Special Issue Article - Imaging in Medicine (2011) Volume 3, Issue 6
Application of ultrasound-guided wire placement in head and neck cancer biopsy: where are we now?
Dimitra Christodoulou1*, Jasdeep Bajwa1, Gulcan Gok2, Robert Hywel Thomas1 and David Crispin Howlett1
1Radiology Department, Eastbourne District General Hospital, Kings Drive, Eastbourne, East Sussex, BN21 2UD, UK
2Maxillofacial Surgery Department, Eastbourne District General Hospital, Kings Drive, Eastbourne, East Sussex, BN21 2UD, UK
- *Corresponding Author:
- Dimitra Christodoulou
Radiology Department Eastbourne
District General Hospital Kings Drive
Eastbourne, East Sussex BN21 2UD, UK
Tel.: 07872164848
Fax: +44 1323 435 853
E-mail: dimitra1@doctors.org.uk
Abstract
Ultrasound-guided wire localization is a well-recognized technique in breast surgical practice and has recently been described in the management of impalpable head and neck pathology with both benign and malignant lesions having been successfully excised utilizing this technique. This article reviews the technique of ultrasound-guided wire localization in the neck, its benefits and indications, and its current and future applications.
Keywords
head and neck pathology; impalpable; ultrasound-guided wire localization
Background
Ultrasound-guided wire localization (USGWL), or ultrasound-guided needle localization, is a wellestablished technique in the management of breast pathology [1]. Its use in the management of impalpable head and neck lesions has been described more recently with benefits of accurate operative localization, reduced operating time and reduced tissue damage being cited [2–4]. Localization of impalpable lesions in a region of such complex anatomy is attractive, especially if lesions are tiny metastatic deposits. USGWL can be particularly useful in the postinstrumentation neck where there has been distortion of normal anatomy.
Technique of USGWL
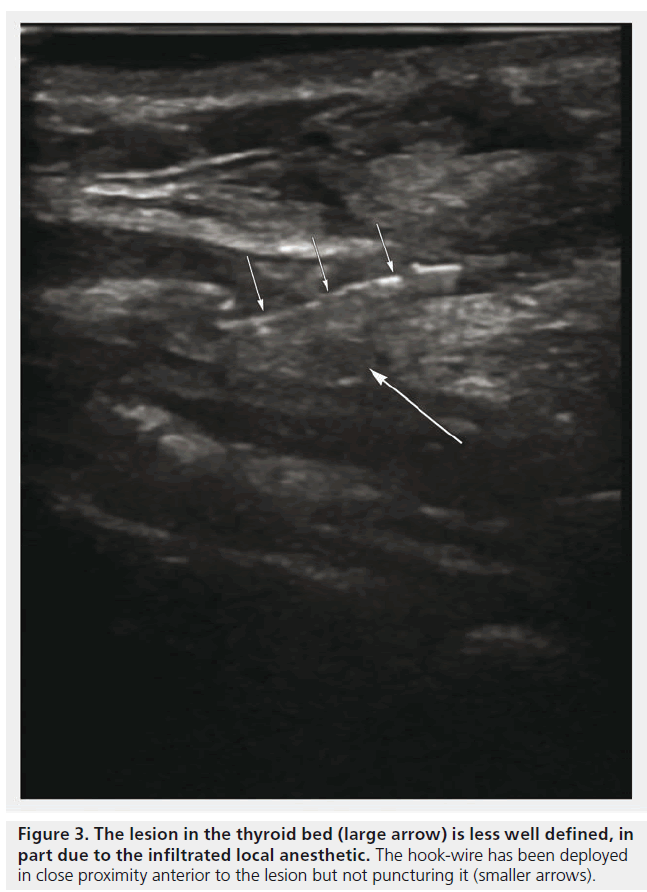
Usually the procedure is performed preoperatively in the ultrasound department, although it can be carried out in theater. This will be discussed further later. In the head and neck, the lesion of interest is identified sonographically using a high resolution linear array broadband (6–15 MHz) ultrasound probe. The frequency of the transducer can be varied according to the depth of the lesion. The access point for the wire is marked on the skin, which is then cleaned and draped as part of the aseptic technique used to perform the procedure. The transducer is covered with a sterile probe cover and sterile coupling gel is used. Local anesthetic is instilled with care under ultrasound guidance as small lesions may be obscured by the infiltrated fluid. Infiltrating up to the lesion rather than into it helps to avoid this problem as does real-time scanning. A small nick is made in the skin to aid the passage of the needle.
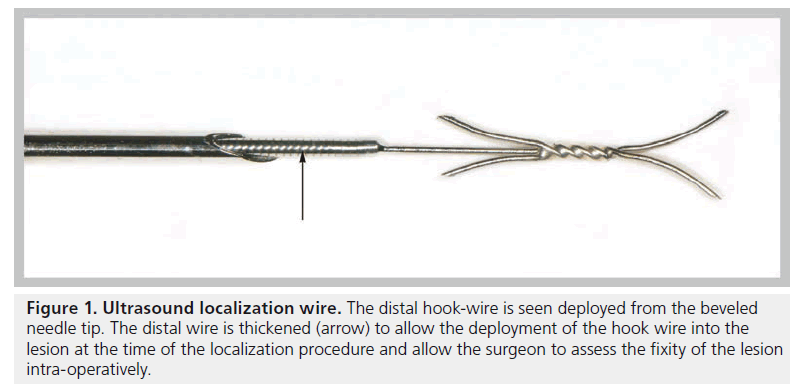
The bore of the beveled needle used in wire localizations contains the hook-wire within it which is anchored in place only when fully extruded from the needle (Figure 1). The wire component protrudes beyond the base of the needle and is used to gently push the hook out of the needle to deploy it when the needle tip position is satisfactory. The needles are available in different lengths and diameters. The authors use a 19 gauge needle for wire localizations in the head and neck, through which the wire inserts centrally, as described.
Figure 1. Ultrasound localization wire. The distal hook-wire is seen deployed from the beveled needle tip. The distal wire is thickened (arrow) to allow the deployment of the hook wire into the lesion at the time of the localization procedure and allow the surgeon to assess the fixity of the lesion intra-operatively.
Using ultrasound guidance, the lesion is identified and the needle containing the hook-wire is advanced so that its tip is located either within the lesion or in proximity to it. The hook is deployed by fixing the needle firmly with one hand and gently advancing the wire with the other until there is an audible and palpable ‘click’. At this point the hook-wire is anchored within the tissues and cannot usually be retracted, although there are needles available that have retractable hooks. The wire is thickened distally to allow for manipulation during deployment. In addition, the distal thickening allows the surgeon to manipulate the lesion during the dissection to assess for fixity and mobility.
The needle is removed over the wire and the thread extending from the tip of the hook-wire is seen on the skin surface. This is flexible and soft compared with the distal portion and can be trimmed or folded back onto the patient’s skin. The thread may be fixed with a crocodile clip to avoid migration of the wire, although the hook-wire itself tends to provide adequate fixation.
After deployment, with the patient still assuming the position for surgery, the hook may be scanned again and a skin marker placed overlying the lesion indicating its site and depth relative to surface anatomy. The depth of the wire from the skin surface is also recorded. Some needles possess centimeter measurement markers to accurately gauge the distance from the skin to the lesion. Sonographic needle visualization can be improved using a granular coating over the needle tip, which deflects the ultrasound beam making the needle tip echogenic and easier to visualize within the soft tissues. These needle types are currently only available to use on a case-by-case basis.
As a result of the USGWL technique the surgeon can follow the wire from the skin surface to locate the otherwise impalpable lesion.
Technical factors
USGWL for impalpable lesions is particularly useful in patients with disrupted anatomy, for example, secondary to radiotherapy or as a result of previous instrumentation. It may also be considered in benign disease where there has not been previous surgery if the surgeon feels it will be beneficial. A diagnostic ultrasound is performed prior to the USGWL procedure and ideally individual cases are then discussed by the surgeon and radiologist. This is useful for the radiologist to determine the position of the neck during the operation and the route of dissection in order to allow patient positioning during wire localization. It is also helpful if the surgeon can attend the ultrasound department for the wire localization procedure and can also mark the incision site onto the patient with a marker pen. The USGWL procedure can then be performed in the same plane of approach and patient position to complement subsequent surgical intervention.
The wire can be deployed either within, or in proximity to, the lesion depending on local anatomy and pathology and the surgeon must be aware of how the wire has been deployed to ensure adequate resection in theater.
Review of imaging, clinical examination and available histology will assess the possibility of lesion malignancy. In some cases, it is desirable to avoid puncturing the lesion and leaking contents into the surrounding area and needle tract due to the potential risk of tumor seeding. Tumor seeding along the tract created by fine needle aspirations and radiofrequency ablations has been documented [5–7]. Tract seeding remains a hypothetical risk in any intervention, particularly if multiple passes are required, and tends to relate to needle size. In the case of large thyroglossal cysts under pressure, needle localization may risk bursting the cyst and seeding the contents ectopically. Lesion localization using a wire has the benefit of the surgeon visualizing the wire position at the time of the operation and being able to excise the wire tract in addition to the lesion to reduce the risk of seeding.
Other potential complications of the localization procedure are related to damage to vital structures that are in close proximity in the head and neck. These complications include vascular, neurological and upper aerodigestive tract injury, although the major vessels and esophagus are clearly identified sonographically. In cases where the needle tract is not excised, the tissues through which the wire passes will have resultant edema, which may be similar to that expected from a needle biopsy in another anatomical region. This, however, is offset by the benefit of accurate intra-operative localization that USGWL offers, and subsequent reduction in operating time and intra-operative tissue damage.
Both pre- and intra-operative USGWL have been documented. Placing the wire pre-operatively in the ultrasound department ensures that equipment is readily available, there are sufficient staff skilled in this procedure, and the environment is familiar for the radiologist and optimal lighting conditions can be achieved. In addition, the surgeon may be present at the time of the scan, which is useful for surgical planning. However, intraoperative ultrasound has its advantages, including minimizing patient anxiety as the wire placement and lesion excision can be performed together, and helping to yield immediate results as in the case of histological examination of testicular lesions [8]. In addition, with no delay between wire localization and theater, the patient will not be moving and the risk of wire migration is therefore avoided.
Applications in the head & neck
USGWL has been described for both malignant and benign lesions within the head and neck [9–11].
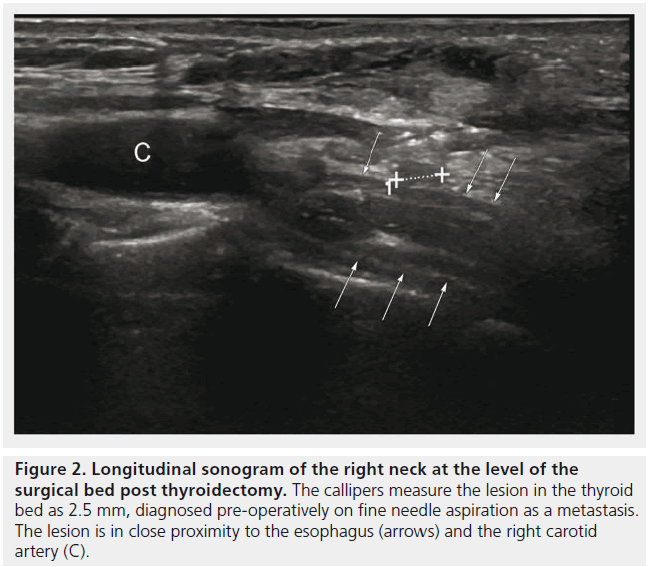
It has been used in the context of recurrent thyroid cancer determined by a rising thyroglobulin level, follow-up staging scans and positive cytology from a fine needle aspirate of a thyroid nodule in the thyroid bed [Howlett DC, Unpublished Data]. A hook-wire was placed adjacent to the 2.5 mm metastatic nodule bounded by the carotid artery laterally, esophagus posteriorly and trachea medially (Figures 2 & 3). This was a technically difficult USGWL due to the location and proximity of vital structures. Histology confirmed excised metastatic papillary thyroid carcinoma.
Figure 2. Longitudinal sonogram of the right neck at the level of the surgical bed post thyroidectomy. The callipers measure the lesion in the thyroid bed as 2.5 mm, diagnosed pre-operatively on fine needle aspiration as a metastasis. The lesion is in close proximity to the esophagus (arrows) and the right carotid artery (C).
USGWL for recurrent lymph node metastases in papillary thyroid carcinoma can be more effective than neck dissection [9]. USGWL has been used for selected lymph node diagnosis [10] and Zimmerman et al. described intraoperative ultrasound-guided needle localization in neck re-exploration where fibrous tissue can obscure the lesion during the operation [11].
Thomas et al. described a patient with a history of appendiceal carcinoid who presented with symptoms of recurrence and had a negative staging CT [3]. Further imaging with an octreotide isotope scan and ultrasound confirmed recurrence in an impalpable lymph node in the neck. Preoperatively, a wire was deployed in proximity to the level IV left neck lymph node adjacent to the common carotid and subclavian arteries and resected at surgery.
In the context of benign lesions, Thomas et al. also describe a patient with persistent thyrotoxicosis post-thyroidectomy for Grave’s disease [3]. An ultrasound of the neck demonstrated a solid nodule in the infra-hyoid region. As the histology from the initial thyroidectomy had demonstrated micropapillary carcinoma as an incidental finding, a biopsy was performed to confirm benignancy. A thyroid uptake scan demonstrated ectopic thyroid tissue in the infrahyoid region. The ectopic thyroid tissue was impalpable clinically but visible on ultrasound, and therefore USGWL was used, resulting in successful excision of the benign lesion.
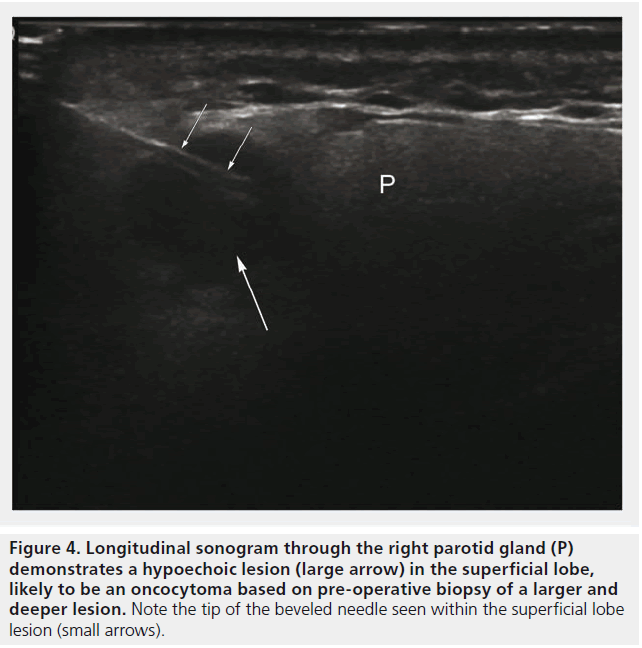
Figure 4. Longitudinal sonogram through the right parotid gland (P) demonstrates a hypoechoic lesion (large arrow) in the superficial lobe, likely to be an oncocytoma based on pre-operative biopsy of a larger and deeper lesion. Note the tip of the beveled needle seen within the superficial lobe lesion (small arrows).
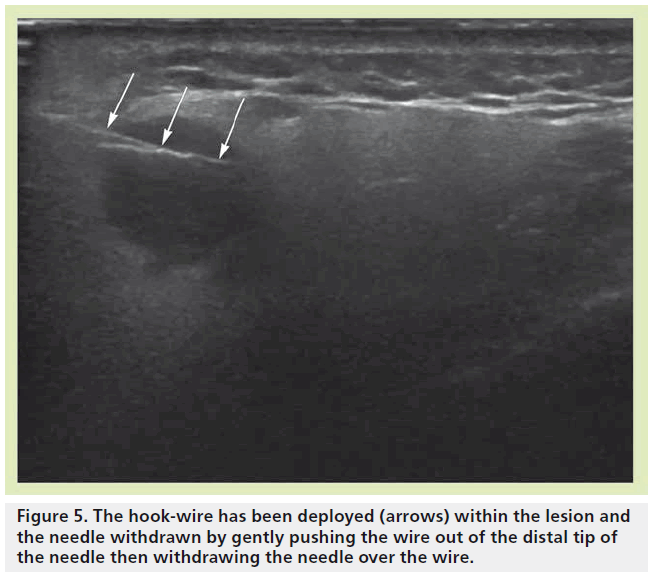
Breeze et al. described a symptomatic neck swelling, which was identified clinically on initial examination, found to be cystic on ultrasound and aspirated under ultrasound guidance [12]. Cytology confirmed a benign branchial cyst; however, following the aspiration, the cyst became clinically impalpable. It remained visible sonograpically and preoperative USGWL was performed to assist the surgeon. Intraoperatively the cyst was only palpable late into the operation as it was encased in dense fibrous tissue. Woodhouse et al. described the necessity of USGWL to target a parotid lesion for excisional biopsy for a definitive histological diagnosis to avoid parotidectomy as per the patient’s request [4]. The patient was an elderly male who presented with a right parotid swelling for 6 months that was painless and nonprogressive. Multiple, bilateral, circumscribed hypoechoic lesions were identified in both glands on ultrasound, identical in texture (Figure 4). MRI demonstrated multiple encapsulated lesions of similar morphology and the lesions were thought to be of the same etiology. Core biopsies were taken from a dominant lesion on the right, and histology of the lesion suggested that it was likely to be a benign oncocytoma, but malignancy could not be entirely excluded due to the nature of oncocytic carcinoma diagnosis. As the patient did not want a parotidectomy, the decision was made to remove the superficial lesion for histology, and assume that the other lesions were similar due to their imaging appearances. The lesions within the parotid gland were in close proximity and the authors were keen to avoid breaching the capsule of the larger lesion due to the possible risk of malignancy, or seeding from a benign lesion. Preoperative USGWL was therefore favored over skin marking, targeting a small superficial lesion (Figure 5). The wire was introduced via a pre-auricular approach aligned to the surgical operative plane to ensure complete excision of the lesion and the needle tract to remove any risks of seeding. A diagnosis of parotid oncocytoma was confirmed on histology. The remaining parotid lesions have remained static over 2 years based on clinical follow-up and MRI surveillance. These cases demonstrate the utility of USGWL for malignant and benign lesions, and the efficacy of the technique in guiding surgeons to ensure excision of impalpable lesions.
Ultrasound
Ultrasound is an appealing imaging modality as it is readily available, inexpensive and safe. Not only can scans be performed quickly but imaging is in real time, can be used for most areas of the body and is particularly amenable to assess complex head and neck anatomy. In addition, ultrasound equipment is portable and can be performed pre- or intra-operatively as required. Hence, ultrasound has significant advantages over CT, MR and fluoroscopy. However, the operator needs to be trained in ultrasound, know the normal anatomy of the region of interest, and be skilled in needle placement. This is usually a radiologist who will often have other imaging available as part of the work-up to diagnose an impalpable lesion and will use this in their decision to site the wire during the localization procedure.
Alternatives to USGWL
Current alternatives to USGWL are techniques recently described in breast practice, for example radioguided occult lesion localization, which uses ultrasound guidance to inject a radioactive tracer into the lesion. A g probe, which detects the radioactivity, is used intraoperatively to identify the lesion for excision and postoperatively to check the specimen and wound site to ensure complete resection [13]. Radioactive seed localization has also been proposed [14]. A significant limitation to both of these techniques is the exposure of the patient and the staff to radioactivity and neither are currently applicable in the head and neck. In addition, depending on the tracer used, there may be physiological uptake in the thymus or salivary glands, which may pose difficulties for the surgeon if in close proximity to the pathological neck lesion requiring resection.
Alternative imaging modalities have been used for wire localizations outside of the breast. CT-guided wire localization has been described for a symptomatic muscular axillary arch [15], lung lesions [16] and also for impalpable cervical lymph nodes identified on PET-CT [17]. As with MR, static, single plane images are produced, however, the most significant limitation to this is the use of ionizing radiation, which is undesirable for radiosensitive organs in the head and neck. Hoang et al. [17] did not use intravenous contrast during CT-guided hookwire placement; however, it is feasible that intravenous contrast would be required in certain cases, which poses the risk of contrast-induced nephropathy, contrast allergy, and would require more time and expense to work-up the patient for the scan.
Conclusion
USGWL has a wide and increasing range of applications. Performed by practitioners skilled in ultrasound and ultrasound-guided techniques, it is a safe and successful method to precisely locate a variety of lesions. The technique helps to minimize tissue damage as surgery is targeted, reducing operative time and improved confidence regarding lesion resection.
Future perspective
Pre-operative wire localization is currently performed more than intra-operative wire localization. In the future there may be increased use of ultrasound in theater for a variety of specialties, depending on local availability of expertise. This may involve ultrasound imaging without wire localization depending on the region of interest, for example Woydt et al. used intra-operative ultrasound alone to locate and resect deep-seated intracerebral cavernous hemangiomas [18]. Head and neck oncology is a challenging subspecialty and USGWL presents an accurate and safe technique facilitating successful surgical outcomes, and is likely to be adopted more widely in this specialty in the future.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
Papers of special note have been highlighted as:
* of interest
* of considerable interest
- Rissanen TJ, Makarainen HP, Kiviniemi HO, Suramo IIJ. Ultrasonographically guided wire localisation of non palpable breast lesions. J. Ultrasound Med. 1, 183–188 (1994).
- Fletcher AM, Preston TW, Kuehn DM, Clark ED, Van Daele D, Hoffman H. Ultrasound-guided needle localization of recurrent paratracheal thyroid cancer. Ann. Otol. Rhinol. Laryngol. 118(7), 475–478 (2009).
- Thomas RH, Burke C, Howlett D. A technical note: pre-operative ultrasoundguided wire localization in head and neck surgery. Eur. Arch. Otorhinolaryngol. 268, 743–746 (2011). & Summary of two case reports in which ultrasound-guided wire localization (USGWL) was used pre-operatively to localize impalpable, benign ectopic thyroid tissue in a patient at risk of micropapillary thyroid cancer, and an impalpable metastatic neck lymph node.
- Woodhouse NR, Williams MD, Saha S, Howlett DC. Ultrasound guided wire localisation to aid surgical biopsy of impalpable parotid oncocytoma. Int. J. Oral Maxillofac. Surg. 40, 427–429 (2011). & Case report describing the technique of USGWL and its role in the management of a complex parotid lesion.
- Shinohara S, Yamomoto E, Tanabe M, Maetani T, Kim T. Implantation metastasis of head and neck cancer after fine needle aspiration biopsy. Auris Nasus Larynx. 28, 377–380 (2001).
- Slywotzky C, Maya M. Needle tract seeding of transitional cell carcinoma following fine-needle aspiration of a renal mass. Abdom. Imaging 19, 174–176 (1994).
- Hiraki T, Mimura H, Gobara H et al. Two cases of needle-tract seeding after percutaneous radiofrequency ablation for lung cancer. J. Vasc. Interv. Radiol. 20, 415–418 (2009).
- Browne RFJ, Jeffers M, McDermott T et al. Technical report. Intra-operative ultrasoundguided needle localization for impalpable testicular lesions. Clin. Rad. 58(7), 566–569 (2003).
- Duprez R, Lebas, P, Marc OS, Mongois E, Emy P, Michenet P. Preoperative US-guided hook-needle insertion in recurrent lymph nodes of papillary thyroid cancer: a help for the surgeon. Eur. J. Radiol. 73, 40–42 (2010). & This study of eight patients describes the reliability of USGWL in asymptomatic and impalpable thyroid cancer recurrence detected on follow-up ultrasound or biochemistry.
- Bryant JA, Siddiqi NJ, Loveday EJ, Irvine GH. Presurgical ultrasound guided anchor-wire marking of impalpable cervical lymph nodes. J. Laryngol. Otol. 119, 627–628 (2005).
- Zimmerman P, DaSilva M, Izquierdo R, Cico L, Kort K, Numann P. Intraoperative needle localisation during neck reexploration. Am. J. Surg. 188, 92–93 (2004).
- Breeze J, Willliams MD, Howlett DC. Ultrasound guided localisation during the excision of an impalpable branchial cyst. Br. J. Oral. Maxillofac. Surg. 46, 686–687 (2008). & On clinical examination postaspiration the branchial cyst became impalpable and therefore USGWL was used to locate the lesion for surgical excision where it was found encased in fibrous tissue.
- Van der Ploeg IMC, Hobbelink M, van der Bosch MAAJ, Mali WPTM, Borel Rinkes IHM, van Hillegersberg R. Radioguided occult lesion localisation (ROLL) for non palpable breast lesions: a review of the literature. Eur. J. Surg. Oncol. 34(1), 1–5 (2008).
- Gray RJ, Pockaj BA, Karstaedt PJ, Roarke MC. Radioactive seed localization of nonpalpable breast lesions is better than wire localization. Am. J. Surg. 188, 377–380 (2004).
- Sellon JL, Murthy NS, Schmit GD, Spinner RJ. Wire-guided resection of a muscular axillary arch causing neurovascular compression. J. Surg. Orthop. Adv. 19(4), 229–233 (2010).
- Chen YR, Yeow KM, Lee JY et al. CT-guided hook wire localization of subpleural lung lesions for video-assisted thorascopic surgery (VATS). J. Formos. Med. Assoc. 106(11), 911–918 (2007).
- Hoang JK, De Jesus R, Eastwood JD, Gafron, Witsell DL. CT-guided hookwire placement: a technical innovation for preoperative localization of nonpalpable cervical lymph nodes. Am J. Neuroradiol. doi:10.3174/ajnr (2011) (Epub ahead of print).
- Woydt M, Krone A, Soerensen N, Roosen K. Ultrasound-guided neuronavigation of deep-seated cavernous haemangiomas: clinical results and navigation techniques. Br. J. Neurosurg. 15(6), 485-495 (2001).