Review Article - Interventional Cardiology (2013) Volume 5, Issue 5
Current evidence base for chronic total occlusion revascularization
- Corresponding Author:
- Simon J Walsh
Belfast Heart Centre Royal
Victoria Hospital, Grosvenor Road,
Belfast, BT12 6BE, Northern Ireland
E-mail: simon.walsh@belfasttrust.hscni.net
Abstract
Chronic total occlusion (CTO) is defined as when atherosclerotic coronary artery disease (CAD) produces the complete or almost complete obstruction of flow in an epicardial vessel for a period of 3 months or greater. Successful revascularization of CTOs is associated with improvement in symptoms, quality of life and prognosis. The safety and success of percutaneous treatment of CTO has increased in recent years, particularly with the advent of hybrid approaches combining antegrade, retrograde and limited subintimal methods. Although no randomized controlled trial data directly comparing different treatment strategies are available, this review will summarize the available data supporting the use of CTO percutaneous coronary intervention (PCI) to improve patient outcomes.
Keywords
chronic total occlusion, indications, percutaneous revascularization, successful recanalization
Chronic total occlusion (CTO) is defined as when atherosclerotic coronary artery disease (CAD) produces the complete or almost complete obstruction of flow in an epicardial vessel for a period of 3 months or greater [1,2]. Successful revascularization of CTOs is associated with improvement in symptoms, quality of life and prognosis [3]. The safety and success of percutaneous treatment of CTO has increased in recent years, particularly with the advent of hybrid approaches combining antegrade, retrograde and limited subintimal methods [4]. Although no randomized controlled trial data directly comparing different treatment strategies are available, this review will summarize the available data supporting the use of CTO percutaneous coronary intervention (PCI) to improve patient outcomes.
Prevalence & current management
Registry data demonstrate that 15–30% of patients undergoing diagnostic coronary angiography will have at least one occluded coronary artery [5,6]. Prevalence data are more variable, mainly owing to differing definitions of what constitutes a CTO lesion and limitations of the study’s design. The Canadian CTO registry reported a prevalence of 18.4% in patients with significant CAD undergoing nonurgent coronary angiography [7], while a retrospective review of >6500 patients reported CTO lesions in up to 52% of patients [8]. However, the true prevalence is probably unknown owing to the proportion of patients who have little or no symptoms.
Patients are referred for CTO revascularization for a variety of reasons. Most commonly, typical symptoms of stable exertional angina or a positive noninvasive test prompt coronary angiography. Alternatively, a coincidental nonculprit CTO lesion is found during treatment for an acute coronary syndrome. Indeed, new presentations with acute coronary syndrome are rarely directly attributable to CTO lesions, although many patients with CTO lesions will have evidence of previous myocardial infarction (MI) [9,10].
The treatment options available to patients with documented CTOs include medical therapy alone or in combination with PCI or coronary artery bypass graft (CABG). CABG has historically been the preferred revascularization option owing to its higher immediate procedural success rate in the CTO vessel. In addition, many CTO patients have multivessel disease and will more frequently require target vessel revascularization (TVR) after PCI. The Canadian CTO registry data demonstrate that out of 1697 patients, only 10% had attempted CTO PCI. In total, 20% had PCI performed in non-CTO arteries, 44% were treated with medical therapy and 26% underwent CABG [7]. Other factors that may have contributed to the low referral rate for CTO PCI include physician skepticism over the benefits of CTO PCI and financial disincentives for the hospital. With respect to the durability of successful CTO PCI the advent of drug-eluting stents has significantly reduced the risk of restenosis and need for repeat revascularization. TVR rates for CTO PCI are now comparable to those for other ‘off-label’ drug-eluting stent procedures [11]. Although the rate of TVR following CTO PCI may reach as high as 16% [12,13], it is also important to recognize that in a randomized trial of 400 patients assessing 1‑year patency after bypass grafting of collateralized CTO vessels only 23% of non-left anterior descending artery CTO grafts remained patent. However, the surgical results of grafting left anterior descending artery CTOs were much better with 100% patency at 12 months [14].
Use of the SYNTAX score to guide CTO revascularization
There are no trials specifically comparing out-comes following CABG or PCI in CTO patients. The SYNTAX trial assessed the optimal method of revascularization for patients with multivessel CAD [15], of whom around one-quarter in each treatment arm had at least one CTO. Overall, the trial found that as the complexity and extent of coronary disease increased (as assessed by the SYNTAX score), major adverse cardiac event rates increased at 3 years in patients treated with PCI compared with CABG [16].
CTOs contribute significantly to the SYNTAX score owing to their complexity and lower success rate compared with non-CTO PCI. Hence the presence of a CTO currently represents one of the most common reasons for CABG referral [8,17,18]. However, the treatment and outcome of CTOs within the SYNTAX trial differed considerably from contemporary practice. Less than 50% of SYNTAX CTO lesions were successfully treated by PCI. In comparison, 70% of CTOs were successfully re-opened with PCI in the Canadian Multicenter registry [7], and success rates of >85% are now reported in high volume centers [19]. The poorer procedural outcomes in the SYNTAX CTO subset may reflect varying degrees of operator experience or differences in case selection and preprocedural planning. Case selection may be particularly relevant since the overall success rate of CTO bypass grafting was also only 68% on an intention-to- treat basis [20]. This highlights the situation whereby use of the SYNTAX score alone may weigh a decision towards CABG, whereas in contemporary practice using newer devices and second- or third-generation drug-eluting stents, CTO PCI could offer an acceptable alternative with respect to procedural success, outcomes and TVR. To more accurately compare revascularization options in CTO, patients will require the development of novel angiographic scoring systems to reliably predict CTO PCI success in individual cases. Such systems will additionally need to incorporate assessment of viability and ischemia in the CTO territory to determine whether revascularization of the CTO by either technique is appropriate.
Improving procedural success
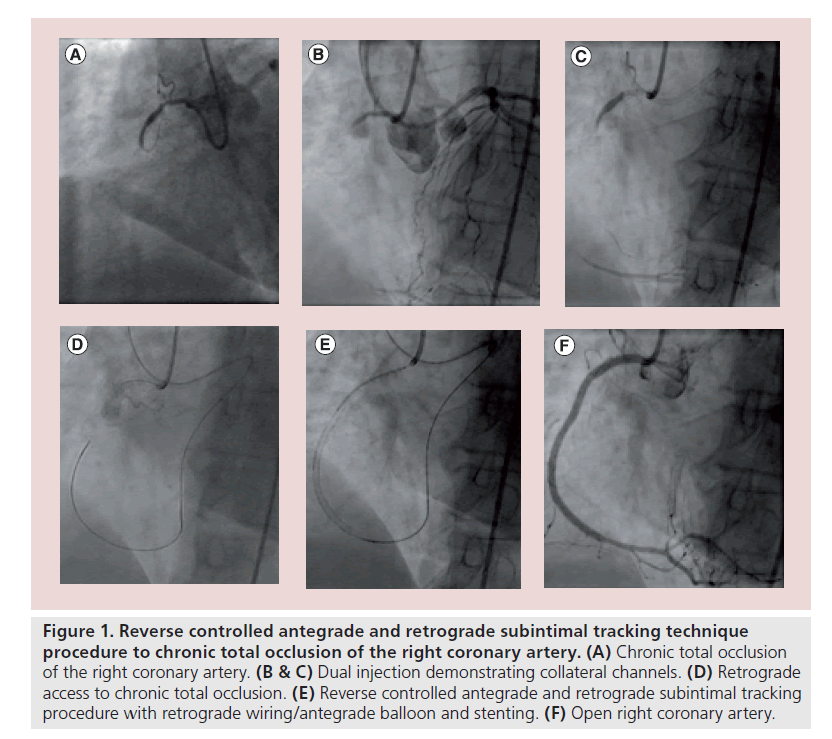
Procedural success in recanalizing CTOs depends on a number of factors. Cases are carefully selected with consideration given to the clinical context and symptom burden relating to both the culprit lesion, extent of coronary disease in other vessels, left ventricular (LV) function, presence of valvular disease and the technical likelihood of success [2]. However, as operator experience grows and development of dedicated CTO equipment continues, it is likely that an increasing proportion of CTOs can be selected for PCI. Indeed, success rates now approach 90% in the hands of experienced CTO PCI operators (Figure 1) [4,21–23]. These latest studies reflect modern practice, in high-volume CTO centers where the use of highly specialized equipment and precise preprocedural planning has become routine. It is important to appreciate that at each center, there will be a significant operator learning curve and this must be factored into revascularization decisions. For example, in the study by Whitlow et al., a procedural success rate of 67% for the first 75 cases recruited for the FAST-CTO study rose to 87% for the second 75 cases [23], and Thompson et al. reported that success rates using the retrograde approach increased from 75 to 90% during 395 cases [4].
Figure 1. Reverse controlled antegrade and retrograde subintimal tracking technique procedure to chronic total occlusion of the right coronary artery. (A) Chronic total occlusion of the right coronary artery. (B & C) Dual injection demonstrating collateral channels. (D) Retrograde access to chronic total occlusion. (E) Reverse controlled antegrade and retrograde subintimal tracking procedure with retrograde wiring/antegrade balloon and stenting. (F) Open right coronary artery.
Benefits of successful CTO revascularization
Prospective registry data have demonstrated that successful PCI of a CTO lesion is associated with better symptomatic outcome, a reduced need for CABG, a lower rate of major adverse cardiac events at 12 months and improved survival when compared with unsuccessful attempts [1,3,10,21,24,25]. Proposed contributors to improved survival include improved LV function, reduction in risk of ischemia-related malignant arrhythmias and better tolerance of contralateral coronary occlusion [3,24]. These will be reviewed below.
Improved tolerability of acute coronary syndrome events
A CTO of a nonculprit vessel is a strong predictor of cardiogenic shock [26,27] and mortality in ST-elevation MI (STEMI) [27–32].
Mortality in patients with a noninfarct related artery (IRA) CTO is increased twofold compared with STEMI patients with single-vessel disease (1‑year mortality 63 vs 31%) [30]. This so-called ‘double jeopardy’ of a non-IRA CTO and a newly occluded artery is seen in 7–13% of patients presenting with STEMI [31–33]. After primary PCI, non-IRA CTOs are associated with impaired reperfusion [34], reduced immediate LV ejection fraction and further deterioration of LV function over the following year with an associated increase in mortality [31].
The presence of CTO in a non-IRA has a comparable effect on the outcome of non- STEMI (NSTEMI) patients. A retrospective study comparing non-IRA CTO with triple-vessel disease without CTO demonstrated a 12‑month mortality of 21% in the CTO group and 12% in the non-CTO group [35].
Ischemia burden & clinical symptoms
CTO lesions can cause varying degrees of ischemic burden depending on the extent of prior infarction in the subtended myocardium and the adequacy of any collateral blood supply. The extent of ischemic burden may have significant impact on the benefits of revascularization.
When compared with optimal medical therapy (OMT) alone, it has been shown that revascularized patients with moderate-to-large amounts of inducible ischemia measured by myocardial perfusion stress imaging (defined by >12.5% of ischemic myocardium) have a survival benefit [36]. However, the COURAGE trial showed that although reduction in ischemia by PCI led to better relief from angina and reduced need for subsequent revascularization, rates of death, nonfatal MI and need for hospitalization were not lowered by the addition of PCI to OMT. The benefits of ischemia reduction were thus clear, but the optimal method by which to achieve ischemia reduction (OMT or PCI plus OMT) was less certain [37].
Ischemic burden in CTO patients has been shown to be significantly reduced by PCI [38]. Patients with baseline ischemia saw a significant reduction following PCI, with those with the severest ischemia at baseline enjoying the largest reduction at 15 months postrevascularization (-16.26% change; p ≤ 0.0001); mild baseline ischemia (-1.7% change; p = 0.008); moderate baseline ischemia (-6.32% change; p ≤ 0.0001). The COURAGE nuclear substudy reported similar findings whereby the reduction in ischemic myocardium measured by myocardial perfusion scintigraphy was greater with PCI plus OMT than with OMT alone (-2.7 vs -0.5%) and a greater proportion of patients with moderate-to- severe ischemia achieved a significant (≥5%) reduction in ischemia with PCI [39].
The ongoing ISCHEMIA trial [101], will expand the findings of the COURAGE trial by determining the optimal management strategy for patients with stable CAD and moderate-to- severe ischemia. Uniquely, patients will be randomized to OMT or OMT plus PCI before angiographic assessment. It is hoped that this strategy will eliminate selection bias against trial participation related to angiographic lesion severity (the occulostenotic reflex).
In previous trials, 85–90% of patients with CTO lesions are reported as symptomatic of ‘typical angina’ [9,10,40]. Successful CTO PCI is associated with improvement in angina status, physical abilities and overall quality of life, quantified using the Seattle Angina Questionnaire [41]. Although these results were most significant in the patient group reporting preprocedural angina, the effect was also noted in asymptomatic patients. Six out of 13 studies included in a meta-analysis comparing successful and failed CTO recanalization recorded angina status and have shown that successful recanalization was associated with a significant reduction in residual/recurrent angina. These pooled data demonstrated a 55% relative reduction in residual angina (odds ratio: 0.45; 95% CI: 0.30–0.67) [25].
Asymptomatic patients remain a controversial group. Likelihood of revascularization has been shown to consistently increase with increasing inducible ischemia to approximately 10–12.5% of myocardial ischemia, after which point the likelihood of revascularization becomes more dependent on the presence of typical anginal symptoms [36].
Arrhythmia risk
Ischemia, arrhythmia and sudden cardiac death have an important association. Indeed the extent of stress perfusion defects on single-photon emission computed tomography perfusion imaging has been used as a risk stratification tool for sudden cardiac death in CAD patients with ejection fraction >35% [42].
Patients with CTOs have a greater risk of sudden cardiac death or appropriate implantable cardioverter defibrillator therapy compared with non-CTO patients [43]. Chronic hypoperfusion of myocardium and associated electrical instability may serve to explain the link with life-threatening arrhythmias. The VACTO study analyzed implantable cardioverter defibrillator therapy in patients with CAD and found that 21% of patients with CTO had appropriate device therapy after 1-year follow-up compared with 7% in the non-CTO group. More than 30% of CTO patients had appropriate device therapy after 3-year follow-up, compared with 15% in the non-CTO group [43]. These data not only highlight the association between CTO and arrhythmia, but also identify CTO as an important independent predictor of device therapy.
LV function & myocardial viability
CTOs are associated with both impaired LV function and adverse remodeling [31]. Several small studies have assessed the effects of CTO PCI on LV function [44,45]. The largest of these studied 27 patients before, and 5 months after, successful PCI for CTO by contrast-enhanced MRI. Improvement was observed in both LV end-diastolic and end-systolic volumes but mean left ventricular ejection fraction (LVEF) did not change significantly. The presence of viability (defined by <50% transmurality of scar in a segment of LV myocardium) predicted improvement in segmental wall thickening, end-systolic volume and LVEF [45].
Other studies have shown improvement in LV function following CTO PCI, but the overall effect is small [46–49]. A study of 21 patients using cardiovascular MRI for evaluation of LV function 3 years after CTO recanalization found a nonsignificant mean improvement in ejection fraction (from 60 ± 9% to 63 ± 11%; p = 0.11) and significant decreases in mean end-systolic and -diastolic volume indicies, as above [50]. Another retrospective study demonstrated over-all improvements in LV function but differences between MI and non-MI patients in the impact of CTO recanalization [46].
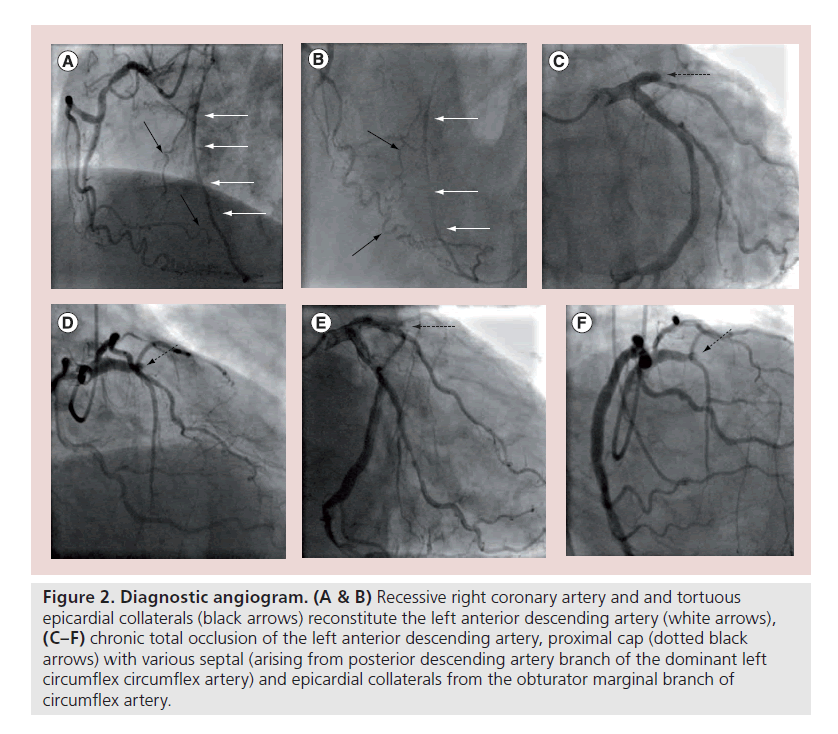
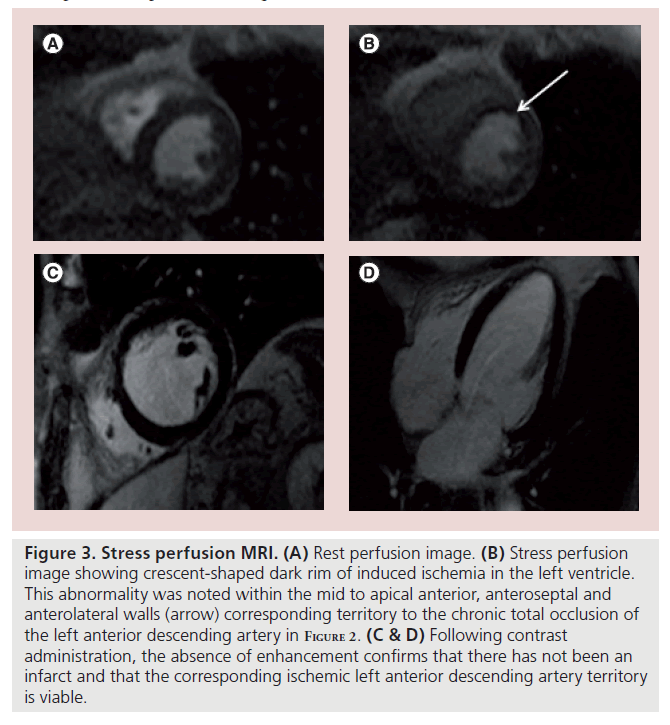
Important questions remain over the best marker for predicting functional recovery postrevascularization and whether measures such as improved segmental wall motion, reduction in LV volumes, reduction in ischemia and improvement in LVEF actually confer a prognostic benefit for the patient. Certainly when compared with the effects of other invasive heart failure treatments, such as cardiac resynchronization device therapy, where top quartile responders were shown to have mean increases of up to 14.5% [51,52], the effects of CTO PCI on LVEF are small. However, the effect on LVEF in the overall CTO population may seem less marked owing to normal function at baseline, previously shown in >50% of patients (Figures 2 & 3) [7].
Figure 2. Diagnostic angiogram. (A & B) Recessive right coronary artery and and tortuous epicardial collaterals (black arrows) reconstitute the left anterior descending artery (white arrows), (C–F) chronic total occlusion of the left anterior descending artery, proximal cap (dotted black arrows) with various septal (arising from posterior descending artery branch of the dominant left circumflex circumflex artery) and epicardial collaterals from the obturator marginal branch of circumflex artery.
Figure 3. Stress perfusion MRI. (A) Rest perfusion image. (B) Stress perfusion image showing crescent-shaped dark rim of induced ischemia in the left ventricle. This abnormality was noted within the mid to apical anterior, anteroseptal and anterolateral walls (arrow) corresponding territory to the chronic total occlusion of the left anterior descending artery in Figure 2. (C & D) Following contrast administration, the absence of enhancement confirms that there has not been an infarct and that the corresponding ischemic left anterior descending artery territory is viable.
Major adverse cardiac events & mortality
Historical data from 10 years of follow-up of successful CTO PCI cases demonstrate a survival advantage when compared with failed revascularization [21]. Hoye et al. have shown, in a retrospective registry analysis of 874 patients, that successful PCI of a CTO leads to a significantly improved survival rate (93.5% compared with 88%; p < 0.0001), but also an improvement in survival free from major adverse events (63.7 vs 41.7%; p < 0.0001) over 5 years [3]. More recent data comparing successful with unsuccessful CTO PCI continue to show a similar survival advantage [53]. All-cause mortality at 5 years was 4.5 vs 17.2%, (p = 0.0001) with a significant reduction in need for CABG measured after successful revascularization. These figures underline the importance of successful procedural outcomes.
Conclusion & future perspective
As our understanding of CTO pathology and the development of specific techniques and devices for CTO PCI improves, a wider variety of CTO lesions are amenable to safe percutaneous revascularization. With this comes a responsibility to continually reassess the data supporting CTO revascularization as a tool for improving the lives of patients. At present, although these data support a clear prognostic and symptomatic benefit of successful CTO PCI in comparison to unsuccessful revascularization, we lack randomized controlled trial data comparing CTO revascularization (whether by PCI or CABG) with OMT alone. Until this is available, it remains the role of the Heart Team to decide upon treatment options. Deficiencies of the current SYNTAX score in predicting CTO PCI success in the modern era, along with controversies surrounding ischemia burden, viability assessment and LV function recovery will continue to challenge the Heart Team to arrive at an optimal decision for each patient. While both US and European guidelines for the appropriateness of CTO PCI do exist, they now lag behind clinical practice. Indeed, with the publication of a rapidly increasing body of clinical evidence supporting CTO PCI, it is expected that current guidelines will soon be outdated. It is perhaps more necessary than ever that, when CTO cases are discussed, a high-volume CTO PCI operator versed in the latest techniques is available to advocate the case for PCI.
If the PCI option is selected, then careful strategy planning is required to minimize the risk of complications and to achieve successful revascularization. However, if the primary revascularization strategy is unsuccessful, it is important that the Heart Team is reconvened to discuss further options, since the outcome for patients with unsuccessful attempts remains poor.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Executive summary
Guiding chronic total occlusion revascularization
▪ Chronic total occlusion (CTO) lesions are reasonably common, seen in 15–30% of patients undergoing diagnostic coronary angiography.
▪ SYNTAX scoring is routinely used during decision-making regarding strategies for revascularization. The disproportionate influence of a CTO lesion on the SYNTAX score may no longer be appropriate in experienced CTO centers with the highest procedural success rates.
▪ The use of the Heart Team and individual case review has a role in the appropriate case selection to maximize successful outcomes in the CTO population.
Benefits of successful revascularization
▪ Successful revascularization is important in maximizing short- and long-term outcomes, while unsuccessful attempts increase the rate of postprocedural complications.
Future perspective
▪ Reduction in ischemia, clinical symptoms, arrhythmia, improvement in long-term left ventricle function and survival are important clinical end points for CTO studies. Randomized controlled trial evidence is required to firmly establish the role of CTO percutaneous coronary intervention in patient management.
References
Papers of special note have been highlighted as:
• of interest
- Shah PB. Management of coronary chronic total occlusion. Circulation 123(16), 1780–1784 (2011).
- Stone GW, Kandzari DE, Mehran R et al. Percutaneous recanalization of chronically occluded coronary arteries: a consensus document: part I. Circulation 112(15), 2364–2372 (2005).
- Hoye A, van Domburg RT, Sonnenschein K, Serruys PW. Percutaneous coronary intervention for chronic total occlusions: the Thoraxcenter experience 1992–2002. Eur. Heart J. 26(24), 2630–2636 (2005).
- • Demonstrates that successful revascularization by percutaneous coronary intervention leads to an increase in survival and a reduction in major adverse cardiac events at 5 years.
- Thompson CA, Jayne JE, Robb JF et al. Retrograde techniques and the impact of operator volume on percutaneous intervention for coronary chronic total occlusions an early US experience. JACC Cardiovasc. Interv. 2(9), 834–842 (2009).
- Kahn JK. Angiographic suitability for catheter revascularization of total coronary occlusions in patients from a community hospital setting. Am. Heart J. 126(3 Pt 1), 561–564 (1993).
- Cohen HA, Williams DO, Holmes DR Jr et al.; NHLBI Dynamic Registry. Impact of age on procedural and 1-year outcome in percutaneous transluminal coronary angioplasty: a report from the NHLBI Dynamic Registry. Am. Heart J. 146(3), 513–519 (2003).
- Fefer P, Knudtson ML, Cheema AM et al. Current perspectives on coronary chronic total occlusions: the Canadian Multicenter Chronic Total Occlusions Registry. J. Am. Coll. Cardiol. 59(11), 991–997 (2012).
- • Important large contemporary registry of chronic total occlusion data, highlighting the need for randomized controlled trials in this field.
- Christofferson RD, Lehmann KG, Martin GV et al. Effect of chronic total coronary occlusions on treatment strategy. Am. J. Cardiol. 95(9), 1088–1091 (2005).
- Hoher M, Wohrle J, Grebe OC et al. A randomized trial of elective stenting after balloon recanalization of chronic total occlusions. J. Am. Coll. Cardiol. 34(3), 722–729 (1999).
- Olivari Z, Rubartelli P, Piscione F et al. Immediate results and one-year clinical outcome after percutaneous coronary interventions in chronic total occlusions: data from a multicenter, prospective, observational study (TOAST-GISE). J. Am. Coll. Cardiol. 41(10), 1672–1678 (2003).
- Ko DT, Chiu M, Guo H et al. Safety and effectiveness of drug-eluting and bare-metal stents for patients with off- and on-label indications. J. Am. Coll. Cardiol. 53(19), 1773–1782 (2009).
- Saeed B, Kandzari DE, Agostoni et al. Use of drug-eluting stents for chronic total occlusions: a systematic review and meta-analysis. Cath. Cardiovasc. Interv. 77(3), 315–332 (2011).
- Colmenarez HJ, Escaned J, Fernandez C et al. Efficacy and safety of drug-eluting stents in chronic total occlusion recanalization: a systematic review and meta-analysis. J. Am. Coll. Cardiol. 55(17), 1854–1866 (2010).
- Widimsky P, Straka Z, Stros P et al. One-year coronary bypass graft patency: a randomized comparison between off-pump and on-pump surgery. Angiographic results of the PRAGUE-4 trial. Circulation 110(22), 3418–3423 (2004).
- Serruys PW, Morice MC, Kappetein AP et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N. Engl. J. Med. 360(10), 961–972 (2009).
- • SYNTAX trial comparing percutaneous coronary intervention and coronary artery bypass graft in patients with untreated threevessel and/or left-main coronary artery disease.
- Head SJ, Holmes DR, Mack MJ et al. Risk profile and 3‑year outcomes from the SYNTAX percutaneous coronary intervention and coronary artery bypass grafting nested registries. JACC Cardiovasc. Interv. 5(6), 618–625 (2012).
- King SB III, Lembo NJ, Weintraub WS et al. A randomized trial comparing coronary angioplasty with coronary bypass surgery. N. Engl. J. Med. 331(16), 1044–1050 (1994).
- Bourassa MG, Roubin GS, Detre KM et al. Bypass angioplasty revascularization investigation: patient screening, selection and recruitment. Am. J. Cardiol. 75(9), 3C–8C (1995).
- Rathore S, Matsuo H, Terashima M et al. Procedural and in-hospital outcomes after percutaneous coronary intervention for chronic total occlusions of coronary arteries 2002 to 2008: impact of novel guidewire techniques. JACC Cardiovasc. Interv. 2(6), 489–497 (2009).
- Farooq V, Serruys PW, Gardcia-Garcia HM et al. The negative impact of incomplete angiographic revascularization on clinical outcomes and its association with total occlusions: the SYNTAX trial. J. Am. Coll. Cardiol. 61(3), 282–294 (2013).
- Suero JA, Marso SP, Jones PG et al. Procedural outcomes and long-term survival among patients undergoing percutaneous coronary intervention of a chronic total occlusion in native coronary arteries: a 20‑year experience. J. Am. Coll. Cardiol. 38(2), 409–414 (2001).
- Tsuchikane E, Yamane M, Mutoh M et al.; Retrograde Summit Investigators. Japanese multicenter registry evaluating the retrograde approach for chronic coronary total occlusion. Cath. Cardiovasc. Interv. doi:10.1002/ ccd.24823 (2013) (Epub ahead of print).
- Whitlow PL, Burke MN, Lombardi WL et al. Use of a novel crossing and re-entry system in coronary chronic total occlusions that have failed standard crossing techniques: results of the FAST-CTOs (Facilitated Antegrade Steering Technique in Chronic Total Occlusions) trial. JACC Cardiovasc. Interv. 5(4), 393–401 (2012).
- Stone GW, Reifart NJ, Moussa I et al. Percutaneous recanalization of chronically occluded coronary arteries: a consensus document: part II. Circulation 112(16), 2530–2537 (2005).
- Joyal D, Afilalo J, Rinfret S. Effectiveness of recanalization of chronic total occlusions: a systematic review and meta-analysis. Am. Heart J. 160(1), 179–187 (2010).
- Bataille Y, Dery JP, Larose E et al. Deadly association of cardiogenic shock and chronic total occlusion in acute ST-elevation myocardial infarction. Am. Heart J. 164(4), 509–515 (2012).
- van der Schaaf RJ, Timmer JR, Ottervanger JP et al. Long-term impact of multivessel disease on cause-specific mortality after ST elevation myocardial infarction treated with reperfusion therapy. Heart 92(12), 1760–1763 (2006).
- Moreno R, Conde C, Perez-Vizcayno MJ et al. Prognostic impact of a chronic occlusion in a noninfarct vessel in patients with acute myocardial infarction and multivessel disease undergoing primary percutaneous coronary intervention. J. Invasive Cardiol. 18(1), 16–19 (2006).
- Sanz G, Castaner A, Betriu A et al. Determinants of prognosis in survivors of myocardial infarction: a prospective clinical angiographic study. N. Engl. J. Med. 306(18), 1065–1070 (1982).
- van der Schaaf RJ, Vis MM, Sjauw KD et al. Impact of multivessel coronary disease on long-term mortality in patients with ST-elevation myocardial infarction is due to the presence of a chronic total occlusion. Am. J. Cardiol. 98(9), 1165–1169 (2006).
- Claessen BE, van der Schaaf RJ, Verouden NJ et al. Evaluation of the effect of a concurrent chronic total occlusion on long-term mortality and left ventricular function in patients after primary percutaneous coronary intervention. JACC Cardiovasc. Interv. 2(11), 1128–1134 (2009).
- Bataille Y, Dery JP, Larose E et al. Incidence and clinical impact of concurrent chronic total occlusion according to gender in ST-elevation myocardial infarction. Catheter. Cardiovasc. Interv. 82(1), 19–26 (2013).
- Lexis CP, van der Horst IC, Rahel BM et al. Impact of chronic total occlusions on markers of reperfusion, infarct size, and long-term mortality: a substudy from the TAPAS-trial. Catheter. Cardiovasc. Interv. 77(4), 484–491 (2011).
- Claessen BE, Dangas GD, Weisz G et al. Prognostic impact of a chronic total occlusion in a non-infarct-related artery in patients with ST-segment elevation myocardial infarction: 3‑year results from the HORIZONS-AMI trial. Eur. Heart J. 33(6), 768–775 (2012).
- Gierlotka M, Tajstra M, Gasior M et al. Impact of chronic total occlusion on 12‑month mortality in patients with non-ST segment elevation myocardial infarction treated by percutaneous intervention (from the PL-ACS Registry). Int. J. Cardiol. doi:10.1016/j. ijcard.2012.09.086 (2012) (Epub ahead of print).
- Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 107(23), 2900–2906 (2003).
- • Demonstrates the survival benefit of percutaneous coronary intervention over medical therapy alone in patients with inducible ischemia by stress myocardial perfusion imaging.
- Boden WE, O’Rourke RA, Teo KK et al. Optimal medical therapy with or without PCI for stable coronary disease. N. Engl. J. Med. 356(15), 1503–1516 (2007).
- Safley DM, Koshy S, Grantham JA et al. Changes in myocardial ischemic burden following percutaneous coronary intervention of chronic total occlusions. Catheter. Cardiovasc. Interv. 78, 337–343 (2011).
- Shaw LJ, Berman DS, Maron DJ et al. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation 117(10), 1283–1291 (2008).
- Rubartelli P, Niccoli L, Verna E et al. Stent implantation versus balloon angioplasty in chronic coronary occlusions: results from the GISSOC trial. JACC Interv. Cardiol. 32(1), 90–96 (1998).
- Grantham JA, Jones PG, Cannon JL, Spertus JA. Quantifying the early health status benefits of successful chronic total occlusion recanalization: results from the FlowCardia’s Approach To Chronic Total Occlusion Recanalization (FACTOR) Trial. Circ. Cardiovasc. Qual. Outcomes 3(3), 284–290 (2010).
- Piccini JP, Starr AZ, Horton JR et al. Single-photon emission computed tomography myocardial perfusion imaging and the risk of sudden cardiac death in patients with coronary disease and left ventricular ejection fraction >35%. JACC Imaging 56(3), 206–214 (2010).
- Nombela-Franco L, Mitroi CD, Fernandez- Lozano I et al. Ventricular arrhythmias among implantable cardioverter-defibrillator recipients for primary prevention: impact of chronic total coronary occlusion (VACTO primary study). Circ. Arrhythm. Electrophysiol. 5(1), 147–154 (2012).
- Kirschbaum SW, Rossi A, Boersma E et al. Combining magnetic resonance viability variables better predicts improvement of myocardial function prior to percutaneous coronary intervention. Int. J. Cardiol. 159(3), 192–197 (2012).
- Baks T, van Geuns RJ, Duncker DJ et al. Prediction of left ventricular function after drug-eluting stent implantation for chronic total coronary occlusions. J. Am. Coll. Cardiol. 47(4), 721–725 (2006).
- Chung C-M, Nakamura S, Tanaka K et al. Effect of recanalization of chronic total occlusions on global and regional left ventricular function in patients with or without previous myocardial infarction. Catheter. Cardiovasc. Interv. 60(3), 368–374 (2003).
- Melchior JP, Doriot PA, Chatelain et al. Improvement of left ventricular contraction and relaxation synchronism after recanalization of chronic total coronary occlusion by angioplasty. J. Am. Coll. Cardiol. 4, 763–768 (1987).
- Sirnes PA, Myreng Y, Molstad P et al. Improvement in left ventricular ejection fraction and wall motion after successful recanalization of chronic total occlusion. Eur. Heart J. 19, 273–281 (1998).
- Danchin N, Angioi M, Cador R et al. Effect of late percutaneous angioplastic recanalization of total coronary artery occlusion on left ventricular remodelling, ejection fraction, and regional wall motion. Am. J. Cardiol. 78, 729–735 (1996).
- Kirschbaum SW, Baks T, van den Ent M et al. Evaluation of left ventricular function three years after percutaneous recanalization of chronic total coronary occlusions. Am. J. Cardiol. 101(2), 179–185 (2008).
- Hsu JC, Solomon SD, Bourgoun M et al. Predictors of super-response to cardiac resynchronization therapy and associated improvement in clinical outcome: the MADIT-CRT (multicentre automatic defibrillator implantation trial with cardiac resynchronization therapy) study. J. Am. Coll. Cardiol. 59(25), 2366–2373 (2012).
- Linde C, Abraham WT, Gold MR, Daubert C; REVERSE Study Group. Cardiac resynchronization therapy in asymptomatic or mildly symptomatic heart failure patients in relation to etiology. Results from the REVERSE (the REsynchronization reVErses Remodelling in Systolic Left vEntricular Dysfunction) study. J. Am. Coll. Cardiol. 56(22), 1826–1831 (2010).
- Jones DA, Weerackody R, Rathod K et al. Successful recanalization of chronic total occlusions is associated with improved long-term survival. JACC Cardiovasc. Interv. 5(4), 380–388 (2012).
- ISCHEMIA Study. For physicians (2013). www.ischemiatrial.org/for-physicians (Accessed 19 April 2013)
▪ Website
• ISCHEMIA is a multicenter randomized controlled trial enrolling patients who have demonstrated ischemia on stress imaging. Recruits are randomized to either conservative or invasive management prior to coronary angiography.