Research Article - Imaging in Medicine (2022) Volume 14, Issue 7
A Novel CT Body Position For Breast Cancer Patients, Utilizing A Customized Breast Pad - A Viable MRI Substitute, Producing Superior Results Than Standard MDCT Protocols
Yordan Spirdonov*
Queen Joanna University Hospital, Bulgaria
Abstract
Breast cancer staging with unclear local status after mammography and ultrasonography is by guidelines done with MRI, however, we are faced with a diagnostic and methodologic problem when MRI is contraindicated or impossible to perform. Deformation, distortion, change of density and location of the mammary glands (including their pathologies) occur with standard MDCT in supine position. To replace MRI, we introduced the prone position for staging without MRI on a specially designed CT breast pad (RCD-008478879-0001 and RCD-008478879-0002). The protocol (modus Spirdonov) includes MDCT scanning of the thorax and upper abdomen with contrast with 50-60 seconds delay. We present results of 114 patients with breast cancer scanned on our CT breast pad. Measurements along the midclavicular line in 113 women showed reduction of the anteroposterior mammary gland diameter 2 to 6.8 times when comparing supine CT scanning with prone (modus Spirdonov MDCT). Another finding was the lateral deviation of the mammilla up to 105º. Based on our experience, we concluded that in 9.6% of cases the standard MDCT protocol was inaccurate in determining the cancer location and relation to the surrounding structures. In a comparative group of 19 patients, who had MRI and CT (modus Spirdonov) performed, the results and conclusions were fully concordant and with minimal measurement differences. In summation, MDCT modus Spirdonov, performed on our CT breast pad, surpasses the standard supine position in determining the breast cancer lesion dimensions, location and analysing the surrounding tissues. MDCT modus Spirdonov, when combined with the CT breast pad, is a true alternative to MRI – when MRI is contraindicated or impossible. Goals: To present the results from prone MDCT of thorax and abdomen performed on the CT breast pad for locoregional staging of patients with breast cancer - when MRI is impossible to perform.
Keywords
Body MDCT • breast carcinoma • magnetic resonance imaging • TNM classification • chest wall • contraindications
Introduction
Accuracy in breast cancer staging, in accordance with the TNM classification system, is essential for the treatment and prognosis of every patient. Our target group was patients whose local status (multifocality/multicentricity, lesion dimensions, relations to skin, retromammillary space and thoracic wall) could not be assessed by mammography and ultrasound. In these cases MRI is indicated. When permorning the latter is impossible, a diagnostic difficulty arises.
In the standard MDCT supine position gravity dislocates the mammary glands laterally, distorts and deforms the gland parenchyma, alters the parenchymal density itself and the localization and distribution of any pathologic lesions.
In trying to cope with these diagnostic diffictulties when staging without MRI at our disposal, we began scanning in a new body position with a specially designed pad – aiming to replace MRI scanning in these cases. We present our findings and observations from scanning 114 breast cancer patients using this method. All of the patients had had the carcinoma diagnosed and verified with mammography, ultrasound and core-needle biopsy respectively.
Methods
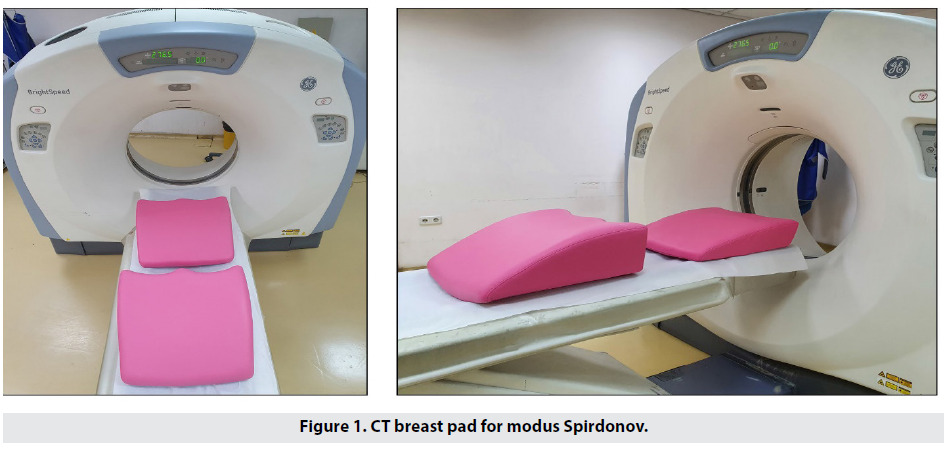
Patients were scanned with a GE BrightSpeed CT scanner. Instead of lying supine, the patient is placed in a prone position with their chest supported.In order to achieve this we designed a universal pad (CT breast pad for modus Spirdonov – Figure 1) with two different heights – 22 and 14cm respectively, depending on the individual chest and breast size. The pad is made from hard polyurethane foam (radiolucent), wedge-shaped, and open in the front with two arches for the breasts. The pad is placed on the scanner table and the patient lies on top of it. This way the chest is supported and steadily fixed in our desired position well shown on the topograms.
The acquired detailed images in this position are informative and close to those obtained by MRI.
In summary the MRI contraindications which we encountered can be divided in three groups:
1. Absolute – pacemakers and other wellknown contraindications.
2. Anatomical – thoracic cage variants and pathologies (very large size, deformations of spine, severe scoliosis), large breasts that cannot fit in the coils.
3. Conditional – claustrophobia, fear from the magnetic field, refusal to use contrast matter, etc.
The sizes of MRI coils are the first limiting factor. The free space above the antenna - particularly in GE Healthcare 1.5 T – is 24cm high by 54cm wide. Above our pads in GE Bright Speed CT apparatus, the free space dimensions were respectively 35.5 / 43.5 cm in height, and 68 cm in width. We gain 11.5 / 19.5 cm in height and 14 cm in width. The second limiting factor is the size of openings in the MRI coils. In CT, the modus Spirdonov breast pad has practically no limitations in the size of mammary glands. The only limiting factor for performing of MDCT modus Spirdonov remains the body weight of the patient, up to 180 kg. These parameters extend the cohort for MDCT breast scanning with patients who are not eligible for MRI.
The examinations were performed with GE Bright Speed after positioning of patient on the modus Spirdonov breast pad with slice thickness of 5mm, before and after semiautomatic injection of 1-2 ml/kg, 4 mL/s Iomeron 400, at 50-60 seconds. Further in the text this protocol will be abbreviated as “modus Spirdonov”. The obtained native and contrast-enhanced MDCT images, reconstructions, subtractions, involving mammary glands, thoracic cage, and abdomen, are reviewed. The control group of 19 patients was examined with GE Healthcare 1.5T by protocol: Ax T2 FSE, As DWI, +C Ax Vibrant multiphase (6 phase), Cor T2 FSE Fat Sat, left Sag T2 FSE Fat Sat, right Sag T2 FSE Fat Sat.
Standard MDCT and MDCT modus Spirdonov were reviewed by two radiologists, each with 17 years’ experience in breast cancer imaging, who were unaware of the MRI results. Another radiologist with similar credentials independently analyzed the MRI itself. All of them had access to the MG, US, and the histologic report. The results from standard MDCT, MDCT modus Spirdonov, and MRI were classified according to BI-RADS.
Material
For a period of 41 months (from October 2017 to March 2021) we scanned 114 patients (113 female and one male) with standard MDCT and MDCT modus Spirdonov. The age ranged from 26 to 96 years. All of them filled in and signed an informed consent. The group included patients with performed MG, US with BI-RADS 4 or 5, in which CNB was performed under US control. We aimed to overcome the aforementioned difficulties in staging, simultaneously with examining the upper abdomen.
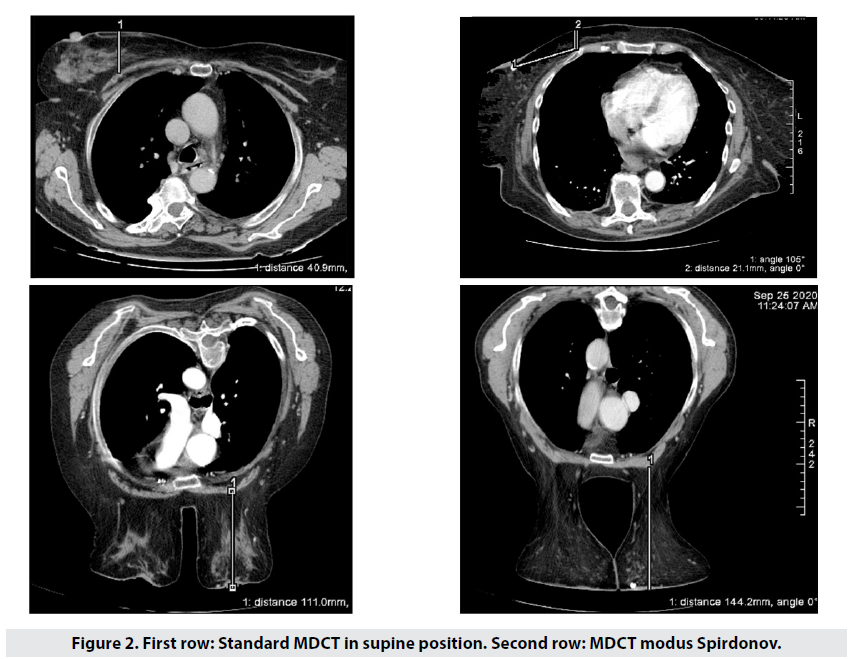
We would like to point out the fact that in the standard supine body position there is marked deformation and distortion of breast parenchyma, as well as change in the density, location and distribution of lesions, depending very much on and varying with the size of breasts. In 113 patients, the midclavicular breast anteroposterior diameter showed wide variation – 2.7 to 6.8 times longer when prone (Figure 2) when compared with the supine position.
The varying lateral mammillar deviation and parenchymal redistribution cause such marked differences in appearance, that the reviewer could mistake the images for those of another patient.
A distinct diagnostic obstacle is cases of histologically proven breast cancer where suspicion of multifocality/multicentricity and chest wall, skin or retromammillary space invasion persists, but MRI is contraindicated. This compelled us to diverge from the NCCN guidelines and CT scan 24 patients with preliminary lesion size below 20mm.
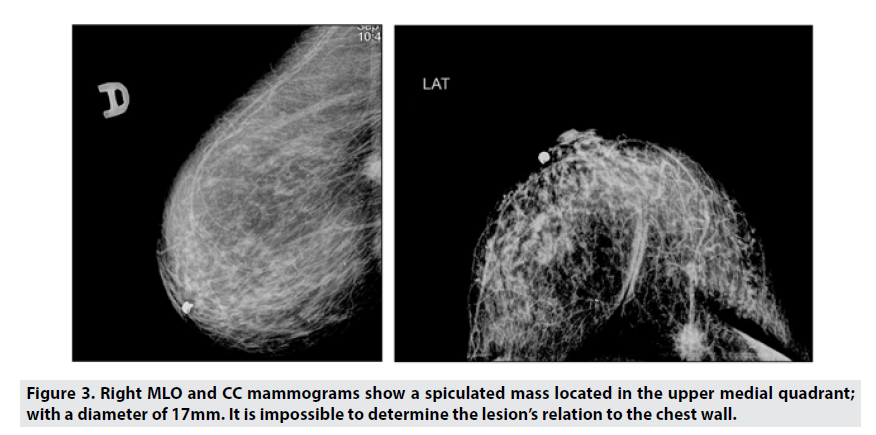
We present a female patient with mammographies in craniocaudal (CC) and mediolateral oblique (MLO) projections, which showed an upper medial quadrant lesion – Figure 3.
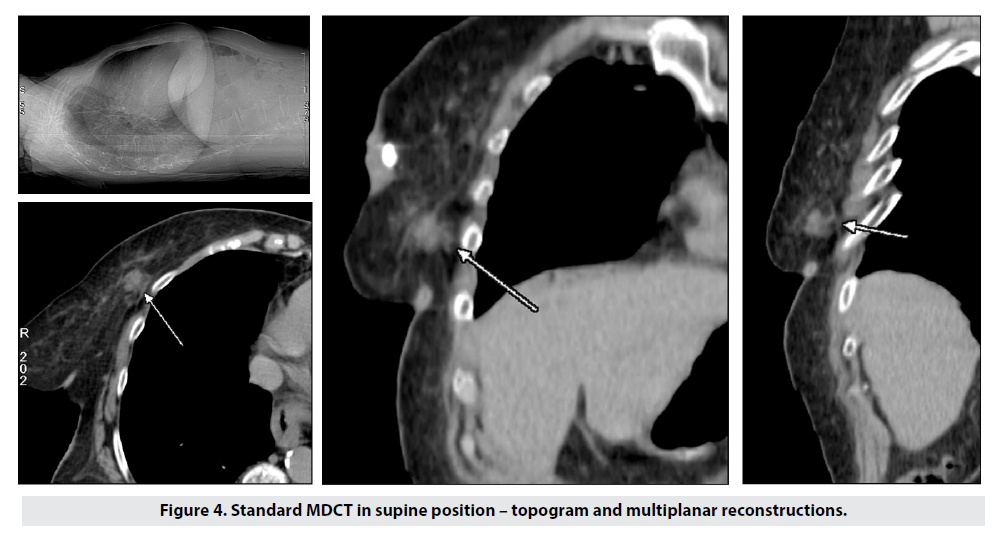
We initially performed standard supine CT, which demonstrated the lesion in contact with the chest wall, with signs of infiltration of the surrounding and underlying tissues. The breast parenchyma was distorted and displaced – Figure 4.
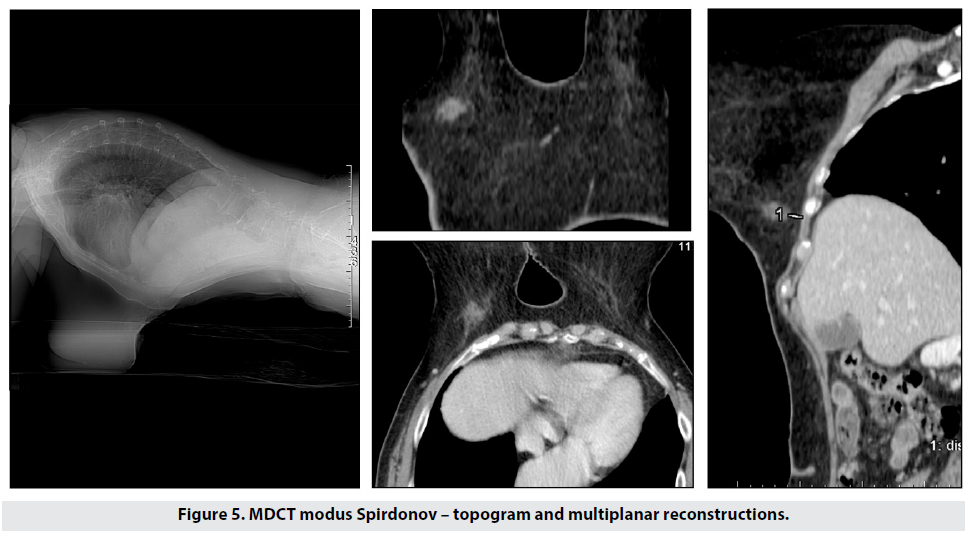
For comparison we scanned the patient using our prone protocol (Figure 5), and the acquired images and reconstructions clearly showed the following:
1. Lesion size of 15mm, 9.9mm away from the chest wall;
2. The true lesion location was in the lower medial quadrant.
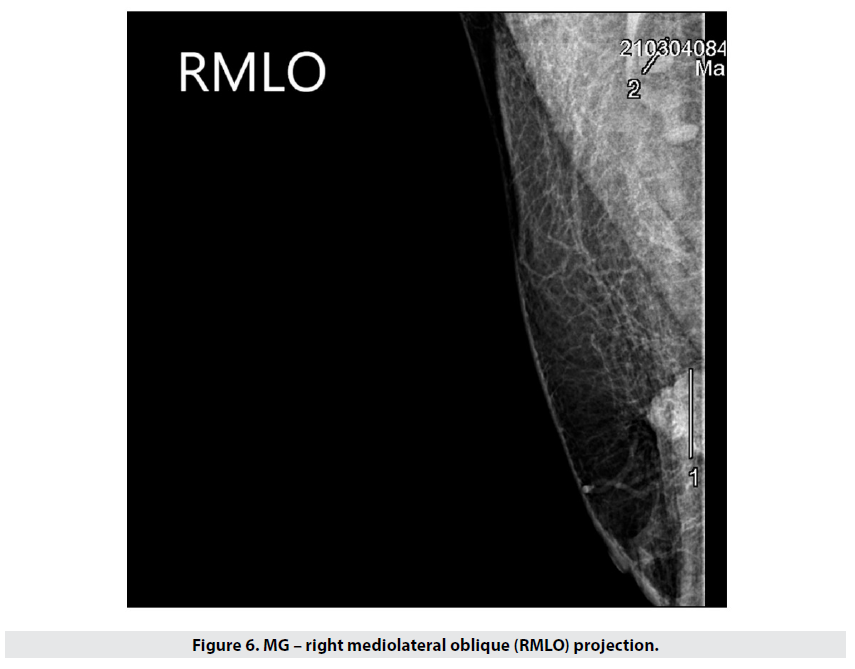
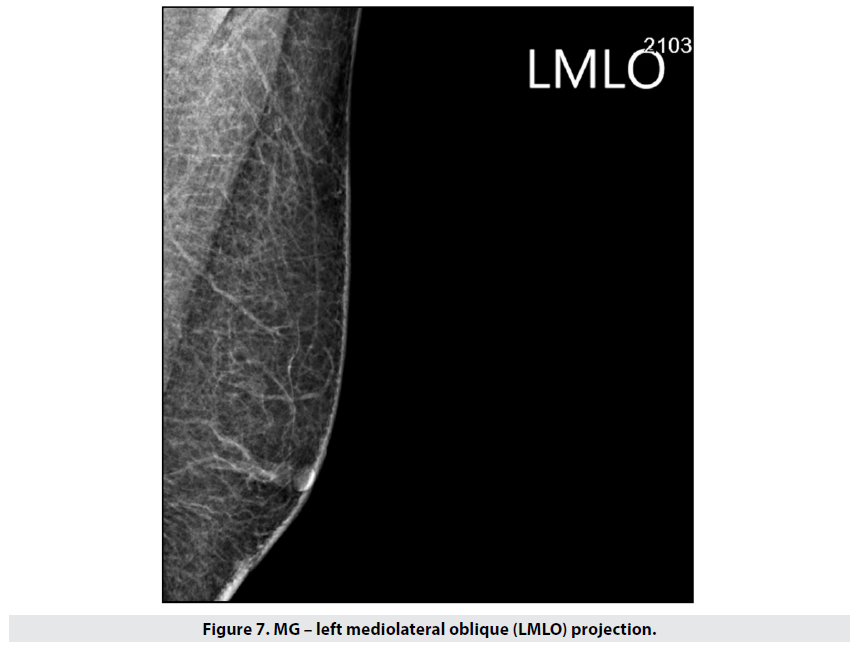
A similar case was that of a man with a right upper lateral quadrant lesion. Mammography showed a dense irregular and lobulated opacity 27mm wide, with unclear margins towards the chest wall – Figure 6 (the finding is at the edge of the visual field). Left breast – unremarkable (Figure 7).
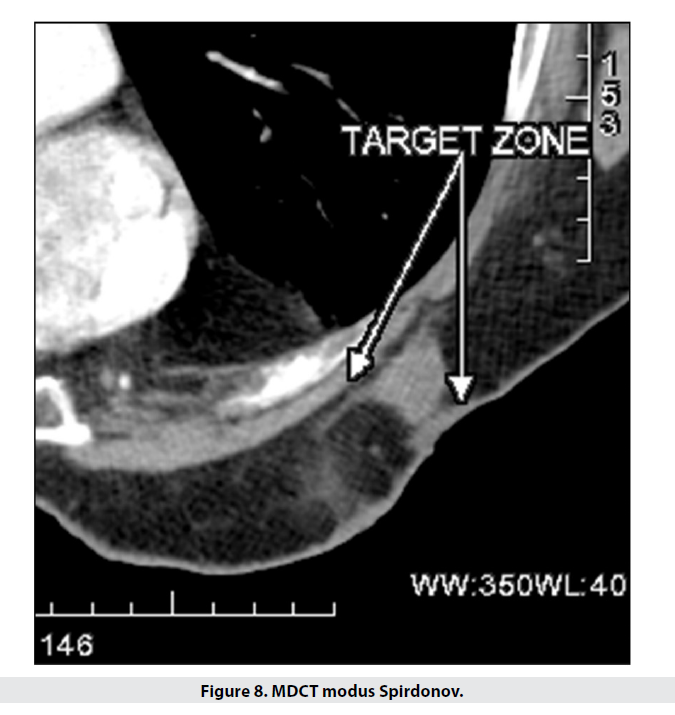
Our areas of interest were the chest wall and skin and subcutaneous tissue. The initial investigation was the prone CT scan, which showed a 25mm lesion with no chest wall invasion. The only finding was subcutaneous tissue traction, induration and edema, without skin involvement – Figure 8.
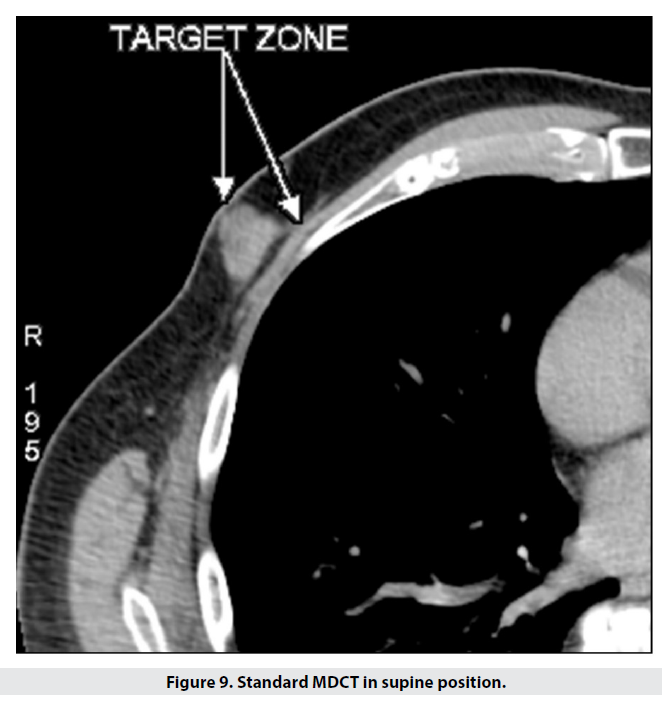
For comparison, we scanned the patient supine. In this study the lesion appeared to be in contact with the chest wall medially, with skin and subcutaneous tissue seemingly unchanged – Figure 9.
The postoperative histologic report defined the tumour as poorly differentiated G3 invasive ductal carcinoma, 25mm in diameter, with hypoderm involvement; no carcinomatous infiltration of the overlying skin. These findings fully coincide with the results of our prone CT study, as opposed to the standard supine scan.
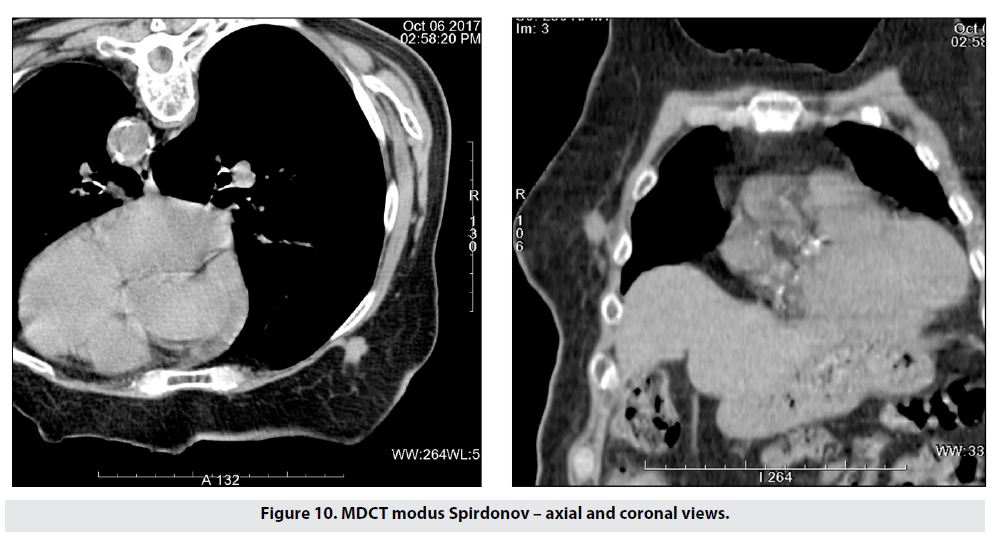
Figure 10 shows our first patient, scanned with our prone CT protocol. The study showed a 14mm right breast lesion infiltrating the chest wall.
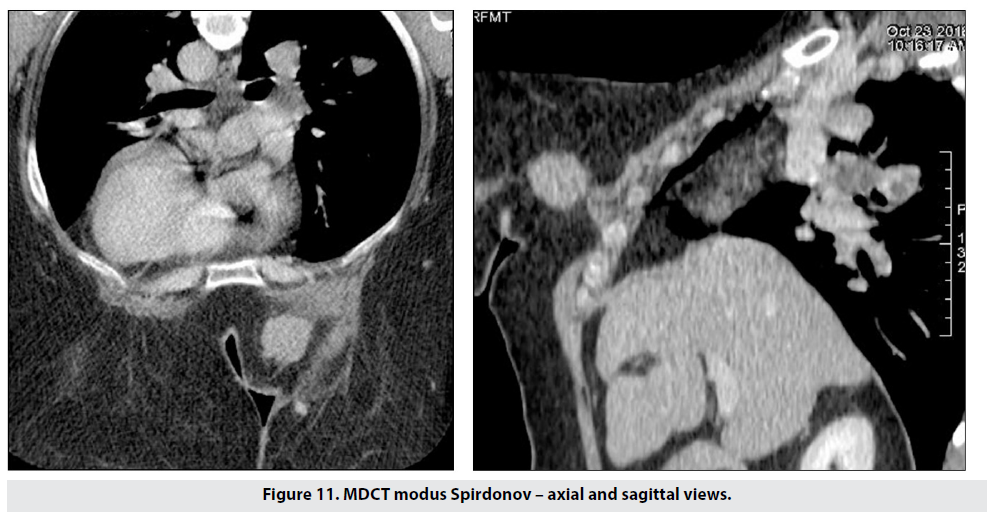
Figure 11 shows the capabilites of the method for detecting chest wall invasion and pulmonary spread simultaneously. This patient was contraindicated for MRI due to breast size and severe thoracic kyphosis.
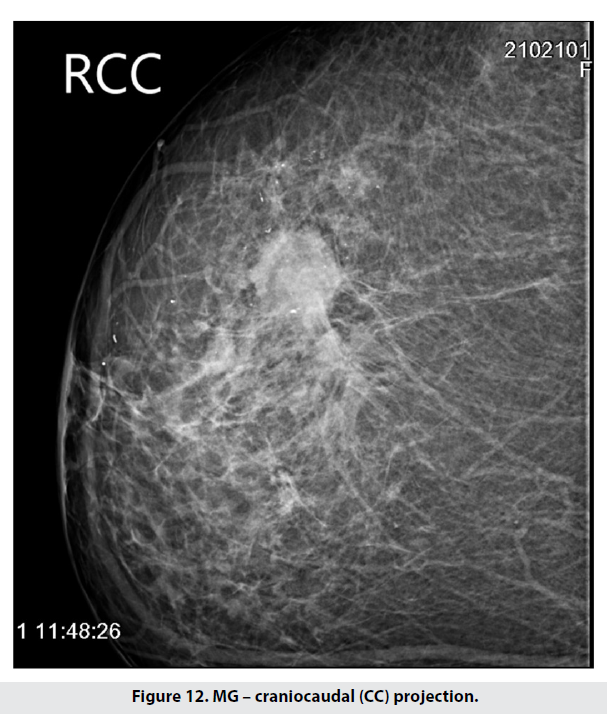
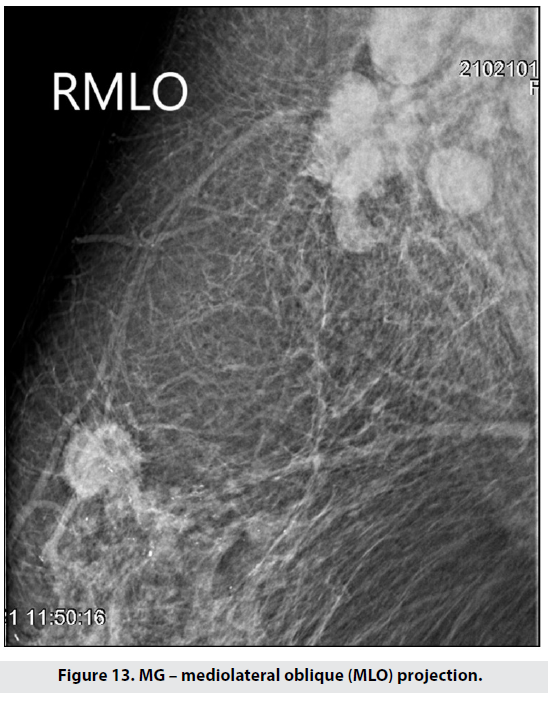
The next case is of a patient of whom we had to take targeted mammographies due to large breast size. The right CC showed a 29mm lesion laterally and anteriorly, together with grouped microcalcifications – Figure 12. On the MLO radiograph a cluster of enlarged lymph nodes was evident in the axilla – Figure 13.
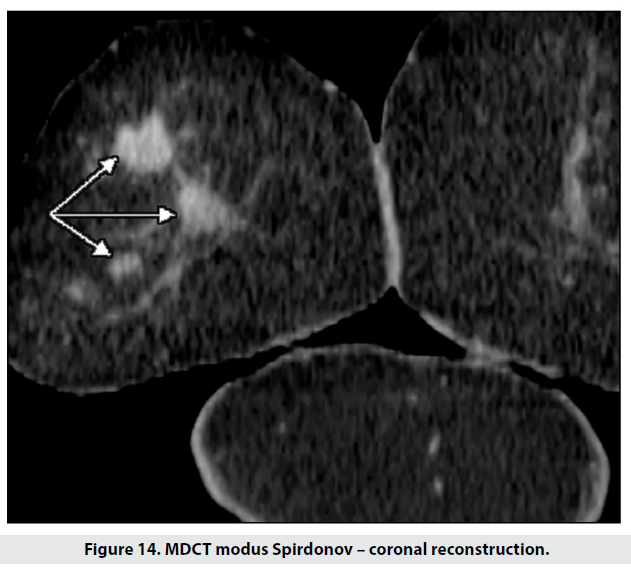
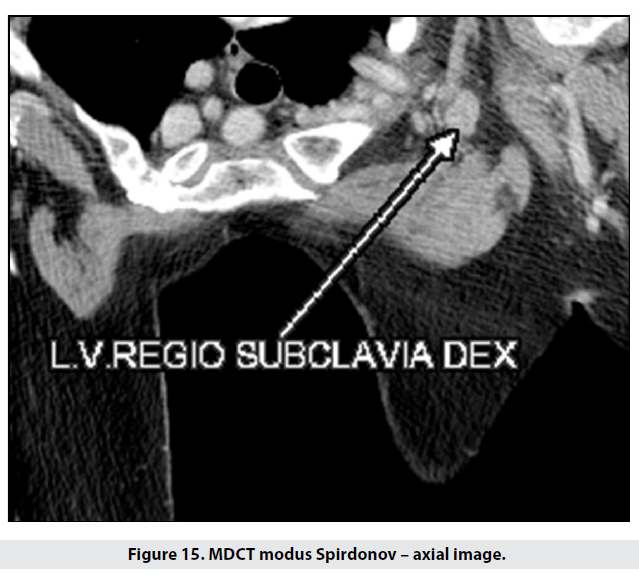
Next we performed a prone CT scan with coronal reformats, which showed two new lesions – 22 and 12mm respectively (Figure 14). Besides the previously known axillary lymph nodes, a new metastatic node (20mm) was discovered along the right subclavian vein (Figure 15).
In order to perform organ-sparing surgery and intraoperative radiotherapy, the surgical team needs precise information about the lesion and patient. Our prone CT modus Spirdonov was the method of choice in assessing and staging 21 patients. Figure 16 shows a right lower lateral quadrant lesion in the axial, saggital and coronal planes. The lesion was estimated to be 15.5mm in diameter, with no skin involvement, at a sufficient distance from the mammilla; the axilla was unremarkable. The age of the patient, alongside the imaging findings, allowed lumpectomy and IORT (intraoperative radiation therapy) in accordance with the ASTRO (American Society for Radiotherapy and Oncology) and ESTRO (European Society for Radiotherapy and Oncology) criteria.
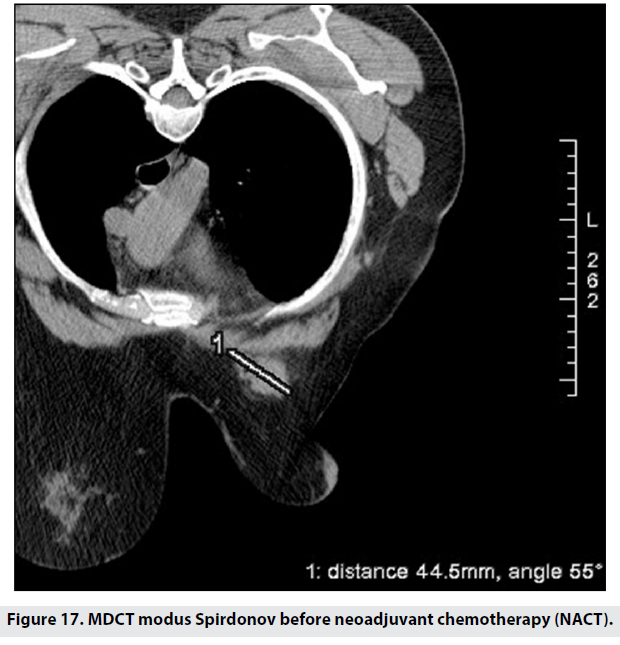
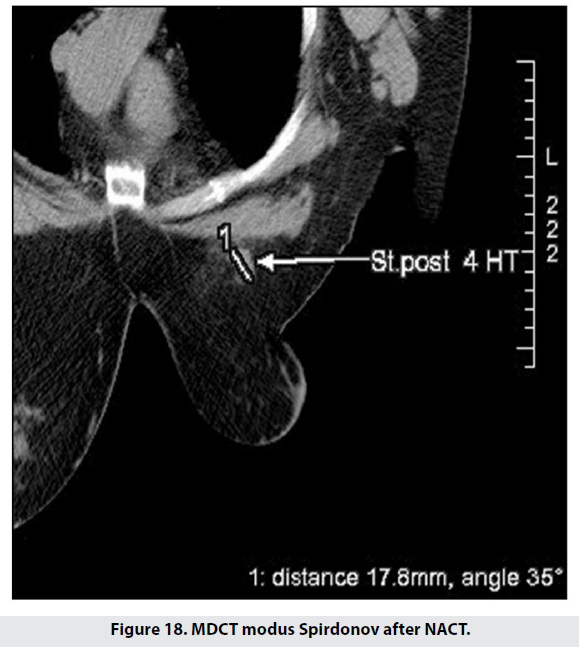
We used the prone CT scanning technique to follow-up 17 patients’ response to neoadjuvant chemotherapy – Figures 17 and 18. The latter figure shows a clear size reduction as well as separation from the chest wall.
Figure 17: MDCT modus Spirdonov before neoadjuvant chemotherapy (NACT).
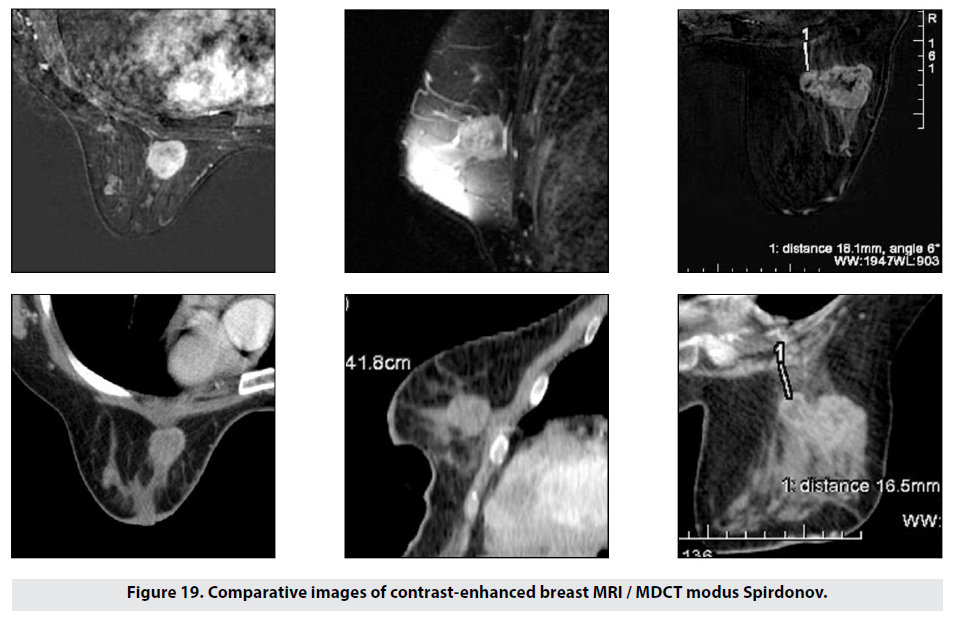
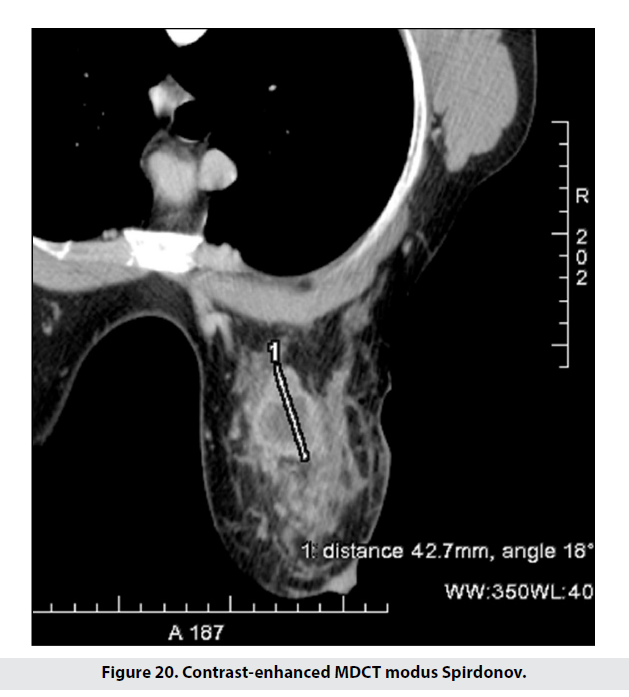
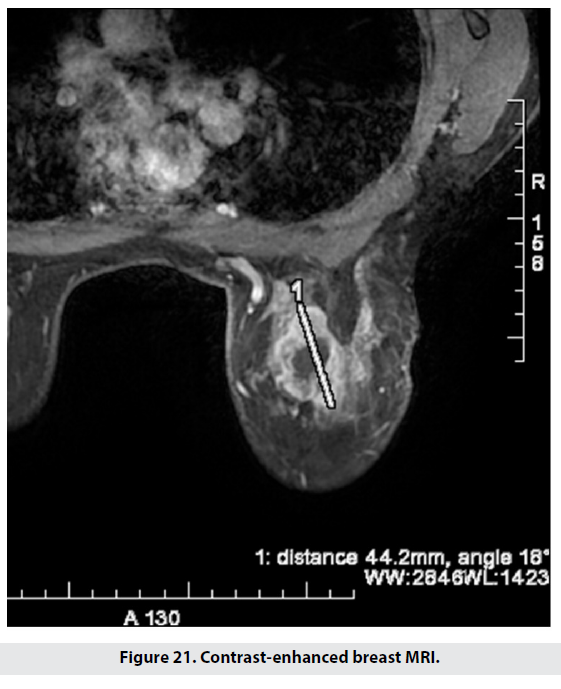
To compare results between modus Spirdonov prone CT and standard breast MRI, patients were assessed based on 19 staging criteria. The acquired results from the two imaging methods were verified histologically with respect to multifocality/multicentricity, size and location, signs of involvement of chest wall, skin, and mamilla. The obtained images from MDCT modus Spirdonov were detailed and very close to those of MRI, including no significant measurement differences (Figures 19-21).
Results
114 patients with breast cancer – diagnosed by MG and US – were scanned with MDCT modus Spirdonov, while the lesions discovered were further evaluated with US-guided CNB. The average patient age was 55 years (median: 56 years; SD: 13.1 years; range: 26-96 years).
The excluding factors for breast MRI in our 95 patients have the following distribution: absolute – 10; anatomical – 79; relative – 6 patients.
In our 113 female patient cohort, measurements were made along the midclavicular line when scanning supine and prone. The results show a marked reduction in the anteroposterior breast dimensions in supine scanning as compared to the prone position – 2 to 6.8 times. The most frequently measured value was 2.7 times and this index increases proportionately to the breast size.
Furthermore, we found lateral deviation of the mammilla of up to 105°.
We note the fact that due to the deformation and lateralization of the mammary glands in 11 out of 114 patients (9.6%), standard MDCT determined inaccurately the location of the lesion and its relations to the adjacent tissues by quadrants, in comparison with MDCT modus Spirdonov, which were verified operatively.
The found the optimal scanning window for the contrast series to be between 50 and 60 seconds, for the best visualization of the changes in the breast parenchyma along with any pathologic lesions. This is the optimal time for imaging the subclavian vein, mediastinal, lung, and liver metastases portovenous phase.
In 17 patients when assessing the response to neoadjuvant chemotherapy, we found the difference between our tumour size estimate and that of the pathologic report to be less than 4mm.
Lumpectomy was performed in 21 patients with IORT in accordance with the ASTRO and ESTRO criteria. The difference in carcinoma size determined with MDCT modus Spirdonov varied only up to 2 mm from the definitive histologic report.
Out of 11 patients with retromammillary lesions our results differed from the histologic report only once being falsely positive regarding chest wall invasion.
In 15 out of 114 patients (13.1%) with T2, T3, and T4 disease, MDCT modus Spirdonov and standard MDCT proved hepatic and pulmonary metastases without difference in the conclusions.
In 10 out of 114 patients (8.8%) our method discovered additional findings five malignancies and five fibroadenomas.
Worth noting is that in our cohort, out of 24 patients with initial T1 disease, four were upstaged to T4; and out of 72 patients with initial T2 disease, nine were upstaged to T4 after scanning by our method.
A statistical analysis, and comparison of MDCT modus Spirdonov with standard MDCT, was implemented by the use of linear regression and rho correlation analysis of Spearman with respect to the size of tumour in millimeters. The statistical significance was accepted at 95% level of confidence (P<0.05). The study analyzed the results for 114 patients. The difference with the final size of tumor given by a pathologist and determined by standard MDCT (median: 3.12; 95% CI: 2.86-3.39; SD: 1.428), and modus Spirdonov (median: 1.82; 95% CI: 1.57-2.08; SD: 1.371), was considerable and significant (p<0.001).
The correlation between the methods and referent sizes of pathological finding (benchmark) was analyzed. Both methods have high correlation of standard MDCT (Spearman’s rho 0.91, P < 0.001), and modus Spirdonov (Spearman’s rho 0.856, P < 0.001). A linear connection was found between the two methods (standard MDCT = 0.901 × modus Spirdonov + 1.479; rho coefficient of correlation of Spearman, 0.861; P < 0.001, correlational coefficient of Pearson, 0.866; P < 0.001).
The test of Friedman in the control group of 19 patients showed statistically significant difference in the result in standard MDCT compared to MRI and modus Spirdonov (p < 0.001): MRI (Mean Rank: 1.50), modus Spirdonov (Mean Rank: 1.53), standard MDCT (Mean Rank: 2.97).
The analysis by criteria for staging of the control group, (19 patients with successively performed MRI and CT modus Spirdonov), verified operatively and histologically with respect to size, location, and signs of involvement of thoracic wall, skin, and mamilla, provided full compliance in the results and conclusions for breast cancer with minimal clinically insignificant differences in the determination of sizes.
Discussion
The most commonly used breast imaging method is mammography, followed by digital breast tomosynthesis (DBT); they are performed with compression that deforms the breast parenchyma. The benefit of MG is limited in dense breasts, which with DBT is overcome to some extent due to the narrow angle of scanning. A comparatively new technique for visualization of breasts is Dedicated Cone-Beam Breast Computed Tomography (DCBBCT). In all of these techniques, regardless of the breast positioning, analysis of the entirety of the chest wall and axilla is impossible. DCBBCT has proven itself to be as successful in diagnosing breast cancer as conventional imaging methods. We must, however, note that both mammary glands, simultaneously with thoracic wall, axillae, and both subclavian arteries and veins, can only be entirely visualized with MRI, MDCT, and PET/CT.
Comparing our MDCT (supine and prone) lesion measurements with those at histology is reassuring of the capabilities of this imaging modality. The differences in measurements vary between 3.12mm and 1.82mm (for the supine and prone position respectively). It is evident that MDCT modus Spirdonov surpasses the standard supine position in this regard. Our data is comparable to the results of other researchers, who discovered differences of less than 5mm and less than 6mm.
Several research teams examined the utility of supine MDCT to diagnose and locally stage breast cancer. We support their conclusions that MDCT is an accurate preoperative imaging modality. Only one research group expresses doubts regarding the efficiency of MDCT (7% false positive results in multifocal/multicentric disease).
One research team retrospectively analyzed standard MDCT studies after performing mammography and ultrasound and found additional benign as well as malignant breast lesions.
In our cohort out of 114 patients MDCT modus Spirdonov discovered additional management altering findings after mammography and ultrasound in 8.8% of cases. We found that the 50-60 second contrast series is optimal in displaying in detail both breast lesions as well as distant metastases. Our window of scanning is earlier than that which other research teams use and recommend – in DCBBCT 120s; in 3D body MDCT 100s; 80-90s and 90 and 300s. We point out that the single, at-once contrast administration is a definite advantage of MDCT over DCBBCT.
We found a relatively low sensitivity of MDCT (lower when supine when compared to the prone position) in detecting microcalcifications only 65%. Other teams express similar difficulties when working with DCBBCT.
The newer 3D body MDCT and other specialized devices are emerging as promising new methods which are nearing breast MRI in capabilities. One team /15/ reports that native DCBBCT has a comparable sensitivity to breast MRI and that CE-CBBCT has lower sensitivity, but higher specificity than MRI. Other teams compared chest MDCT to MRI and reported high results for sensitivity, specificity and accuracy in 3D body MDCT. This gives them reason to conclude that the modality could be an alternative to and replace 3D MRI as a preoperative imaging method of choce in breast cancer. Team explores the rare side effects of the gadolinium contrast agent’s nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD).
Worth remembering is that a positive MRI result is actually falsely positive in 83%. Taking into account the contraindications, prices of the examination itself and the patient discomfort this all reduces its usability in practice.
A very important consideration is that the aforementioned results of comparing both methods (breast MRI and 3D body MDCT) are from standard supine studies. We believe they could be even more competitive against MRI when performed prone using the CT breast pad for modus Spirdonov (thereby overcoming tissue deformation and distorsion and reducing discrepancies regarding localization and surrounding tissue infiltration).
Two other teams also performed targeted trials examining the possibilities of MDCT as an alternative to MRI. Our findings completely concur with their conclusions. Only these two teams scanned their patiens using a “specially made device” and a “support for positioning” respectively essentialy copies of the MRI coils. We started with an identical device in 2017, and reported the preliminary results in September of 2019. The breast openings and the height of the support proved to be a problem for patients. This was the reason for us to alter the pad and produce two models with differing thicknesses, both open in the front /Figure 1/. Unlike our cohort, these teams scanned only the chest in patients with T2 and T3 carcinoma /20/ ranging from 6 to 100mm in size /21/. Our analysis discovered lung and liver metastases in 13.1% of patients with T2, T3 and T4 carcinoma.
Our small control group of 19 patients, who had had breast MRI and body CT modus Spirdonov performed, showed full concordance in the conclusions. We point out the advantage of body CT modus Spirdonov over MRI that it cannot only locally stage the disease; it can simultaneously also demonstrate metastatic spread mediastinal, pulmonary, hepatic, skeletal. This allows for the patient to have the shortest possible route towards starting therapy or operative treatment. The images acquared using body MDCT modus Spirdonov are identical to those of breast MRI, which is routinely used by modern surgeons.
We achieved our TNM staging goals without increasing the patient’s radiation dose, without increasing the cost of the investigation, in a short amount of time, in a relatively comfortable environment and body position, while overcoming tissue deformation and distorsion seen in supine body MDCT.
Conclusions
Body MDCT modus Spirdonov, together with the CT breast pad, surpasses standard body MDCT in determining measurements and localization of lesions as well as infiltration of the adjacent tissues. This proves the method to be a real alternative to breast MRI when performing the latter is not achievable. We recommend staging of breast cancer patients (even T1, when there is suspicion for chest wall invasion) to be performed using this method when MRI is not available.
Based on our experience, our team recommends performing chest CT in women in the prone position of MDCT modus Spirdonov, regardless of the indications. This position reduces often completely the parenchymal distorsion and thus could increase the chances of discovering subclinical malignant breast lesions. This is especially important in healthcare systems without an integrated mass screening program.
References
- Mehershahi S, Mantri N, Sun H et al. Metastasis From Gastric Signet Ring Cell Adenocarcinoma Presenting as a Rectosigmoid Stricture: A Rare Case. Cureus [Internet]. 12 (2020)
- Bosmon FT, Carneiro F, Hruban RH et al. WHO Classification of Tumours of the Digestive System [Internet]. World Health Organization. (2010).
- Sonoda H, Kawai K, Yamaguchi H et al. Lymphogenous metastasis to the transverse colon that originated from signet-ring cell gastric cancer: A case report and review of the literature. Clin Res Hepatol Gastroenterol. 41, e81–6 (2017).
- Ogiwara H, Konno H, Kitayama Y, et al. Metastases from gastricadenocarcinoma presenting as multiple colonic polyps: report of a case. Surg today. 24, 473-475 (1994).
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref