used drugs by studied patients were Metformin, Glibenclamide, Acetylsalicylic Acid, Insulin, Cetirizine, Losartan, Nifedipine, Amlodipine, Lisinopril+Hydro and Simvastatin (Table 3). Amongst these, Metformin and Glibenclamide were the generic and commonly used drugs, and together with insulin accounted for most of the direct medical cost. Generally, about half of the patients (51.2%) were insulin dependent in the hospital. For several years now, the main diabetes management regime for type 2 diabetes patients at the study hospital include oral medication, exercise, dietary plan and insulin injection. Typically, type 2 diabetes patients unlike type- 1 patients are non-insulin dependent at initial stages of the illness. However, insulin therapy often becomes necessary when oral hypoglycemic agents are no longer effective. Reasons ascribed to the phenomenon by hospital management were: (1) it is the hospital’s standard practice to use insulin to normalize severely high glucose levels of type 2 diabetes patients; (2) patients’ resistance to medication over time (e.g. the average years patients had been diagnosed with type 2 diabetes in this study was 8years); and (3) to supplement patients medication in order to keep glucose at normal levels and prevent further complication risk.
Diabetes patients generally pay for health services both by insurance (national and private) and out-of-pocket. Medications used by patients generally were available, and majority of them (97%) were National Health Insurance Scheme (NHIS) subscribers. However, the NHIS’s reimbursement fee paid for some diabetes medications was lower than the actual cost [26]. Hence, patients were made to pay for the price difference – up to about 20% of some expensive drugs, for example insulin.
▪ Direct and indirect costs
Table 5 shows that the estimated total monthly management cost of complicated type 2 diabetes was US$9,980.62, with direct healthcare management cost constituting about 94% of this total cost. Of the direct cost, medical cost makes up about 83%. The dominance of medical cost was largely due to medicines cost. Indirect healthcare management cost was about 6%. The mean total monthly healthcare management costs were US$38.68 (95% CI: 5.53-71.84). The total productive days lost by employed type 2 diabetes patients was 304 days, with an average productive lost days of 3 days in a month. About 52% of the productivity days lost was due to seeking health care (i.e., travel, waiting and consultation time). Overall, medical cost was more than 7 times the non-medical cost and 13 times that of the indirect cost. As shown in Table 6, patients on treatment for 5 years and above incurred significantly higher direct cost compared to those below 5 years, US$40.03 ± 40.71 (p<0.05) (p<0.05). There was statistically significant difference in the indirect cost in relation to age (p<0.001) and employment status (p<0.001). Furthermore, employed patients incurred significantly higher total cost compared to those unemployed (p<0.05).
| Cost type | Cost component | Type 2 Diabetes patients | Total Cost | Cost profile (%) | |
|---|---|---|---|---|---|
| Men (n=51) |
Women (n=207) | ||||
| Direct cost | Medical cost | ||||
| Consultation | 256.41 | 1,056.41 | 1,312.82 | 13.1 | |
| Laboratory tests | 82.00 | 317.69 | 399.69 | 4.0 | |
| Medicines | 1,152.31 | 5,371.56 | 6,523.86 | 65.4 | |
| Sub-total: | 1,490.72 | 6,745.66 | 8,236.38 | 82.5 | |
| Non-medical cost | |||||
| Travel | 164.46 | 515.00 | 679.46 | 6.8 | |
| Food | 77.49 | 304.87 | 382.36 | 3.8 | |
| Miscellaneous | 20.51 | 37.56 | 58.08 | 0.6 | |
| Sub-total: | 262.46 | 857.44 | 1,119.90 | 11.2 | |
| Total direct cost | 1,753.18 | 7,603.09 | 9,356.27 | 93.7 | |
| Indirect Cost 2 | |||||
| Productivity lost in seeking health care (hours): | |||||
| Travel time | 12.52 | 33.55 | 46.07 | 0.5 | |
| Waiting & consulting time | 65.04 | 215.79 | 280.83 | 2.8 | |
| Productivity lost due to absenteeism (hours): | 106.67 | 190.77 | 297.44 | 3.0 | |
| Total indirect cost | 184.23 | 440.11 | 624.34 | 6.3 | |
| Total healthcare management cost | 1,937.41 | 8,043.20 | 9,980.62 | 100.0 | |
| 1 – US$1.00 equivalent to GHS3.90 (Bank of Ghana average monthly interbank exchange rate, June 2016) 2 - National minimum wage per day of GHS8.00 was used to value lost productivity (Ministry of Finance, June 2016) |
|||||
Table 5. Estimated healthcare management cost of complicated type 2 diabetes care (US$).
| Characteristic | Direct Cost | Indirect Cost | Total Cost | |||
|---|---|---|---|---|---|---|
| Mean ± SD (US$) |
p-value | Mean ± SD (US$) |
p-value | Mean ± SD (US$) |
p-value | |
| Sex** | ||||||
| Male | 34.38 ± 20.44 | 0.83 | 3.61 ± 5.66 | 0.07 | 37.99 ± 20.42 | 0.61 |
| Female | 36.73 ± 35.42 | 2.13 ± 4.21 | 38.86 ± 35.41 | |||
| Age*** | ||||||
| < 35 | 30.78 ± 21.99 | 0.48 | 3.88 ± 6.24 | <0.001* | 34.66 ± 22.65 | 0.84 |
| 35-44 | 28.15 ± 12.82 | 8.41 ± 11.44 | 36.56 ± 14.36 | |||
| 45-55 | 34.25 ± 17.21 | 2.86 ± 3.25 | 37.11 ± 18.17 | |||
| >55 | 38.02 ± 38.14 | 1.65 ± 3.18 | 39.67 ± 38.27 | |||
| Marital Status** | ||||||
| Married | 36.17 ± 21.25 | 0.29 | 3.05 ± 5.58 | 0.06 | 39.22 ± 21.97 | 0.17 |
| Unmarried | 36.35 ± 40.71 | 1.86 ± 3.10 | 38.22 ± 40.63 | |||
| Educational Level*** | ||||||
| No education | 33.10 ± 18.02 | 0.91 | 2.04 ± 3.02 | 0.52 | 35.32 ± 18.81 | 0.95 |
| Primary | 36.91 ± 38.78 | 2.80 ± 5.42 | 39.71 ± 38.92 | |||
| Secondary | 36.73 ± 25.30 | 1.96 ± 2.51 | 38.69 ± 25.14 | |||
| Tertiary | 37.52 ± 22.04 | 1.28 ± 1.77 | 38.80 ± 21.95 | |||
| Employment Status** | ||||||
| Employed | 36.16 ± 42.06 | 0.34 | 4.69 ± 5.44 | <0.001* | 40.85 ± 22.15 | 0.003* |
| Unemployed | 36.16 ± 21.87 | 0 | 36.16 ± 42.05 | |||
| Monthly income (USD)** | ||||||
| ≤ 150 | 34.43 ± 19.83 | 0.95 | 2.73 ± 4.32 | 0.59 | 37.16 ± 20.63 | 0.67 |
| >150 | 35.94 ± 23.58 | 3.32 ± 6.05 | 39.25 ± 23.27 | |||
| Length of treatment (Years)** | ||||||
| ≤ 5 | 32.12 ± 19.58 | 0.03* | 2.61 ± 4.80 | 0.21 | 34.73 ± 20.19 | 0.04 |
| >5 | 40.03 ± 40.71 | 2.27 ± 4.38 | 42.30 ± 40.75 | |||
| * Significant level at p<0.05 **Wilcoxon Rank Sum test used to determine significant difference in costs distribution *** Kruskal-Wallis test used to determine statistical significant difference in costs distribution |
||||||
Table 6. Relationship between mean cost and patients’ characteristics.
Sensitivity analysis conducted showed a change of +2.0%, +3.3% and +4.6% in total healthcare management cost with variation in medicine costs by 3%, 5% and 7% respectively. Changes in wage rates, also yielded percentage change of +0.2, +0.3 and +0.4 respectively in total healthcare management cost. Furthermore, concurrent variations in both medicine and wage rate by 3%, 5% and 7% resulted in +2.1%, +3.6% and +5% changes in total healthcare management cost respectively.
▪ Intangible cost
Figure 2 shows that about 59% of the patients incurred moderated intangible cost, which was slightly higher in women (59%). About 35% of the patients also reported incurring low intangible cost, which was slightly higher in men.
Figure 2. Intangible cost of diabetes by sex.
Finally, about 6% of type 2 diabetes patients with complications endured high intangible cost which was reported fairly equal in both sexes. There was no statistically significant difference in intangible burden and all the socio-demographic characteristics of studied type 2 diabetes patients suffering complications.
Discussion
This study provides an assessment of the economic burden of managing type 2 diabetes with complications in Ghana. The study result suggests that complicated diabetes were more prevalent among females and the elderly. The estimated total management cost of type 2 diabetes with complications was about US$9,981 with direct management cost representing about 94% of the total healthcare management cost. Type 2 diabetes patients suffering complications averagely spent about US$39, and most of them endure moderate intangible cost burden. Other studies have also shown that type 2 diabetes is more prevalent among the elderly in Canada and the USA respectively [29,30].
Similar to previous studies, the direct cost of type 2 diabetes patient healthcare formed a greater portion of the total cost of patient healthcare [3,31]. The main cost driver of the direct cost was medication in this study. Patients on treatment for 5 years and above incurred significantly higher direct cost burden compared to those below 5 years, US$40.03 ± 40.71 (p<0.05). Findings from other studies concluded that the direct cost of diabetes healthcare constituted a lesser proportion of the total cost [17,32]. The differences may be due to estimation prevalence approaches, geographical differences and the scope of costs considered in these two studies. Due to the chronic and complex nature of the disease, diabetes patients may either be unable to work or effectively work as they could prior to the onset of the disease [33]. Thus, diabetes management leads to a considerable increase in absenteeism. The study findings revealed that diabetes patients with complications averagely lost about 3 working days in a month due to work absenteeism. The total indirect healthcare management cost estimated was about US$624 per month, which translates into about US$7,492 annually. Valued work absenteeism alone constituted approximately 48% of the total indirect cost and 3% of total healthcare management cost. Furthermore, the difference in indirect cost in relation to age and employment status was statistically significant (p<0.001). Employed patients incurred significantly higher total cost compared to those unemployed (p<0.05), apparently because they were gainfully employed and thus lost higher valuable productive work days. Findings of this study corroborates other report which showed that valued indirect cost formed less than half of the total cost of diabetes healthcare management cost [3,31].
Those with diabetes (especially with complications) are twice more likely to suffer depression compared to those without diabetes [34]. Other studies reported that intangible burden suffered due to diabetes contributes significantly to the overall cost burden [17,34]. Majority of diabetes patients (with complications) suffer various degrees of intangible burden ranging from moderate to high in relation to physical pain, psychological pain, social relationship, functional limitation and quality of life [35,36]. Findings of this study corroborates a WHO report which observed that management of the diabetes disease especially by insulin injection may be inconvenient and psychologically stressful [33]. There was no significant relationship between intangible cost and age as well as sex (p>0.05).
This study has limitations. (1) The study focused on diabetes patients with identified complications which formed a small subset diabetes patients; (2) all costs are not accounted for such as caregivers and other non-medical costs to the families; (3) the time analysis was limited and focused on only a month of care; (4) productivity losses due to presenteeism and costs of premature mortality were not considered in the estimation of indirect cost; and (5) intangible cost were not valued in monetary terms. However, notwithstanding all these limitations, the study results can be used to inform evidence-based policy setting for NHIS tariffs on diabetes, and other pricing works in the health sector, since cost is one of the important ingredients in policy formulation.
Conclusion
Generally type 2 diabetes with complications are predominant among the elderly and their health care management poses considerable economic burden to patients. The direct healthcare management cost is often higher than the indirect cost due to medication cost. In order to reduce the economic burden to patients, it is recommended that diabetes healthcare services should be further decentralized to all lower level health facilities, and patients be encouraged to undertake regular physical activities and hobbies. Additionally, patients must be encouraged to enroll onto health insurance schemes. This would help eliminate or substantially reduce health expenditure associated with diabetes complications management. Furthermore, in order to reduce the burden of direct medical cost on patients, health insurance schemes should cover the full cost of diabetes drugs including insulin.
Acknowledgement
The authors thank the Eastern Regional Health Administration and Eastern Regional Hospital for their cordiality, support and technical assistance during the field work. We are also grateful to the patients who participated in the study. Views expressed in this study are those of the authors and in no way represent the views or stated policies of the Ghana Health Service. Finally, the authors have no conflicts of interest with respect to this study.
Samuel K. Amon is responsible for collected data, analyzed, interpreted data, drafted the manuscript and approved the final version of the manuscript. Moses K. S. Aikins is responsible for the conception and design of the study, approved the final version of the manuscript and the guarantor of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
References
- Mathers CD, Loncar D, Projections of global mortality and burden of disease from 2002 to 2030. PLoS medicine. 3(11):e442 (2006).
- http://www.contexto.org/pdfs/COMPETwef08.pdf
- Association AD, Economic costs of diabetes in the US in 2012. Diabetes care. 36(4), 1033–1046 (2013).
- Bolin K, Gip C, Mörk AC et al. Diabetes, healthcare cost and loss of productivity in Sweden 1987 and 2005—a register‐based approach. Diabetic Medicine. 26(9), 928–934 (2009).
- Association AD. Standards of medical care in diabetes—2011. Diabetes care. 34(Supplement 1), S11–S61 (2011).
- Nisar MU, Asad A, Waqas A et al. Association of Diabetic Neuropathy with Duration of Type 2 Diabetes and Glycemic Control. Cureus. 7(8), e302–e302 (2015).
- http://www.medicinenet.com/script/main/hp.asp
- Driver VR, Fabbi M, Lavery LA et al. The costs of diabetic foot: the economic case for the limb salvage team. J. Vasc. Surgery. 52(3), 17S–22S (2010).
- Abbas ZG, Archibald LK. Challenges for management of the diabetic foot in Africa: doing more with less. Int. Wound. Jour. 4(4), 305–313 (2007).
- Mbanya JC, Assah FK, Saji J et al. Obesity and type 2 diabetes in sub-sahara Africa. Current Diab. Reports. 14(7), 1–8 (2014).
- Brown JB, Ramaiya K, Besançon S et al. Use of medical services and medicines attributable to diabetes in Sub-Saharan Africa. PloS one. 9(9), e106716 (2014).
- Walker R, Whiting D, Unwin N et al. Stroke incidence in rural and urban Tanzania: a prospective, community-based study. The Lancet Neurology. 9(8), 786–792 (2010).
- http://apps.who.int/iris/bitstream/10665/204871/1/9789241565257_eng.pdf
- Ahmed S, Cannon CP, Giugliano RP et al. The independent and combined risk of diabetes and non-endstage renal impairment in non-ST-segment elevation acute coronary syndromes. Int. J. Cardiol. 131(1), 105–112 (2008).
- Dall TM, Zhang Y, Chen YJ et al. The economic burden of diabetes. Health Affairs. 29(2), 297–303 (2010).
- Kirigia JM, Sambo HB, Sambo LG et al. Economic burden of diabetes mellitus in the WHO African region. BMC. IHHR. 9(1), 6 (2009).
- Schofield D, Cunich MM, Shrestha RN et al. The economic impact of diabetes through lost labour force participation on individuals and government: evidence from a microsimulation model. BMC Pub. Health. 14(1), 220 (2014).
- Togoe H. Household burden of chronic diseases in Ghana. Ghana Med. J. 46(2), 54–58 (2012).
- Susan van D, Beulens JW, Yvonne T et al. The global burden of diabetes and its complications: an emerging pandemic. EJCPR. 17(1 suppl), s3–s8 (2010).
- http://www.who.int/management/programme/ncd/Chronic-disease-an-economic-perspective.pdf?ua=1
- Bahia LR, Araujo DV, Schaan BD et al. The costs of type 2 diabetes mellitus outpatient care in the Brazilian public health system. JISPOR. 14(5S), S137–S140 (2011).
- Malone DC, Lawson KA, Smith DH et al. A cost of illness study of allergic rhinitis in the United States. JACI. 99(1), 22–27 (1997).
- Addo R, Nonvignon J, Aikins M. Household costs of mental health care in Ghana. J. Ment. Health Policy Econ. 16(4), 151–159 (2013).
- Asare KH, Aikins M. Health facility cost of Buruli ulcer wound treatment in Ghana: a case study. VHRI. 4(1), 14–18 (2014).
- http://www.ghanahealthservice.org/ghs-category.php?cid=5
- https://pure.york.ac.uk/portal/en/publications/methods-for-the-economic-evaluation-of-health-care-programme-third-edition(e43f24cd-099a-4d56-97e6-6524afaa37d1).html
- http://ir.knust.edu.gh/bitstream/123456789/6870/1/GIFTY%20KUMI-AMPOFO.pdf
- Zhao W, Chen Y, Lin M et al. Association between diabetes and depression: Sex and age differences. Public Health. 120(8), 696–704 (2006).
- Zhuo X, Zhang P, Barker L et al. The lifetime cost of diabetes and its implications for diabetes prevention. Diabetes Care. 37(9), 2557–2564 (2014).
- Chatterjee S, Riewpaiboon A, Piyauthakit P et al. Cost of diabetes and its complications in Thailand: a complete picture of economic burden. HSCC. 19(3), 289–298 (2011).
- Barcelo A, Aedo C, Rajpathak S et al. The cost of diabetes in Latin America and the Caribbean. BWHO. 81(1), 19–27 (2003).
- http://www.who.int/mediacentre/factsheets/fs312/en/
- Anderson RJ, Freedland KE, Clouse RE et al. The prevalence of comorbid depression in adults with diabetes. Diabetes Care. 24(6), 1069–1078 (2001).
- Donald M, Dower J, Ware R et al. Living with diabetes: rationale, study design and baseline characteristics for an Australian prospective cohort study. BMC Public Health. 12(1), 8 (2012).
- Trovato GM, Catalano D, Martines GF et al. Psychological Stress Measure in Type 2 Diabetes Mellitus. ERMPSJ. 10(1), 69–74 (2006).