Review Article - International Journal of Clinical Rheumatology (2021) Volume 16, Issue 5
Platelet rich plasma therapy for shoulder tendinopathy: a systematic review
- *Corresponding Author:
- Pooja Pithadia
Department of Medical Biotechnology, Medica Stem Cells, Marylebone, London, United Kingdom
E-mail: pooja@medicastemcells.com
Abstract
Background: There is afascinating interest inplatelet-rich plasma (PRP)injection as a treatment for shoulder tendinopathy.
Objective: To determine the efficacy of platelet-rich plasma (PRP) injections for shoulder tendinopathycompared with other existing conventional methods.
Design: Systematic review
Data Sources: PubMed, Scopus, EMBASE, and Cochrane Librarypublished up to October 15, 2020 Study Eligibility Criteria:Randomized controlled trials, single-arm interventional study, and a prospective open-label study comparing PRP with conventional methods (saline, sham injection, dry needling, corticosteroid. non-steroidal anti-inflammatory drugs, physiotherapy, and hyaluronic acid) in patients with shoulder tendinopathy. The search included only in vivo studies and excludednon-human studies.
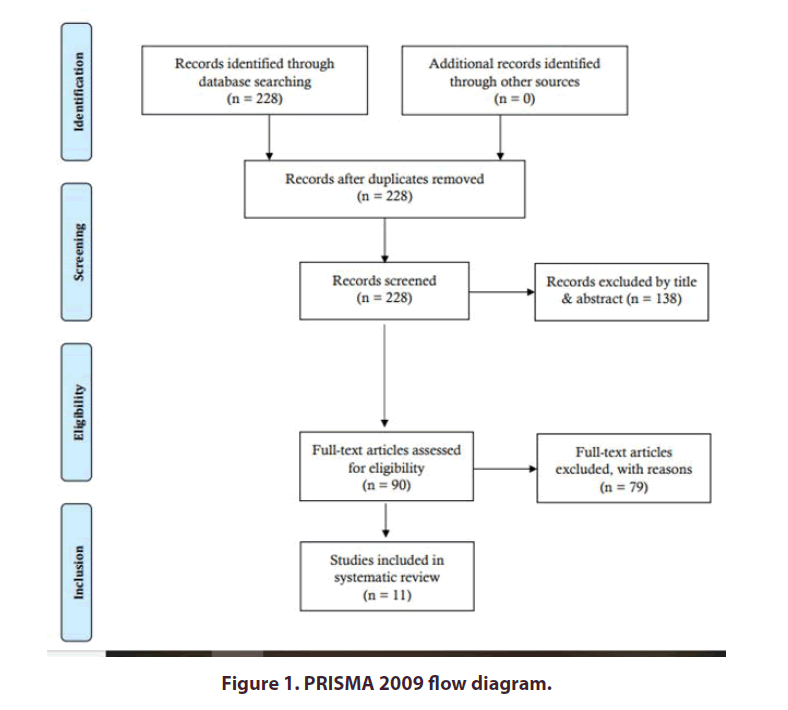
Study Appraisal and Synthesis Methods: A systematic review was carried out in accordance with the PRISMA statement. The authors reviewed and tabulated data according to the year of study and journal, study type and level of evidence, study population, intervention, outcomes, and interpretation.
Results: Among the 228 records screened, 11 studies were included in the systematic review study. The selected studies focused on the application of PRP in the treatment of shoulder tendinopathy. Among 11 studies, 9 studies demonstrated favourable outcomes such as improved pain and functional scoresafter the PRP application for shoulder tendinopathy. In two studies, no statistically significant differences were seen regarding clinical outcomes.
Conclusions: Injection of PRP is more efficacious than control injections in patients with shoulder tendinopathy.
Keywords
PRP • platelet-rich plasma • systematic review • rotator cuff tendinopathy • shoulder tendinopathy
Abbreviations: PRP: Platelet-Rich Plasma; EMBASE: Excerpta Medica Database; RCT: Rotator Cuff Tendinopathy; NSAIDs: Non-Steroidal Anti-Inflammatory Drugs; TGF-β: Transforming Growth Factor-beta; PGDF: Platelet-Derived Growth Factor; VEGF: Vascular Endothelial Growth Factor; EGF: Epidermal Growth Factor; PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses; MRI: Magnetic Resonance Imaging; ROM: Range of Motion; VAS: Visual Analogue Scale; SDQ: Shoulder Disability Questionnaire; SPADI: Shoulder Pain and Disability Index; WORC: Western Ontario Rotator Cuff Index; DASH: Disabilities of the Arm, Shoulder and Hand; SH: Sodium Hyaluronate; PTRCT: Partial-Thickness Rotator Cuff Tendinopathy; ASES: American Shoulder and Elbow Surgeons Shoulder Score; CMS: Constant-Murley Score; SST: Sterling Structural Therapy
Introduction
Supraspinatus, infraspinatus, teres minor, and subscapularistendons together constitute the rotator cuff, which provides stability to the shoulder joint by allowing itscomplete range of motion [1]. However, hypermobility,strain, irritation, and poor mechanics leads to tendons' painful conditions, termed'Tendinitis' [2].
Degeneration weakens the tendon and exacerbates the pain further with complete failure,termed as 'tendinosis' [2,3]. Both these tendinitis and tendinosis represent tendon issues and together called tendinopathy[4]. Neer believed that the shoulder tendinopathy process started with tendonitis, progressed to tendinosis with degeneration and partial-thickness tears, and ultimately resulted in full-thickness tears [5].
Rotator Cuff Tendinopathy (RCT)is the most common cause of shoulder discomfort. A cross-sectional study reported that around 86% of all clinical diagnoses of shoulder ache and disability were rotator cuff abrasions [6]. A combination of intrinsic factors (tendon hypervascularity, changes in the composition of the matrix of the tendon, anddecreased cellular activity), as well as extrinsic factors (repetitive microtrauma, compression from anatomical structures, and impingement),causes inflammation followed byprogressiverotator cuffdegeneration [1,6]. Usually, shoulder pain and stiffness will worsen at night, where the patient cannot lie on the affected side. As the disease progresses, the intensity of pain and stiffness increases, restricting even simple activities such as hair grooming or dressing.
Furthermore, palpable snapping and coarse crepitation on the passive rotation of the shoulder show fibrosis or partial/ complete rotator cuff rupture, severely restrictedmovements, followed by secondary shoulder osteoarthritis [7]. Conservative treatments for RC tendinopathy include rest, activity modification, Non- Steroidal Anti-Inflammatory Drugs (NSAIDs), physical therapy, and corticosteroid injections. However, none of the existing therapies showsconsistent improvement in functional,clinical, and radiological outcomes and available evidence recommends that effective intervention for early tendinosis and low-grade tears is still vague [6]. Physical therapy(exercise and manual therapy) takes a prolonged time for recovery, where patient compliance is required to get maximal effect [8]. Though NSAID treatment and corticosteroidinjections are known to alleviate inflammation and pain, severe gastrointestinalcomplications after prolonged oral NSAID administration, as well as inhibition of collagen synthesis and increased risk of tendon failure caused by repeated corticosteroid injections, are important concerns [9]. Hence, the use of growth factors has been recommended to improve the healing process and promote tendon regeneration during treatment [10].
The autologous growth factors like transforming growth factor-beta (TGF-β), Platelet-Derived Growth Factor (PDGF), Vascular Endothelial Growth Factor (VEGF), and Epidermal Growth Factor (EGF) found in Platelet-Rich Plasma (PRP) play a critical role in cell proliferation, cell differentiation, chemotaxis, and angiogenesis [11]. Using PRP in tendon healing isbased on the fact that tendinopathy reduces stem cell numbers, disorganise matrix and hypoperfusion. The use of autologous platelets can revascularise the tendon injury site, accelerate its healing, and improve pain and functional limitations in rotator cuff pathologies [12]. Platelet-Rich Plasma (PRP) is the plasma's cellular componentwith a higher platelet concentration more than baseline levels of 1,50,000/ml to 3,00,000/ml than whole blood, obtained by centrifuging the whole blood [10,13].
According to the American College of Rheumatology (ACR) and European League Against Rheumatism (EULAR) recommendations, Platelet-Rich Plasma (PRP) treatment is recommended despite having concerns like heterogeneity and lack of standardization in PRP preparation. Moreover, the use of PRP therapy was based on the clinical experience of the experts [14].
Objectives
In this review, we aim to investigate PRP injection's effectiveness regarding pain reduction and functional improvement compared with the conventional methods, including saline, sham injection, dry needling,corticosteroid, non-steroidal anti-inflammatory drugs, physiotherapy, and hyaluronic acid in adult patients with rotator cuff tendinopathy.
Methods
This systematic review was performed following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statementin Figure 1 [15].
Eligibility criteria
All participants in the trials had to have a clinical diagnosis of shoulder tendinopathy. We excluded articles published before the year 2000.
Search strategy
A comprehensive, systematic literature search and analysis were performed onOctober 15, 2020, by the authors involved in this study. The databases of MEDLINE (PubMed), Scopus, EMBASE, and the Cochrane librarywere searched without time limits. The following keywords were used in different combinations: 'shoulder tendinopathy', 'rotator cuff tendinopathy, 'platelet-rich plasma', 'PRP therapy', 'PRP vs corticosteroids', 'PRP vs physical therapy', and 'non-surgical methods for shoulder tendinopathy'. We limited the search to articles in English, and only human studies were included. After assessing all titles and abstracts, the relevant articles were selected. All bibliographies for eachselected article were also searched to identify further relevant literature. These articles were finally collected and subjected to the already established inclusion and exclusion criteria before the review's commencement.
Study selection
All studies were included if their design could be classified into one of the three categories: randomised controlled trial, single-arm interventional study, and prospective open-label study.
The inclusion criteria of shouldertendinopathy comprisetendinosis, rotator cuff tendinopathy,and partial rotator cuff tear. Studies that included subjects of complete rotator cufftears, adhesive capsulitis, trauma, calcific rotator cuff disease, or rheumatological disease were excluded.
Data collection
Studies that have a PRP-treated group along with a control group were eligible for inclusion. The control group included saline, sham injection, dry needling,acorticosteroid:non-steroidal anti- inflammatory drugs, physiotherapy, and hyaluronic acid. The quantity of injections or the injection-guiding technique was not limited.The post-interventional follow-ups were allottedfor not more than a year.
Summary measures
We considered pain reduction and functional improvement as the primary and secondary outcome, respectively.
Synthesis of results
The researchers independently recorded the study design, population, intervention, outcome measure and interpretation.
Results
Study selection
Of the 228 articles initially identified by the search, 11 met the inclusion criteria. These articles describe PRP outcome with respect to other conservative treatment modalitiesin Table I for systematic reviewing.
| Articles | Study | Intervention | Subjects enrolled (n)/ controls enrolled (n') | Outcome | Conclusion |
|---|---|---|---|---|---|
| [9] | Single-centre, prospective, double-blinded, randomized controlledtrial (Level 1) | PRP Vs Dry needling (ultrasound guidance); PRP preparation: (3 ml extracted from centrifuged 25 ml blood) |
39 RCT patients with a supraspinatus tendon lesion (tendinosis or a partial tear less than 1.0 cm, but not a complete tear) (20/19). 6 months follow-up |
PRP shows significant improvement in mean Shoulder Pain and Disability Index with no severe complication in either group. | Autologous PRP causes a progressive reduction in pain and disability, compared to dry needling. Hence, PRP injections are safe, useful, & superior to the dry needling |
| [12] | Randomised clinical trial (Level 2) | PRP Vs Corticosteroid injection (MRI guidance) | 35 patients with chronic rotator cuff tendinopathy for more than 40 years old; (17/18) Assessment - 1, 3, 6 months follow-up |
Both groups showed statistically significant improvements in outcome after injection when compared with before injection. No statistically significant differences between the two groups. | PRP therapy may be employed in patients more than 40 years old instead of corticosteroid injection due to lack of severe adverse effects unlike steroid group |
| [15] | Randomised clinical trial | PRP Vs corticosteroid injection (ultrasound guidance) | 30 patients with RCT (15/15). Assessment - before & 8 weeks after injection |
Significant improvement in both groups after injection regarding the range of motion (ROM) (flexion, abduction, extension, internal and external rotation), Visual Analogue Scale (VAS), & Shoulder Disability Questionnaire (SDQ). Significant improvement in the frequency of tendinitis/bursitis in the steroid group compared to PRP. In contrast, the improvement in the tear and effusion was higher in PRP compared to steroid group. | Both PRP and corticosteroid injections were effective. PRP is a safe and good alternative to corticosteroid. The ultrasound-guided injection may improve efficacy. |
| [10] | Double-blind Randomised controlled trial; Level 1. | PRP Vs Sham injection; (ultrasound-guided). PRP preparation: (5 mL PRP extracted from centrifuged 54 mL blood) |
40 patients (18 years to 70 years age) with RCT or partial tear (20/20); Assessment - 3, 6, 12, 24 weeks & 1-year follow-up | No significant difference between two groups in SPADI, WORC (Western Ontario Rotator Cuff Index), and VAS scores. Within each group, the SPADI, WORC, and VAS scores showed significant improvements compared with baseline at all time points. No significant group × time interactions in the range of motion measures | PRP injection was not more effective in improving pain, disability, quality of life, and range of motion than placebo in patients who were treated with an exercise program. |
| [16] | Prospective open-label study | PRP for patients' refractory to physical therapy and corticosteroid (ultrasound-guided) |
18 RCT patients (3 mL 1% xylocaine followed by 3.5 mL PRP) | Improvement in VAS pain score, functional outcomes, external rotation test It improved MRI appearance by 1 to 3 points in 16 patients. Satisfactory score: 12 completely satisfied, 5 satisfied, & 1 unsatisfied |
PRP - safe, significant, sustained improvement in pain, function, and MRI outcomes |
| [7] | Prospective clinical study | PRP for patients' refractory to physical therapy & corticosteroid | 20 RCT patients (4 mL autologous PRP) Assessment – 3 months follow up |
Improvement in VAS score and functional outcome Improvement in empty cane test, drop arm test, and theta band external rotation at 90° The decline in mean analgesic use |
PRP - safe and effective |
| [17] | Single-arm interventional study | PRP (ultrasound-guided) | 30 RCT (supraspinatus tendon thickness). Assessment –- 4, 8, 12, and 24 weeks follow up | Significant improvement in pain and disability score No significant radiological improvement in tendon thickness till 12 weeks, but observed a decrease in tendon thickness finally at 24 weeks |
PRP - safe, cheap, and painless outpatient procedure showing promising results compared to other treatment modalities |
| [18] | Randomized controlled trial+ observational | PRP Vs Placebo (4ml saline )(ultrasound-guided) + 3-month home-based, daily exercise |
9 (7/2) RCT patients Assessment – 1, 2, 3, 6 months |
Patients receiving PRP showed improvements in pain (VAS), disability (DASH), and tendon pathology, unlike placebo group. | PRP injection showed improvement in pain, function, and tendon pathology. |
| [19] | Randomised controlled trial | PRP Vs Physical therapy (PT). PRP preparation: 6 mL extracted from 15 mL peripheral blood activated by CaCl2 | 70 (35/35) RCT patients with chronic partial supraspinatus tears in MRI. Assessment – 12 months |
Improved ROM in the physical therapy group, while significantly better DASH score is seen in the PRP group | Compared with PT, PRP will be a well-tolerated application that showed promising results |
| [20] | A double-blind, random sed controlled trial | PRP Vs Sodium hyaluronate (SH) PRP preparation:4mL PRP extracted from centrifuged 20 mL autologous venous blood |
45/47 patients with partial-thickness RCT (PTRCT) detected by clinical examination &MRI. Assessment – before & after 1, 3, 6, and 12 months |
Significant improvement in the PRP group &PRP+SH group in the tear size, Constant, ASES score, and visual analogue scale. | PRP best in healing small to medium PTRCT. Moreover, the combined PRP+SH injection yielded a better outcome than PRP or SH alone. |
| [21] | Randomised controlled trial/level 1 | PRP vs corticosteroid. PRP preparation: (2.5 ml PRP extracted from centrifuged 10 ml blood) Leucocyte reduced |
20/20 RCT patients with painful partial RC tears diagnosed by MRI. Assessment – before & after 6 weeks, 3 and 6 months | Both injection groups showed significantly better outcomes over time compared to before injection. Statistically significant improvement in the PRP group regarding VAS, ASES, CMS and SST when compared with the steroid group. MRI showed a slight nonsignificant improvement in tendinopathy/tear in both groups; however, no significant difference between the two groups. | PRP showed better results compared to corticosteroid; still, no significantly better results could be observed after 6 months. Hence, PRP could be an excellent alternative to corticosteroid injection |
Table I. Chronological list of published literature studies included in the systematic review and their findings.
Study characteristics
The search strategy included studies from 2013 until 2020. The study characteristics extracted from the eleven selected studies (research author, publication year, the study design, type of intervention, the number of patients assigned, the duration of the study, outcomes measured, and conclusion) are summarised in Table 1.
Safety of PRP therapy
None of the studiesanalysed in this systematic review reported any adverse side effect related to PRP administration.
Discussion
Rotator cuff tendinopathyis one of the most common causes of shoulder pain and discomfort. There is still an ongoing debate in the medical community regarding NSAIDs, physical therapy, or corticosteroid injections conservative treatment modalities.
Rest and ice therapy are the well-accepted first-line options. Physical therapy is often considered the first line of RCT management. A good rehabilitation program for the rotator cuff muscles should include a range of motion exercises, stretching,eccentric strengthening, balancing of muscular tone, and scapular stabilisation. Eccentric strengthening canimprove tendon healing and reduce pain in chronic RCT patients [16]. Exercise therapy has its possible beneficial effect on tendon homeostasis, prevent adverse effects of immobilisation, and aids in collagen turnover [17]. The exercise had statistically significant effects on pain reduction and function improvement but not on the range of motion or strength. Manual therapy enhancesexercise's effects;still, supervised exercise was not different from home exercise programs [18]. If there has been no significant relief from shoulder pain in two to three months, then other treatment options will be considered.
A current meta-analysis recommended that NSAIDs are less effective than corticosteroid injections achieving patient remission rate with shoulder pain at 4-weeksor 6-weekspost-treatment [19]. Hence, corticosteroid injections are often used to treat the shoulder pain associatedwith rotator cuff tendinopathies.
Corticosteroid injection, due to its anti-inflammatory effect,limits the accumulation of macrophages and leukocytes and the release of vasoactive kinins. It reduces the prostaglandin formation, contributing to the inflammation procedurethat may lead to pain relief and mechanical improvement [20]. Several in vitro studies revealed that corticosteroid provided therapeutic effect to the tendon and the surrounding connective tissues by inhibiting collagen along with inflammatory suppression [21]. Such a positive therapeutic outcome of corticosteroids may last only for a short duration since its repetitive administration may reduce cell viability and proliferation and deteriorate specific parts of the injected tendon tomake it more prone to rupture[22]. However, the efficiency of corticosteroid injections for RCT is still questionable. A systematic review by the American Academy of Orthopaedic Surgeons revealedthe least efficacy for corticosteroid injections in RCT treatment [23]. Considering the low efficacy and complications of corticosteroid injections, patients and providers are looking for better options. As all participants in this cohort were refractory to former conservative modalities, PRP seems to have provided additional benefits.
PRP consists of proteins that change the patient's pain receptors and reduce pain sensation with its anti-inflammatory effect on injured tendons [24]. Studies revealed that the PRP injection significantly improved pain, joint ROM, and shoulder function in patients with partial rotator cuff tear [1,25]. Deepak Chaudhary et al., 2016 [7] and Scarpone et al.[16]26also reported that asingle injection of PRP is safe and effective in treating refractory RCT. No side effect was observed during PRP treatment except pain at the injection site, which lasted for only ten minutes and relieved naturally [7]. Furthermore, Scarpone et al. [26] found significant improvement in function, pain, and radiological scores. Similarly, there is a drastic improvement in pain score after the single PRP injection dose [27]. Hence, it is worth studying the comparison of PRP injections with the available conventional methods.
In a double-blinded RCT, Kesikburun et al.[10] compared the effect of a single PRP injection with a placebo where PRP had no benefit over placebo in terms of pain, disability, quality of life, and range of motion. This study utilised a leukocyte rich PRP formulation that could have caused a harmful effect in the early healing stages.
Rha et al, [9] compared PRP therapy with dry needling, where PRP provided more symptomatic relief and functional improvement than dry needling. It shows that exercise might have improved the tendinopathycondition, which might have concealed PRP's positive effect. Whether PRP remains beneficial to those who do not respond to exercise therapy requires further research. Even the needling causes bleeding, which can stimulate inflammation and promote tendon healing. However, the range of motion was improved equally in both the PRP and dry needling groups. The reason for PRP's dominance to dry needling may be the more substantial therapeutic effects ofPRP injections than dry needling or a different therapeutic mechanism synergistic to dry needling.Finnoff et al. [28] recommended that the PRP fills the void created by dry needling treatment and stimulates tissue regeneration, leading to dominant results. Due to its coagulative properties, PRP solidifies to form a gel-like three-dimensional structure that helps stay at the target area long enough to heal the injuredpartwithout exogenous platelet activation. Additionally, exogenous platelet activation with calcium chloride or bovine thrombin can control the speed of the release of growth factors.Further study will help in elucidating the PRP therapeutic mechanism.
IIhanli et al. [19] 29 compared PRP therapy with physiotherapy in supraspinatus tendinopathytreatment and concluded that PRP therapy might be as effective as physiotherapy. Cai et al., 2019 [25] showed thatSH and PRP's combined injection yielded a better clinical outcome than SH or PRP alone.Niazi et al, 2020 [30] reported that PRP is a cheap, safe, and easily prepared outpatient procedure showing promising results when compared to physiotherapy, arthroscopy, and surgeries. However, PRP injection could provide further functional benefits over exercise therapy or physiotherapy, which requires further investigation.
Thus, PRP's dominance over the control group, including sham injection with saline, physical therapy, and dry needling, maybe due to its more potent therapeutic effects and increased regenerate tissue homeostasis [9,29].
Though Mohaghegh S et al. [12] could not find any significant differences between PRP and corticosteroid injection in terms of pain relief, range of motion, and function improvements for chronic rotator cuff tendinopathy.It is recommended to follow PRP treatment in patients with more than 40-years-old instead of corticosteroid injection dueto the lack of complicationsin PRP group unlike corticosteroid group, especially for the elderly. On the contrary, Shams et al. [23] reported a statistically significant improvement in pain and functional scores in the PRP group compared to the corticosteroid groupfor patients with a partial supraspinatus tear. The use of leucocyte reduced PRP in this study may have yielded better results. Direct comparison studies of PRP with corticosteroid injections in the RCT treatment are conflicting. Some show a significant benefit of PRP over corticosteroids,while others show no difference [15].
Thus, PRP has been used as an adjunct to accelerate healing in soft tissue injuries and decrease blood loss. This PRP application is relatively novel and has been proven to work in other forms of tendinopathy. But there is minimal research when it comes to the efficacy of rotator cuff tendinopathy treatment. Furthermore, higher-quality studies should be performedto determine PRP's efficacyin comparison with other conventional treatment modalities [31,32].
Limitations
First, there was heterogeneity in the patient groups and diagnostic criteria among different studies. Shouldertendinopathy, including supraspinatus tendinosis, supraspinatus tear,rotator cuff tendinosis, rotator cuff tear, and subacromial impingement, was enrolledin different studies. Additionally, a diagnostic image via MRI or ultrasonography wasused for confirmation. Hence, it was impossible to categorise the patients accurately for a subgroup analysis classified by clinically or image-diagnosed subgroups.
Second, the PRP injection guidance technique to the subacromial space or injured tendon may influence the outcome. Seven of the included studies in our systematic review used ultrasound guidance. But there is no description ofthe guidance method in the remaining studies. Hence, it is not possible to compare the effect of varied guidance methods.
Third, there are various control groups,such assaline, sham injection, dry needling,acorticosteroid: non-steroidal anti-inflammatory drugs, physiotherapy, and hyaluronic acid.
Fourth, this systematic review includes randomised controlled trials, a single-arm interventional study, and a prospective open-label study. Hence, it is not possible to interpret eitherpatient age orsymptom duration with treatment outcomes.
Fifth, there is no detailed information about the exact PRPcomposition, including platelet/leukocyte concentration, biochemical analysis, and preparation method. There were heterogeneities in doses, preparation, and regimen within every group of injectantsin the enrolled studies,which may influence the outcomes.
Conclusion
The present systematic review showed that PRP injection might be safer and more effective than the control group (saline, sham injection, dry needling, corticosteroid. non-steroidal anti-inflammatory drugs, physiotherapy, and hyaluronic acid) in pain reduction for patients with rotator cuff tendinopathy. The current evidence is promising, but there is a lack of a clinical study exploring combination regimens for treating rotator cuff tendinopathy.Though PRP's use has potential benefits such as faster recovery, improved functional outcomes, and a reduction in a relapse of tendon injuries, its application in shoulder tendinopathy is still weakly supported due to the lack of standardisation. Hence, high-qualitydouble-blinded randomised controlled trials with a larger study population must be undertaken further to compare PRP with other treatment methods and characterisePRP's optimal preparation to maximiseits benefit in treating shoulder tendinopathy.
Declarations
Ethics approval and consent to participate
Not Applicable.
Consent for publication
Not Applicable.
Availability of data and materials
Not Applicable.
Competing Interests
The authors declare that they have no competing interests.
Funding
Not Applicable.
Acknowledgements
Not Applicable.
Data availability
PubMed, Scopus, EMBASE, and Cochrane Library published up to October 15, 2020. According to the year of study and journal, the authors reviewed and tabulated data, study type and level of evidence, study population, intervention, outcomes, and interpretation.
Author Contribution
PP recommended the title, concept and drafted an outline of the paper.MJS carried out the selection of the papers included in the present review and drafted the systematic review article. PP, STand PS carried out the final editing of the paper. All authors read and approved the final review article.
References
- Singh SKK, Ojha A. Platelet-rich plasma for the improvement in shoulder function in rotator cuff disorders. Int. J. Res. Orthop. 5(1), 156–161 (2019).
- Obaid H, Connell D. Cell therapy in tendon disorders: what is the current evidence? Am. J. Sports. Med. 38(10), 2123–2132 (2010).
- Khan KM, Cook JL, Bonar Fet al. Histopathology of common tendinopathies. Update and implications for clinical management. Sports. Med.27(6), 393–408 (1999).
- Seitz AL, McClure PW, Finucane S et al. Mechanisms of rotator cuff tendinopathy: intrinsic, extrinsic, or both?.Clin. Biomech. 26(1), 1–12 (2011).
- Biberthaler P, Wiedemann E, Nerlich A et al. Microcirculation associated with degenerative rotator cuff lesions. In vivo assessment with orthogonal polarisation spectral imaging during arthroscopy of the shoulder. J. Bone. Joint. Surg. Am. 85-A(3), 475–480 (2003).
- Phadke A, Singh B, Bakti N. Role of platelet rich plasma in rotator cuff tendinopathy- clinical application and review of literature. J. Clin. Orthop. Trauma.10, 244e247 (2019).
- Deepak Chaudhary, Kumar Rohit, RajeshwarKalla. Functional outcome and results of platelet rich plasma (PRP) in rotator cuff tendinopathy. Int. J. Sci. Res.5(1), 2277–8179 (2016).
- Naslund GK, Fredrikson M, Hellenius ML et al. Determinants of compliance in men enrolled in a diet and exercise intervention trial: a randomised, controlled study. Patient. Educ. Couns. 29, 247–256 (1996).
- Rha DW, Park GY, Kim YK et al. Comparison of the therapeutic effects of ultrasound-guided platelet-rich plasma injection and dry needling in rotator cuff disease: a randomised controlled trial. Clin. Rehabil. 27, 113–122 (2013).
- SerdarKesikburun, Arif Kenan Tan, Bilge Yilmazet al.Platelet-rich plasma injections in the treatment of chronic rotator cuff tendinopathy: A randomised controlled trial with 1-year follow-up. Am. J. Sports. Med. 41: 2609 (2013).
- Werner S, Grose R. Regulation of wound healing by growth factors and cytokines. Physiol. Rev.83, 835–870 (2003).
- Mohaghegh S, Emam MM, Gachkar L. Comparative evaluation of platelet rich plasma(prp) and corticosteroid injection in chronic rotator cuff tendinopathy. J. Orthop. Ther. JORT–174 (2017).
- Marx RE. Platelet-rich plasma (PRP): what is PRP and what is not PRP?.Implant. Dent. 10(4), 225–228 (2001).
- Kolasinski SL, Neogi T, Hochberg MC et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis. Care. Res. (Hoboken). 72(2), 149–162 (2020).
- Ibrahim DH, El-Gazzar NM, El-Saadany HM et al. Ultrasound-guided injection of platelet rich plasma versus corticosteroid for treatment of rotator cuff tendinopathy:Effect on shoulder pain, disability, range of motion and ultrasonographic findings. The. Egyptian. Rheumatologist. 41, 157–161 (2019).
- Jonsson P, Wahlström P, Öhberg L et al. Eccentric training in chronic painful impingement syndrome of the shoulder: Results of a pilot study. Knee. Surg. Sports. Traumatol. Arthrosc. 14(1), 76–81 (2006).
- Spargoli G. Treatment of rotator cuff tendinopathy as a contractile dysfunction. a clinical commentary. Int. J. Sports Phys. Ther. 14, 148–158 (2019).
- Kuhn JE. Exercise in the treatment of rotator cuff impingement: a systematic review and a synthesised evidence-based rehabilitation protocol. J. Shoulder. Elbow. Surg. 18(1), 138–160 (2009).
- Zheng XQ, Li K, Wei YD et al. Nonsteroidal anti-inflammatory drugs versus corticosteroid for treatment of shoulder pain: a systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 95(10), 1824–1831 (2014).
- Hong JY, Yoon SH, Moon DJ et al. Comparison of high- and low-dose corticosteroid in subacromial injection for periarticular shoulder disorder: a randomised, triple-blind, placebo-controlled trial. Arch. Phys. Med. Rehabil. 92, 1951–1960 (2011).
- Paavola M, Kannus P, Ja¨rvinen TA et al. Treatment of tendon disorders. Is there a role for corticosteroid injection?.Foot. Ankle. Clin. 7, 501–513 (2002).
- Dean BJ, Lostis E, Oakley T et al. The risks and benefits of glucocorticoid treatment for tendinopathy: a systematic review of the effects of local glucocorticoid on tendon. Semin. Arthritis. Rheum. 43, 570–576 (2014).
- Shams A, El-Sayed M, Gamal O et al. Subacromial injection of autologous platelet-rich plasma versus corticosteroid for the treatment of symptomatic partial rotator cuff tears. Eur. J. Orthop. Surg. Traumatol. 26, 837–842 (2016).
- Zhang J, Wang JH. PRP treatment effects on degenerative tendinopathy – an in vitro model study. Muscles. Ligaments. Tendons. J.4, 10–7 (2014).
- Cai Y, Sun Z, Liao B et al. Sodium hyaluronate and platelet-rich plasma for partial-thickness rotator cuff tears. Med. Sci. Sports. Exerc. 51, 227–233 (2019).
- Scarpone M, Rabago D, Snell Eet al.Effectiveness of platelet-rich plasma injection for rotator cuff tendinopathy: a prospective open-label study. Glob. Adv. Health. Med.2(2), 26–31 (2013).
- Sengodan VC, Kurian S, Ramasamy R. Treatment of partial rotator cuff tear with ultrasound-guided platelet-rich plasma. J. Clin. Imaging. Sci.7, 32 (2017).
- Finnoff JT, Fowler SP, Lai JK et al. Treatment of chronic tendinopathy with ultrasound-guided needle tenotomy and platelet-rich plasma injection. PM. R.3, 900–911 (2011).
- Ilhanli I, Guder N, Gul M. Platelet-rich plasma treatment with physical therapy in chronic partial supraspinatus tears. Iran. Red. Crescent. Med. J. 17(9), e23732 (2015).
- Niazi GE, Hassan MS, Elfawy DM. Ultrasound-guided injection of platelet-rich plasma (PRP) in rotator cuff tendinopathy: effect on patients' symptoms and supraspinatus tendon thickness. Egypt. J. Radiol. Nucl. Med. 51, 111 (2020).
- Liberati A, Altman DG, Tetzlaff J et al. The PRISMA statement for reporting systematic reviews and meta analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 339, b2700 (2009).
- Wesner M, Defreitas T, Bredy H, Pothier L et al. A pilot study evaluating the effectiveness of platelet-rich plasma therapy for treating degenerative tendinopathies: A randomised control trial with synchronous observational cohort. PLoS. One. 11(2), e0147842 (2016).