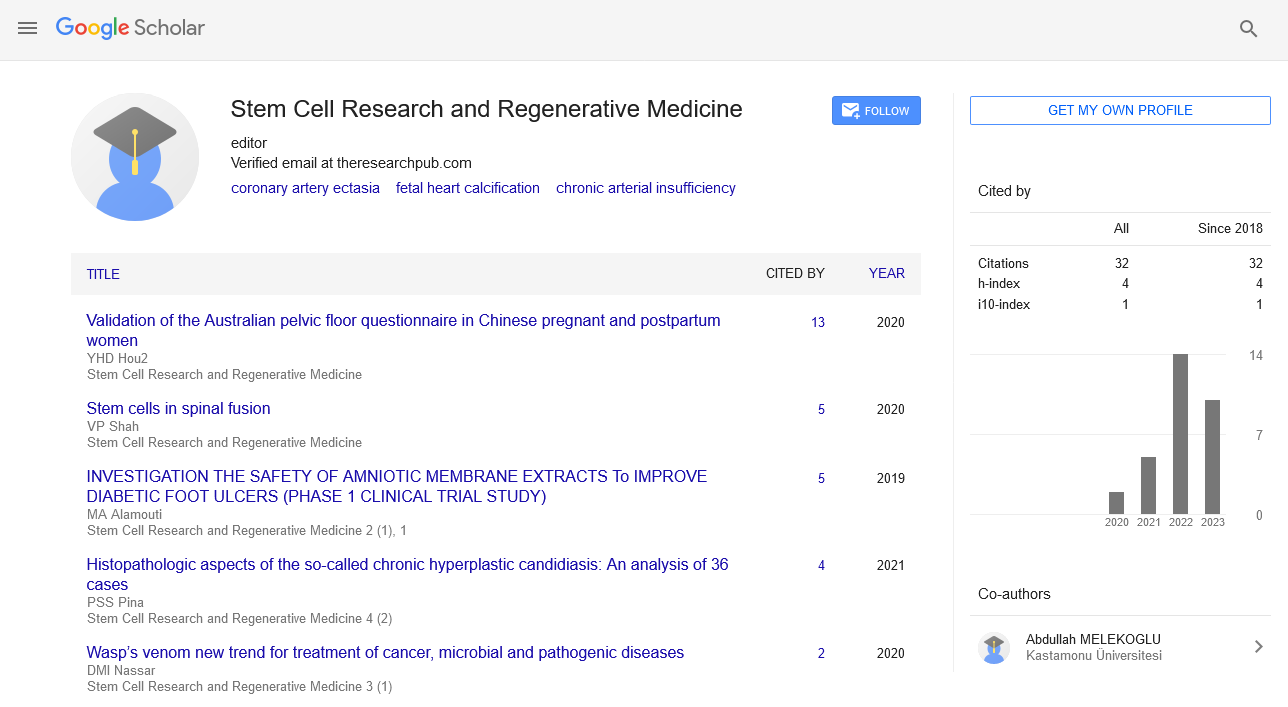
Perspective - Stem Cell Research and Regenerative Medicine (2024) Volume 7, Issue 3
Tumor Cell Biology: Mechanisms, Challenges, and Therapeutic Strategies
- Corresponding Author:
- Sandra van Vlierberghe
Department of oncology,
Vrije Universiteit Brussel,
Brussels,
Belgium
E-mail: SVvlier@UGent.be
Received: 29-May-2024, Manuscript No. SRRM-24-137542; Editor assigned: 31-May-2024, Pre QC No. SRRM-24-137542 (PQ); Reviewed: 12-Jun-2024, QC No. SRRM-24-137542; Revised: 21-Jun-2024, Manuscript No. SRRM-24-137542 (R); Published: 28-Jun-2024, DOI: 10.37532/ SRRM.2024.7(3).203-205
Abstract
Tumor cell biology is a rapidly evolving field that seeks to understand the complex mechanisms underlying cancer development, progression, and metastasis. This review provides an in-depth analysis of the key cellular and molecular processes driving tumorigenesis, the challenges in targeting these mechanisms, and the innovative therapeutic strategies being developed to combat cancer. By examining recent advancements and future directions in tumor cell science, this article aims to shed light on the intricate biology of cancer cells and highlight the potential for novel treatments to improve patient outcomes.
Keywords
Cell biology ● Metastasis ● Cancer ● Treatment ● Cell growth
Introduction
Cancer is a multifaceted disease characterized by uncontrolled cell growth and the ability to invade surrounding tissues and metastasize to distant organs. Understanding the biology of tumor cells is crucial for developing effective therapies. Tumor cells exhibit several hallmark traits, including sustained proliferative signaling, evasion of growth suppressors, resistance to cell death, limitless replicative potential, induction of angiogenesis, and activation of invasion and metastasis. These characteristics result from genetic and epigenetic alterations that disrupt normal cellular functions and enable malignant transformation.
Description
Mechanisms of tumorigenesis: The development of cancer involves a series of genetic mutations and epigenetic modifications that drive the transformation of normal cells into malignant ones. Key mechanisms include:
Oncogenes and tumor suppressor genes: Oncogenes are mutated or overexpressed versions of normal genes (proto-oncogenes) that promote cell proliferation and survival. Examples include MYC, RAS, and HER2.
Tumor suppressor genes, such as TP53, RB1, and BRCA1/2, normally inhibit cell growth and promote apoptosis. Loss-of-function mutations in these genes remove critical growth restraints.
Genomic instability: Cancer cells often exhibit high levels of genomic instability, resulting in an increased mutation rate. This instability can be caused by defects in DNA repair mechanisms, such as those involving BRCA1/2 or mismatch repair genes.
Epigenetic alterations: Epigenetic changes, including DNA methylation, histone modification, and non-coding RNA regulation, play a crucial role in gene expression and tumor progression. Aberrant epigenetic modifications can silence tumor suppressor genes or activate oncogenes.
Cell cycle dysregulation: Disruption of normal cell cycle control is a hallmark of cancer. Mutations in cell cycle regulators, such as Cyclin-Dependent Kinases (CDKs) and their inhibitors (e.g., p16INK4a), lead to unchecked cell division.
Apoptosis evasion: Tumor cells often evade programmed cell death (apoptosis) through alterations in apoptotic pathways. Overexpression of anti-apoptotic proteins (e.g., BCL-2) or loss of pro apoptotic factors (e.g., BAX, BAK) contributes to cell survival.
Telomere maintenance: Cancer cells maintain telomere length through the activation of telomerase or Alternative Lengthening of Telomeres (ALT) mechanisms, allowing for limitless replication potential.
Tumor microenvironment: The Tumor Microenvironment (TME) consists of a dynamic network of cancer cells, stromal cells, immune cells, Extracellular Matrix (ECM), and signaling molecules. The TME plays a crucial role in tumor progression and therapeutic resistance.
Cancer-Associated Fibroblasts (CAFs): CAFs secrete growth factors, cytokines, and ECM components that promote tumor growth, invasion, and metastasis. They also contribute to the remodeling of the ECM, facilitating cancer cell migration.
Immune cells: The immune system can both suppress and promote tumor growth. Tumor- Infiltrating Lymphocytes (TILs) may attack cancer cells, while regulatory T cells (Tregs) and Myeloid-Derived Suppressor Cells (MDSCs) can inhibit anti-tumor immune responses.
Angiogenesis: Tumors stimulate the formation of new blood vessels to supply nutrients and oxygen through the secretion of angiogenic factors like VEGF. Angiogenesis is critical for tumor growth and metastasis.
Hypoxia: Hypoxic conditions within the TME activate Hypoxia-Inducible Factors (HIFs), which regulate genes involved in angiogenesis, metabolism, and cell survival. Hypoxia contributes to therapeutic resistance.
Metastasis: Metastasis is a complex process involving the dissemination of cancer cells from the primary tumor to distant sites. Key steps include:
Epithelial-Mesenchymal Transition (EMT): EMT is a process by which epithelial cells acquire mesenchymal properties, enhancing their migratory and invasive capabilities. EMT is regulated by transcription factors such as SNAIL, SLUG, and TWIST.
Invasion and migration: Cancer cells invade surrounding tissues by degrading the ECM through the secretion of proteolytic enzymes like Matrix Metalloproteinases (MMPs). Migration is facilitated by changes in cell adhesion molecules and cytoskeletal dynamics.
Circulating Tumor Cells (CTCs): CTCs enter the bloodstream or lymphatic system, where they must survive shear stress and immune attack. They can form microemboli with platelets, aiding their survival and extravasation at distant sites.
Colonization: Successful metastasis requires the colonization of distant organs, where cancer cells must adapt to the new microenvironment and establish secondary tumors. This process is influenced by organ-specific factors and interactions with the local stroma.
Therapeutic strategies: Advancements in our understanding of tumor cell biology have led to the development of novel therapeutic strategies aimed at targeting specific mechanisms of cancer progression.
Targeted therapies: Targeted therapies are designed to inhibit specific oncogenic pathways. Examples include Tyrosine Kinase Inhibitors (TKIs) like imatinib for BCR-ABL positive chronic myeloid leukemia and HER2 inhibitors like trastuzumab for HER2 positive breast cancer.
Immunotherapy: Immunotherapies harness the body’s immune system to fight cancer. Immune checkpoint inhibitors (e.g., anti-PD-1, anti- CTLA-4) have shown remarkable efficacy in several cancers by reactivating T cells. CAR T-cell therapy, which involves engineering a patient’s T cells to target specific tumor antigens, has also achieved significant success in hematological malignancies.
Epigenetic therapies: Epigenetic drugs aim to reverse abnormal gene expression patterns in cancer cells. DNA methyltransferase inhibitors (e.g., azacitidine) and histone deacetylase inhibitors (e.g., vorinostat) are examples of epigenetic therapies approved for certain cancers.
Combination therapies: Combining different therapeutic modalities can enhance efficacy and overcome resistance. Examples include combining targeted therapies with immunotherapies or combining chemotherapy with angiogenesis inhibitors.
Precision medicine: Precision medicine tailors treatment based on the genetic and molecular profile of an individual’s tumor. Advances in genomic sequencing and biomarker identification have enabled the selection of therapies that are most likely to be effective for specific patients.
Challenges and future directions
Despite significant progress, several challenges remain in the field of tumor cell science.
Therapeutic resistance: Resistance to therapy is a major obstacle in cancer treatment. Mechanisms of resistance include genetic mutations, activation of alternative signaling pathways, and changes in the TME. Understanding these mechanisms is essential for developing strategies to overcome resistance.
Tumor heterogeneity: Tumors are highly heterogeneous, with significant variability in genetic, epigenetic, and phenotypic characteristics within and between tumors. This heterogeneity complicates the development of effective treatments and contributes to therapeutic resistance.
Minimal Residual Disease (MRD): MRD refers to the small number of cancer cells that remain in the body after treatment and can lead to relapse. Detecting and targeting MRD is critical for achieving long-term remission.
Metastasis: Preventing and treating metastasis remains a significant challenge. Understanding the molecular mechanisms that drive metastatic spread and developing therapies that target these processes are crucial for improving patient outcomes.
Immune evasion: Tumors employ various strategies to evade immune detection and destruction. Developing therapies that can overcome immune evasion and enhance antitumor immunity is a key area of research.
Future directions in tumor cell science include the development of more effective and less toxic therapies, leveraging advances in genomics and proteomics to identify new therapeutic targets, and improving our understanding of the interactions between tumor cells and the TME. Additionally, advancements in singlecell sequencing and spatial transcriptomics will provide deeper insights into tumor heterogeneity and the spatial organization of tumors, informing the development of more precise and effective treatments.
Conclusion
Tumor cell biology is a complex and dynamic field that continues to evolve rapidly. Advances in our understanding of the mechanisms underlying tumorigenesis, the interactions between tumor cells and their microenvironment, and the processes driving metastasis have led to the development of innovative therapeutic strategies. Despite the challenges, ongoing research and technological advancements hold promise for improving the diagnosis, treatment, and outcomes for patients with cancer. As we continue to unravel the intricacies of tumor cell science, the potential for developing more effective and personalized cancer therapies becomes increasingly attainable.