Research Article - International Journal of Clinical Rheumatology (2021) Volume 16, Issue 2
Selective serotonin reuptake inhibitors and serotonin norepinephrine reuptake inhibitors: Impact on trabecular bone score and bone mineral density in primary fibromyalgia
- *Corresponding Author:
- Muhammad M Harb
Department of Physical Medicine, Rheumatology and Rehabilitation, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
E-mail: Dr_2MH@Yahoo.com
Abstract
Background: Fibromyalgia is a chronic musculoskeletal pain disorder characterized by widespread pain at multiple tender points, sleep disturbance and fatigue, which subsequently affect quality of life.The aim of our study is to determine the correlation between consumption of SSRIs and SNRIs in patients with primary fibromyalgia, and BMD and TBS.
Methods and Findings: A cross-sectional study carried out on 150 Egyptian participants. Patients were divided into 2 main groups: treatment group including 100 patients (50 on SSRI, and 50 on SNRI) diagnosed with primary myelofibrosis, and control group including 50 age-matched subjects (25 healthy individual, and 25 with primary myelofibrosis but receiving medications other than SSRI and SNRI).BMD and TBS were significantly low in SSRI and SNRI treatment groups compared to healthy control. In older population, lumbar spine (L1-L4) BMD and TBS decreased significantly in SSRI group. Also, control patients with primary fibromyalgia showed low BMD.
Conclusion: Our study showed that patients with primary myelofibrosis, especially old population, whose treatment involved SSRIs or SNRIs had low BMD and low TBS. Additionally, patients with primary fibromyalgia who neither received SSRI nor SNRI also experienced low BMD. Thus, primary myelofibrosis could be considered as a contributing factor for low BMD.
Keywords
fibromyalgia • SSRI • SNRI • BMD • TBS • osteoporosis
Introduction
Fibromyalgia is a chronic musculoskeletal pain disorder and its underling etiology remains unclear. It is characterized by several clinical manifestations including widespread pain at multiple tender points; sleep disturbance and fatigue, which subsequently affect quality of life. Previous studies revealed that patients with fibromyalgia may experience some psychiatric disorders such as anxiety and depression. Hence, antidepressants are considered to alleviatesymptomsassociated with fibromyalgia [1-3].
Reduction in physical activity and impaired ambulation in patients with fibromyalgia will limit their exposure to sunlight. This put them at high risk of developing osteoporosis [4,5], a disease characterized by reduction of bone mass and alteration of bone microarchitecture due to low Bone Mineral Density (BMD) [6,7].
BMD is assessed by usingdual X-ray absorptiometry(DXA) to detect possibility of fracture, and expressed as T-score. Based on obtained T-scores, bone density could be classified accordingly to: normal (T-score >1), osteopenia (T-score between -1 and -2.5), and osteoporosis (T-score <-2.5). However, BMD does not provide information about bone quality and strength of bone microarchitecture[7,8].
Trabecular bone score (TBS) is a novel gray-level texture parameter that can be calculated from 2D DXA images. It is considered an effective noninvasive measurement of bonemicroarchitecture applied by quantifying variation in grey-level texture from one pixel to the next, given that high TBS values indicate strong bone microarchitecture, and low values reflectweak bone microarchitecture [9,10].
Two classes of antidepressants have been used for modulation of pain accompanied with fibromyalgia, Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin and Norepinephrine Reuptake Inhibitors (SNRIs)[3]. Despite being effective, studies showed that they are associated with increased risk of fracture and reduced BMD [11,12].
Our study aims to determine the correlation between consumption of SSRIs and SNRIs in patients with primary fibromyalgia, and BMD and TBS.
Methods
Study design
A cross-sectional study was carried out on 150 Egyptian participants recruited from Rheumatology, Physical Medicine and Rehabilitation Department at Al-Hussein and Sayed Galal, Al-Azhar University Hospitals. The study was conducted from June 2018 to December 2018.
Patients were allocated into two main groups. Firstly, treatment group involving 100 patients diagnosed with primary fibromyalgia, which was further subdivided into 2 groups based on type of medication patients had received to 50 patients on SSRIs, and 50 patients on SNRIs.Secondly,control group which included 50 participants, also subdivided into 2 groups each with 25 patients diagnosed with primary fibromyalgia whose prior treatment regimen did not involve SSRIs or SNRIs, and 25 healthy individuals selected by nurses and medical staff.
The study was approved by the medical ethics committee at Al-Azhar University, and informed consent forms were obtained from all participants.
Inclusion and exclusion criteria
Patients were included in treatment group if they met the 2010 ACR diagnostic criteria for fibromyalgia, and if their prior treatment regimen was based on SSRIs or SNRIs at least for 6 months. The 2010 ACR diagnostic criteria for fibromyalgia are[13]:
• Widespread pain index (WPI) ≥7 and symptom severity (SS) scale score ≥5, or WPI ≥3-6 and SS scale score ≥9.
• Symptoms have been present at a similar level for at least 3 months.
• Patient does not have a disorder that would otherwise explain the pain.
On the other hand, patients were excluded if they were younger than 30 or older than 65 years of age, and if they were suffering from one of the collagen diseases (Rheumatoid Arthritis (RA), Systemic Lupus Erythematosus(SLE), Systemic Sclerosis (SS), Mixed Connective Tissue Disease (MCTD), or others), systemic disease, chronic obstructive pulmonary disease associated with asthma or inflammatory bowel disease, or autoimmune diseases such as autoimmune hepatitis and celiac disease. Being alcoholic, addicting to drugs, or on a corticosteroid regimen for more than 6 months in addition to a history of traumatic vertebral fractures were also among the exclusion criteria. Pregnant and lactating women were excluded as well.
Medical history and examination
Before running our study, full medical history was obtained from all eligible participants. This includes family, past, and present history of any underlying condition. All items considered during taking full medical history of patients are enumerated in the appendix.
General examinationshave been performed for all patients, this included scalp, eye, skin, cardiac, chest, abdominal, and neuropsychiatric examinations. Additionally, joint examination was performed (skin discoloration, muscle wasting, deformities, swelling either generalized or localized, hotness, tenderness, active and passive movement).
Moreover, the following laboratory findings have been investigated for all participants including: Complete Blood Count (CBC), C-Reactive Protein(CRP), Erythrocyte Sedimentation Rate (ESR), liver and kidney function tests, blood glucose level, and autoimmune profile. Devices and methods that were used to test the above are detailed in the appendix.
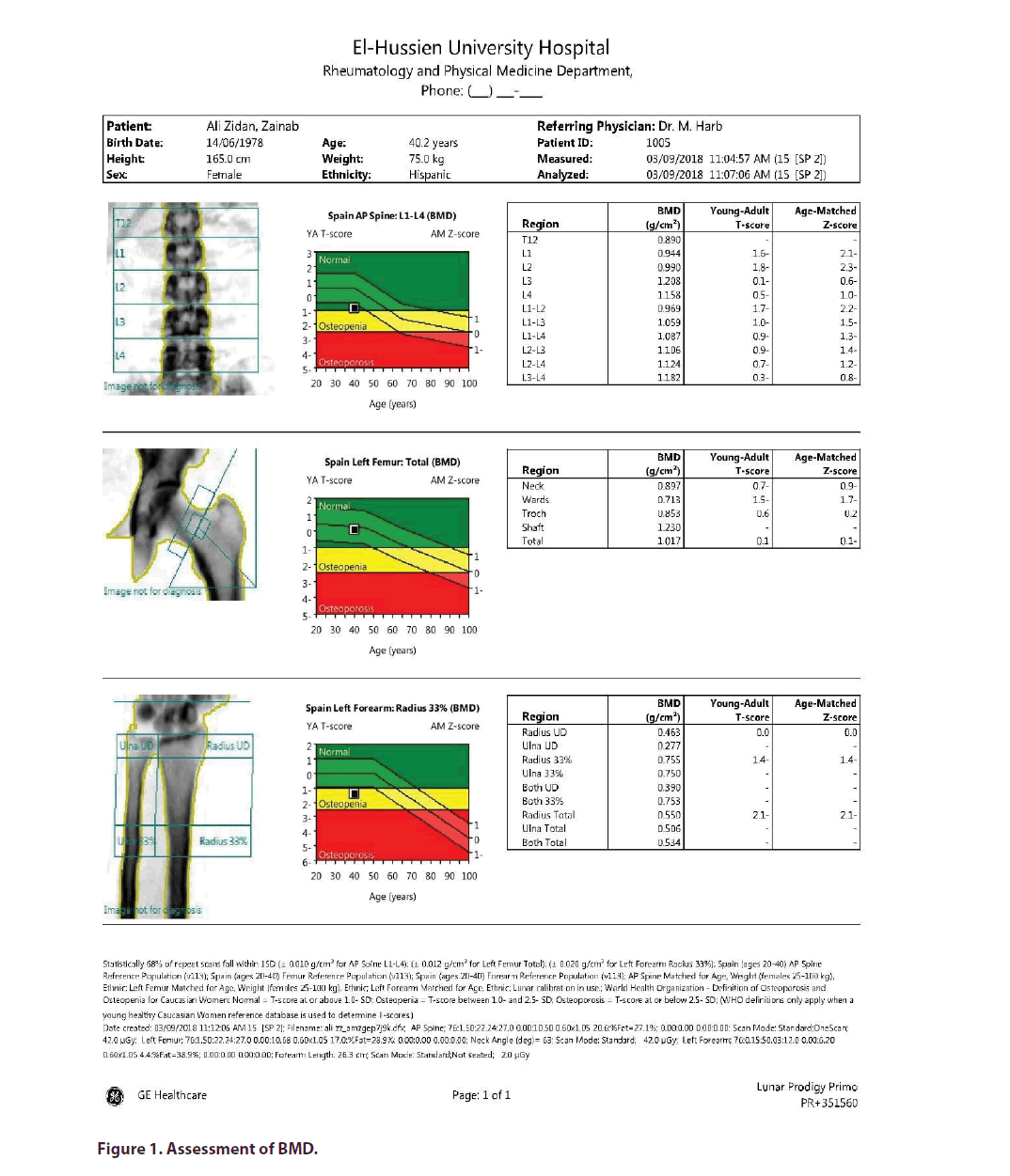
Assessment of BMD
For all participants, lumbar spine, left proximal femur and left distal forearm had been assessed for BMD by using DXA [Brand: GE-Lunar, Model: Prodigy Primo. Madison, WI, USA. SN: 35156] to predict probability of fractures (Figure 1).
With a BMD T-score ranging from more -1 to lower than -2.5, the World Health Organization (WHO) has establishedthe diagnostic criteria for osteoporosis. T-score represents how far the BMD Standard Deviation (SD) is away from the mean of a healthy individual [7].
For measurement of BMD using DXA, patientswere laidin a supine position on the imaging table. During lumbar spine imaging, the patient’s legs were raised by an angle of 90 degrees on a support. For measurement of the left forearm, left arm was supported and directed on the imaging table while the patient was setting beside it. During hip imaging, legs were left straight, feet were fixed and the direction of the measured leg was set at an angle of 30 degrees with an inward rotation [14].
Assessment of TBS
TBS had been measured for lumbar spine using iNsight® software [version 2.0, Med-Imaps, installed on GE Lunar: Prodigy].For the same spinal region, TBS was calculated by analyzing BMD images obtained during DXA scan, using iNsight® software uploaded into bone densitometer (Figure 2). The resultant trabeculographyprovided local TBS values of lumbar spine(L1-L4), taking into consideration that TBS is categorized as normal (≥ 1.350), partially degraded (between 1.200 and 1.350), and degraded (≤ 1.200) [15].
Statistical analysis
Data were statistically analyzed using Statistical Package for Social Science (SPSS) version 20.0 [Inc., Chicago, Illinois, USA]. Numerical data were expressed as mean ± SD, while categorical data were expressed as frequency and percentages. The following tests were used for analysis: one-way analysis of variance (ANOVA) was used during comparison between more than 2 means, while independent t-test was used to compare between 2 means. Also, Least Significant Difference (LSD) test, Chi-square (x2) test, and Pearson’s correlation coefficient (r) test were used for multiple comparison between different variables, comparing between categorical values, and determining level of association between 2 sets of variables, respectively. The Confidence Interval (CI) was set to 95%, and p values were considered significant (<0.05), highly significant (<0.001), or insignificant (>0.05).
Results
Demographic characteristics of all 150 subjects involved in our study are illustrated in (Table 1). Subjects’ ages ranged from 30 to 60 years and each of the 4 subgroups had almost half of its subjects younger than 45 years, and the other half older than 45 years. RegardingBody Mass Index (BMI), the majority of subjects were generally obese across all subgroups. There were no statistically significant differences found for any of the demographic characteristics (age, height, weight, BMI, and obesity) among all subgroups.
| Data | SSRI (n=50) | SNRI (n=50) | Control FMS (n=25) | Healthy control (n=25) | F/x2# | p-value |
|---|---|---|---|---|---|---|
| Age (years) | ||||||
| Mean ± SD | 45.08 ± 9.49 | 45.50 ± 4.49 | 44.76 ± 9.11 | 45.12 ± 8.47 | 0.054 | 0.983 |
| Range | 30_60 | 37_55 | 30_60 | 31_60 | ||
| <45 years | 24 (48.0%) | 25 (50.0%) | 12 (48.0%) | 12 (48.0%) | ||
| ≥45 years | 26 (52.0%) | 25 (50.0%) | 13 (52.0%) | 13 (52.0%) | ||
| Height (cm) | ||||||
| Mean ± SD | 154.78 ± 8.16 | 154.71 ± 10.63 | 156.99 ± 6.24 | 158.44 ± 9.85 | 1.294 | 0.279 |
| Range | 140_190.5 | 140_190.5 | 145_170 | 122_176 | ||
| Weight (kg) | ||||||
| Mean ± SD | 77.86 ± 20.89 | 79.09 ± 23.70 | 78.54 ± 17.54 | 81.46 ± 14.53 | 0.176 | 0.913 |
| Range | 27.2_115 | 27.2_115 | 27.2_100 | 40.8_112 | ||
| BMI [wt/(ht)^2] | ||||||
| Mean ± SD | 33.03 ± 8.59 | 33.28 ± 10.14 | 31.82 ± 6.77 | 32.72 ± 6.66 | 0.17 | 0.917 |
| Range | 11.7_46.2 | 11.71_46.22 | 11.7_40.8 | 15.4_46.4 | ||
| Obesity | ||||||
| Normal | 9 (18.0%) | 11 (22.0%) | 2 (8.0%) | 2 (8.0%) | 4.200# | 0.072 |
| Overweight | 4 (8.0%) | 3 (6.0%) | 8 (32.0%) | 5 (20.0%) | ||
| Obese | 37 (74.0%) | 36 (72.0%) | 15 (60.0%) | 18 (72.0%) | ||
Table 1. Comparison between groups according to the demographic data.
Lumbar spine
With respect to anteroposterior (AP) lumbar spine BMD, it was significantly higher in healthy control group (1.21 ± 0.09) compared to SSRI group (0.99 ± 0.13), SNRI group (1.1 ± 0.15), and control group with fibromyalgia (1.06 ± 0.15) (p<0.001). Additionally, AP lumbar spine Bone Mineral Content (BMC)also was found to be significantly higher in healthy control group (60.36 ± 9.22) when compared to SSRI group (48.63 ± 9.15), SNRI group (57.94 ± 9.67), and control group with fibromyalgia (52.66 ± 10.31) (p< 0.001) (Table 2).
| SSRI (n=50) | SNRI (n=50) | Control FMS (n=25) | Healthy control (n=25) | ANOVA | p-value | |
|---|---|---|---|---|---|---|
| AP Spine L1-L4 BMD | ||||||
| Mean ± SD | 0.99 ± 0.13 | 1.10 ± 0.15a | 1.06 ± 0.15a | 1.21 ± 0.09abc | 15.477 | <0.001** |
| Range | 0.74_1.38 | 0.61_1.44 | 0.74_1.29 | 1.09_1.40 | ||
| AP Spine L1-L4 BMC | ||||||
| Mean ± SD | 48.63 ± 9.15 | 57.94 ± 9.67a | 52.66 ± 10.31 | 60.36 ± 9.22ac | 11.92 | <0.001** |
| Range | 35.00_72.15 | 33.64_80.00 | 33.76_71.48 | 46.85_79.13 | ||
Table 2. Comparison between the groups according to AP lumbar spine L1-L4 BMD and BMC.
The lumbar spine (L1-L4) T-score and Z-score of all studied groups are detailed in (Table 3). Data showed that healthy control group had the highest T-score (0.09 ± 0.73) compared to control group with fibromyalgia (-1.08 ± 1.21), SSRI group (-1.94 ± 1.04), and SNRI group (-2.31 ± 0.83) (p<0.001). Regarding the SNRI group with the lowest T-score, the percentage of patients classified as osteopenicand osteoporotic compared to SSRI group were (58% vs. 40%) and (42% vs. 42%), respectively.
| L1-L4 | SSRI (n=50) | SNRI (n=50) | Control FMS (n=25) | Healthy control (n=25) | F/x2# | p-value |
|---|---|---|---|---|---|---|
| L1-L4 T-Score | ||||||
| Mean ± SD | -1.94 ± 1.04 | -2.31 ± 0.83a | -1.08 ± 1.21ab | 0.09 ± 0.73abc | 39.542 | <0.001** |
| Range | -3.70_1.51 | -4.68_-1.12 | -3.65_0.77 | -0.84_1.64 | ||
| Normal | 9 (18.0%) | 0 (0.0%) | 14 (56.0%) | 25 (100.0%) | 88.795# | <0.001** |
| Osteopenia | 20 (40.0%) | 29 (58.0%) | 6 (24.0%) | 0 (0.0%) | ||
| Osteoporosis | 21 (42.0%) | 21 (42.0%) | 5 (20.0%) | 0 (0.0%) | ||
| L1-L4 Z-Score | ||||||
| Mean ± SD | -1.35 ± 1.07 | -0.75 ± 1.35a | -0.86 ± 1.28a | -0.02 ± 1.03abc | 6.974 | <0.001** |
| Range | -3.36_2.55 | -4.34_2.79 | -2.66_1.53 | -1.71_2.55 | ||
| Normal | 17 (34.0%) | 30 (60.0%) | 13 (52.0%) | 21 (84.0%) | 18.594# | 0.005* |
| Osteopenia | 26 (52.0%) | 15 (30.0%) | 10 (40.0%) | 4 (16.0%) | ||
| Osteoporosis | 7 (14.0%) | 5 (10.0%) | 2 (8.0%) | 0 (0.0%) | ||
Table 3. Comparison between the groups according to L1-L4 T-score and z-score.
According to data obtained in (Table 4), lumbar spine (L1-L4) TBS was significantly higher in healthy control group (1.44 ± 0.17) when compared to SSRI group (1.32 ± 0.16), SNRI group (1.28 ± 0.23), and control group with fibromyalgia (1.46 ± 0.19) (p<0.001).
| TBS L1-L4 | SSRI (n=50) | SNRI (n=50) | Control FMS (n=25) | Healthy control (n=25) | F/x2# | p-value |
|---|---|---|---|---|---|---|
| TBS L1-L4 | ||||||
| Mean ± SD | 1.32 ± 0.16 | 1.28 ± 0.23 | 1.46 ± 0.19ab | 1.44 ± 0.17ab | 7.361 | <0.001** |
| Range | 0.94_1.71 | 0.27_1.61 | 0.99_1.75 | 0.79_1.63 | ||
| TBS L1-L4 | ||||||
| Degraded | 12 (24.0%) | 11 (22.0%) | 2 (8.0%) | 1 (4.0%) | 13.678# | 0.033* |
| Partially degraded | 8 (16.0%) | 11 (22.0%) | 3 (12.0%) | 1 (4.0%) | ||
| Normal | 30 (60.0%) | 28 (56.0%) | 20 (80.0%) | 23 (92.0%) | ||
Table 4. Comparison between the groups according to TBS L1-L4.
Left femur
Both BMD and BMC of left femur were significantly higher in healthy control group (1.04 ± 0.12 and 32.63 ± 4.49) compared to SSRI group (0.89 ± 0.18 and 27.02 ± 4.44), SNRI group (0.99 ± 0.17 and 30.20 ± 5.48), and control group with fibromyalgia (0.97 ± 0.11 and 30.40 ± 4.69) (p<0.001 for both values) (Table 5).
| SSRI (n=50) | SNRI (n=50) | Control FMS (n=25) | Healthy control (n=25) | ANOVA | p-value | |
|---|---|---|---|---|---|---|
| Left Femur Total BMD | ||||||
| Mean ± SD | 0.89 ± 0.18 | 0.99 ± 0.17a | 0.97 ± 0.11a | 1.04 ± 0.12abc | 6.001 | <0.001** |
| Range | 0.49_1.78 | 0.74_1.78 | 0.75_1.14 | 0.78_1.28 | ||
| Left Femur Total BMC | ||||||
| Mean ± SD | 27.02 ± 4.44 | 30.20 ± 5.48a | 30.40 ± 4.69a | 32.63 ± 4.49abc | 8.437 | <0.001** |
| Range | 14.67_34.46 | 19.75_45.70 | 20.47_37.23 | 23.43_42.07 | ||
Table 5. Comparison between the groups according to left femur total BMD and BMC.
Total T-score and total Z-score were significantly higher in healthy control group when compared to all other groups (p<0.001 and p=0.012, respectively) (Table 6). Additionally, SSRI group was associated with the highest percentage of osteopenia (50%) and osteoporosis (4%) among all studied groups.
| SSRI (n=50) | SNRI (n=50) | Control FMS (n=25) | Healthy control (n=25) | F/x2# | p-value | |
|---|---|---|---|---|---|---|
| Left Femur Total T-Score | ||||||
| Mean ± SD | -0.90 ± 1.47 | -0.07 ± 1.43a | -0.23 ± 0.93ab | 0.32 ± 0.96abc | 5.907 | <0.001** |
| Range | -4.28_6.48 | -2.14_6.48 | -2.05_1.12 | -1.84_2.34 | ||
| Left Femur Total T-Score | ||||||
| Normal | 23 (46.0%) | 37 (74.0%) | 20 (80.0%) | 23 (92.0%) | 22.198# | <0.001** |
| Osteopenia | 25 (50.0%) | 13 (26.0%) | 5 (20.0%) | 2 (8.0%) | ||
| Osteoporosis | 2 (4.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Left Femur Total Z-Score | ||||||
| Mean ± SD | -0.88 ± 1.39 | -0.39 ± 1.41a | -0.25 ± 0.91ab | 0.10 ± 0.91abc | 3.758 | 0.012* |
| Range | -3.03_6.43 | -2.77_6.43 | -1.81_1.81 | -1.65_2.07 | ||
| Left Femur Total Z-Score | ||||||
| Normal | 25 (50.0%) | 35 (70.0%) | 19 (76.0%) | 24 (96.0%) | 17.866# | 0.007* |
| Osteopenia | 24 (48.0%) | 14 (28.0%) | 6 (24.0%) | 1 (4.0%) | ||
| Osteoporosis | 1 (2.0%) | 1 (2.0%) | 0 (0.0%) | 0 (0.0%) | ||
Table 6. Comparison between groups according to left femur total T-score and z-score.
Left forearm
Concerning left forearm total T-score, it was found to be significantly higher in healthy control group (-0.29 ± 1.18) compared to SSRI group (-1.97 ± 1.49), SNRI group (-0.89 ± 1.64), and control group with fibromyalgia (-0.95 ± 1.82) (p<0.001). Once more, SSRI group scored the highest percentage of osteoporosis (36%) among all other groups. Similarly, total Z-score was significantly higher in healthy control group as opposed to other groups (p< 0.001) (Table 7).
| SSRI (n=50) | SNRI (n=50) | Control FMS (n=25) | Healthy control (n=25) | F/x2# | p-value | |
|---|---|---|---|---|---|---|
| Left Forearm Total T-Score | ||||||
| Mean ± SD | -1.97 ± 1.49 | -0.89 ± 1.64a | -0.95 ± 1.82ab | -0.29 ± 1.18abc | 7.82 | <0.001** |
| Range | -5.57_2.01 | -5.57_3.12 | -5.19_2.37 | -2.05_1.79 | ||
| Left Forearm Total T-Score | ||||||
| Normal | 15 (30.0%) | 27 (54.0%) | 12 (48.0%) | 15 (60.0%) | 17.095 | 0.009* |
| Osteopenia | 17 (34.0%) | 15 (30.0%) | 9 (36.0%) | 10 (40.0%) | ||
| Osteoporosis | 18 (36.0%) | 8 (16.0%) | 4 (16.0%) | 0 (0.0%) | ||
| Left Forearm Total Z-Score | ||||||
| Mean ± SD | -1.65 ± 1.47 | -0.81 ± 1.63a | -0.69 ± 1.78ab | -0.13 ± 1.14abc | 6.175 | <0.001** |
| Range | -5.57_2.01 | -5.57_3.12 | -5.19_2.37 | -2.05_2.49 | ||
| Left Forearm Total Z-Score | ||||||
| Normal | 17 (34.0%) | 28 (56.0%) | 14 (56.0%) | 19 (76.0%) | 15.221 | 0.019* |
| Osteopenia | 19 (38.0%) | 14 (28.0%) | 7 (28.0%) | 6 (24.0%) | ||
| Osteoporosis | 14 (28.0%) | 8 (16.0%) | 4 (16.0%) | 0 (0.0%) | ||
Table 7. Comparison between groups according to left forearm total T-score and Z-score.
Table 8 marked the significance of age in T-score and Z-score of lumbar spine (L1-L4), left femur, and left forearm in SSRI group. Results showed that L1-L4 T-score was significantly higher in subjects <45 years of age than those ≥45 years -1.58 ± 1.08 and -2.26 ± 0.89 (p=0.018), respectively. Moreover, left forearm total T-score and total Z-score also were significantly higher in younger age subjects than those above 45 years with p values equal to 0.21 and 0.046, respectively.
| SSRI | <45 years | ≥45 years | t-test | |||
|---|---|---|---|---|---|---|
| Mean | ± SD | Mean | ± SD | t | p-value | |
| L1-L4 T-Score | -1.58 | 1.08 | -2.26 | 0.89 | 5.982 | 0.018* |
| L1-L4 Z-Score | -1.25 | 1.16 | -1.45 | 1 | 0.413 | 0.524 |
| Left Femur Total T-Score | -0.54 | 1.74 | -1.23 | 1.1 | 2.843 | 0.098 |
| Left Femur Total Z-Score | -0.62 | 1.74 | -1.12 | 0.94 | 1.636 | 0.207 |
| Left Forearm Total T-Score | -1.47 | 1.58 | -2.43 | 1.27 | 5.671 | 0.021* |
| Left Forearm Total Z-Score | -1.25 | 1.6 | -2.01 | 1.26 | 3.53 | 0.046* |
Table 8. Comparison between age <45 years versus ≥45 years according to T-score and Z-score in SSRI group.
Discussion
We examined the correlation between using SSRIs and SNRIs and low BMD and TBS among patients diagnosed with primary fibromyalgia. Our results revealed that SSRIs were associated with higher decrease in lumbar spine BMD than SNRIs, consequently, lower BMC was obtained. This wasin accordance with what had been found by Richards et al.[16].
Both SSRI and SNRI group showed reduction in spine T-score which was accompanied with weak bone microarchitecture and increased the risk of osteoporosis. This was consistent with the results of recently published study [17]. However, our data defined higher risk of osteopenia in SNRI group.Additionally, TBS decreased significantly in treatment group,which reflected fractureprone bone microarchitecture.
Left femurBMD along with T-score and Z-score were lower in treatment group compared to control, with high risk of osteopenia particularly in SSRI group. Data from meta-analysis by Rabenda et al. supported our findings [18].
Significant decline in Left forearm total T-score and total Z-score was found in treatment groups when compared to control, which was also reported in previous studies [16,19].
This work described the impact of age among SSRIs group, that a significant reduction in spine T-score and forearm total T-score was obtained. Thus, our resultssupported the negative correlation between age and increased risk of fracture [16,20].
Taking into account low femur and forearm T-score in control group with primary fibromyalgia, our study suggested fibromyalgia as predisposing factor to osteoporosis, which was confirmed in previous studies [4,5,21].
Our work provides evidence that SSRIs and SNRIs are associated with significant reduction in BMD and TBS in patients with primary fibromyalgia. This is consistent with what had been reported that these group of medications are associated with increased risk of fracture (lumbar spine, femur, forearm) and susceptibility to osteoporosis [16,18,19].
Therefore, we recommend involvement of calcium vitamin D supplements in treatment regimen of patients with fibromyalgia, particularly older population, for prophylaxis of osteoporosis. Additionally, older population should be put on another SSRI-free regimen.
Conclusion
Our study demonstrated that patients with primary myelofibrosis, especially old population, whose treatment involved SSRIs or SNRIs had low BMD and low TBS. Additionally, patients with primary fibromyalgia who neither received SSRI nor SNRI also experienced low BMD. Thus, primary myelofibrosis could be considered as a contributing factor for low BMD.
Acknowledgements
None.
Funding
This study did not receive any funding.
Competing and conflicting Interests
The authors declare no competing interest.
References
- Bellato E, Marini E, Castoldi F et al. Fibromyalgia syndrome: etiology, pathogenesis, diagnosis, and treatment. Pain. Res. Treat. 2012, 426130 (2012).
- Wolfe F, Smythe HA, Yunus MB et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis. Rheum. 33(2), 160−172 (1990).
- Lawson K. Tricyclic antidepressants and fibromyalgia: what is the mechanism of action? Expert. Opin. Investig. Drugs. 11(10), 1437−1445 (2002).
- Upala S, Yong W, Sanguankeo A. Bone mineral density is decreased in fibromyalgia syndrome: a systematic review and meta-analysis. Rheumatol. Int. 37(4), 617−622 (2016).
- Olama S, Senna M, Elarman M et al. Serum vitamin D level and bone mineral density in premenopausal Egyptian women with fibromyalgia. Rheumatol. Int. 33(1), 185−192 (2012).
- Kelly R, McDonald L, Jensen N et al. Impacts of Psychological Stress on Osteoporosis: Clinical Implications and Treatment Interactions. Front. Psychiatry. (2019).
- Akkawi I, Zmerly H. Osteoporosis: Current Concepts. Joints. 6(2), 122−127 (2018).
- Cheng P, Qi H, Di W et al. Establishment of TBS reference plots and correlation between TBS and BMD in healthy mainland Chinese women. Arch. Osteoporos. 11(5) (2016).
- Harvey NC, Glüer CC, Binkley N et al. Trabecular bone score (TBS) as a new complementary approach for osteoporosis evaluation in clinical practice. Bone. 78, 216−224 (2015).
- Hans D, Barthe N, Boutroy S et al. Correlations Between Trabecular Bone Score, Measured Using Anteroposterior Dual-Energy X-Ray Absorptiometry Acquisition, and 3-Dimensional Parameters of Bone Microarchitecture: An Experimental Study on Human Cadaver Vertebrae. J. Clin. Densitom. 14(3), 302−312 (2011).
- Haney EM, Warden SJ, Bliziotes MM. Effects of selective serotonin reuptake inhibitors on bone health in adults: time for recommendations about screening, prevention and management? Bone. 46(1), 13−17 (2010).
- Panday K, Gona A, Humphrey MB. Medication-induced osteoporosis: screening and treatment strategies. Ther. Adv. Musculoskelet. Dis. 6(5), 185−202 (2014).
- Wolfe F, Clauw DJ, Fitzcharles MA et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis. Care. Res (Hoboken). 62(5), 600−610 (2010).
- Salem D, Talaat S, Abdel-Halim MR et al. Assessment of bone mineral density by dual x-ray absorptiometry in dermatological patients treated by corticosteroids. Indian. J. Dermatol. 55(3), 238−245 (2010).
- Grigorie D, Coles D, Sucaliuc A. Trabecular Bone Score (Tbs) has a Poor Discriminative Power for Vertebral Fractures in 153 Romanian Patients with Primary Hyperparathyroidism. Acta. Endocrinol. 14(2), 208−212 (2018).
- Richards JB, Papaioannou A, Adachi JD et al. Effect of Selective Serotonin Reuptake Inhibitors on the Risk of Fracture. Arch. Intern. Med. 167(2), 188–194 (2007).
- Ak E, Bulut SD, Bulut S et al. Evaluation of the effect of selective serotonin reuptake inhibitors on bone mineral density: an observational cross-sectional study. Osteoporos. Int. 26(1), 273−279 (2015).
- Rabenda V, Nicolet D, Beaudart C et al. Relationship between use of antidepressants and risk of fractures: a meta-analysis. Osteoporos. Int. 24(1), 121−137 (2012).
- Moura C, Bernatsky S, Abrahamowicz M et al. Antidepressant use and 10-year incident fracture risk: the population-based Canadian Multicentre Osteoporosis Study (CaMoS). Osteoporos. Int. 25(5), 1473-1481 (2014).
- Haney EM, Chan BKS, Diem SJ et al. Association of Low Bone Mineral Density With Selective Serotonin Reuptake Inhibitor Use by Older Men. Arch. Intern. Med. 167(12), 1246–1251 (2007).
- Swezey RL, Adams J. Fibromyalgia: a risk factor for osteoporosis. J. Rheumatol. 26(12), 2642–2644 (1999).