Review Article - Interventional Cardiology (2014) Volume 6, Issue 3
Coronary artery stenting in elderly patients: where are we now
- Corresponding Author:
- Carlo
Briguori
Laboratory of Interventional Cardiology, Clinica Mediterranea, Via Orazio, 2, I-80121, Naples, Italy
Tel: +39 081 7259 764
Fax: +39 081 7259 777
E-mail: carlobriguori@clinicamediterranea.it
With the increase of the elderly population, the number of these patients undergoing percutaneous coronary intervention (PCI) has increased considerably. The elderly are, given the presence of comorbidities and frailty, at higher risk of mortality and morbidity following PCI. However, the elderly appear to derive significant benefits in terms of quality of life and might derive greater benefits from revascularization compared with younger patients. PCI is clearly effective in old age, but a careful approach to patient selection is essential to obtain better outcomes. In this qualitative review, we sought to examine the role and the risks of PCI in the older patients and the strategies to lower the adverse events in this particular set of patients.
Abstract
With the increase of the elderly population, the number of these patients undergoing percutaneous coronary intervention (PCI) has increased considerably. The elderly are, given the presence of comorbidities and frailty, at higher risk of mortality and morbidity following PCI. However, the elderly appear to derive significant benefits in terms of quality of life and might derive greater benefits from revascularization compared with younger patients. PCI is clearly effective in old age, but a careful approach to patient selection is essential to obtain better outcomes. In this qualitative review, we sought to examine the role and the risks of PCI in the older patients and the strategies to lower the adverse events in this particular set of patients.Keywords
acute coronary syndrome, elderly, percutaneous coronary intervention
The world has never seen an aged population as currently exists globally. The increase in life expectancy has raised the average age of the population by increasing the number of surviving older people. Currently, 21% of the population in the more developed regions is aged 60 years or over, and by 2050 almost 33% of the population is projected to be 60 years or over [1].
The increasing age also places the population at risk of cardiovascular disease and is a powerful predictor of death and other major adverse cardiovascular events (MACE) in patients with coronary artery disease (CAD) [2–5]. Despite the improvement in percutaneous interventions and medical therapy, CAD remains the leading cause of morbidity and mortality among the elderly and its prevalence and severity increases with advancing age [6].
Evidence from trials of coronary revascularization has shown that patients at high risk derive greater benefit from revascularization than patients at low risk [7–9]. Thus, older patients, presenting more cardiovascular risk factors and higher risk of subsequent cardiovascular events, might derive greater benefit from revascularization [9,10]. However, community studies have shown that elderly patients are less likely to undergo percutaneous coronary intervention (PCI) and those that undergo coronary revascularization are typically treated less aggressively.
Despite the efforts made in the last updates, the current guidelines still do not take fully into account the complexity in the management and treatment of older patients, based on observational studies, post hoc analysis or randomized clinical trials in which they are frequently excluded for the presence of comorbidities requiring multiple medications or because of functional or cognitive limitations [11,12]. In recent years, the growing statistical importance of the older patients with CAD in the whole population and the development of new technologies and evidence based periprocedural medications made the PCI in this set of patients more feasible, increasing the amount of published data regarding this challenging field in interventional cardiology. In a cohort study conducted in Denmark, 3792 elderly patients (>80 years old) were treated with PCI and the annual proportion increased from 224 (5.4%) in 2002 to 588 (10.2%) in 2009 [13]. In the SCAAR trial, a total of 144,039 patients undergoing a PCI for the first time between January 1990 and December 2010 were analyzed; patients aged >75 years in 1990 were 5.8%, in 2000 were 15.9% and currently represent 28% of the whole PCI population [14]. The 2011 guidelines for PCI acknowledge that older adults constitute a growing proportion of patients considered for PCI. In one series examining trends over 25 years, the proportion of patients undergoing PCI who were 75–84 years of age doubled and those older than age 85 years increased fivefold [11].
Despite that these data support a more aggressive attitude, the limit between benefit and harm is often vague. The management and the adoption of the most beneficial therapeutic strategy in the elderly with CAD represents one of the current challenges for interventional cardiologists.
In this qualitative review, we sought to examine the role of PCI in elderly patients with stable coronary disease and acute coronary syndromes (ACS) and the strategies to lower adverse events in this particular set of patients. Where not differently specified, elderly patients has been defined as patients aged over 75 years.
Frailty & increased PCI-related risk in the elderly
Predicting risk in the elderly may be problematic given their highly variable health, social and cognitive status. Age is an independent risk factor for adverse outcomes in many conditions and is usually included in risk scores. However, the assessment of frailty represents comprehensively the vulnerability typical of the elderly and is emerging as a superior predictor when compared with chronological age. Frailty, denoting a multidimensional syndrome characterized by increased vulnerability and decreased physiologic reserves, is also known to be associated with an increase in long-term mortality in patients with cardiovascular disease [15,16]. Singh et al. found that 66% of patients >65 years of age undergoing PCI are either frail or have intermediate frailty and that the inclusion of measures of frailty, comorbidity and quality-of-life (QOL) status improves risk statification and predicts adverse outcomes and mortality better than the traditional cardiovascular risk scores, based on traditionally assessed cardiovascular risk factors [16].
Frailty in this setting increases the potential for complications and may limit the scope for symptomatic improvement. CAD in elderly patients is more extensive than in younger patients with a higher prevalence of three-vessel and left main CAD; nevertheless, two reasons make these patients less likely to undergo PCI: lower procedure success rates; and worse short-term prognosis [17,18]. Often the feasibility of performing PCI in elderly patients causes concern; operators must take into account a more extensive and diffuse patterns of atherosclerosis in the arterial beds, increased vascular stiffness and endothelial dysfunction [19]. Severe coronary calcification, which may lead to coronary dissections, stent underexpansion or the need for more invasive procedures such as rotational atherectomy, while peripheral vascular disease with a tortuous aorto–iliac system and often subclavian vessels, make coronary approaches difficult and may significantly affect access for interventional procedures.
Moreover, because of their frailty and comorbidities, elderly patients undergoing a percutaneous intervention run an increased risk of procedure-related complications, which are associated with higher mortality rates. In three large registries, the authors observed that in-hospital mortality was up to five-times higher in the most elderly group compared with those aged <80 years [20–22].
Despite these considerations, in current practice, up to 25% of all PCI are performed in patients over the age of 75 years and 12% are performed in those aged over 80 years, and this number has increased sharply over the past decade [20,21].
Stable angina
The prevalence of angina in population-based studies increases with age in both sexes, from 5 to 7% in women aged 45–64 years to 10 to 12% in women aged 65–84 years, and from 4 to 7% in men aged 45–64 years to 12 to 14% in men aged 65–84 years [23]. However, diagnosis of CAD is often difficult in the elderly because of the presence of atypical symptoms and common coexisting conditions, including the limited capacity to exercise and their high prevalence of baseline ECG changes that render exercise test data less reliable.
For choosing the optimal treatment strategy in the individual patient, both the complexity of CAD and concomitant comorbidities have to be taken into account. Therefore, cautious risk stratification is an essential aspect of this clinical decision-making process. A variety of risk scores has been developed to further stratify CAD patients, and to give additional information whether a patient should undergo PCI, coronary artery bypass graft (CABG) or optimal medical therapy (OMT) alone. Sinning et al. demonstrated that the combination of the SYNTAX score and the EuroSCORE as a combination of angiographical and clinical risk factors is beneficial in selecting the appropriate revascularization strategy for the individual patient and to further improve outcomes, especially in high-risk patients such as elderly patients [24]. Older patients with multivessel disease are more often referred to PCI than CABG, but age should not be the sole criterion for the choice of type of revascularization. Although a slight advantage of surgical over percutaneous revascularization might exist for elderly patients with multivessel coronary disease, especially if diabetic [25–27]; surgical revascularization should remain an option only for a selected population of highly functioning elderly patients with few comorbidities.
In the prespecified analysis of clinical outcomes by age from the COURAGE trial [28], given the known limitations of the study, OMT was as effective in stable CAD patients aged <65 years as in patients aged >65 years, and PCI, when added to OMT, did not prevent ‘hard’ clinical outcomes such as death or myocardial infarction (MI) during long-term follow-up. In addition, older patients were angina-free at 60 months of follow-up with similar rates for those treated with PCI (80%) and OMT (73%).
In the randomized TIME trial, the authors compared an invasive strategy versus OMT in 303 patients aged 75 years and older with stable angina [29] and found a reduction in the risk of MACE in the invasive arm, which was largely driven by the reduction in rate of rehospitalization. Patients managed medically had a twofold increased risk of an adverse cardiovascular outcome compared with those undergoing myocardial revascularization. At a 4-year follow-up, an invasive strategy resulted in decreased MACE and improved QOL compared with a conservative strategy of OMT. However, the invasive strategy was associated with a trend toward increased mortality [30].
The Alberta Provincial Project for Outcome Assessment and Coronary Heart Disease Study [31] strengthened the evidence that elderly patients experience the largest absolute risk reductions associated with CABG or PCI compared with younger patients. Among the 6181 patients aged 70 years or older, the improvements in health status observed with coronary revascularization were similar or greater than those seen in patients aged <70 years.
These findings illustrating the benefits of an aggressive revascularization strategy in elderly patients are confirmed by the analysis of the German ALKK registry based on the data of 35,534 consecutive patients (7645 [21.5%] were aged between 75 and 84 years, and 744 [2.1%] patients were older than 85 years) undergoing elective PCI in which the authors found no differences in intraprocedural complications during elective PCI between younger and elderly patients. Although in-hospital major adverse cardiac and cerebrovascular events were somewhat higher in the elderly, the overall event rate was low [32].
Notwithstanding the positive results emerging from nonrandomized studies, the higher in-hospital mortality rates associated with revascularization, particularly in patients older than 75–80 years, raises some concerns and the indication for PCI in very elderly patients still remains questionable. Since PCI is mainly performed for pain relief and not for a higher life expectancy, this should be recommended only after careful consideration of patient preferences and desired outcomes, functional capacity and QOL, as well as therapeutic alternatives.
The importance of improvements in health status and QOL in influencing decision-making in this patient group tends to grow compared with the importance of survival end points. Especially as patients get older, it is reasonable that their objective may be to live better rather than longer.
Acute coronary syndrome
Age is one of the most important predictors of risk in ACS. The prevalence of ACS-related complications such as heart failure, bleeding, stroke, renal failure and infections increases markedly with age and patients aged >75 years have at least double the mortality rate of those <75 years [33]. The elderly are at particular risk of bleeding; it is therefore essential to dose the antithrombotic therapies, particularly in relation with renal function.
In the setting of ACS, the American College of Cardiology/ American Heart Association guidelines recommend that the elderly patient’s candidacy for intervention is evaluated with similar standards to those used for younger patients in deference to the wishes of the patient and his family [34]. Although it has been widely demonstrated that routine early invasive management yields superior outcomes in patients >65 years of age with ACS [35–37], in current clinical practice these patients are less likely to undergo invasive procedures than younger patients [38–42].
Elderly patients have been historically excluded from ACS randomized trials because of their comorbidities and potentially high mortality rates. Therefore, evidence has been extrapolated from studies of younger patients, which precludes extending the study findings to the population that experiences the most morbidity and death from ACS.
In the treatment of older patients, one should prioritize relief of symptoms treating the culprit lesion and avoidance of bleeding complications. Moreover, a complete revascularization in patients with multivessel CAD, neither significantly influences the rate of repeat revascularizations, nor acute and 12 months total adverse events [43–45].
Non-ST-elevation MI
Non-ST-segment elevation ACS (NSTE-ACS) is the most common presentation of acute ischemic heart disease in elderly patients; in European registries of NSTE-ACS, 27–34% of patients are aged >75 years [46]. There has been considerable debate about the optimal therapy for elderly patients in this set of patients. Landmark randomized trials and registries demonstrated that compared with younger patients, elderly patients with unstable angina or non-ST-elevation MI had a markedly increased rate of adverse ischemic outcomes and that an early coronary angiography and revascularization (<48 h after hospital admission) leads to better in-hospital and long-term outcomes [47–50]. This strategy had a greater absolute benefit for the reduction of death or nonfatal MI in older patients than in younger patients, and both the absolute and relative benefits increased with increasing age. Of note, the early invasive strategy may increase major bleeding among patients older than 75 years of age [49].
Damman et al. analyzed the impact of the initial management strategy on the 5-year risk of cardiovascular death or MI, according to the patients’ age categories in the FRISC II, ICTUS and RITA 3 trials and found that, in patients with NSTE-ACS, the long-term benefit of the routine invasive strategy over the selective invasive strategy was evident for patients aged 65–74 years (hazard ratio [HR]: 0.72; 95% CI: 0.58–0.90) and those aged ≥75 years (HR: 0.71; 95% CI: 0.55–0.91), but not in those aged <65 years (HR: 1.11; 95% CI: 0.90–1.38) [51].
In the Elderly ACS trial, 313 patients ≥75 years of age with NSTE-ACS were randomly allocated to an early aggressive strategy or an initially conservative strategy [52]. Patients with an initially conservative treatment experienced significantly more ischemic events during index admission and within 1 year, a 20% difference in the rates of major adverse cardiac and cerebrovascular events between the early aggressive and the initially conservative cohorts was observed. Moreover, patients with elevated troponin levels on admission randomized to an early aggressive approach had a significant 57% reduction of the primary end point rate.
PCI in very old patients (>85 years) appeared to be safe in the study conducted by Rana et al. [53]. In this registry, the authors showed that, in 294 patients over the age of 85 years undergoing PCI for ACS, 1-year mortality rates were 17.7%. In elderly patients who underwent revascularization during the index admission, there was a larger absolute reduction in mortality at 6 months compared with patients <70 years of age (7 vs 1.8%, respectively).
ST-elevation MI
Management of MI in the elderly presents special challenges compared with younger patients. Delays in the emergency activation are common among older adults, often due to atypical symptoms and/or lack of symptom recognition [54]. Treatment may also include delay or lack of reperfusion, increased risk of antithrombotic therapy and presence of comorbidity and renal impairment, which require dosing adjustment.
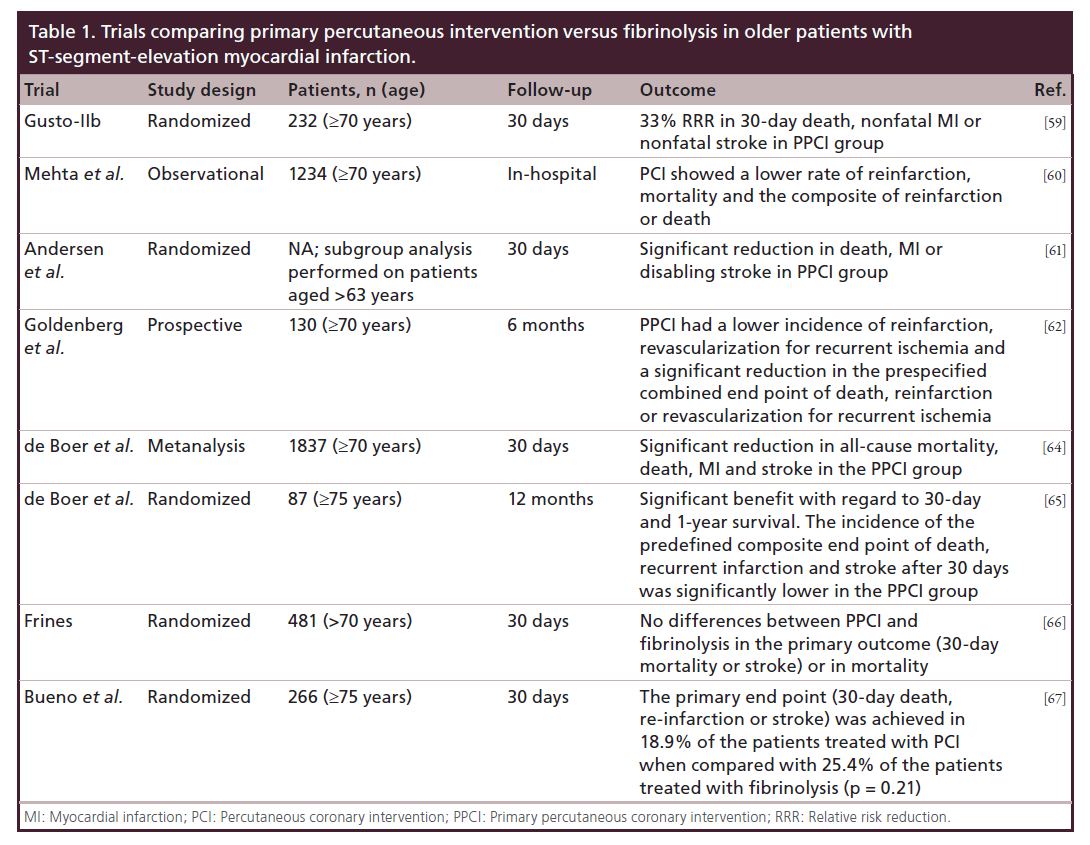
The decision of reperfusion strategies to be made must depend on the availability of resources for reperfusion in each practice. Overall, thrombolysis is not commonly utilized in the elderly age group in contemporary practice [55,56]. The leading reasons center on concerns regarding increased bleeding, intracranial hemorrhage and higher in-hospital mortality. Primary PCI (PPCI) is particularly attractive in the elderly, since it offers the advantage of high successful reperfusion rates in this very high-risk population, avoiding the risks of bleeding associated with fibrinolytic therapy. Considerable evidence from registries and subanalysis of randomized trials conducted in the last two decades indicates that PPCI is superior to fibrinolytic therapy in the elderly, reducing recurrent ischemia, reinfarction, stroke and death [57–62] and shows up to five-times higher mortality when compared with younger patients [63].
In a meta-analysis of 22 randomized trials comparing PPCI with fibrinolysis, de Boer et al. showed a mortality reduction favoring primary PCI in all age strata, as well as reductions in the risk of repeat MI and stroke [64].
So far, three randomized trials have assessed the efficacy of primary PCI versus fibrinolysis in the elderly. A small study evaluating 87 patients aged ≥75 years showed that PPCI was superior to thrombolysis with streptokinase revealing a decrease of the composite end point of death, re-infarction or stroke at 1 year (13 vs 44%; p = 0.001) [65]. In the Senior PAMI trial [66], which randomized 481 patients >70 years old, although PPCI did not reduce the primary end point of 30-day death or disabling stroke, it was superior among patients 70–80 years old to thrombolytic therapy at reducing the combined end point of death, disabling stroke or re-infarction, a secondary end point (7.7 vs 17.0%; p < 0.01). Moreover, a nonsignificant trend towards a higher mortality rate in patients >80 years old was allocated to PPCI (19 vs 16%). The TRIANA study, including 266 patients aged >75 years, reported a trend toward reduction in the 30-day composite end point of death, re-infarction or disabling stroke with PPCI (18.9 vs 25.4%; p = 0.21). Recurrent ischemia was encountered less commonly in primary PCI-treated patients (0.8 vs 9.7%; p = 0.001) [67]. Of note, both the Senior PAMI and TRIANA trials were terminated before completion because of slow recruitment. The results of the main trials comparing primary percutaneous intervention versus fibrinolysis are summarized in Table 1.
Lowering risk & improving outcomes of PCI in the elderly
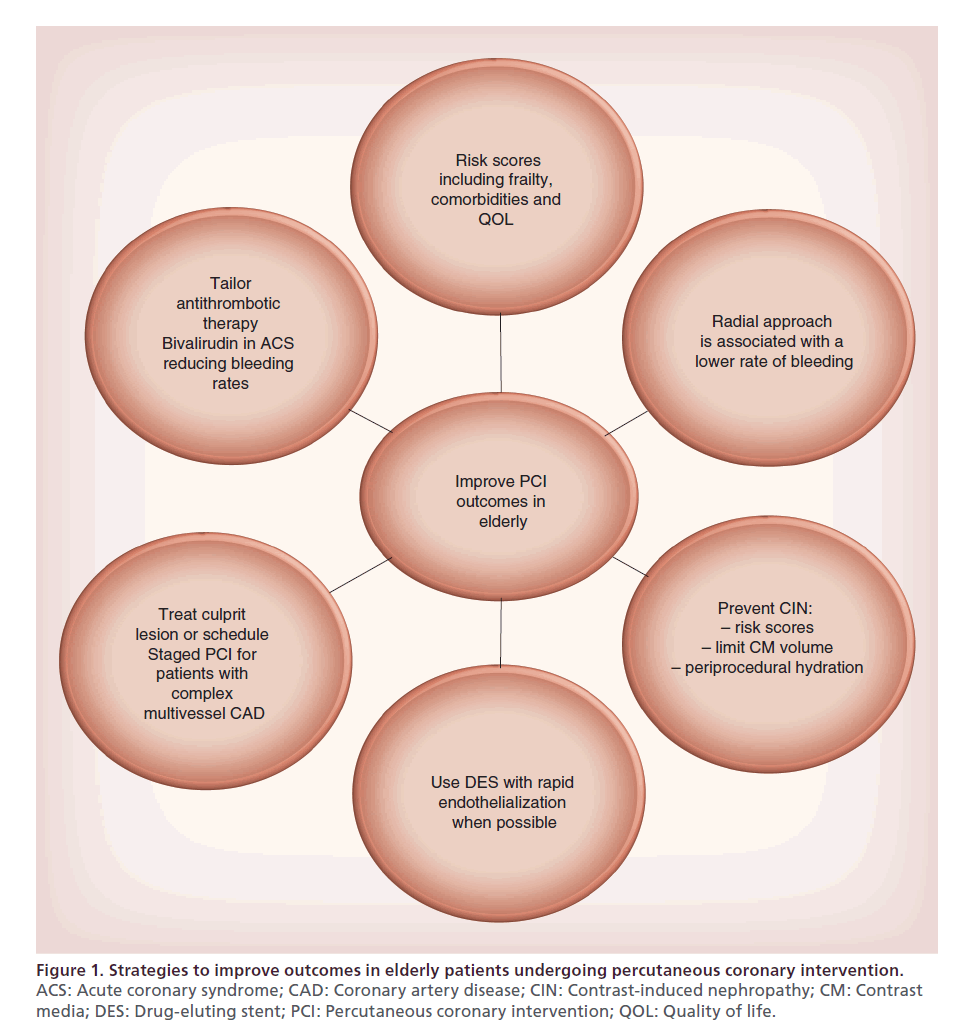
Frailty and the presence of significant comorbidities such as renal insufficiency, multiorgan dysfunction and extensive vascular disease may explain the increased mortality rates in elderly patients undergoing PCI. Over the last 10 years, new therapeutic tools, including devices and medications, have been developed to reduce periprocedural complications. General recommendations to improve outcomes in elderly patients undergoing PCI are depicted in Figure 1.
Figure 1. Strategies to improve outcomes in elderly patients undergoing percutaneous coronary intervention.
ACS: Acute coronary syndrome; CAD: Coronary artery disease; CIN: Contrast-induced nephropathy; CM: Contrast
media; DES: Drug-eluting stent; PCI: Percutaneous coronary intervention; QOL: Quality of life.
Risk stratification
To achieve better outcomes in patients undergoing PCI, it is essential for interventionists to perform a careful case selection and the decision on how to manage the single older patient should include the patient’s preillness mental status, physical condition, patient wishes and QOL and be based on the estimated ischemic and bleeding risk, estimated life expectancy, and risks and benefits of revascularization [16]. Frailty stratification predicts a patient’s risk of death and need for institutional care and, as aforementioned, should be included in the risk models for the elderly. In their study, Graham et al. expanded the use of a simple frailty assessment tool such as the Edmonton Frail Scale to a group of elderly patients with ACS. Higher Edmonton Frail Scale scores were associated with increased comorbidity, longer lengths of stay, decreased procedure use and, after adjusting for baseline risk factor differences using a burden of illness variable, with increased mortality [68].
Bleeding
Periprocedural bleeding and vascular complications are associated with worst clinical outcome, prolonged hospital stay and increased short- and long-term mortality, especially in elderly patients with ACS [69–72] who are at highest risk for bleeding after PCI. The reduced glomerular filtration rate (GFR) with the consequent reduction in renal drug elimination and the altered hemostatic state with a tendency towards increased bleeding in response to antithrombotic agents in the elderly, makes the choice of the antithrombotic therapy paramount in avoiding this complication. The selection of vascular access in the elderly represents equally a crucial point in prevention of bleeding and worse outcomes.
Antiplatelet therapy
Aspirin should be prescribed well before revascularization and thereafter lifelong, at low (≤100 mg/day) doses. Clopidogrel, given its ease of use, friendly therapeutic window and low cost, should be considered as the receptor P2Y12 blocker of choice. Prasugrel is a thirdgeneration oral thienopyridine with more potent platelet P2Y12 inhibitory effects than clopidogrel. Post hoc analyses from the TRITON-TIMI 38 trial clarified that, in patients older than 75 years, prasugrel has no net clinical advantage over clopidogrel as the ischemic benefit is offset by the risk of bleeding [73]. Although the use of prasugrel in patients ≥75 years of age is generally not recommended, according to the EMA, a reduced 5-mg prasugrel maintenance dose may be considered in the elderly. The safety and efficacy of a 5-mg dose of prasugrel in elderly patients with NSTE-ACS medically treated has been evaluated in the TRILOGYACS trial [74]. The authors did not observe any differences in ischemic and bleeding outcomes between reduced-dose prasugrel and clopidogrel 75 mg/day in the elderly cohort.
Ticagrelor is the first member of a new class of potent reversible P2Y12 receptor antagonists that do not require metabolism and have direct action on the P2Y12 receptor. In a substudy of the PLATO trial, the clinical benefit of ticagrelor over clopidogrel in patients with ACS with respect to the composite of cardiovascular death, MI and stroke; MI; cardiovascular death; stent thrombosis or all-cause mortality, was not significantly different between patients aged ≥75 years and those aged <75 years. No increased risk of major bleeding complications with ticagrelor versus clopidogrel was observed in patients aged ≥75 years or patients aged <75 years [75].
Notwithstanding the trend towards a clinical benefit, treatment with glycoprotein IIb/IIIa inhibitor (GPI) in elderly patients with ACS who undergo PCI is still controversial. Although guidelines do not suggest dose modifications based on age, careful patient selection is mandatory and dosing adjustment based on GFR is necessary for small-molecule GPIs (tirofiban and eptifibatide), which are cleared renally. An increase in minor bleeding should be expected when using GPIs in patients 75 years of age and older, but the potential treatment benefit may surpass the slightly increased risk for minor access site bleeding complications. Broadened use of vascular closure devices in this specific patient population may lower the rate of such complications.
Anticoagulation during PCI
It is essential to tailor antithrombotic therapy before, during and after PCI in the elderly. Bivalirudin is a direct thrombin inhibitor that has some peculiar advantages over heparins, such as lack of dependence on plasma protein. This property results in a more predictable response. A subanalysis of the ACUITY trial demonstrated that despite no significant differences in efficacy, rates of non-CABG major and minor bleeding in elderly patients with NSTE-ACS undergoing PCI were reduced in every age group (6.1 vs 12.3% in patients older than 75 years) with bivalirudin alone versus heparin plus GPIs [76]. These results are consistent with those of the REPLACE-2 trial, in which a statistically significant reduction in the rate of mortality at 1 year was demonstrated only in the subgroup of patients older than 75 years of age [77]. Finally, Lemesle et al. found that bivalirudin use was associated with a 62% relative reduction in postprocedural bleeding (HR: 0.38; 95% CI: 0.22–0.65; p = 0.001) compared with heparin plus GPIs [78].
Access site
The elderly are at particular risk of access-related complications mainly because of the higher prevalence of native vascular disease and a greater susceptibility to the antihrombotic therapy during and after PCI. The radial approach, abolishing almost totally the access site bleeding, is associated with a lower rate of bleeding and similar procedural success rates compared with the femoral approach [79]. Since elderly patients have significantly higher baseline risk of arterial access complication [80], the reduced rates of lower local vascular complications may be beneficial for this group.
These benefits appear to be pronounced among experienced radial operators and in patients with ACS [81–83]. Multiple studies have also shown an association between transradial PCI and reduced mortality [84,85], but the mechanisms underlying this benefit are unclear. Moreover, time-to-ambulation is significantly reduced with the radial approach, which helps eliminate or reduce the risk of venous thrombosis and pulmonary embolism among elderly patients.
Prevention of contrast-induced nephropathy
The presence of multiple comorbidities, including chronic kidney disease (CKD), and more complex lesions, requiring greater amounts of contrast medium during procedures, increases the risk of contrastinduced nephropathy (CIN) that has been associated with adverse outcomes and early and late mortality following PCI [86].
The best approach to prevent CIN is to identify patients at risk using risk scores [87,88], to minimize the amount of administered contrast media and provide adequate periprocedural hydration according to the current guidelines recommendations [12]. The use of nephrotoxic drugs should be suspended for at least 2 days prior to contrast media exposure, while OMT before exposure to contrast media should include statins, β-blockers and angiotensin-converting enzyme inhibitors or sartans.
In CKD patients with diffuse atherosclerosis, performing diagnostic and interventional procedures separately and scheduling staged PCI in multivessel disease patients reduces the total volume exposure to contrast media. The risk of CIN increases significantly when the ratio of contrast volume to GFR exceeds 3.7 [89].
Although serum creatinine is a marker of renal function, it does not represent an ideal marker of acute kidney injury [90]. For this reason, new biomarkers, such as cystatin C and neutrophil gelatinaseassociated lipocalin, which allow an earlier and more accurate diagnosis of acute kidney injury, have been identified [91,92].
Procedural issues
Stent choice should include a comprehensive evaluation of the risk of restenosis, thrombosis, bleeding and patient’s compliance. Bare-metal stents may be considered the device of first choice in elderly patients undergoing PCI, given the primary goal of minimizing the risk of bleeding and the presence of a health status often requiring multiple diagnostic and therapeutic invasive procedures. On the other hand, the high prevalence of CKD, diabetes and complex lesions in this set of patients should make the operators adopt a more effective strategy, in order to reduce the risk of repeat revascularization and implanting drug-eluting stents (DES).
Data from large registries demonstrated that patients receiving DES had significantly better clinical outcomes including mortality, MI and repeat revascularization than those who received bare-metal stents, without an associated increase in major bleeding or stroke [93–95]. These results are consistent even in patients requiring more challenging procedures like chronic total occlusion [96] and small vessel lesions [97]. In the randomized XIMA trial enrolling 800 octogenarian stable patients, DES implantation were associated with a lower incidence of MI and target vessel revascularization, without an increased incidence of major bleeding [98].
Especially in the elderly, the bleeding risk correlates with the duration of dual antiplatelet therapy (DAPT) [99]. Although the optimal duration of DAPT is still lacking scientific ground, in DES trials, as recommended by guidelines, prolonged DAPT intake for at least 12 months was mandatory. Results from recent randomized trials comparing 3 versus 12 months of DAPT among patients with low-risk profile CAD treated with zotarolimus-eluting stents, suggest the noninferiority for short- vs long-term DAPT with no significant difference in any of the individual components of the primary end point (cardiovascular death, MI, stent thrombosis, target vessel revascularization or bleeding) [100,101]. Moreover, in the PARIS registry, most adverse events occurred while patients were taking DAPT and cardiac events after DAPT cessation depended on the clinical circumstance and reason for cessation and attenuates over time; physician-guided discontinuation was associated with a substantially lower MACE risk, while disruptions due to bleeding or noncompliance were associated with a substantially increased risk. Patients who had temporary DAPT interruption lasting up to 14 days did not have an increased rate of thrombotic events [102]. Trials evaluating early struts coverage using the optical coherence tomography imaging demonstrated a low percentage of uncovered struts 3 months after DES implantation, adding new implication on DAPT duration [103].
As previously stated, in patients with culprit-only multivessel disease, the revascularization approach should be envisioned. Previous studies have noted that older patients who were completely revascularized undertook a much higher risk, such as acute or subacute thrombosis, sudden death or bleeding [93,104] and no differences in acute and 12 months total events between completely or incompletely revascularized subjects [43–45].
Lesion preparation and poststenting optimization should be parsimoniously pursued, as these may indeed have a detrimental impact on periprocedural events.
Coronary bifurcations should be approached with a conservative stance, unless a large side branch does compromise itself causing symptoms or instability [105]. Thus, a provisional stenting strategy should be pursued in most coronary bifurcation lesions. Moreover, diffuse stenting should be avoided and spot stenting adopted instead, to minimize the risk of stent thrombosis.
Stent delivery through calcified lesions may be difficult and stent may be underexpanded due to high resistance of the calcified plaques. The use of rotational atherectomy is particularly useful in the case of very tight calcified lesions that may resist dilation at low balloon inflation pressures, or cause coronary rupture at the highest possible balloon pressure.
Future perspective
With the growth of the elderly population, the proportion of these patients undergoing PCI is increasing considerably. Although the development of new therapeutic tools including devices and medications has improved the outcome in elderly patients, this remains less favorable than in younger patients.
To date, evidence regarding PCI in the elderly allow us to confirm that these patients would benefit from a more invasive strategy both in the stable and ACS settings, but given the increase of this population, the need for specifically designed randomized trials may become crucial in the future. In the next years, evidence-based guidelines should be adapted for elderly patients with multimorbidity and the stratification with new risk scores including disease-specific risk, comorbidity and frailty should be common practice. It has been demonstrated that the radial approach is effective in reducing bleeding complications, but future studies should focus specifically on the role of the radial approach in the setting of bivalirudin-based treatment regimens.
In the elderly, as in the other high-risk subgroups, therapeutic strategies and the degree of invasiveness should be tailored as much as possible and a careful and comprehensive approach to patient selection is paramount to obtain the best outcomes.
Finally, the correct duration of DAPT in patients undergoing PCI is still controversial. A better understanding of the relation between struts coverage and adverse events and the development of DES requiring a more reasonable DAPT duration in the elderly is of the utmost importance.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Executive summary
Increased percutaneous coronary intervention-related risk in the elderly
• Coronary artery disease (CAD) represents the leading cause of morbidity and mortality among the elderly patients and its prevalence and severity increases with advancing age.
• The elderly might derive greater benefit from revascularization compared with younger patients but, given the presence of a higher risk for in-hospital mortality and morbidity due to a precarious health status, they are less likely to undergo percutaneous coronary intervention (PCI).
Elderly with chronic coronary
• In choosing the optimal treatment strategy for the individual patient, a cautious risk stratification represents an essential aspect of this clinical decision-making process; both the complexity of CAD and concomitant comorbidities have to be taken into account.
• Evidence from clinical trials suggest that an invasive strategy results in decreased rates of major adverse cardiovascular events and an improved quality of life compared with a conservative strategy of optimization of medical therapy.
Elderly presenting acute coronary syndrome
• Elderly patients have been selectively excluded from acute coronary syndrome (ACS) randomized trials. Therefore, evidence has been extrapolated from studies of younger patients, which precludes extending the study findings to the population that experiences the most morbidity and death from ACS.
• In patients with non-ST-segment elevation ACS, an early coronary angiography and revascularization leads to better in-hospital and long-term outcomes.
• Considerable evidence from registries and randomized trials indicate that primary PCI is superior to fibrinolytic therapy in the elderly patients with ST-elevation myocardial infarction.
How to improve outcomes of PCI in the elderly
• New therapeutic tools have been developed to reduce periprocedural and long term complications:
–– The use of risk scores that include the evaluation of frailty, comorbidities and quality of life;
–– It is essential to tailor antithrombotic therapy, bivalirudin in ACS patients is effective in reducing bleeding rates;
–– The radial approach, abolishing almost totally the access site bleeding, is associated with a lower rate of bleeding compared with the femoral approach and similar procedural success rates;
–– The best approach to prevent contrast-induced nephropathy is to identify patients at risk using risk scores, to minimize the amount of administered contrast media and provide adequate periprocedural hydration;
–– Drug-eluting stents significantly improve clinical outcomes including mortality, myocardial infarction and repeat revascularization compared with those who received bare-metal stents, without an associated increase in major bleeding.
References
Papers of special note have been highlighted as: • of interest; •• of particular interest
- United Nations. World Population Ageing 2009. www.un.org/esa/population/publications/WPA2009/ WPA2009_WorkingPaper.pdf
- Boersma E, Pieper KS, Steyerberg EW et al. Predictors of outcome in patients with acute coronary syndromes without persistent ST-segment elevation. Results from an international trial of 9461 patients. The PURSUIT Investigators. Circulation 101, 2557–2567 (2000).
- Granger CB, Goldberg RJ, Dabbous O et al. Predictors of hospital mortality in the global registry of acute coronary events. Arch. Intern. Med. 163, 2345–2353 (2003).
- Holmes DR Jr, White HD, Pieper KS, Ellis SG, Califf RM, Topol EJ. Effect of age on outcome with primary angioplasty versus thrombolysis. J. Am. Coll. Cardiol. 33, 412– 419 (1999).
- Singh M, Mathew V, Garratt KN et al. Effect of age on the outcome of angioplasty for acute myocardial infarction among patients treated at the Mayo Clinic. Am. J. Med. 108, 187–192 (2000).
- Global Status Report on Noncommunicable Diseases 2010. World Health Organization, Geneva, Switzerland (2011).
- Anderson JL, Adams CD, Antman EM et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology/ American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-STElevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J. Am. Coll. Cardiol. 50, 1–157 (2007).
- Giugliano RP, Lloyd-Jones DM, Camargo CA, Makary MA, O’Donnell CJ. Association of unstable angina guideline care with improved survival. Arch. Intern. Med. 160, 1775–1780 (2000).
- Lakatta EG. Changes in cardiovascular function with aging. Eur. Heart J. 11(Suppl. C), 22–29 (1990).
- Alexander KP, Roe MT, Chen AY et al.; for the CRUSADE Investigators. Evolution in cardiovascular care for elderly patients with non-ST-segment elevation acute coronary syndromes: results from the CRUSADE National Quality Improvement Initiative. J. Am. Coll. Cardiol. 46, 1479–1487 (2005).
- Forman D, Wenger NK. What do the recent American Heart Association/American College of Cardiology Foundation Clinical Practice Guidelines tell us about the evolving management of coronary heart disease in older adults? J. Geriatr. Cardiol. 10(2), 123–128 (2013).
- Wijns W, Kolh P, Danchin N et al. Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (-11) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 31, 2501–2555 (2010).
- Antonsen L, Jensen LO, Thayssen P et al. Comparison of outcomes of patients >80 years of age having percutaneous coronary intervention according to presentation (stable vs unstable angina pectoris/non-ST-segment elevation myocardial infarction vs ST-segment elevation myocardial infarction). Am. J. Cardiol. 108, 1395–1400 (2011).
- Fokkema ML, James SK, Albertsson P et al. Population trends in percutaneous coronary intervention: 20-year results from the SCAAR (Swedish Coronary Angiography and Angioplasty Registry). J. Am. Coll. Cardiol. 61(12), 1222–1230 (2013).
- Afilalo J, Karunananthan S, Eisenberg MJ, Alexander KP, Bergman H. Role of frailty in patients with cardiovascular disease. Am. J. Cardiol. 103, 1616–1621 (2009).
- Singh M, Rihal CS, Lennon RJ et al. Influence of frailty and health status on outcomes in patients with coronary disease undergoing percutaneous revascularization. Circ. Cardiovasc. Qual. Outcomes 4, 496–502 (2011).
- Rathore SS, Mehta RH, Wang Y, Radford MJ, Krumholz HM. Effects of age on the quality of care provided to older patients with acute myocardial infarction. Am. J. Med. 114(4), 307–315 (2003).
- Sheifer SE, Rathore SS, Gersh BJ et al. Time to presentation with acute myocardial infarction in the elderly: associations with race, sex, and socioeconomic characteristics. Circulation 102 (14), 1651–1656 (2000).
- Singh M, Peterson ED, Roe MT et al. Trends in the association between age and in-hospital mortality after percutaneous coronary intervention: National Cardiovascular Data Registry experience. Circ. Cardiovasc. Interv. 2, 20–26 (2009).
- Ferrari AU, Radaelli A, Centala M. Aging and the cardiovascular system. J. Appl. Physiol. 95, 2591–2597 (2003).
- Bauer T, Mollmann H, Weidinger F et al. Predictors of hospital mortality in the elderly undergoing percutaneous coronary intervention for acute coronary syndromes and stable angina. Int. J. Cardiol. 151(2), 164–169 (2011).
- McKellar SH, Brown ML, Frye RL, Schaff HV, Sundt TM. Comparison of coronary revascularization procedures in octogenarians: a systematic review and meta-analysis. Nat. Clin. Pract. Cardiovasc. Med. 5, 738–746 (2008).
- National Institutes of Health NH, Lung, and Blood Institute. Morbidity & Mortality: 2012 Chart Book on Cardiovascular, Lung, and Blood Diseases. National Heart, Lung, and Blood Institute, Bethesda, MD, USA (2012).
- Sinning JM, Asdonk T, Erlhofer C et al. Combination of angiographic and clinical characteristics for the prediction of clinical outcomes in elderly patients undergoing multivessel PCI. Clin. Res. Cardiol. 102(12), 865–873 (2013).
- Kappetein AP, Feldman TE, Mack MJ et al. Comparison of coronary bypass surgery with drug-eluting stenting for the treatment of left main and/or three-vessel disease: 3-year follow-up of the SYNTAX trial. Eur. Heart J. 32, 2125–2134 (2011).
- Farkouh ME, Domanski M, Sleeper LA et al.; the FREEDOM Trial Investigators. Strategies for multivessel revascularization in patients with diabetes. N. Engl. J. Med. 367, 2375–2384 (2012).
- Lichtman JH, Kapoor R, Wang Y et al. Temporal trends of outcomes for nonagenarians undergoing coronary artery bypass grafting, 1993 to 1999. Am. J. Cardiol. 100, 1630–1634 (2007).
- Teo KK, Sedlis SP, Boden WE et al. Optimal medical therapy with or without percutaneous coronary intervention in older patients with stable coronary disease: a pre-specified subset analysis of the COURAGE (Clinical Outcomes Utilizing Revascularization and Aggressive druG Evaluation) trial. J. Am. Coll. Cardiol. 54(14), 1303–1308 (2009).
- The TIME Investigators. Trial of invasive medical therapy in elderly patients with chronic symptomatic coronary-artery disease (TIME): a randomized trial. Lancet 358, 951–957 (2001).
- Pfisterer M. Long-term care in elderly patients with clinical angina managed therapy by optimal medical therapy. Circulation 110, 1213–1218 (2004).
- Graham MM, Norris CM, Galbraith PD, Knudtson ML, Ghali WA; for the APPROACH Investigators. Quality of life after coronary revascularization in the elderly. Eur. Heart J. 27, 1690–1698 (2006).
- Rittger H, Hochadel M, Behrens S et al. Interventional treatment and outcome in elderly patients with stable coronary artery disease: results from the German ALKK registry. Herz 39(2), 212–218 (2013).
- Fox KA, Dabbous OH, Goldberg RJ et al. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (GRACE). BMJ 333, 1091 (2006).
- Antman EM, Hand M, Armstrong PW et al. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, writing on behalf of the 2004 Writing Committee. Circulation 117, 296–329 (2008).
- Fox KA, Poole-Wilson PA, Henderson RA et al.; Randomized Intervention Trial of unstable Angina Investigators. Interventional versus conservative treatment for patients with unstable angina or non-ST-elevation myocardial infarction: the British Heart Foundation RITA 3 randomised trial. Randomized Intervention Trial of unstable Angina. Lancet 360, 743–751 (2002).
- The Fragmin and Fast Revascularization During Instability in Coronary Artery Disease (FRISC) Investigators. Invasive compared with non-invasive treatment in unstable coronaryartery disease: FRISC-II prospective randomised multicentre study. Lancet 354, 708 (1999).
- Cannon CP, Weintraub WS, Demopoulos L et al.; TACTICS (Treat Angina with Aggrastat and Determine Cost of Therapy with an Invasive or Conservative Strategy) Thrombolysis in Myocardial Infarction 18 Investigators. Comparison of early invasive and conservative strategies in patients with unstable coronary syndromes treated with the glycoprotein IIb/IIIa inhibitor tirofiban. N. Engl. J. Med. 344, 1879–1887 (2001).
- Stone PH, Thompson B, Anderson HV et al. Influence of race, sex, and age on management of unstable angina and non-Qwave myocardial infarction: the TIMI III registry. JAMA 275, 1104–1112 (1996).
- Giugliano RP, Camargo CA Jr, Lloyd-Jones DM et al. Elderly patients receive less aggressive medical and invasive management of unstable angina: potential impact of practice guidelines. Arch. Intern. Med. 158, 1113–1120 (1998).
- Hasdai D, Holmes DR Jr, Criger DA, Topol EJ, Califf RM, Harrington RA. Age and outcome after acute coronary syndromes without persistent ST-segment elevation. Am. Heart J. 139, 858–866 (2000).
- Bhatt DL, Greenbaum A, Roe MT, Harrington RA, Li Y, Smith S. An early invasive approach to acute coronary syndromes in CRUSADE: a dissociation between clinical guidelines and current practice [Abstract]. Circulation 106(Suppl. 19), II-494 (2002).
- Yusuf S, Flather M, Pogue J et al. Variations between countries in invasive cardiac procedures and outcomes in patients with suspected unstable angina or myocardial infarction without initial ST elevation. OASIS (Organisation to Assess Strategies for Ischaemic Syndromes) Registry Investigators. Lancet 352, 507–514 (1998).
- Varani E, Aquilina M, Balducelli M et al. Percutaneous coronary interventions in octogenarians: acute and 12 month results in a large single-centre experience. Catheter Cardiovasc. Interv. 73, 449–454 (2009).
- Glaser R, Selzer F, Faxon DP et al. Clinical progression of incidental, asymptomatic lesions discovered during culprit vessel coronary intervention. Circulation 111, 143–149 (2005).
- Chen J, Xue Q, Bai J et al. Incomplete revascularization in the drug eluting stent era permits meaningful long-term (12–78 months) outcomes in patients ≥75 years with acute coronary syndrome. J. Geriatr. Cardiol. 9, 336–343 (2012).
- Antman EM, Cohen M, Bernink PJ et al. The TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision making. JAMA 284, 835–842 (2000).
- Rosengren A, Wallentin L, Simoons M et al. Age, clinical presentation, and outcome of acute coronary syndromes in the Euroheart acute coronary syndrome survey. Eur. Heart J. 27, 789–795 (2006).
- Eagle KA, Lim MJ, Dabbous OH et al. A validated prediction model for all forms of acute coronary syndrome: estimating the risk of 6-month postdischarge death in an international registry. JAMA 291, 2727–2733 (2004).
- Cannon CP, Weintraub WS, Demopoulos LA et al. Comparison of early invasive and conservative strategies in patients with unstable coronary syndromes treated with the glycoprotein IIb/IIIa inhibitor tirofiban. N. Engl. J. Med. 344(25), 1879–1887 (2001).
- Alexander KP, Roe MT, Chen AY et al.; for the CRUSADE Investigators. Evolution in cardiovascular care for elderly patients with non-ST-segment elevation acute coronary syndromes: results from the CRUSADE National Quality Improvement Initiative. J. Am. Coll. Cardiol. 46, 1479–1487 (2005).
- Damman P, Clayton T, Wallentin L et al. Effects of age on long-term outcomes after a routine invasive or selective invasive strategy in patients presenting with non-ST segment elevation acute coronary syndromes: a collaborative analysis of individual data from the FRISC II, ICTUS-RITA-3 (FIR) trials. Heart 98, 207–213 (2012).
- Savonitto S, Cavallini C, Petronio AS et al. Early aggressive versus initially conservative treatment in elderly patients with non-ST-segment elevation acute coronary syndrome: a randomized controlled trial. JACC Cardiovasc. Interv. 5, 906–916 (2012).
- Rana O, Ryan M, O’Kane P et al. Percutaneous coronary intervention in the very elderly (>85 years old): trends and outcomes. Br. J. Cardiol. 20, 27–31 (2013).
- Grosmaitre P, Le Vavasseur O, Yachouh E et al. Significance of atypical symptoms for the diagnosis and management of myocardial infarction in elderly patients admitted to emergency departments. Arch. Cardiovasc. Dis. 106(11), 586–592 (2013).
- Smith LG, Herlitz J, Karlsson T, Berger AK, Luepker RV. International comparison of treatment and long-term outcomes for acute myocardial infarction in the elderly: Minneapolis/St. Paul, MN, USA and Goteborg, Sweden. Eur. Heart J. 34(41), 3191–3197 (2013).
- Medina HM, Cannon CP, Fonarow GC et al. Reperfusion strategies and quality of care in 5339 patients age 80 years or older presenting with ST-elevation myocardial infarction: analysis from get with the guidelines-coronary artery disease. Clin. Cardiol. 35(10), 632–640 (2012).
- Keeley EC, Boura JÁ, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomized trials. Lancet 361, 13–20 (2003).
- Stone GW, Grines CL, Browne KF et al. Predictors of in-hospital and 6 month outcome after acute myocardial infarction in the repefusion era; the Primary Angioplasty in Myocardial Infarction (PAMI) trial. J. Am. Coll. Cardiol. 25, 370–377 (1995).
- The Global Use of Strategies to Open Occluded Coronary Arteries in Acute coronary Syndromes (GUSTO IIb) Angioplasty Substudy Investigators. A clinical trial comparing primary coronary angioplasty with tissue plasminogen activator for acute myocardial infarction. N. Engl. J. Med. 336, 1621–1628 (1997).
- Mehta RH, Sadiq I, Goldberg RJ et al.; for the GRACE Investigators. Effectiveness of primary percutaneous coronary intervention compared with that of thrombolytic therapy in elderly patients with acute myocardial infarction. Am. Heart J. 147, 253–259 (2004).
- Andersen HR, Nielsen TT et al. A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. N. Engl. J. Med. 349(8), 733–742 (2003).
- Goldenberg I, Matetzky S, Halkin A et al. Primary angioplasty with routine stenting compared with thrombolytic therapy in elderly patients with acute myocardial infarction. Am. Heart J. 145(5), 862–867 (2003).
- Degeare VS, Stone GW, Grines CL et al. Angiografic and clinical characteristics associated with increase in hospital mortality in elderly patients with acute myocardial infarction undergoing percutaneous intervention (a pooled analysis of the primary angioplasty in myocardial infarction trials). Am. J. Cardiol. 86, 30–34 (2000).
- de Boer SP, Westerhout CM, Simes RJ et al.; for the PCAT- 2 Trialists Collaborators Group. Mortality and morbidity reduction by primary percutaneous coronary intervention is independent of the patient’s age. JACC Cardiovasc. Interv. 3, 324–331 (2010).
- de Boer MJ, Ottervanger JP, van’t Hof AW et al. Reperfusion therapy in the elderly patients with acute myocardial infarction: a randomized comparison of primary angioplasty and thrombolytic therapy. J. Am. Coll. Cardiol. 39, 1723–1728 (2002).
- Grines C. SENIOR PAMI: a prospective randomized trial of primary angioplasty and thrombolytic therapy in elderly patients with acute myocardial infarction. Presented at: Transcatheter Cardiovascular Therapeutics 2005. Washington, DC, USA, 19 October 2005.
- Bueno H, Betriu A, Heras M et al. Primary angioplasty vs fibrinolysis in very old patients with acute myocardial infarction: TRIANA (TRatamiento del Infarto Agudo de miocardio eN Ancianos) randomized trial and pooled analysis with previous studies. Eur. Heart J. 32(1), 51–60 (2011).
- Graham MM, Galbraith PD, O’Neill D et al. Frailty and outcome in elderly patients with acute coronary syndrome. Can. J. Cardiol. 29(12), 1610–1615 (2013).
- Ndrepepa G, Berger PB, Mehilli J et al. Periprocedural bleeding and 1-year outcome after percutaneous coronary interventions: appropriateness of including bleeding as a component of a quadruple end point. J. Am. Coll. Cardiol. 51, 690–697 (2008).
- Chatriwalla AK, Amin AP, Kennedy KF et al. National Cardiovascular Data R: association between bleeding events and inhospital mortality after percutaneous coronary intervention. JAMA 309, 1022–1029 (2013).
- Rao SV, Dai D, Subherwal S et al. Association between periprocedural bleeding and long-term outcomes following percutaneous coronary intervention in older patients. JACC Cardiovasc. Interv. 5, 958–965 (2012).
- Mehran R, Pocock S, Nikolsky E et al. Impact of bleeding on mortality after percutaneous coronary intervention results from a patient-level pooled analysis of the REPLACE-2 (Randomized Evaluation of PCI Linking Angiomax to Reduced Clinical Events), ACUITY (Acute Catheterization and Urgent Intervention Triage Strategy), and HORIZONSAMI (Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction) trials. JACC Cardiovasc. Interv. 4, 654–664 (2011).
- Wiviott SD, Braunwald E, McCabe CH et al.; TRITONTIMI 38 Investigators. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N. Engl. J. Med. 357, 2001–2015 (2007).
- Roe MT, Goodman SG, Ohman EM et al. Elderly patients with acute coronary syndromes managed without revascularization insights into the safety of long-term dual antiplatelet therapy with reduced-dose prasugrel vs standarddose clopidogrel. Circulation 128, 823–833 (2013).
- Husted S, James S, Becker RC et al. Ticagrelor versus clopidogrel in elderly patients with acute coronary syndromes: a substudy from the prospective randomized PLATelet inhibition and patient Outcomes (PLATO) trial. Circ. Cardiovasc. Qual. Outcomes 5, 680–688 (2012).
- Lopes RD, Alexander KP, Manoukian SV et al. Advanced age, antithrombotic strategy, and bleeding in non-STsegment elevation acute coronary syndromes. Results from the ACUITY (Acute Catheterization and Urgent Intervention Triage Strategy) trial. J. Am. Coll. Cardiol. 53, 1021–1030 (2009).
- Feit F, Voeltz MD, Attubato MJ et al. Predictors and impact of major hemorrhage on mortality following percutaneous coronary inter- vention from the REPLACE-2 Trial. Am. J. Cardiol. 100, 1364–1369 (2007).
- Lemesle G, De Labriolle A, Bonello L et al. Impact of bivalirudin on in-hospital bleeding and six-month outcomes in octogenarians undergoing percutaneous coronary intervention. Catheter Cardiovasc. Interv. 74(3), 428–435 (2009).
- Jolly SS, Amlani S, Hamon M et al. Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and metaanalysis of randomized trials. Am. Heart J. 157, 132–140 (2009).
- Piper WD, Malenka DJ, Ryan TJ et al. Predicting vascular complications in percutaneous coronary interventions. Am. Heart J. 145, 1022–1029 (2003).
- Romagnoli E, Biondi-Zoccai G, Sciahbasi A et al. Radial Versus Femoral Randomized Investigation in ST- segment Elevation Acute Coronary Syndrome: The RIFLE-STEACS (Radial Versus Femoral Randomized Investigation in STElevation Acute Coronary Syndrome) study. J. Am. Coll. Cardiol. 60, 2481–2489 (2012).
- Jolly SS, Yusuf S, Cairns J et al.; RIVAL trial group. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet 377, 1409–1420 (2011).
- Verheugt FW, Steinhubl SR, Hamon M et al. Incidence, prognostic impact, and influence of antithrombotic therapy on access and nonaccess site bleeding in percutaneous coronary intervention. JACC Cardiovasc. Interv. 4, 191–197 (2011).
- Chase AJ, Fretz EB, Warburton WP et al. Association of the arterial access site at angioplasty with transfusion and mortality:Association of the arterial access site at angioplasty with transfusion and mortality: the MORTAL study (Mortality benefit Of Reduced Transfusion after percutaneous coronary intervention via the Arm or Leg. Heart 94, 1019–1025 (2008).
- Joyal D, Bertrand O, Rinfret S et al. Meta-analysis of ten trials on the effectiveness of the radial versus the femoral approach in primary percutaneous coronary intervention. Am. J. Cardiol. 109, 813–818 (2012).
- McCullough PA. Contrast-induced acute kidney injury. J. Am. Coll. Cardiol. 51, 1419–1428 (2008).
- Mehran R, Aymong ED, Nikolsky E et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J. Am. Coll. Cardiol. 44, 1393–1399 (2004).
- Gurm HS, Seth M, Kooiman J, Share DA. Novel tool for reliable and accurate prediction of renal complications in patients undergoing percutaneous coronary intervention. J. Am. Coll. Cardiol. 61(22), 2242–2248 (2013).
- Laskey WK, Jenkins C, Selzer F et al. Volume-to-creatinine clearance ratio: a pharmacokinetically based risk factor for prediction of early creatinine increase after percutaneous coronary intervention. J. Am. Coll. Cardiol. 50, 584–590 (2007).
- Guitterez NV, Diaz A, Timmis GC et al. Determinants of serum creatinine trajectory in acute contrast nephropathy. J. Interv. Cardiol. 15, 349–354 (2002).
- Briguori C, Visconti G, Rivera NV et al. Cystatin C and contrastinduced acute kidney injury. Circulation 121(19), 2117–2122 (2010).
- McCullough PA, Williams FJ, Stivers DN et al. Neutrophil gelatinase-associated lipocalin: a novel marker of contrast nephropathy risk. Am. J. Nephrol. 35(6), 509–514 (2012).
- Douglas PS, Brennan JM, Anstrom KJ et al. Clinical effectiveness of coronary stents in elderly persons: results from 262,700 Medicare patients in the American College of Cardiology-National Cardiovascular Data Registry. J. Am. Coll. Cardiol. 53, 1629–1641 (2009).
- Patel MR, Marso SP, Dai D et al. Comparative effectiveness of drug-eluting versus bare-metal stents in elderly patients undergoing revascularization of chronic total coronary occlusions: results from the national cardiovascular data registry, 2005–2008. JACC Cardiovasc. Interv. 5, 1054–1061 (2012).
- The impact of sirolimus-eluting stent implantation in the elderly: a report from the e-Cypher Registry (Abstr). Circulation 110, II–3009 (2004).
- Wang TY, Masoudi FA, Messenger JC et al. Percutaneous coronary intervention and drug-eluting stent use among patients > = 85 years of age in the United States. J. Am. Coll. Cardiol. 59, 105–112 (2012).
- Puymirat E, Mangiacapra F, Peace A et al. Safety and effectiveness of drug-eluting stents versus bare-metal stents in elderly patients with small coronary vessel disease. Arch. Cardiovasc. Dis. 106(11), 554–561 (2013).
- de Belder A, de la Torre Hernandez JM, Lopez-Palop R et al. A prospective randomized trial of everolimus-eluting stents versus bare metal stents in octogenarians: xience or vision stents for the management of angina in the elderly – the Xima trial. J. Am. Coll. Cardiol. 63(14), 1371–1375 (2013).
- Tada T, Natsuaki M, Morimoto T et al. CREDO-Kyoto PCI/ CABG Registry Cohort-2 Investigators. Duration of dual antiplatelet therapy and long-term clinical outcome after coronary drug-eluting stent implantation: landmark analyses from the CREDO-Kyoto PCI/CABG Registry Cohort-2. Circ. Cardiovasc. Interv. 5, 381–391 (2012).
- Kim B-K, Hong M-K, Shin DH et al. A new strategy for discontinuation of dual antiplatelet therapy: the RESET Trial (real safety and efficacy of 3-month dual antiplatelet therapy following endeavor zotarolimus-eluting stent implantation. J. Am. Coll. Cardiol. 60, 1340–1348 (2012).
- Feres F, Costa RA, Abizaid A et al. Three vs twelve months of dual antiplatelet therapy after zotarolimus-eluting stents. The OPTIMIZE randomized trial. JAMA 310(23), 2510–2522 (2013).
- Mehran R, Baber U, Steg PG et al. Cessation of dual antiplatelet treatment and cardiac events after percutaneous coronary intervention (PARIS): 2 year results from a prospective observational study. Lancet 382(9906), 1714–1722 (2013).
- Kim S, Kim JS, Shin DH et al. Comparison of early strut coverage between zotarolimus- and everolimus-eluting stents using optical coherence tomography. Am. J. Cardiol. 111(1), 1–5 (2013).
- Daniel EF, David AC, Stephen GE et al. Long-term paclitaxel-eluting stent outcomes in elderly patients. Circ. Cardiovasc. Interv. 2, 178–187 (2009).
- Maeng M, Holm NR, Erglis A et al. Long-term results after simple versus complex stenting of coronary artery bifurcation lesions: Nordic Bifurcation Study 5-year follow-up results. J. Am. Coll. Cardiol. 62(1), 30–34 (2013).
• Demonstrated that the inclusion of the measures of frailty, comorbidities and quality of life improves the discriminating ability of the risk model derived from routine cardiovascular risk factors.
•• The TIME trial was the first prospective randomized treatment trial in elderly patients with chronic symptomatic coronary artery disease. At 4-year follow-up, an invasive strategy resulted in decreased major adverse cardiovascular events and improved quality of life compared with a conservative strategy of optimization of medical therapy.
• This meta-analysis of the FRISC II–ICTUS–RITA-3 trials shows that long-term reduction in the composite of cardiovascular death or myocardial infarction with routine invasive strategy compared with a selective invasive strategy is mainly seen in patients aged ≥65 years.
• The results of this study complement those previously found in the Senior PAMI trial suggesting that primary percutaneous coronary intervention may offer clinical advantage over fibrinolytic therapy as manifested by the trends towards improvements in the combined end point of death, reinfarction and stroke at 30 days in the oldest patients.