Case Report - International Journal of Clinical Rheumatology (2020) Volume 15, Issue 1
A ‘crowning’ diagnosis: Fever, neck pain, and diffuse polyarthritis as a fulminant first presentation of pseudogout
- Corresponding Author:
- Samuel Gaine
Graduate Entry Medical School
University of Limerick, Limerick, Ireland
E-mail: u2samuel@gmail.com - Maximilian F. Konig
Division of Rheumatology
The Johns Hopkins University School of Medicine
Baltimore, MD, USA
E-mail: konig@jhmi.edu
Abstract
Background: Calcium Pyrophosphate Deposition Disease (CPPD) rarely presents as a diffuse polyarthritis with systemic features. Case presentation: A 75-year-old man with no prior history of rheumatic disease presented with acuteonset diffuse polyarthritis and severe neck pain, accompanied by fevers, leucocytosis, and elevated acute phase reactants. After excluding infectious aetiologies, a synovial fluid aspirate revealed a highly neutrophilic inflammatory infiltrate and rare calcium pyrophosphate dihydrate crystals. Cervical CT confirmed periodontoid calcium deposits consistent with the crowned dens syndrome. The patient was diagnosed with acute CPPD, and his joint and neck pain improved rapidly with colchicine and glucocorticoids. Conclusion: In addition to arthrocentesis and microscopic crystal analysis, cervical CT can lend support to a diagnosis of pseudogout complicated by CDS. In patients presenting with fever and neck pain, recognition that CDS can be a prominent or isolated feature of acute CPPD facilitates diagnosis, limits unnecessary procedures, and allows for early initiation of appropriate therapy.
Keywords
calcium pyrophosphate deposition disease • pseudogout • crowned dens syndrome • CT
Abbreviations
CDS: Crowned Dens Syndrome; CPPD: Calcium Pyrophosphate Deposition Disease; CT: Computed Tomography; GCA: Giant Cell Arthritis; PMR: Polymyalgia Rheumatica; RS3PE: Remitting Seronegative Symmetrical Synovitis with Pitting Edema
Introduction
Calcium pyrophosphate dihydrate crystal deposition disease (CPPD), often referred to as pseudogout, is the second most common form of crystalline arthritis. CPPD results from formation of calcium pyrophosphate dihydrate crystals in cartilage, synovium, and other soft tissues, which can trigger local or systemic inflammatory responses [1]. CPPD frequently manifests as episodic acute mono- or oligo arthritis that can mimic gout. While often recognised clinically and radiographically, the gold standard for diagnosis of CPPD arthritis is arthrocentesis with demonstration of positively birefringent calcium pyrophosphate dihydrate crystals under polarized light.
Hartley first reported on the association of CPPD with acute neck pain, later coined the ‘Crowned Dens Syndrome’ (CDS) by Bouvet et al. [2,3] The term CDS has been used to describe both the clinical syndrome arising from inflammation associated with calcium deposits around the odontoid process and the radiographic entity. Here, we report a case of fulminant polyarthritis complicated by CDS as a rare first presentation of CPPD in an elderly man. Although periodontoid calcification can be observed in asymptomatic patients, identification of CDS by CT was an important aid to the correct diagnosis in this man without prior history of joint disease [4].
Case Report
Case presentation
A 75-year-old retired man with hereditary spherocytosis, hypertension, type II diabetes mellitus, and right rotator cuff injury presented with fevers and sudden-onset of diffuse joint pain and swelling.
He was in his usual state of health until three days prior to presentation when he awoke with severe pain in his shoulders, elbows, wrists, hands, knees, and ankles. He noted chills and subjective fever. The following day, the pain spread to include his lower back and neck. He was unable to make a grip or brush his teeth due to pain and stiffness in his hands and shoulders. He presented to a nearby hospital where he was noted to be febrile to 38.2 C. He was empirically started on doxycycline for possible tick-borne illness and discharged home.
Due to persistence of his joint pain, he presented to the emergency department for further evaluation and management. While he endorsed progressive worsening of his diffuse joint pain and swelling to the degree that did no longer allow him to get out of bed, he denied any headache, jaw claudication, visual changes, sore throat, cough, dyspnoea, chest pain, abdominal pain, diarrhoea, or urinary symptoms. He resided near a wooded area where he regularly walked along the grassy perimeter, but did not recall any tick bites or rashes. He had an extensive travel history. He spent time in Florida from November to May and, the previous summer, he had visited Israel and Italy with his wife. In prior years, he had visited Africa and Asia. He had no history of tuberculosis or malaria. He was up to date in his vaccinations. He had not started any new medications. His family history was significant for coronary artery disease, but not revealing of any autoimmune diseases or malignancies.
On initial examination, he was febrile to 38.3C (100.9F), heart rate 103, blood pressure 162/77 mmHg, respiratory rate 16, and SpO2 99%. He was lying in bed without moving his extremities unless prompted. He had conjunctival icterus. He had neck pain/stiffness with flexion or rotational movement; the range of active motion in his neck was significantly limited. His musculoskeletal exam was notable for significant joint tenderness in his shoulders, elbows, wrists, MCPs, PIPs, knees, and ankles. There was synovitis in his elbows, wrists, MCPs, PIPs, and knees bilaterally. There were large bilateral knee effusions and warmth without erythema. There was prominent pitting oedema on the dorsum of both hands.
Investigations
Laboratory findings were notable for a leucocytosis to 13.7 [NR: 4.5-11], microcytic anaemia with Hb 10.1 [NR: 13.5-17.5] and MCV 72.8 [NR: 80-96], and thrombocytopenia to 92 [NR: 150-450] which was chronically low. ESR was elevated to 76 mm/hr [NR: <22] and CRP 15.3 [NR: <3]; BUN was 28 mg/dL [NR: 7 to 20] and creatinine 1.1 mg/dL [NR: 0.5-1.1] with an elevated BUN/Cr ratio of 25; hyperbilirubinemia to 2.3 mg/dL [NR: 0.1 to 1.2], which was unconjugated; other LFTs were normal. His uric acid level was 6.5 mg/dL [NR: 3.4-7].
A chest X-ray revealed subtle right midlung and left base parenchymal opacities suggestive of atelectasis. An X-ray of the hands showed degenerative changes at the first carpometacarpal joints and distal interphalangeal joints. There was no chondrocalcinosis.
Autoimmune serologies obtained by the primary team were notable for negative ANA, rheumatoid factor, and anti-Cyclic Citrullinated Peptide (CCP) antibodies. His infectious disease workup was negative, and his fevers had not improved on initial empirical antibiotic therapy.
A day after his presentation, the man’s case was reviewed by the in-hospital rheumatology consult service. Left knee arthrocentesis was performed to exclude infectious arthritis and evaluate for crystalline arthritis. A CT with contrast of the neck soft tissue was also ordered in the setting of normal hand and wrist radiographs.
Differential diagnosis
The differential diagnosis for this man’s presentation is broad. We considered crystalinduced arthritis, including gout and CPPD. Despite his polyarticular disease, there was sparing of the smaller joints of his feet and notably no podagra, which may have supported a diagnosis of gout. While CPPD can present as arthritis and fever, this fulminant presentation of febrile polyarthritis without prior history of joint pain did not quite fit the typical picture of an acute pseudogout attack. Viral polyarthritis, such as parvovirus B19 and chikungunya arthritis (home in Florida, but no rashes were present), could not yet be excluded from the differential. Other possible aetiologies included Polymyalgia Rheumatica (PMR), Giant Cell Arteritis (GCA), endocarditis, and less likely septic arthritis pending arthrocentesis.
Other insidious-onset forms of inflammatory arthritis such as seronegative rheumatoid arthritis, spondyloarthropathies, and autoimmune connective tissue diseases were deemed less likely given both the acuity of his symptoms and lack of other suggestive features. Lyme disease was also considered unlikely, given lack of a erythema migrans, recollection of tick bite, response to doxycycline, and negative Lyme antibodies. Remitting Seronegative Symmetrical Synovitis with Pitting Edema (RS3PE) syndrome, a rare form of at times paraneoplastic tenosynovitis that is more prone to occur in elderly men, was also considered as a possible diagnosis given his prominent dorsal hand oedema. Adult-onset Still’s disease is exceedingly uncommon in his age group, and additional clinical features that would have prompted consideration of this diagnosis (Table 1).
Table 1. Differential Diagnosis of Fever, Neck Pain & Diffuse Polyarthritis.
| Aetiologies | ||
|---|---|---|
| Infectious | Autoinflammatory | Other |
| Lyme Disease Endocarditis Parvovirus B19 Chikungunya Virus Septic Arthritis |
Gout Pseudogout Adult Onset Stills Disease Seronegative Rheumatoid Arthritis |
RS3PE |
| Autoimmune | ||
| Rheumatoid Arthritis Spondyloarthropathies Giant Cell Arthritis Polymyalgia Rheumatica Other Connective Tissue Diseases |
Diagnosis
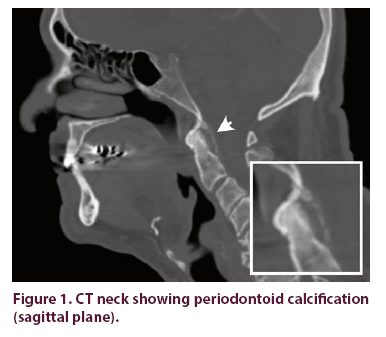
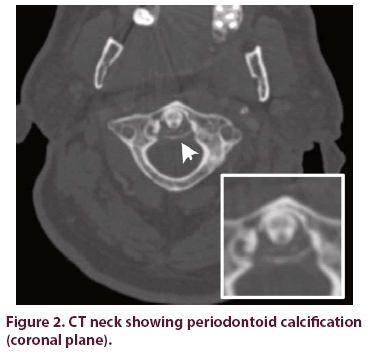
Arthrocentesis showed 14,272 leukocytes with a PMN predominance (86%), a lower count than would be expected with septic arthritis. Rare positively birefringent, rhomboid-shaped crystals consistent with calcium pyrophosphate dihydrate were observed by polarized light microscopy of centrifuged synovial fluid. CT neck revealed calcific radiodensities at the craniocervical junction with mild pannus and erosion of the posterior surface of the odontoid process, consistent with CDS. These findings confirmed the diagnosis of acute CPPD (Figures 1 and 2), while suggesting a longer-standing subclinical process.
Management
The patient was started on colchicine and continued on indomethacin, resulting in some improvement of his pain within 24 hours. Due to the substantial burden of his arthritis and negative blood and synovial fluid cultures, he was given a single dose of methylprednisolone 125 mg IV to gain better control of his symptoms. Within the next 24 hours, he noticed a dramatic improvement in his range of motion and pain which continued over the subsequent days. He was able to get out of bed and started ambulating with assistance.
One week after presentation, he felt able to perform his normal ADLs. He was discharged on a colchicine taper and as-needed prescription for future flares. He received home physical therapy and was advised to use a roller for a few weeks at home. He was discouraged from driving until any residual stiffness in his neck fully resolved. Over the next year, the patient experienced recurrence of mild joint discomfort and stiffness. His symptoms resolved and he remained symptomfree with re-initiation of daily colchicine.
Discussion
CPPD appears to affect about 5 per 1000 individuals and is primarily a disease of the elderly (mean age at diagnosis of 68) [5]. The disease has the potential to mimic several forms of inflammatory (peri-) arthritis, and distinct clinical presentations have been delineated: acute CPPD (pseudogout), chronic CPPD (pseudo-osteoarthritis or pseudo-rheumatoid arthritis), pseudo PMR, pseudo-neuropathic arthropathy, and most commonly asymptomatic chondrocalcinosis [6].
Acute arthritis and fever is not an uncommon presentation of CPPD. However, fulminant presentations characterized by acute polyarthritis involving nearly every peripheral joint and the axial skeleton in a patient with no prior history of rheumatic disease is rare.
This patient’s course highlights two instructive clinical issues. Firstly, CPPD can mimic several diseases, including autoimmune and infectious forms of arthritis, meningitis, vasculitis such as giant cell arteritis, and malignancy. In the absence of a prior history of joint disease, the differential diagnosis can be broad [1,7,8]. However, the sudden onset and severity of his joint symptoms, neck pain, and absence of clinical response to empiric antibiotic therapy narrowed the differential diagnosis to suggest a crystalline arthritis or acute viral arthritis in this patient.
Secondly, acute neck pain, particularly in the setting of suspected CPPD, should raise clinical suspicion for CDS [4,9]. Recognition of these clinical patterns and a thoughtful approach to workup can help avoid unnecessary testing, invasive procedures (e.g., lumbar punctures, temporal artery biopsy), and limit exposure to ineffective or inappropriate treatments (e.g., antibiotics, opioids) [8]. On initial presentation, the patient declined a lumbar puncture that was offered to exclude meningitis. In this patient with few risk factors (e.g., obesity and type 2 diabetes) and otherwise no radiographic evidence of CPPD, CT neck imaging was used to support the clinical suspicion of CDS.
Compared with gout, pseudogout attacks may take longer to reach peak intensity [6]. Similar to gout, CPPD can manifest with systemic features such as fevers (50%), leucocytosis, and elevated acute phase reactants, but typically has a more insidious onset. Pseudogout attacks are typically characterized by mono- or oligoarthritis, with joint pain, tenderness, swelling, and erythema affecting larger joints such as the knees (>90%), shoulders (36-48%), and ankles (32-35%) [8,10]. Podagra, which is a common feature of gout, is much less common in CPPD (<20%) [6,8].
Differentiation from gout or septic arthritis requires arthrocentesis and synovial fluid analysis for cell count with differential, crystals, Gram stain and culture. Pseudogout is confirmed by the demonstration of CPPD crystals, which often have the appearance of rhomboid-shaped or rod-like structures that exhibit weakly positive or no birefringence by compensated polarized light microscopy [11] Given the high prevalence of asymptomatic chondrocalcinosis in the aging population, the co-existence of septic arthritis needs to be considered even in a patient with microscopic or radiographic evidence of CPPD [12].
In one study, the prevalence of periodontoid calcification in patients with pseudogout of the peripheral joints or acute neck pain was higher than that in the general population without neck pain (63% and 64% vs. 13.5%, respectively). The prevalence of calcification increased significantly with age [13]. These results were consistent with those of several previous studies that found pseudogout to be strongly associated with the presence of periodontoid calcification.
CDS can be misdiagnosed as meningitis, epidural abscess, cervical spondylitis, spinal tumour , or PMR/GCA, among other conditions that can present similarly [9]. To avoid unnecessary invasive procedures and inappropriate treatment for acute neck pain, cervical CT should be considered in patients presenting with symptoms suggestive of peripheral pseudogout and acute neck pain in the elderly. In addition, the recognition that periodontoid calcification has higher frequency in pseudogout compared to asymptomatic controls suggests that a CT scan can increase diagnostic certainty when the diagnosis is unclear [4].
Conclusion
We report a case of fulminant CPPD complicated by CDS as a first presentation of pseudogout in an elderly man. This case highlights the variability in clinical presentation of a relatively common disease. In conjunction with arthrocentesis, CT imaging of the neck can increase diagnostic certainty in cases where there is clinical suspicion for CDS, thus avoiding unnecessary procedures, prolonged hospitalization, and exposure to antibiotic therapy.
Availability of data and materials
Data sharing is not applicable to this article since no datasets were generated or analyzed during this study. Ethics approval and consent to participate This case study did not require ethics approval.
Consent for publication
The patient gave written consent for publication of this report.
Competing interests
The authors declare that they have no competing interests.
References
- Rosenthal AK, Ryan LM. Calcium Pyrophosphate Deposition Disease. N. Engl. J. Med. 374(26), 2575–2584 (2016).
- Bouvet JP, Le Parc JM, Michalski B et al. Acute neck pain due to calcifications surrounding the odontoid process: the crowned dens syndrome. Arthitis. Rheum. 28: pp. 1417–1420 (1985).
- Hartley J. Acute Cervical Pain Associated with Retropharyngeal Calcium Deposit. JBJS. 46(8), 1753–1754 (1964).
- Sekijima Y. CPPD crystal deposition disease of the cervical spine: A common cause of acute neck pain encountered in the neurology department. J. Neurol. Sci. 296(1), 79–82 (2010).
- Kleiber BC, Rosenthal AK, Lans D et al. Calcium Pyrophosphate Deposition Disease and Associated Medical Comorbidities: A National Cross-Sectional Study of US Veterans. Arthritis. Care. Res (Hoboken). 69(9), 1400–1406 (2017).
- MacMullan P, McCarthy G. Treatment and management of pseudogout: insights for the clinician. Ther. Adv. Musculoskelet. Dis. 4(2), 121–131 (2012).
- Masuda I, Ishikawa K. Clinical features of pseudogout attack. A survey of 50 cases. Clin. Orthop. Relat. Res. 229, 173–181 (1988).
- Dieppe PA, Alexander GJ, Jones HE et al. Pyrophosphate arthropathy: A clinical and radiological study of 105 cases. Ann. Rheum. Dis. 41(4), 371–376 (1982).
- Scutellari PN, Galeotti R, Leprotti S et al. The crowned dens syndrome. Evaluation with CT imaging. Radiology. Medium. 112(2), 195–207 (2007).
- Bong D, Bennet R. Pseudogout mimicking systemic disease. JAMA. 246(13), 1438–1440 (1981).
- Oka A, Okazaki K, Takeno A et al. Crowned Dens Syndrome: Report of Three Cases and a Review of the Literature. J. Emerg. Med. 49 (1): e9–e13 (2015).
- Papanicolas LE, Hakendorf P, Gordon DL. Concomitant septic arthritis in crystal monoarthritis. J. Rheumatol. 39(1), 157–160 (2012).
- Kobayashi T, Miyakoshi N, Konno N et al. Age-Related Prevalence of Periodontoid Calcification and Its Associations with Acute Cervical Pain. Asian. Spine. J. 12 (6), 1117–1122 (2018).