Review Article - Clinical Investigation (2025) Volume 15, Issue 1
The stem cell of origin and resurrection
- Corresponding Author:
- Borayek Saad
Department of Medicine, Assiut University, Assiut, Egypt
E-mail: abojo920@gmail.com
Received: 03-May-2024, Manuscript No. FMCI-24-133948; Editor assigned: 06-May-2024, PreQC No. FMCI-24-133948 (PQ); Reviewed: 20-May-2024, QC No. FMCI-24-133948; Revised: 03-Feb-2025, Manuscript No. FMCI-24-133948 (R); Published: 10-Feb-2025, DOI: 10.37532/2041-6792.2025.15(1).601-607
Abstract
Stem cell is the “mother cell” that has the potential to differentiate to any type of tissue or organ. This cell is present in the newly formed embryo in the tail bone (coccygeal bone). The whole organs develop as a result of differentiation of this stem cell to different lines of tissues: ectoderm, endoderm, mesoderm. In addition, there are different researches all over the world to extract this stem cell from the patient body and direct it invivo to develop to a tissue or an organ that will be “transplanted to the patient.
Keyword
Induced pluripotent stem cells • Hematopoietic stem cells • Embryonic stem cells • Wisconsin Alumni Research Foundation
Introduction
The Prophet said, “All of the Sons of Adam (men) will decay except for the bone of coccyx (tailbone).
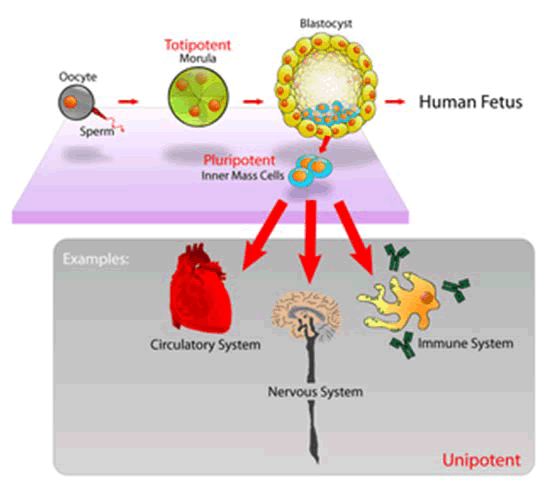
From it he (man) was created and by it he will be reconstructed”. Found in the Two Sahihs (Bukhari and Muslim) it is narrated by way of Al-A`mash from Abu Salih, from Abu Hurayrah (Figure1).
Figure 1: The origin and resurrection of stem.
Modern day science discovered in 1931
The tailbone (coccyx) is the last bone at the end of your spine.
• It is the only part of the body that does not decompose and cannot be destroyed. It cannot be finished even by burning under high temperature.
• The first things to form inside the fertilized egg are the “primitive streak” and “node” (around 15 days later) from which all of the body of the baby originates and cells begin to form. Both of these later turn into the “tailbone”.
• The tailbone contains mother cells for the body.
• The first western scientist to discover the secret of the tailbone was a German named Hans Spemann based at the University of Freiburg im Breisgau, Germany. He called the primitive streak and node the “primary organizer” which clearly suggests that the tailbone was the basic place of origin of the human.
• After many experiments, he concluded that there was nothing that influenced the primary organizer and it could not be destroyed.
• Hans Spemann was awarded the “Noble Prize” in 1935 for this discovery.
Today, WARNEK (an organization responsible for ethical research on human fertilization and genetics) prohibits scientists to conduct experiments on fertilized eggs in which the primitive streak has already been formed. This shows the importance of the streak.
Now think, when Prophet Muhammad’s information about the tailbone has been discovered by modern science, that it is where the human body is created from and that it will not be destroyed until every person shall be resurrected and reformed from it, his news that we shall be raised in another world from this tailbone shall also become true so do not neglect this fact. Peace be upon our Master Muhammad, the final and truthful messenger of Allah Almighty who informed of us this news of the unseen many hundred years ago!
In Arabic this bone is called “Ajbuz-Zanab”. In mammals, roughly 50 to 150 cells make up the inner cell mass during the blastocyst stage of embryonic development, around days 5-14. These have stem-cell capability. In vivo, they eventually differentiate into all of the body’s cell types (making them pluripotent). This process starts with the differentiation into the three germ layers–the ectoderm, mesoderm and endoderm–at the gastrulation stage. However, when they are isolated and cultured in vitro, they can be kept in the stem-cell stage and are known as Embryonic Stem Cells (ESCs).
Literature Review
Adult stem cells are found in a few select locations in the body, known as niches, such as those in the bone marrow or gonads. They exist to replenish rapidly lost cell types and are multipotent or unipotent, meaning they only differentiate into a few cell types or one type of cell. In mammals, they include, among others, hematopoietic stem cells, which replenish blood and immune cells, basal cells, which maintain the skin epithelium, and mesenchymal stem cells, which maintain bone, cartilage, muscle and fat cells. Adult stem cells are a small minority of cells; they are vastly outnumbered by the progenitor cells and terminally differentiated cells that they differentiate into [1].
Research into stem cells grew out of findings by Canadian biologists Ernest McCulloch, James till and Andrew J. Becker at the University of Toronto and the Ontario Cancer Institute in the 1960’s [2,3]. As of 2016, the only established medical therapy using stem cells is hematopoietic stem cell transplantation [4]. first performed in 1958 by French oncologist Georges Mathé. Since 1998 however, it has been possible to culture and differentiate human embryonic stem cells (in stem-cell lines). The process of isolating these cells has been controversial, because it typically results in the destruction of the embryo. Sources for isolating ESCs have been restricted in some European countries and Canada, but others such as the UK and China have promoted the research [5]. Somatic cell nuclear transfer is a cloning method that can be used to create a cloned embryo for the use of its embryonic stem cells in stem cell therapy [6]. In 2006, a Japanese team led by Shinya Yamanaka discovered a method to convert mature body cells back into stem cells. These were termed induced Pluripotent Stem Cells (iPSCs) [7].
The classical definition of a stem cell requires that it possesses two properties:
Self-renewal: The ability to go through numerous cycles of cell growth and cell division, known as cell proliferation, while maintaining the undifferentiated state.
Potency: The capacity to differentiate into specialized cell types. In the strictest sense, this requires stem cells to be either totipotent or pluripotent to be able to give rise to any mature cell type, although multipotent or unipotent progenitor cells are sometimes referred to as stem cells. Apart from this, it is said that stem cell function is regulated in a feedback mechanism.
Self-renewal
Two mechanisms ensure that a stem cell population is maintained (doesn’t shrink in size).
Asymmetric cell division: A stem cell divides into one mother cell, which is identical to the original stem cell and another daughter cell, which is differentiated.
When a stem cell self-renews, it divides and does not disrupt the undifferentiated state. This self-renewal demands control of cell cycle as well as upkeep of multipotency or pluripotency, which all depends on the stem cell [8-13].
Stochastic differentiation: when one stem cell grows and divides into two differentiated daughter cells, another stem cell undergoes mitosis and produces two stem cells identical to the original.
Stem cells use telomerase, a protein that restores telomeres, to protect their DNA and extend their cell division limit (the Hayflick limit) [14].
Potency specifies the differentiation potential (the potential to differentiate into different cell types) of the stem cell [15]. Totipotent (also known as omnipotent) stem cells can differentiate into embryonic and extraembryonic cell types. Such cells can construct a complete, viable organism [15]. These cells are produced from the fusion of an egg and sperm cell. Cells produced by the first few divisions of the fertilized egg are also totipotent.
Pluripotent stem cells are the descendants of totipotent cells and can differentiate into nearly all cells i.e., cells derived from any of the three germ layers.
Multipotent stem cells can differentiate into a number of cell types, but only those of a closely related family of cells. Oligopotent stem cells can differentiate into only a few cell types, such as lymphoid or myeloid stem cells. Unipotent cells can produce only one cell type, their own, but have the property of selfrenewal, which distinguishes them from non-stem cells identification.
In practice, stem cells are identified by whether they can regenerate tissue. For example, the defining test for bone marrow or Hematopoietic Stem Cells (HSCs) is the ability to transplant the cells and save an individual without HSCs. This demonstrates that the cells can produce new blood cells over a long term. It should also be possible to isolate stem cells from the transplanted individual, which can themselves be transplanted into another individual without HSCs, demonstrating that the stem cell was able to self-renew.
Properties of stem cells can be illustrated in vitro, using methods such as clonogenic assays, in which single cells are assessed for their ability to differentiate and self-renew. Stem cells can also be isolated by their possession of a distinctive set of cell surface markers. However, in vitro culture conditions can alter the behavior of cells, making it unclear whether the cells shall behave in a similar manner in vivo. There is considerable debate as to whether some proposed adult cell populations are truly stem cells.
Embryonic Stem Cells (ESCs) are the cells of the inner cell mass of a blastocyst, formed prior to implantation in the uterus. In human embryonic development the blastocyst stage is reached 4–5 days after fertilization, at which time it consists of 50–150 cells. ESCs are pluripotent and give rise during development to all derivatives of the three germ layers: Ectoderm, endoderm and mesoderm. In other words, they can develop into each of the more than 200 cell types of the adult body when given sufficient and necessary stimulation for a specific cell type. They do not contribute to the extraembryonic membranes or to the placenta.
During embryonic development the cells of the inner cell mass continuously divide and become more specialized. For example, a portion of the ectoderm in the dorsal part of the embryo specializes as ‘neurectoderm’, which will become the future central nervous system. Later in development, neurulation causes the neurectoderm to form the neural tube. At the neural tube stage, the anterior portion undergoes encephalization to generate or ‘pattern’ the basic form of the brain. At this stage of development, the principal cell type of the CNS is considered a neural stem cell.
The neural stem cells self-renew and at some point transition into Radial Glial Progenitor Cells (RGPs). Early-formed RGPs self-renew by symmetrical division to form a reservoir group of progenitor cells. These cells transition to a neurogenic state and start to divide asymmetrically to produce a large diversity of many different neuron types, each with unique gene expression, morphological and functional characteristics. The process of generating neurons from radial glial cells is called neurogenesis. The radial glial cell, has a distinctive bipolar morphology with highly elongated processes spanning the thickness of the neural tube wall. It shares some glial characteristics, most notably the expression of Glial Fibrillary Acidic Protein (GFAP). The radial glial cell is the primary neural stem cell of the developing vertebrate CNS, and its cell body resides in the ventricular zone, adjacent to the developing ventricular system. Neural stem cells are committed to the neuronal lineages (neurons, astrocytes and oligodendrocytes) and thus their potency is restricted.
Nearly all research to date has made use of mouse Embryonic Stem Cells (mES) or human Embryonic Stem Cells (hES) derived from the early inner cell mass. Both have the essential stem cell characteristics, yet they require very different environments in order to maintain an undifferentiated state. Mouse ES cells are grown on a layer of gelatin as an extracellular matrix (for support) and require the presence of Leukemia Inhibitory Factor (LIF) in serum media. A drug cocktail containing inhibitors to GSK3B and the MAPK/ERK pathway, called 2i, has also been shown to maintain pluripotency in stem cell culture. Human ESCs are grown on a feeder layer of mouse embryonic fibroblasts and require the presence of basic fibroblast growth factor (bFGF or FGF-2). Without optimal culture conditions or genetic manipulation, embryonic stem cells will rapidly differentiate.
A human embryonic stem cell is also defined by the expression of several transcription factors and cell surface proteins. The transcription factors Oct-4, Nanog, and Sox2 form the core regulatory network that ensures the suppression of genes that lead to differentiation and the maintenance of pluripotency. The cell surface antigens most commonly used to identify hES cells are the glycolipids stage specific embryonic antigen 3 and 4 and the keratan sulfate antigens Tra-1-60 and Tra-1-81. The molecular definition of a stem cell includes many more proteins and continues to be a topic of research.
By using human embryonic stem cells to produce specialized cells like nerve cells or heart cells in the lab, scientists can gain access to adult human cells without taking tissue from patients. They can then study these specialized adult cells in detail to try to discern complications of diseases or to study cell reactions to proposed new drugs.
Because of their combined abilities of unlimited expansion and pluripotency, embryonic stem cells remain a theoretically potential source for regenerative medicine and tissue replacement after injury or disease. However, there are currently no approved treatments using ES cells. The first human trial was approved by the US Food and Drug Administration in January 2009. However, the human trial was not initiated until October 13, 2010 in Atlanta for spinal cord injury research. On November 14, 2011 the company conducting the trial (Geron Corporation) announced that it will discontinue further development of its stem cell programs. Differentiating ES cells into usable cells while avoiding transplant rejection are just a few of the hurdles that embryonic stem cell researchers still face. Embryonic stem cells, being pluripotent, require specific signals for correct differentiation if injected directly into another body, ES cells will differentiate into many different types of cells, causing a teratoma. Ethical considerations regarding the use of unborn human tissue are another reason for the lack of approved treatments using embryonic stem cells. Many nations currently have moratoria or limitations on either human ES cell research or the production of new human ES cell lines.
Mesenchymal Stem Cells (MSC) or mesenchymal stromal cells, also known as medicinal signaling cells are known to be multipotent, which can be found in adult tissues, for example, in the muscle, liver, bone marrow and adipose tissue. Mesenchymal stem cells usually function as structural support in various organs as mentioned above, and control the movement of substances. MSC can differentiate into numerous cell categories as an illustration of adipocytes, osteocytes, and chondrocytes, derived by the mesodermal layer. Where the mesoderm layer provides an increase to the body’s skeletal elements, such as relating to the cartilage or bone. The term “meso” means middle, infusion originated from the Greek, signifying that mesenchymal cells are able to range and travel in early embryonic growth among the ectodermal and endodermal layers. This mechanism helps with space-filling thus, key for repairing wounds in adult organisms that have to do with mesenchymal cells in the dermis (skin), bone or muscle.
Mesenchymal stem cells are known to be essential for regenerative medicine. They are broadly studied in clinical trials. Since they are easily isolated and obtain high yield, high plasticity, which makes able to facilitate inflammation and encourage cell growth, cell differentiation and restoring tissue derived from immunomodulation and immunosuppression. MSC comes from the bone marrow, which requires an aggressive procedure when it comes to isolating the quantity and quality of the isolated cell, and it varies by how old the donor. When comparing the rates of MSC in the bone marrow aspirates and bone marrow stroma, the aspirates tend to have lower rates of MSC than the stroma. MSC are known to be heterogeneous and they express a high level of pluripotent markers when compared to other types of stem cells, such as embryonic stem cells. MSCs injection leads to wound healing primarily through stimulation of angiogenesis.
Cell cycle control
Further information: Cell cycle
Embryonic Stem Cells (ESCs) have the ability to divide indefinitely while keeping their pluripotency, which is made possible through specialized mechanisms of cell cycle control. Compared to proliferating somatic cells, ESCs have unique cell cycle characteristics such as rapid cell division caused by shortened G1 phase, absent G0 phase, and modifications in cell cycle checkpoints which leaves the cells mostly in S phase at any given time. ESCs’ rapid division is demonstrated by their short doubling time, which ranges from 8 to 10 hours, whereas somatic cells have doubling time of approximately 20 hours or longer. As cells differentiate, these properties change: G1 and G2 phases lengthen, leading to longer cell division cycles. This suggests that a specific cell cycle structure may contribute to the establishment of pluripotency.
Discussion
Particularly because G1 phase is the phase in which cells have increased sensitivity to differentiation, shortened G1 is one of the key characteristics of ESCs and plays an important role in maintaining undifferentiated phenotype. Although the exact molecular mechanism remains only partially understood, several studies have shown insight on how ESCs progress through G1 and potentially other phases so rapidly.
The cell cycle is regulated by complex network of cyclins, Cyclin-dependent kinases (Cdk), Cyclindependent kinase inhibitors (Cdkn), Pocket Proteins of the Retinoblastoma (Rb) family, and other accessory factors. Foundational insight into the distinctive regulation of ESC cell cycle was gained by studies on mouse ESCs (mESCs). mESCs showed a cell cycle with highly abbreviated G1 phase, which enabled cells to rapidly alternate between M phase and S phase. In a somatic cell cycle, oscillatory activity of Cyclin-Cdk complexes is observed in sequential action, which controls crucial regulators of the cell cycle to induce unidirectional transitions between phases: Cyclin D and Cdk4/6 are active in the G1 phase, while Cyclin E and Cdk2 are active during the late G1 phase and S phase; and Cyclin A and Cdk2 are active in the S phase and G2, while Cyclin B and Cdk1 are active in G2 and M phase. However, in mESCs, this typically ordered and oscillatory activity of Cyclin-Cdk complexes is absent. Rather, the Cyclin E/Cdk2 complex is constitutively active throughout the cycle, keeping Retinoblastoma protein (pRb) hyperphosphorylated and thus inactive. This allows for direct transition from M phase to the late G1 phase, leading to absence of D-type cyclins and therefore a shortened G1 phase. Cdk2 activity is crucial for both cell cycle regulation and cell-fate decisions in mESCs; downregulation of Cdk2 activity prolongs G1 phase progression, establishes a somatic cell-like cell cycle, and induces expression of differentiation markers.
In human ESCs (hESCs), the duration of G1 is dramatically shortened. This has been attributed to high mRNA levels of G1-related Cyclin D2 and Cdk4 genes and low levels of cell cycle regulatory proteins that inhibit cell cycle progression at G1, such as p21CipP1, p27Kip1 and p57Kip2. Furthermore, regulators of Cdk4 and Cdk6 activity, such as members of the Ink family of inhibitors (p15, p16, p18 and p19), are expressed at low levels or not at all. Thus, similar to mESCs, hESCs show high Cdk activity, with Cdk2 exhibiting the highest kinase activity. Also similar to mESCs, hESCs demonstrate the importance of Cdk2 in G1 phase regulation by showing that G1 to S transition is delayed when Cdk2 activity is inhibited and G1 is arrest when Cdk2 is knocked down. However unlike mESCs, hESCs have a functional G1 phase. hESCs show that the activities of Cyclin E/Cdk2 and Cyclin A/Cdk2 complexes are cell cycle-dependent and the Rb checkpoint in G1 is functional.
ESCs are also characterized by G1 checkpoint nonfunctionality, even though the G1 checkpoint is crucial for maintaining genomic stability. In response to DNA damage, ESCs do not stop in G1 to repair DNA damages but instead, depend on S and G2/M checkpoints or undergo apoptosis. The absence of G1 checkpoint in ESCs allows for the removal of cells with damaged DNA, hence avoiding potential mutations from inaccurate DNA repair. Consistent with this idea, ESCs are hypersensitive to DNA damage to minimize mutations passed onto the next generation.
Some of the fundamental patents covering human embryonic stem cells are owned by the Wisconsin Alumni Research Foundation (WARF)–they are patents 5,843,780, 6,200,806, and 7,029,913 invented by James A. Thomson. WARF does not enforce these patents against academic scientists, but does enforce them against companies.
In 2006, a request for the US Patent and Trademark Office (USPTO) to re-examine the three patents was filed by the Public Patent Foundation on behalf of its client, the non-profit patent-watchdog group Consumer Watchdog (formerly the Foundation for Taxpayer and Consumer Rights). In the reexamination process, which involves several rounds of discussion between the USPTO and the parties, the USPTO initially agreed with Consumer Watchdog and rejected all the claims in all three patents, however in response, WARF amended the claims of all three patents to make them more narrow, and in 2008 the USPTO found the amended claims in all three patents to be patentable. The decision on one of the patents (7,029,913) was appealable, while the decisions on the other two were not. Consumer Watchdog appealed the granting of the 913 patent to the USPTO’s Board of Patent Appeals and Interferences (BPAI) which granted the appeal, and in 2010 the BPAI decided that the amended claims of the 913 patent were not patentable. However, WARF was able to re-open prosecution of the case and did so, amending the claims of the 913 patent again to make them more narrow, and in January 2013 the amended claims were allowed.
In July 2013, Consumer Watchdog announced that it would appeal the decision to allow the claims of the 913 patent to the US Court of Appeals for the Federal Circuit (CAFC), the federal appeals court that hears patent cases. At a hearing in December 2013, the CAFC raised the question of whether Consumer Watchdog had legal standing to appeal; the case could not proceed until that issue was resolved.
Diseases and conditions where stem cell treatment is being investigated include.
• Diabetes
• Androgenic alopecia and hair loss
• Rheumatoid arthritis
• Parkinson’s disease
• Alzheimer’s disease
• Respiratory disease
• Osteoarthritis
• Stroke and traumatic brain injury repair
• Learning disability due to congenital disorder
• Spinal cord injury repair
• Heart infarction
• Anti-cancer treatments
• Baldness reversal
• Replace missing teeth
• Repair hearing
• Restore vision and repair damage to the cornea
• Amyotrophic lateral sclerosis
• Crohn’s disease
• Wound healing
Male infertility due to absence of spermatogonial stem cells. In recent studies, scientists have found a way to solve this problem by reprogramming a cell and turning it into a spermatozoon. Other studies have proven the restoration of spermatogenesis by introducing human iPSC cells in mice testicles. This could mean the end of azoospermia.
Female infertility: Oocytes made from embryonic stem cells. Scientists have found the ovarian stem cells, a rare type of cells (0.014%) found in the ovary. They could be used as a treatment not only for infertility, but also for premature ovarian insufficiency.
Critical limb Ischemia
Research is underway to develop various sources for stem cells and to apply stem cell treatments for neurodegenerative diseases and conditions, diabetes, heart disease and other conditions. Research is also underway in generating organoids using stem cells, which would allow for further understanding of human development, organogenesis and modeling of human diseases.
Conclusion
In more recent years, with the ability of scientists to isolate and culture embryonic stem cells, and with scientists’ growing ability to create stem cells using somatic cell nuclear transfer and techniques to create induced pluripotent stem cells, controversy has crept in, both related to abortion politics and to human cloning.
Hepatotoxicity and drug-induced liver injury account for a substantial number of failures of new drugs in development and market withdrawal, highlighting the need for screening assays such as stem cell-derived hepatocyte-like cells, that are capable of detecting toxicity early in the drug development process.
References
- Becker Andrew J, Ernest A. McCulloch, James E till. Cytological demonstration of the clonal nature of spleen colonies derived from transplanted mouse marrow cells. Nature. 197:452-454 (1963).
[Crossref] [Google Scholar] [PubMed]
- Siminovitch L, McCulloch EA, Till JE. The distribution of colony-forming cells among spleen colonies. J Cell Comp Physiol. 327-336 (1963).
[Crossref] [Google Scholar] [PubMed]
- Müller AM, Huppertz S, Henschler R. Hematopoietic stem cells in regenerative medicine: Astray or on the path?. Transfus Med Hemother. 43:247-254 (2016).
[Crossref] [Google Scholar] [PubMed]
- Choate B, Paz R. Stem cells and society. Stem Cells. 26 (2011).
- Tuch BE. Stem cells: A clinical update. Aust Fam Phys 35:719-721 (2006).
[Google Scholar] [PubMed]
- Ramalho-Santos M, Willenbring H. On the origin of the term “stem cell”. Cell Stem Cell. 1:35-38 (2007).
[Google Scholar] [PubMed]
- Mahla RS. Stem cells applications in regenerative medicine and disease therapeutics. Int J Cell Biol. 6940283 (2016).
[Crossref] [Google Scholar] [PubMed]
- Winslow R, Mundy A. First embryonic stem-cell trial gets approval from the FDA. Wall Street J. 23:23-41 (2009).
- Wu DC, Boyd AS, Wood KJ. Embryonic stem cell transplantation: Potential applicability in cell replacement therapy and regenerative medicine. Front Biosci. 12:4525-4535 (2007).
[Crossref] [Google Scholar] [PubMed]
- Zomer HD, Vidane AS, Goncalves NN, et al. Mesenchymal and induced pluripotent stem cells: general insights and clinical perspectives. Stem Cells Cloning. 125-134 (2015).
[Crossref] [Google Scholar] [PubMed]
- Caplan AI. Mesenchymal stem cells. J Orthop Res. 9:641-650 (1991).
[Crossref] [Google Scholar] [PubMed]
- Krasilnikova OA, Baranovskii DS, Lyundup AV, et al. Stem and somatic cell monotherapy for the treatment of diabetic foot ulcers: Review of clinical studies and mechanisms of action. Stem Cell Rev Rep. 18:1974-1985 (2022).
[Crossref] [Google Scholar] [PubMed]
- Koledova Z, Krämer A, Kafkova LR, et al. Cell-cycle regulation in embryonic stem cells: Centrosomal decisions on self-renewal. Stem Cells Dev. 19:1663-1678 (2010).
[Crossref] [Google Scholar] [PubMed]
- Barta T, Dolezalova D, Holubcova Z, et al. Cell cycle regulation in human embryonic stem cells: Links to adaptation to cell culture. Exp Biol Med. 23:271-275 (2013).
[Crossref] [Google Scholar] [PubMed]
- Zaveri L, Dhawan J. Cycling to meet fate: Connecting pluripotency to the cell cycle. Front Cell Dev Biol. 6:57 (2018)
[Crossref] [Google Scholar] [PubMed]