Review Article - Imaging in Medicine (2013) Volume 5, Issue 5
Advancing our understanding of the brain in autism: contribution of functional MRI and diffusion tensor imaging
Lauren E Libero1 and Rajesh K Kana*1Department of Psychology, University of Alabama at Birmingham, CIRC 235G, 1719 6th Avenue South, Birmingham, AL 35294-0021, USA
- *Corresponding Author:
- Tel.: +1 205 934 3171
Fax: +1 205 975 6330
Email: rkana@uab.edu
Abstract
Keywords
autism; diffusion tensor imaging; effective connectivity; functional connectivity; functional MRI; white matter
“We must, then, assume that these children have come into the world with innate inability to form the usual, biologically provided affective contact with people, just as other children come into the world with innate physical or intellectual handicaps. If this assumption is correct, a further study of our children may help to furnish concrete criteria regarding the still diffuse notions about the constitutional components of emotional reactivity. For here we seem to have pure-culture examples of inborn, autistic disturbances of affective contact.”
– Leo Kanner (1943)
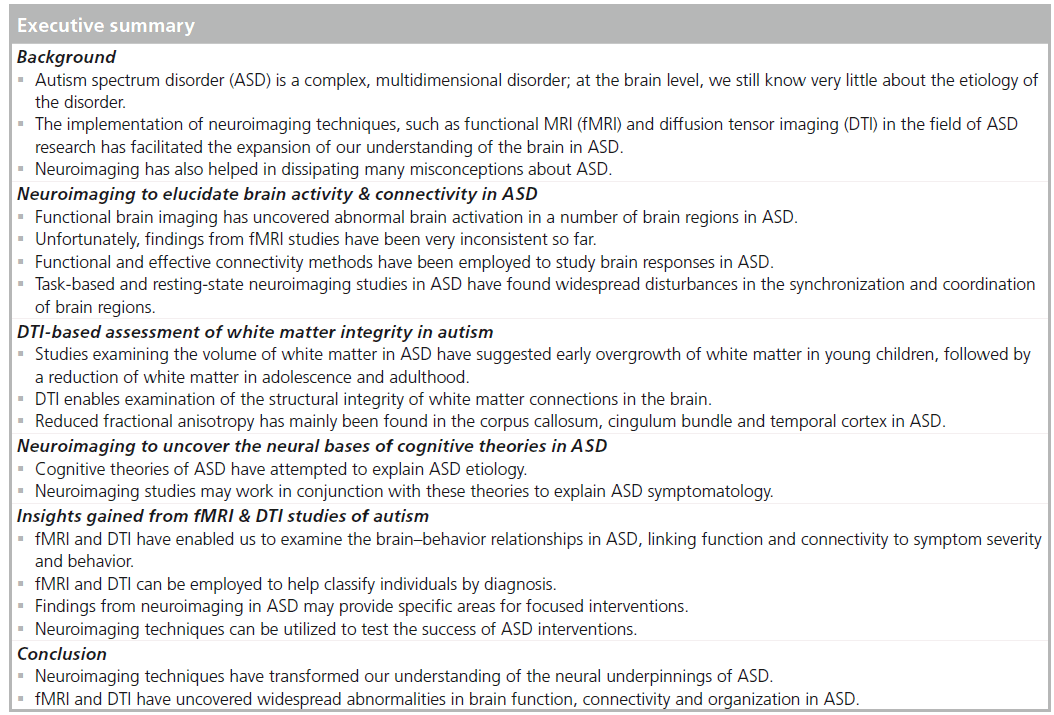
In the first historical reference to autism spectrum disorder (ASD), Kanner emphasized the potential biological association of the disorder, describing how some inborn abnormalities must be driving the behavioral impairments seen in the affected children studied [1]. Since 1943, the quest for understanding the biological basis of ASD has been the focus of autism research. Although such neurobiological pursuits have not resulted in establishing a firm etiology of the disorder, significant strides have been made in these areas have been made. Neuroscience and genetics research have certainly illuminated our understanding of the biological underpinnings of ASD and the nature of brain functioning in ASD. Although electrophysiological, cellular and animal models have significantly contributed to a better conceptualization of ASD, the advent of modern neuroimaging techniques have revolutionalized neuroscience research in autism. Specifically, the development and implementation of functional MRI (fMRI) and diffusion tensor imaging (DTI) techniques have facilitated an explosion of research and discovery in the field. Within the last few decades, fMRI and DTI have provided scientists with sophisticated neuroimaging tools to study the live human brain in vivo, thus paving the way for neurobiologically informed characterization of the biological basis of ASD.
Despite Kanner’s early suggestion of a biological cause for ASD, decades of research have not provided a single and widely accepted etiology of ASD. This may perhaps reflect the inherent difficulty in explaining a complex multidimensional disorder such as ASD, which is essentially a constellation of a wide range of impairments in social, communicative and behavioral domains. Shortly after Kanner’s original paper, psychoanalytic theories emerged, rejecting the possibility of a biological role in the etiology of ASD. Indeed, it should be noted that Kanner himself came to dismiss a biological link for the disorder, favoring an etiology for ASD founded in familial relationships and behavioral upbringing [2]. This view was then popularized by the publication of Bettelheim’s famous book The Empty Fortress. Bettelheim’s controversial view focused on ‘refrigerator’ mothers who are cold, distant and do not provide their babies with adequate stimulation and affection, causing their children to withdraw into an autistic state [3]. At a time when Freudian psychology ruled, such a proposition emphasizing the mother–child bond seemed, to many, to be a logical progression of thought, on how one could become autistic. By contrast to popular psychological theories blaming inefficient parenting as the cause of ASD, Rimland published his neurobiological theory of ASD in 1964 [4]. Rimland argued that there was no evidence proving the refrigerator mother theory, thus the etiology of ASD must have a different source. He believed physiological factors, specifically physical abnormalities in the brain (possibly the reticular formation) were responsible for the symptoms of ASD. This was the first significant step in eroding the negative effects of Bettelheim’s claims and moving towards a more biological-based understanding of the disorder. In 1978, Damasio and Maurer published a neurobiological account of ASD, after finding similarities between the behaviors of individuals with ASD and the behavior of adults with frontal cortex damage [5]. They suggested that dysfunction in the mesolimbic cortex, frontal and temporal lobes, neostriatum, and thalamus, may underlie the ASD symptomatology. This marked a movement towards establishing a brain–behavior relationship in ASD. Early studies of the brain in autism focused on auditory nerve and brain stem evoked responses [6,7], rapid eye movement activity during rapid eye movement sleep [8] and brainwaves measured by EEG [9] with limited results. Based on visual observations of affected children’s physical features, the field also focused on measuring brain volume and cell counts, via head circumference measurements [10–13] and post-mortem investigations [14–19]. While the results of these studies were inconsistent, they highlighted widespread abnormalities in the brain in ASD, emphasizing the need for further neurobiological investigations.
In the last two decades, neuroimaging research has played an important role in eliminating speculative psychoanalytic accounts of autism and in clearing up misconceptions about the disorder. While previous methods were limited to indirect or surface measures (event-related potentials, EEG and head circumference) of the brain, or post-mortem samples (necropsy), neuroimaging has supplied a vital avenue for studying the brain in great detail in ASD while at work and in vivo. fMRI and DTI methods allow researchers to examine not only the organization and connectivity of the brain but also how the brain responds in real time to stimuli. Since the brain can be investigated in live humans, information gathered about the brain can also be associated with more precise and current behavioral information (rather than resorting to secondary resources such as patient records or interviews of surviving relatives). In addition, patients can be studied longitudinally (allowing for developmental studies of the brain in ASD), a vital dimension in the context of neurodevelopmental disorders such as ASD. fMRI and DTI are also sophisticated and more versatile in terms of what they enable researchers to examine. Data from these modalities can include task-based brain activity, blood flow, examining the brain at rest, measuring different types of connectivity, and establishing links between biology and behavior. Neuroimaging studies provide evidence for widespread functional and structural abnormalities in the brain, seen early on in babies and toddlers with ASD [20]. Such evidence has helped to establish ASD as a disorder of neurodevelopmental origin. Neuroimaging studies have uncovered widespread abnormalities in the autistic brain at focal as well as at global levels, leading to a systems-level characterization of the disorder [20]. This paper will explore the contribution of neuroimaging, especially fMRI and DTI methods, in advancing our understanding of the neural mechanisms underlying autism. Furthermore, we will examine the impact of a comprehensive characterization of autism in uncovering the causes of behavioral impairments, in identifying and classifying individuals with and without autism, and in developing better treatments for affected individuals.
Neuroimaging to elucidate brain functioning in ASD
The number of published fMRI studies in the field of autism has increased dramatically in the last decade, with published biology-based studies in ASD representing a fourfold increase from 2000 to 2010 [21]. These studies have examined several domains of thinking, such as social, cognitive and visuospatial processing, in children and adults with ASD completing tasks including face processing, theory-of-mind, language comprehension, embedded figures tasks, response-inhibition tasks, reward processing, biological motion and working memory. Findings from these studies point to several foci in the brain that respond differently in individuals with autism compared with typically developing control participants [20,22–24]. In particular, studies have found decreased activation in the medial and dorsolateral prefrontal cortex and anterior cingulate cortex [25–31], amygdala [32–35], fusiform gyrus [33,34,36–38], superior temporal sulcus (STS) [39], and the mirror neuron system [40,41].
Many of the aforementioned findings of deviant brain responses may underlie the triad of impairments that are the hallmark of ASD. However, inconsistency across studies has been a key issue affecting the impact of these findings. The relatively consistent findings include altered brain activity in the fusiform gyrus during face processing [36,37] and in the STS during biological motion perception [39,42], suggesting potential neural signatures of social cognitive impairments in ASD. In addition to decreased brain activity, significantly greater activity has been found mainly in relatively posterior visuospatial areas for tasks involving visual memory and spatial reasoning [30,43–45], perhaps suggesting intact or enhanced visual and detail-oriented abilities in individuals with ASD. Although these findings are vital in identifying specific nodes of the brain that function differently in autism, the widespread nature and large number of these regions make it rather difficult to account for autism. Nevertheless, they suggest a systems-wide problem in brain functioning in autism rather than a focal abnormality.
One of the primary gains from neuroimaging research has been uncovering how the brain in ASD functions and how this compares and contrasts with the typical developing brain. Using fMRI and DTI, we have been able to explore brain activation and the connections (functional, effective and structural) that are subserving brain functions. While fMRI-based brain activity measures are helpful in gaining valuable information about the brain functioning in ASD, they are also constrained by several factors. For instance, as most fMRI studies are task-based, presenting certain types of stimuli and asking participants to respond to questions, the information obtained about regions that are over- or under-activated is heavily dependent on the nature and quality of a given task. Recently, task-free resting-state fMRI studies have investigated baseline or default brain activity differences in individuals with ASD as they rested in the MRI scanner. These studies have found altered patterns of activity in individuals with ASD in regions (medial prefrontal cortex, rostral anterior cingulate cortex, posterior cingulate cortex [PCC] and precuneus) that are pa rt of the default mode network [46,47]. Task-based and resting-state fMRI studies suggest altered recruitment of cortical areas in accomplishing a cognitive task and impairments in modulating brain areas in response to cognitive demands in individuals with ASD. Despite these widespread brain activity differences seen in ASD, questions remain as to the extent to which these focal abnormalities can explain autism. Additional ways to glean more information about the brain in autism are discussed next.
fMRI-based assessment of brain connectivity in ASD
In addition to the focal brain activity maps obtained from fMRI, during the past several years studies have started to examine the coordinated functioning (brain connectivity), or the failure to do so, of different brain areas in ASD. If ASD is indeed a systems-level disorder of disruptions in the brain, it may be the interaction of many areas and/or their anatomical connections to one another that are dysfunctional rather than the specific brain regions by themselves. Furthermore, examining connectivity explains the synchrony of the brain (functional connectivity), the influence of regions on each other (effective connectivity) and the underlying anatomical connections (anatomical or white matter connectivity) that support the cognitive functions of the brain.
Functional connectivity examines interregional temporal correlations of brain activation (as measured by fMRI) in remote brain regions [48]. This technique allows both the communication between brain regions and how different regions may work together as a team to serve specific functions to be investigated. In ASD, functional connectivity fMRI studies have uncovered widespread disturbances in the synchronization of many brain regions [25,28,43,49–54]. Even at rest, individuals with ASD fail to adequately organize their brain activity, as studies have uncovered alterations in anterior–posterior connections during rest [55]. These findings have led to and supported the possibility of disrupted cortical connectivity as an explanatory model for the spectrum of behaviors and impairments in ASD, stating that communication between distant brain areas is compromised in ASD leading to disruption of complex cognitive functioning (and thus may underlie the complex triad of impairments characterizing ASD) [56]. Greater or intact connectivity has also been reported in autism across proximal or local regions, especially in the relatively posterior brain areas [50]. These findings point to the possibility that some connections may be disrupted (causing impairment in social and emotional functioning), whereas other connections may be spared (allowing certain strengths and abilities to remain).
While the insights gained from functional connectivity studies of autism are valuable, functional connectivity is a method for assessing observed correlations, and does not provide insight into the time-lagged causality and directionality of such correlations. Effective connectivity, on the other hand, provides information about the influence that one system exerts over another with respect to a given experimental context [57]. Unlike functional connectivity, which examines correlations of brain regions working in synchrony, effective connectivity examines which brain regions can predict the activation of other regions. In other words, effective connectivity analyzes the flow of information within the brain, investigating which brain regions have causal influence over others. Only a handful of studies have utilized effective connectivity in autism and have found abnormal patterns (reduced or absent effective connectivity between the amygdala and the dorsal medial prefrontal cortex, dorsal medial prefrontal cortex to dorsolateral prefrontal cortex, the dorsolateral prefrontal cortex to the ventral prefrontal cortex and the ventrolateral prefrontal cortex to the STS and increased influence of the prefrontal cortex on the fusiform gyrus) during explicit emotion processing [58], as well as during imitation [59]. Finally, a study by Bird et al. found abnormalities in the influential relationships between face-selective areas (extrastriate cortex) and the V1 [60]. These studies indicate that perhaps the flow of information within the brain is also disrupted in ASD, with some brain regions failing to influence the next area down the line. A disruption in information flow could have drastic effects on how the brain is able to process and respond to incoming information. In summary, functional and effective connectivity may provide complementary aspects of brain functioning and may prove to be critical in gaining valuable information about neural information processing in ASD.
DTI-based assessment of white matter integrity in autism
It is important to note that the functional and effective connectivity impairments in ASD may be the result of underlying anatomical abnormalities. Therefore, establishing structure–function relations is critical in developing a comprehensive picture of the brain organization in ASD. Functional connectivity between distant brain areas in the normal developing population has been found to correlate with white matter integrity in pathways connecting these brain areas [61,62]. Studies regarding the volume of white matter have suggested an early overgrowth of white matter among young children with autism, followed by reduced white matter in adolescence and adulthood relative to controls [13,63–66]. Such volumetric abnormalities may have resulted from aberrations in axonal density or organization, or from myelin abnormalities, either of which could result in aberrant connectivity. DTI provides the opportunity to go beyond the measurement of white matter volume to examine its structural integrity on a voxel-by-voxel basis. Fractional anisotropy (FA), a measure derived from diffusion tensor data, is sensitive to developmental changes and pathological differences in axonal density, size, myelination and the coherence of organization of fibers within a voxel, and thus provides an index of the structural integrity of white matter [67–69]. DTI studies in ASD have found reduced FA and increased mean diffusivity in a number of white matter tracts including the corpus callosum, cingulum and tracts in the temporal lobes [70–75]. These findings underscore the abnormality of brain organization and connection strength in ASD and potentially provide physical evidence for the disruptions in functional connections seen in fMRI studies of ASD [56].
So far, studies of brain connectivity have revealed ASD to be a disorder of altered cortical connectivity. These alterations have helped to explain many symptoms of autism at a global level; in particular, the weaker frontal–posterior connectivity may explain the limited coherence seen in information processing in autism, and the intact or greater connectivity in occipital and parietal areas may explain autism patients’ increased reliance on the visuospatial route for information processing. The functional, causal and anatomical connectivity information may also be useful in identifying specific pathways or tracts to target for intervention in ASD. Improving brain connectivity could improve cognition and ASD behavior, as shown in previous studies in other clinical populations, such as dyslexia [76–78]. In addition, information about connectivity will tell us more about the overall organization of the ASD brain. This may point to other mechanisms (e.g., abnormal cellular organization, cell migration or synaptogenesis) that are causing the problems in connectivity, and thus lead us to a better understanding of the etiology of ASD symptoms.
Neuroimaging to uncover the neural basis of cognitive theories of ASD
In an attempt to explain the behavioral symptoms of ASD, numerous cognitive theories have been proposed, including the weak central coherence, mindblindness, enhanced perceptual functioning, complex information-processing difficulty and executive dysfunction accounts of ASD. The weak central coherence theory posits that the systems usually responsible for combining information to establish overall meaning (coherence) are weakened in ASD, resulting in a cognitive bias towards processing local details as opposed to the global whole [79–81]. The Mindblindness theory is based on the theory-of-mind (attribution of mental states to others) difficulties faced by individuals with ASD, suggesting that the social behavioral impairments seen in ASD that arise from a failure of the systems are required for processing their own mental states and those of others [82]. The enhanced perceptual functioning account suggests that perceptual and visuospatial functions are enhanced in individuals with autism [83,84]. The complex information-processing account posits that the pattern of deficits within and across domains in autism is a reflection of complex informationprocessing demands [85]. Finally, the executive dysfunction theory suggests that weak executive functioning skills lead to the impairments presented by those with ASD [86,87].
While these theories may provide convincing cases for the etiology of the variety of behavioral symptoms seen in ASD, they have not been fully supported by neuroimaging research in ASD. Nevertheless, there are several fMRI and DTI findings that uncover the underlying neural mechanisms that mediate the cognitive and behavioral symptoms explained by these theories. For instance, altered recruitment of the STS in gaze processing and biological motion [39], reduced activity in the medial prefrontal cortex [25,28], weaker connectivity between the prefrontal cortex and posterior areas in tasks of theory-of-mind [28,52], lack of or reduced response in the fusiform face area during face processing [34,36,37] and weaker structural connectivity between the fusiform and amygdala may underlie the social impairments seen in individuals with autism [88]. Therefore, in some ways, fMRI studies have served to support the cognitive theories, finding local processing biases [30,43–45], theory-of-mind deficits [28,32,39,89,90], and executive function impairments [91,92] in the brains of ASD participants. At the same time, other studies have characterized the neural systems underlying global and local processing, theory-of-mind and executive functions [28,93,94]. Thus, cognitive theories of autism in conjunction with corresponding neural-level accounts may be stronger in explaining autism symptomatology rather than either of these in isolation.
Insights gained from fMRI & DTI studies of autism
Establishing brain–behavior relationships
In order to better understand a neurodevelopmental disorder such as ASD, it is extremely important that brain research findings are related to behavioral and cognitive functions. Moreover, it is equally important to apply such information to more translational and practical levels so that it plays a role in improving the symptoms of the individual with ASD. By investigating the relationship between biology and behavior, one can better understand the origins of ASD symptoms and the varying levels of severity. Several neuroimaging studies have correlated brain measures with behavioral or diagnostic measures to illustrate the relationship between the make-up of the brain and ASD symptom severity. For instance, higher activity in the inferior frontal cortex (pars opercularis), insula and limbic structures during an imitation task was found to be related to better social functioning (measured by the social domain of the Autism Diagnostic Observation Schedule [ADOS] [95] and Autism Diagnostic Interview-Revised [ADI-R] [96]) [40]. In another study, higher repetitive behavior scores (on the ADI-R) were associated with greater right anterior cingulate cortex activity in a responsemonitoring task [97]. Greater activity in the right medial and inferior frontal gyrus and STS or middle temporal gyrus was significantly correlated with increased receptive language age and increased activity in these regions was also linked to decreased symptom severity (Childhood Autism Rating Scale [98]) [99]. In the same study, left frontal and temporal regions were negatively correlated with ASD symptom severity. In a study on gaze processing, increased left medial temporal lobe and right superior temporal cortex activity during attention to averted gaze and bilateral visual cortex and left superior parietal sulcus activity during gaze processing were associated with more ASD symptoms (on the Childhood Autism Spectrum Test [100]) [101]. Finally, increased activation in the STS for biological motion was found to be related to lower symptom severity as measured by the Social Responsiveness Scale [42,102]. The findings from these studies provide not only the foci of brain activity that are different in autism, but also how they are mediated by autism symptom severity.
In addition to brain activity, connectivity indices have also been related to autism symptomatology. In a study by Weng and colleagues, there was a correlation between weaker connectivity of the PCC and parahippocampal gyrus, temporal lobe and superior frontal gyrus, and worse reciprocal social interaction (via ADI-R) in participants with autism [103]. In addition, more severe repetitive behavior was linked to weaker connectivity between the PCC and medial prefrontal cortex, temporal lobes and superior frontal gyri. Poor communication (verbal and nonverbal) was found to be associated with overconnectivity between the PCC and temporal lobes and parahippocampal gyrus, and poorer nonverbal communication was associated with overconnectivity between the PCC and superior frontal gyri [88]. Another study found a negative association between reciprocal social interaction (ADI-R) and connectivity between the PCC and right superior frontal gyrus, with weaker connectivity predicting poorer social-interaction skills [104]. In the same study, the severity of restricted and repetitive behaviors was positively associated with connectivity between the PCC and right parahippocampal gyrus (with more severe repetitive behaviors linked to stronger connectivity). A study investigating interhemispheric connectivity during auditory stimulation found that higher connectivity in the inferior frontal gyrus was linked to better expressive language skills (Mullen Scales of Early Learning [105]) and lower inferior frontal gyrus connectivity predicted greater social and communicative symptom severity (ADOS) [106]. In a study on face processing, connectivity between the right fusiform face area and left amygdala correlated with social impairment scores (ADI-R), with reduced connectivity linked to more severe social impairment. In addition, increased connectivity between the right fusiform face area and right inferior frontal gyrus was correlated with increased social severity on the ADOS [107]. Overall, altered functional connectivity patterns may also influence behavioral impairments seen in individuals with autism.
DTI findings have also pointed to a few links between the structural integrity of white matter tracts and symptom severity and functioning in ASD. Decreased FA in the frontal cortex has been linked to increased ASD symptom severity [108] and decreased FA in the cerebellum was linked to increased repetitive behaviors [109]. Lower FA in the subgenual right anterior cingulate cortex has been linked to higher restricted and repetitive behavior scores on the ADI-R [97]. In addition, performance IQ has been linked to FA and radial diffusivity in the corpus callosum [73,74] and radial diffusivity in the temporal stem [110].
Decreased FA in the fornix, superior longitudinal fasciculus, corpus callosum and uncinate fasciculus were linked to increased symptom severity (ADI-R and ADOS) [111]. While there have been fewer DTI studies correlating diffusion data with ASD behavior, these findings also support the idea of the anatomical organization of the brain driving ASD symptom severity and potentially support the link between activation and functional connectivity with ASD behavior.
Overall, the study of the brain–behavior relationship using neuroimaging in ASD has resulted in numerous links being identified between brain activation and connectivity with symptom severity and social functioning, which holds great potential for future therapy development. These results represent the beginning of an investigation into valuable knowledge that can be used to translate what we learn from brain imaging directly to better conceptualization of behavioral impairments and to treating symptoms of the disorder.
Examining neurodevelopment in autism
A neurodevelopmental disorder such as ASD may result from changes in brain development, potentially involving alterations in neurogenesis, cell migration and neuronal connectivity. Therefore, in autism, it is extremely important for neuroscience and neuroimaging research to take into account the neurodevelopmental trajectory. This is especially relevant to studies of brain connectivity in ASD. However, to date, most neurodevelopmental studies in ASD have primarily focused on gray and white matter volume [13,63–66]. While these studies have consistently found an early increase in overall brain volume and white matter volume, followed by a decrease in adolescence and adulthood, they did not address the developmental issues related to the brain in ASD. Among the few neuroimaging studies, a DTI study found age-related decrease in FA in the right paracentral lobule and bilateral superior frontal gyrus in adolescence in ASD, with older adolescents showing a greater decrease in FA [112]. Another DTI study uncovered an interaction between age and diagnosis for the posterior limb of the right internal capsule, with the ASD group showing an increase in FA as age increased [72]. With only two studies specifically studying age effects in white matter integrity, it may be too early to draw firm conclusions regarding the development of white matter tracts in ASD.
Similarly with fMRI, there is a paucity of studies looking specifically at age effects in ASD. Nevertheless, a recent meta-analysis specifically comparing fMRI studies of children and adults showed greater hyper- and hypo-activation in children with ASD compared with adults with ASD [113]. In particular, the study found greater reductions in activation in the parahippocampal gyrus, hippocampus and superior temporal gyrus in children with ASD compared with adults with ASD for social tasks, and increased hyperactivation in the right insula, right middle frontal gyrus and left cingulate for nonsocial tasks [113]. Thus, there are greater activation differences in children with ASD compared with their normal developing peers, and, with age, these differences seem to abate [113].
Although a few neuroimaging studies have addressed brain activation and connectivity in children and adults with ASD, it should be noted that these studies have largely examined only one cohort at a time (including only children or adults). Furthermore, the vast majority of studies involving both children and adults did not include any specific analysis of age effects. In addition, studies have almost entirely focused on adolescents and adults, leaving younger children as an under-represented cohort in the field of ASD neuroimaging. Studies examining ASD from a developmental perspective, either utilizing age as a regressor or collecting longitudinal data, are still scarce. As a result, knowledge is limited regarding the developmental trajectory of brain function and connectivity in ASD. Future studies will hopefully address this situation by including a wider range of age groups within neuroimaging studies and acquiring longitudinal data to examine changes in the brain over time.
Neuroimaging to assist diagnostic classification of individuals with ASD
One of the main limitations when it comes to diagnosing ASD is that current diagnostic methods are based on observing specific behaviors during a short period of time in a clinical evaluation. This is coupled with the fact that the presentation of ASD varies greatly from child to child, making diagnoses that are much more challenging. Owing to these limitations, the median earliest age of ASD diagnosis is 4.5 years [114], while most children receive a diagnosis much later. As it is very difficult to identify ASD children earlier by observing behaviors, a neural marker can make a significant difference in early diagnosis and hence early intervention for affected children. A neural marker (founded in fMRI or DTI) for the disorder could be applied to babies or toddlers who are too young for current ASD behavioral tests. This has strong implications for early intervention and increasing the success of ASD treatment, as earlier intervention has proven to be most effective [115,116].
Several recent fMRI studies have used machine learning techniques to accurately classify participants into autism and control groups using brain activity or brain connectivity indices. Machine learning classification is a computational method that utilizes participant data (such as fMRI time series or FA values) to predict membership of a diagnostic group. Neuroimaging data and diagnostic information submitted to a computer program are used to enable the program to predict group membership based on characteristic features of the data. In other words, a classifier uses the values of different features in a sample data and predicts the class to which that sample belongs (e.g., ASD or normal developing group). One study of toddlers with ASD undergoing auditory stimulation found that interhemisphereic synchronization in inferior frontal gyrus and superior temporal gyrus could significantly predict classification, with 21 out of 29 toddlers correctly identified (72% sensitivity and 84% specificity) [106]. In another study, pairwise functional connectivity (among a lattice of 7266 regions on interest) during the resting state showed 83% sensitivity, 75% specificity and 79% accuracy total, with classification best serving younger subjects (89% accuracy for participants under 20 years of age) [117]. Yet another study examining connectivity during the resting state in ASD, measured by extracting fixation blocks from task-based fMRI studies, found 77.78% accuracy, 76.9% sensitivity and 78.6% specificity in identifying ASD participants [47]. Three studies examined classification of subjects via DTI. One study had 75.34% average accuracy with specificity and 71.88% sensitivity using anisotropic maps and tracts drawn in the splenium [118]. Another study found 78% accuracy, 77% specificity and 78% sensitivity for classification of ASD subjects using white matter regions of interest [119]. The third study used six diffusion coefficients from the superior temporal gyrus and temporal stem to classify participants and found 91.6% accuracy, 93.6% sensitivity and 89.6% specificity [110]. While there are only a handful of classification studies with fMRI and DTI currently published in autism, the results have so far been promising when it comes to accurately classifying groups. It should be noted that one has to be careful not to overinterpret these results, as diagnosing a disorder using these methods needs a more comprehensive understanding of the biology [120]. Nevertheless, this line of research will no doubt become very useful as it is fine tuned and applied to younger participants.
Impact of fMRI & DTI on the development & implementation of treatments
While neural characterization of ASD, relating the brain with behavior and using neural measures for classifying participants are all vital, perhaps the most important and effective aspect is to design novel treatments and interventions based on neurobiological insights. Neuroimaging has had a distinct impact on ASD treatment. Studies investigating treatment effects are especially meaningful for those affected by ASD. Pre–post design studies offer a glimpse at whether the ASD brain is pliable and whether faulty connections could be mended to improve functioning. A recent case study investigated the effects of citalopram (selective serotonin reuptake inhibitor medication) in two individuals with ASD. The treatment was found to be effective in reducing restricted and repetitive behaviors in one subject, but not in the other. For the subject who did display a reduction in restricted and repetitive behaviors, an increase in prefrontal activity was measured during an oddball task [121]. Another study investigated the effects of pivotal response treatment in two children with ASD [122]. The study found that both children had increased activation in social brain areas while viewing biological motion after pivotal response treatment, with one child increasing the response in the left dorsolateral prefrontal cortex and fusiform gyrus, and the other increasing activity in the posterior STS, left ventrolateral prefrontal cortex and right fusiform gyrus [123]. One study implemented a computer-based program to train five ASD participants in facial affect identification (with an additional five participants serving as a no-treatment control group), with the goal of ‘reanimating’ the fusiform gyrus. Although the treatment participants improved their behavioral accuracy and scores on the Frankfurt Test and Training of Facial Affect Recognition eye and face tests, they did not experience any changes in fusiform gyrus activation. However, the participants who completed the program demonstrated increased activation in the right superior parietal lobule for processing facial affect after completing the treatment [124]. Although only a few treatmenteffect studies (with a small number of subjects) have been published thus far, results point to the notion that the brain can be significantly altered (through development of more ‘normal’ activation or compensatory strategies) by various autism therapies.
What fMRI and DTI studies have uncovered can also be used as a guide for treatments, by informing about the specific brain areas that need to be targeted, or in identifying subtypes within ASD with specific differing needs. For example, a study by Alexander and colleagues found that a subgroup of their ASD participants had smaller corpus callosum volumes [73], increased medial and radial diffusivity, and decreased FA, along with low performance IQ and processing speeds. Conturo et al. found lower diffusivity for a tract between the hippocampus and fusiform gyrus for a subgroup of ASD participants who had a low performance on a test of face processing and low performance IQ scores [88]. These studies indicate that brain organization is related to cognitive performance. Perhaps fMRI and DTI can be utilized to identify subpopulations of ASD patients who have differing brain functions, and thus could be identified for tailored treatment that targets their specific needs and more efficiently treats their symptoms.
Among neuroimaging-based treatment of ASD, neurofeedback training is an important avenue in treatment-focused studies of autism. The neurofeedback technique uses live feedback from EEG electrodes to teach subjects to modulate (inhibit or enhance) their own brainwave frequencies. Participants are operantly conditioned or asked to play a computer game while EEG monitors their brainwaves and provides feedback as to whether more or less activity is required. fMRI has steered the field into recognizing abnormalities in brain activity and function. From these findings, we now have treatments targeting specific brain functions [125]. For example, neurofeedback training has been utilized to target abnormal μ-rhythms (indicative of dysfunction in the mirror neuron system [41,126]) in children with ASD [127,128]. fMRI itself can potentially be applied as a live training tool. One team used fMRI for neurofeedback training by employing visual feedback (based on activation) within the scanner to teach participants to adjust their performance on a task to modify their own brain activity [129]. This method could potentially be applied to individuals with ASD. With neurofeedback and other techniques, neuroimaging can be a significant contributor to interventions involving children and adults with ASD.
Conclusion
The advent of neuroimaging has transformed the fields of neuroscience and psychology, and has illuminated our understanding of neurodevelopmental disorders in general, and autism in particular. This paper examined the progress made by fMRI and DTI research in improving our understanding of the brain in autism and in applying that knowledge to design effective treatment plans. Studies of brain activity and connectivity have uncovered widespread abnormalities in ASD. These findings have drastically changed the way we conceptualize ASD as a disorder. A shift from emphasis on focal centers in the brain to a systems-level brain dysfunction has been a promising direction in characterizing ASD. Aberrant activity and connections dispersed across the brain together are impacting the complex processes that depend on concerted effort from many brain centers. In addition, studies linking brain activity and connectivity to ASD symptom severity further illustrate the complicated picture that is the brain in ASD. This is a compelling explanation for why ASD presents as a spectrum disorder with a wide range of symptoms and a wide variety of presentations of the disorder from one individual to the next. The coexistence of impaired and enhanced abilities in autism may underlie disrupted and enhanced connectivity across different nodes in the brain. While this adds to the complexity of the disorder, it also provides potential avenues for exploitation for treatment.
Early intervention and treatment has been found to be extremely effective in autism as it targets brain plasticity more effectively [130]. A key factor affecting this has been the difficulty in early diagnosis, as diagnosis is currently behavior based. fMRI and DTI have started to open the windows for identifying neural signatures that can distinguish a child with autism from a normal developing child as early in development as possible. Classification studies using sophisticated machine learning techniques have the potential to identify individuals with ASD at an early age with high rates of reliability. Identifying individuals earlier will allow for early intervention, potentially resulting in better outcomes overall. In addition, neuroimaging is starting to identify potential subgroups within the ASD population, which will be pivotal in the development of specialized, targeted treatments. In this manner, we can tailor therapy more specifically to improve abilities that are most needed by individuals. An important question in the mind of everyone affected by ASD is whether or not the autistic brain can be shaped and improved. Pre–post brain-based intervention studies and neurofeedback techniques are resulting in changes in brain organization and connectivity. Treatments such as neurofeedback purposely target disrupted brain areas in an attempt to modulate brain activity to what would be expected. By understanding which brain areas require intervention, we can better target our treatments to focus on the areas with the greatest need. Overall, fMRI and DTI have greatly advanced what we know about the brain in autism. Researchers have utilized the versatility of these techniques and have uncovered their potential in informing us about the different facets of the brain in ASD.
Future perspective
Future research in neuroimaging of autism will be more translational with the potential to answer key questions that have intrigued the scientific community. While disruption in brain connectivity in autism is relatively well accepted, its specificity to ASD needs to be established. Future neuroimaging research may follow this line of investigation, along with refining connectivity abnormalities with sophisticated methods and techniques for connectivity data analyses. The use of multimodal imaging to study the brain in ASD may prove to be critical in creating a comprehensive and global picture of the ASD brain. For example, future studies may begin to link brain-related indices with genetic and environmental studies. Understanding the genetic and epigenetic mechanisms that mediate brain development may prove to be critical in understanding the etiology and symptomatology of autism. We hope that future studies will also begin to incorporate currently under-represented areas within the field, such as focusing brain developmental trajectory and studies on younger children and toddlers with autism, especially longitudinal studies. In addition, little is known about the brain in girls and low-functioning individuals with autism, as the focus of neuroimaging has been on high-functioning individuals. Emphasis on these underexplored topics in the future may help to better understand the autism spectrum as a whole. Finally, the diagnostic utility of brain-level alterations in activation and connectivity needs to be established, along with creating neurobiologically informed intervention programs for individuals with autism. We believe that future research in neuroimaging and autism will undertake many, or all, of these priorities.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
Papers of special note have been highlighted as:
•of interest
•of considerable interest
- Kanner L. Autistic disturbances of affective contact. Nerv. Child 2, 217–250 (1943).
- Kanner L. Problems of nosology and psychodynamics in early childhood autism. Am. J. Orthopsychiatry 19(3), 416–426 (1949).
- Bettelheim B. The Empty Fortress: Infantile Autism and the Birth of the Self. The Free Press, NY, USA (1967).
- Rimland B. Infantile Autism: The Syndrome and Its Implications for a Neural Theory of Behavior. Appleton-Century-Crofts, NY, USA (1964).
- Damasio AR, Maurer MG. A neurological model for childhood autism. Arch. Neurol. 35, 777–786 (1978).
- Student M, Sohmer H. Evidence from auditory nerve and brainstem evoked responses for an organic lesion in children with autistic traits. J. Autism Child. Schizophr.8, 13–20 (1978).
- Tanguay PE, Edwards RM, Buchwald J, Schwofel J, Allen V. Auditory brainstem evoked responses in autistic children. Arch. Gen. Psychiatry 38, 174–180 (1982).
- Tanguay PE, Ornitz EM, Forsythe AB, Ritvo ER. Rapid eye movement (REM) activity in normal and autistic children during REM sleep. J. Autism Child. Schizophr. 6, 275–288 (1976).
- Small JG. EEG and neurophysiologic studies of early infantile autism. Biol. Psychiatry 10(4), 385–397 (1975).
- Davidovitch M, Patterson B, Gartside P. Head circumference measurements in children with autism. J. Child Neurol. 11, 389–393 (1996).
- Lainhart JE, Piven J, Wzorek M et al. Macrocephaly in children and adults with autism. J. Am. Acad. Child. Adolesc. Psychiatry 36, 282–290 (1997).
- Miles JH, Hadden LL, Takahashi TN, Hillman RE. Head circumference is an independent clinical finding associated with autism. Am. J. Med. Genet. 95, 339–350 (2000).
- Courchesne E, Carper R, Akshoomoff N. Evidence of brain overgrowth in the first year of life in autism. JAMA 290(3), 337–344 (2003).
- Bauman ML, Kemper TL. Histoanatomic observations of the brain in early infantile autism. Neurology 35, 866–874 (1985).
- Coleman PD, Romano J, Lapham L, Simon W. Cell counts in cerebral cortex in an autistic patient. J. Autism Dev. Disord. 15, 245–255 (1985).
- Aarkrog T. Organic factors in infantile psychoses and borderline psychoses: retrospective study of 45 cases subjected to pneumoencephalography. Danish Med. Bull. 15, 283–288 (1968).
- Williams RS, Hauser SL, Purpura DP, Delong GR, Swisher CW. Autism and mental retardation. Arch. Neurol. 37, 749–753 (1980).
- Bailey A, Luthert P, Dean A et al. A clinicopathological study of autism. Brain 121, 889–905 (1998).
- Kemper TL, Bauman M. Neuropathology of infantile autism. J. Neuropathol. Exp. Neurol. 57(7), 645–652 (1998).
- Williams DL, Minshew NJ. Understanding autism and related disorders: what has imaging taught us? Neuroimaging Clin. N. Am. 17(4), 495–509 (2007). n Presents a condensed overview of imaging in autism spectrum disorder (ASD).
- Office of Autism Research Coordination (OARC), National Institute of Mental Health and Thomson Reuters, Inc. on behalf of the Interagency Autism Coordinating Committee (IACC). IACC/OARC Autism Spectrum Disorder Research Publications Analysis Report: The Global Landscape of Autism Research (2012).
- Anagnostou E, Taylor M. Review of neuroimaging in autism spectrum disorders: what have we learned and where we go from here. Mol. Autism 2(1), 4 (2011). nn Provides a recent review of imaging in ASD.
- Minshew NJ, Keller TA. The nature of brain dysfunction in autism: functional brain imaging studies. Curr. Opin. Neurol. 23(2), 124–130 (2010). Provides a review of functional MRI studies in ASD.
- Dichter GS. Functional magnetic resonance imaging of autism spectrum disorders. Dialogues Clin. Neurosci. 14(3), 319–351 (2012).
- Castelli F, Frith C, Happe F, Frith U. Autism, Asperger syndrome and brain mechanisms for the attribution of mental states to animated shapes. Brain 125(Pt 8), 1839–1849 (2002).
- Wang AT, Lee SS, Sigman M, Dapretto M. Reading affect in the face and voice: neural correlates of interpreting communicative intent in children and adolescents with autism spectrum disorders. Arch. Gen. Psychiatry 64, 698–708 (2007).
- Kana RK, Keller TA, Minshew NJ, Just MA. Inhibitory control in high-functioning autism: decreased activation and underconnectivity in inhibition networks. Biol. Psychiatry 62(3), 198–206 (2007).
- Kana RK, Keller TA, Cherkassky VL, Minshew NJ, Just MA. Atypical frontal-posterior synchronization of theoryof- mind regions in autism during mental state attribution. Soc. Neurosci. 4, 135–152 (2009).
- Luna B, Minshew NJ, Garver KE et al. Neocortical system abnormalities in autism: an fMRI study of spatial working memory. Neurology 59, 834–840 (2002).
- Manjaly ZM, Bruning N, Neufang S et al. Neurophysiological correlates of relatively enhanced local visual search in autistic adolescents. Neuroimage 35, 283–291 (2007).
- Ring H, Baron-Cohen S, Williams S et al. Cerebral correlates of preserved cognitive skills in autism. A functional MRI study of embedded figures task performance. Brain 122, 1305–1315 (1999).
- Baron-Cohen S, Ring HA, Wheelwright S et al. Social intelligence in the normal and autistic brain: an fMRI study. Eur. J. Neurosci. 11, 1891–1898 (1999).
- Critchley HD, Daly EM, Bullmore ET et al. The functional neuroanatomy of social behaviour: changes in cerebral blood flow when people with autistic disorder process facial expressions. Brain 123, 2203–2212 (2000).
- Pierce K, Muller RA, Ambrose J, Allen G, Courchesne E. Face processing occurs outside the fusiform ‘face area’ in autism: evidence from functional MRI. Brain 124, 2059–2073 (2001).
- Ashwin C, Chapman E, Colle L, Baron-Cohen S. Impaired recognition of negative basic emotions in autism: a test of the amygdala theory. Soc. Neurosci. 1, 349–363 (2006).
- Schultz RT, Gauthier I, Klin A et al. Abnormal ventral temporal cortical activity during face discrimination among individuals with autism and Asperger syndrome. Arch. Gen. Psychiatry 57, 331–340 (2000).
- Deeley Q, Daly EM, Page L et al. An event related functional magnetic resonance imaging study of emotion processing in Asperger syndrome. Biol. Psychiatry 62(3), 207–217 (2007).
- Piggot J, Kwon H, Mobbs D et al. Emotion attribution in high-functioning individuals with autistic spectrum disorder: a functional imaging study. J. Am. Acad. Child Adolesc. Psychiatry 43, 473–480 (2004).
- Pelphrey KA, Morris JP, McCarthy G. Neural basis of eye gaze processing deficits in autism. Brain 128(Pt 5), 1038–1048 (2005).
- Dapretto M, Davies MS, Pfeifer JH et al. Understanding emotions in others: mirror neuron dysfunction in children with autism spectrum disorders. Nat. Neurosci. 9(1), 28–30 (2005).
- Williams JH, Whiten A, Suddendorf T, Perrett DI. Imitation, mirror neurons and autism. Neurosci. Biobehav. Rev. 25(4), 287–295 (2001).
- Kaiser MD, Hudac CM, Shultz S et al. Neural signatures of autism. Proc. Natl Acad. Sci. USA 107(49), 21223–21228 (2010).
- Koshino H, Kana RK, Keller TA, Cherkassky VL, Minshew NJ, Just MA. fMRI investigation of working memory for faces in autism: visual coding and underconnectivity with frontal areas. Cereb. Cortex 18, 289–300 (2008).
- Sahyoun CP, Belliveau JW, Soulieres I, Schwartz S, Mody M. Neuroimaging of the functional and structural networks underlying visuospatial versus linguistic reasoning in high-functioning autism. Neuropsychologia 48, 86–95 (2010).
- Damarla SR, Keller TA, Kana RK et al. Cortical underconnectivity coupled with preserved visuospatial cognition in autism: evidence from an fMRI study of an embedded figures task. Autism Res. 3, 273–279 (2010).
- Kennedy D, Redcay E, Courchesne E. Failing to deactivate: resting functional abnormalities in autism. Proc. Natl Acad. Sci. 103, 8275–8280 (2006).
- Murdaugh DL, Shinkareva SV, Deshpande HR, Wang J, Pennick MR, Kana RK. Differential deactivation during mentalizing and classification of autism based on default mode connectivity. PLoS ONE 7(11), e50064 (2012).
- Friston K, Tononi G, Reeke G, Sporns O, Endelman G. Value-dependent selection in the brain: simulation in a synthetic neural model. Neuroscience 59, 229–243 (1994).
- Just M, Cherkassky V, Keller T, Minshew N. Cortical activation and synchronization during sentence comprehension in high-functioning autism: evidence of underconnectivity. Brain 127, 1811–1821 (2004).
- Kana R, Keller T, Cherkassky V, Minshew N, Just M. Sentence comprehension in autism: thinking in pictures with decreased functional connectivity. Brain 129, 2484–2493 (2006).
- Mason RA, Williams DL, Kana RK, Minshew N, Just MA. Theory-of-mind disruption and recruitment of the right hemisphere during narrative comprehension in autism. Neuropsychologia 46, 269–280 (2008).
- Kana RK, Libero LE, Hu CP, Deshpande HD, Colburn JS. Functional brain networks and white matter underlying theory-of-mind in autism. Soc. Cogn. Affect. Neurosci. doi:10.1093/scan/nss106 (2012) (Epub ahead of print).
- Kana RK, Just MA. Autism as a disorder of functional brain connectivity. In: Handbook of Autism Spectrum Disorders. Amaral DG, Geschwind D, Dawson G (Eds.). Oxford University Press, New York, USA, 981–989 (2011). n Provides a specific overview of functional connectivity in ASD.
- Schipul S, Keller T, Just M. Inter-regional brain communication and its disturbance in autism. Front. Neurosci. 5, 1–11 (2011). n Reviews functional connectivity abnormalities in ASD.
- Cherkassky V, Kana R, Keller T, Just M. Functional connectivity in a baseline resting-state network in autism. Neuroreport 17, 1687–1690 (2006).
- Kana, RK, Libero LE, Moore MS. Disrupted cortical connectivity theory as an explanatory model for autism spectrum disorders. Phys. Life Rev. 8(4), 410–437 (2011). nn Provides a comprehensive overview of disrupted connectivity in ASD.
- Büchel C, Friston K. Assessing interactions among neuronal systems using functional neuroimaging. Neural Netw. 13(8–9), 871–882 (2000).
- Wicker B, Fonlupt P, Hubert B, Tardif C, Gepner B, Deruelle C. Abnormal cerebral effective connectivity during explicit emotional processing in adults with autism spectrum disorder. Soc. Cogn. Affect. Neurosci. 3, 135–143 (2008).
- Shih P, Shen M, Ottl B, Keehn B, Gaffrey M, Muller RA. Atypical network connectivity for imitation in autism spectrum disorder. Neuropsychologia 48(10), 2931–2939 (2010).
- Bird G, Catmur C, Silani G, Frith C, Frith U. Attention does not modulate neural responses to social stimuli in autism spectrum disorders. Neuroimage 31, 1614–1624 (2006).
- Cohen MX. Error-related medial frontal theta activity predicts cingulated related structural connectivity. Neuroimage 55, 1373–1383 (2011).
- Teipel SJ, Bokde ALW, Meindl T et al. White matter microstructure underlying default mode network connectivity in the human brain. Neuroimage 49, 2021–2032 (2010).
- Courchesne E, Karns CM, Davis HR et al. Unusual brain growth patterns in early life in patients with autistic disorder: an MRI study. Neurology 57, 245–254 (2001).
- Herbert MR, Ziegler DA, Makris N et al. Localization of white matter volume increase in autism and developmental language disorder. Ann. Neurol. 55, 530–540 (2004).
- Waiter GD, Williams JH, Murray AD, Gilchrist A, Perrett DI, Whiten A. Structural white matter deficits in high-functioning individuals with autistic spectrum disorder: a voxel-based investigation. Neuroimage 24(2), 455–461 (2005).
- Ecker C, Suckling J, Deoni SC et al. Brain anatomy and its relationship to behavior in adults with autism spectrum disorder: a multicenter magnetic resonance imaging study. Arch. Gen. Psychiatry 69(2), 195–209 (2012).
- Basser PJ. Inferring microstructural features and the physiological state of tissues from diffusion-weighted images. NMR Biomed. 8, 333–344 (1995).
- Pierpaoli C, Basser PJ. Toward a quantitative assessment of diffusion anisotropy. Magn. Reson. Med. 36, 893–906 (1996).
- Beaulieu C. The basis of anisotropic water diffusion in the nervous system – a technical review. NMR Biomed. 15, 435–455 (2002).
- Bloemen OJ, Deeley Q, Sundram F et al. White matter integrity in Asperger syndrome: a preliminary diffusion tensor magnetic resonance imaging study in adults. Autism Res. 3(5), 203–213 (2010).
- Barnea-Goraly N, Kwon H, Menon V et al. White matter structure in autism: preliminary evidence from diffusion tensor imaging. Biol. Psychiatry 55, 323–326 (2004).
- Keller TA, Kana RK, Just MA. A developmental study of the structural integrity of white matter in autism. Neuroreport 18, 23–27 (2007).
- Alexander AL, Lee JE, Lazar M et al. Diffusion tensor imaging of the corpus callosum in autism. Neuroimage 34, 61–73 (2007).
- Lee JE, Chung MK, Lazar M et al. A study of diffusion tensor imaging by tissue-specific, smoothing-compensated voxel-based analysis. Neuroimage 44(3), 870–883 (2009).
- Travers BG, Adluru N, Ennis C et al. Diffustion tensor imaging in autism spectrum disorder: a review. Autism Res. 5(5), 289–313 (2012). nn Provides a recent review of diffusion tensor imaging findings in ASD.
- Temple E, Deutsch GK, Poldrack RA et al. Neural deficits in children with dyslexia ameliorated by behavioral remediation: evidence from functional MRI. Proc. Natl Acad. Sci. USA 100(5), 2860–2865 (2003).
- Keller TA, Just MA. Altering cortical connectivity: remediation-induced changes in the white matter of poor readers. Neuron 64, 624–631 (2009).
- Krafnick AJ, Flowers DL, Napoliello EM, Eden GF. Gray matter volume changes following reading intervention in dyslexic children. Neuroimage 57, 733–741 (2011).
- Frith U. Autism: Explaining the Enigma. Blackwell, Oxford, UK (1989).
- Frith U, Happé F. Autism: beyond ‘theory-ofmind’. Cognition 50, 115–132 (1994).
- Happe F. Autism: cognitive deficit or cognitive style? Trends Cogn. Sci. 3(6), 216–222 (1999).
- Baron-Cohen S. Mindblindness: An Essay on Autism and Theory-of-Mind. MIT Press, Cambridge, MA, USA (1995).
- Mottron L, Burack JA, Iarocci G, Belleville S, Enns JT. Locally oriented perception with intact global processing among adolescents with high-functioning autism: evidence from multiple paradigms. J. Child Psychol. Psychiatry 44(6), 904–913 (2003).
- Mottron L, Dawson M, Soulieres I, Hubert B, Burack J. Enhanced perceptual functioning in autism: an update, and eight principles of autistic perception. J. Autism Dev. Disord. 36(1), 27–43 (2006).
- Minshew NJ, Goldstein G. Autism as a disorder of complex information processing. Ment. Retard. Dev. Disabil. Res. Rev. 4, 129–136 (1998).
- Hughes C, Russell J, Robbins T. Evidence for executive dysfunction in autism. Neuropsychologia 32, 477–492 (1994).
- Hughes C, Russell J. Autistic children’s difficulty with mental disengagement from an object: its implications for theories of autism. Dev. Psychol. 29, 498–510 (1993).
- Conturo TE, Williams DL, Smith CD, Gultepe E, Akbudak E, Minshew NJ. Neuronal fiber pathway abnormalities in autism: an initial MRI diffusion tensor tracking study of hippocampo-fusiform and amygdalo-fusiform pathways. J. Int. Neuropsychol. Soc. 14(06), 933–946 (2008).
- Lombardo M, Chakrabarti B, Bullmore E, Baron-Cohen S. Specialization of right temporo-parietal junction for mentalizing and its relation to social impairments in autism. Neuroimage 56, 1832–1838 (2011).
- Schulte-Rüther M. Dysfunctions in brain networks supporting empathy: an fMRI study in adults with autism spectrum disorders. Soc. Neurosci. 6(1), 1–21 (2011).
- Schmitz N, Rubia K, Daly E, Smith A, Williams S, Murphy DG. Neural correlates of executive function in autistic spectrum disorders. Biol. Psychiatry 59, 7–16 (2006).
- Shafritz KM, Dichter GS, Baranek GT, Belger A. The neural circuitry mediating shifts in behavioral response and cognitive set in autism. Biol. Psychiatry 63, 974–980 (2008).
- Just MA, Cherkassky VL, Keller TA, Kana RK, Minshew NJ. Functional and anatomical cortical underconnectivity in autism: evidence from an fMRI study of an executive function task and corpus callosum morphometry. Cereb. Cortex 17, 951–961 (2007).
- Hadjikhani N, Joseph RM, Snyder J et al. Activation of the fusiform gyrus when individuals with autism spectrum disorder view faces. Neuroimage 22, 1141–1150 (2004).
- Lord C, Risi S, Lambrecht L et al. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J. Autism Dev. Disord. 30(3), 205–223 (2000).
- Lord C, Rutter M, Le Couteur A. Autism diagnostic interview-revised: a revised version of a diagnostic interview for caregivers and individuals with possible pervasive developmental disorder. J. Autism Dev. Disord. 24(5), 659–685 (1994).
- Thakkar KN, Polli FE, Joseph RM et al. Abnormal response monitoring, repetitive behavior, and decreased microstructural integrity of white matter underlying anterior cingulate cortex in autism spectrum disorders. Brain 131, 2464–2478 (2008).
- Schopler R, Reichler J, DeVellis RF, Daly K. Toward objective classification of childhood autism: childhood autism rating scale (CARS). J. Autism Dev. Disord. 10(1), 91–103 (1980).
- Redcay E, Courchesne E. Deviant functional magnetic resonance imaging patterns of brain activity to speech in 2–3 year old children with an autism spectrum disorder. Biol. Psychiatry 64(7), 589–598 (2008).
- Scott F, Baron-Cohen S, Bolton P, Brayne C. The CAST (childhood Asperger syndrome test): preliminary development of a UK screen for mainstream primaryschool- age children. Autism 6(1), 9–31 (2002).
- Vaidya CJ, Foss-Feig J, Shook D, Kaplan L, Kenworthy L, Gaillard WD. Controlling attention to gaze and arrows in childhood: an fMRI study of typical development and autism spectrum disorders. Dev. Sci. 14(4), 911–924 (2011).
- Constantino JN, Davis SA, Todd RD et al. Validation of a brief quantitative measure of autistic traits: comparison of the social responsiveness scale with the autism diagnostic interview-revised. J. Autism Dev. Disord. 33(4), 427–433 (2003).
- Weng SJ, Wiggins JL, Peltier SJ et al. Alterations of resting state functional connectivity in the default network in adolescents with autism spectrum disorders. Brain Res. 1313, 202–214 (2010).
- Monk CS, Weng SJ, Wiggins JL et al. Neural circuitry of emotional face processing in autism spectrum disorders. J. Psychiatry Neurosci. 35, 105–114 (2010).
- Mullen EM. Mullen Scales of Early Learning (AGS Edition). Pearson, San Antonio, TX, USA (1995).
- Dinstein I, Pierce K, Eyler L et al. Disrupted neural synchronization in toddlers with autism. Neuron 70, 1218–1225 (2011).
- Kleinhans NM, Richards T, Sterling L et al. Abnormal functional connectivity in autism spectrum disorders during face processing. Brain 131, 1000–1012 (2008).
- Noriuchi M, Kikuchi Y, Yoshiura et al. Altered white matter fractional anisotropy and social impairment in children with autism spectrum disorder. Brain Res. 1362, 141–149 (2010).
- Catani M, Jones DK, Daly E et al. Altered cerebellar feedback projections in Asperger syndrome. Neuroimage 41(4), 1184–1191 (2008).
- Lange N, Dubray MB, Lee JE et al. Atypical diffusion tensor hemispheric asymmetry in autism. Autism Res. 3(6), 350–358 (2010).
- Poustka L, Jennen-Steinmetz C, Henze R, Vomstein K, Haffner J, Sieltjes B. Fronto-temporal disconnectivity and symptom severity in children with autism spectrum disorder. World J. Biol. Psychiatry 13(4), 269–280 (2012).
- Cheng Y, Chou K, Chen I et al. Atypical development of white matter microstructure in adolescents with autism spectrum disorders. Neuroimage 50(3), 873–882 (2010).
- Dickstein DP, Pescosolido MF, Reidy BL et al. Developmental meta-analysis of the functional neural correlates of autism spectrum disorders. J. Am. Acad. Child Adolesc. Psychiatry 52(3), 279–289 (2013).
- Autism and Developmental Disabilities Monitoring Network Surveillance Year 2008 Principal Investigators; Centers for Disease Control and Prevention. Prevalence of autism spectrum disorders – Autism and Developmental Disabilities Monitoring Network, 14 sites, United States, 2008. MMWR Surveill. Summ. 61(3), 1–19 (2012).
- Sheinkopf SJ, Siegel B. Home-based behavioral treatment of young children with autism. J. Autism Dev. Disord. 28(1), 15–23 (1998).
- Harris S, Handleman J. Age and IQ at intake as predictors of placement for young children with autism: a four- to six-year follow-up. J. Autism Dev. Disord. 30(2), 137–142 (2000).
- Anderson JS, Nielsen JA, Froehlich AL et al. Functional connectivity magnetic resonance imaging classification of autism. Brain 134(Pt 2), 3742–3754 (2011).
- Adluru N, Hinrichs C, Chung MK et al. Classification in DTI using shapes of white matter tracts. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2009, 2719–2722 (2009).
- Bloy L, Ingalhalikar M, Eavani H, Roberts TPL, Schultz RT, Verma R. HARDI based pattern classifiers for the identification of white matter pathologies. Med. Image Comput. Comput. Assist. Interv. 14(Pt 2), 234–241 (2011).
- Lange N. Perspective: imaging autism. Nature 491, S17 (2012).
- Dichter GS, Richey JA, Rittenberg AM, Sabatino A, Bodfish J. Reward circuitry function in autism during face anticipation and outcomes. J. Autism Devel. Disord. 42(2), 147–160 (2010).
- Koegel RL, Kern Koegel L. Pivotal Response Treatments for Autism: Communication, Social, and Academic Development. Brookes Publishing, Baltimore, MD, USA (2006).
- Voos AC, Pelphrey KA, Tirrell J et al. Neural mechanisms of improvements in social motivation after pivotal response treatment: two case studies. J. Autism Dev. Disord. 43(1), 1–10 (2013).
- Bolte S, Hubl D, Feineis-Matthews S, Prvulovic D, Dierks T, Poustka F. Facial affect recognition training in autism: can we animate the fusiform gyrus? Behav. Neurosci. 120, 211–216 (2006).
- Coben R, Linden M, Myers TE. Neurofeedback for autistic spectrum disorder: a review of the literature. Appl. Psychophysiol. Biofeedback 35, 83–105 (2010).
- Oberman LM, Hubbard EM, McCleery JP, Altschuler EL, Ramachandran VS, Pineda JA. EEG evidence for mirror neuron dysfunction in autism spectrum disorders. Cogn. Brain Res. 24, 190–198 (2005).
- Pineda JA, Brang D, Hecht E et al. Positive behavioral and electrophysiological changes following neurofeedback training in children with autism. Res. Autism Spectr. Disord. 2(3), 557–581 (2008).
- Coben R, Hudspeth W. Mu-like rhythms in autistic spectrum disorder: EEG analyses and neurofeedback. Presented at: 14th Annual Conference of the International Society for Neuronal Regulation, Atlanta, GA, USA, 7–10 September 2006.
- Yoo SS, Jolesz FA. Functional MRI for neurofeedback: feasibility study on a hand motor task. Neuroreport 13, 1377–1381 (2002).
- Dawson G, Jones EJ, Merkle K et al. Early behavioral intervention is associated with normalized brain activity in young children with autism. J. Am. Acad. Child Adolesc. Psychiatry 51(11), 1150–1159 (2012).


