Review Article - Interventional Cardiology (2023) Volume 15, Issue 2
Overview of lipid-lowering management characteristics in Mexico: Barriers and challenges to overcome
- Corresponding Author:
- Leslie Marisol Lugo-Gavidia Cardiovascular Research Physician, Mexican Academic Consortium for Clinical Data Acquisition SC, Sinaloa, Mexico, E-mail: lesliemarisol.lugogavidia@research.uwa.edu.au
Received date: 07-Feb-2023, Manuscript No. FMIC-23-88986; Editor assigned: 09-Feb-2023, PreQC No. FMIC-23-88986 (PQ); Reviewed date: 23-Feb-2023, QC No. FMIC-23-88986; Revised date: 02-Mar-2023, Manuscript No. FMIC-23-88986 (R); Published date: 10-Mar-2023, DOI: 10.37532/1755- 5310.2023.15(2).664
Abstract
There is now overwhelming evidence supporting the cardiovascular benefits of lipid control. However, despite international recommendations, there is still a big proportion of patients that do not achieve proper lipid control. This outcome is of special interest in low and middle-income countries where higher cardiovascular risk has been reported. Different barriers complicate lipid management in Mexico. These include non-medical determinants of health, risk factors, disease distribution, socioeconomic resources and the health system. In this article, we provide an overview of the characteristics and challenges involved in achieving appropriate lipid control in the Mexican population. Providing a depth understanding of the patient and healthcare system barriers aid to facilitate the development of more effective strategies for improving lipid management according to the country’s necessities and resources.
Keywords
Lipid therapy • LDL-c • Statin • Cardiovascular risk
Introduction
Elevated Low-Density Lipoprotein cholesterol (LDL-c) and elevated no High- Density Lipoprotein cholesterol (non-HDL-c) are major contributors to the development and progression of Cardiovascular Disease (CVD). It is estimated that ~60% of Coronary Artery Disease (CAD) is associated with high cholesterol levels [1-3]. This highlights the importance of early diagnosis and the implementation of adequate treatment. In view of the overwhelming evidence showing the benefit of reducing LDL-c in cardiovascular morbidity and mortality, the Mexican guideline for the diagnosis and treatment of dyslipidaemias has recently been revised to align with international guidelines and to promote lower lipid target goals in at-risk populations (established atherosclerotic cardiovascular disease, diabetes, very high- risk patients) [2-5]. In addition, comparatively elevated estimated rates of people at high risk have been reported in low- and middle-income countries compared to wealthier countries. This factor escalates the human impact of the problem [6]. Additionally, despite the large amount of evidence supporting Lipid-Lowering Therapy (LLT) as the cornerstone treatment of dyslipidaemias, several studies have reported low proportions of established LLT and lipid control across different populations [7-16]. This trend is especially the case in low- and middle-income countries where socioeconomic factors can influence access and adherence to more potent lipid-lowering therapies.
Little is known about lipid management in Mexico, this manuscript aims to provide a comprehensive overview of the current state of knowledge on the management of dyslipidaemias in Mexico. A focus is given to national recommendations and Mexico’s country-specific barriers which adversely impact lipid management.
Barriers in lipid-lowering management in Mexico
Different studies including the Mexican registry to obtain cardiovascular data (REMECAR Registry) have consistently shown big proportions of patients not achieving the recommended LDL-c goals [17].
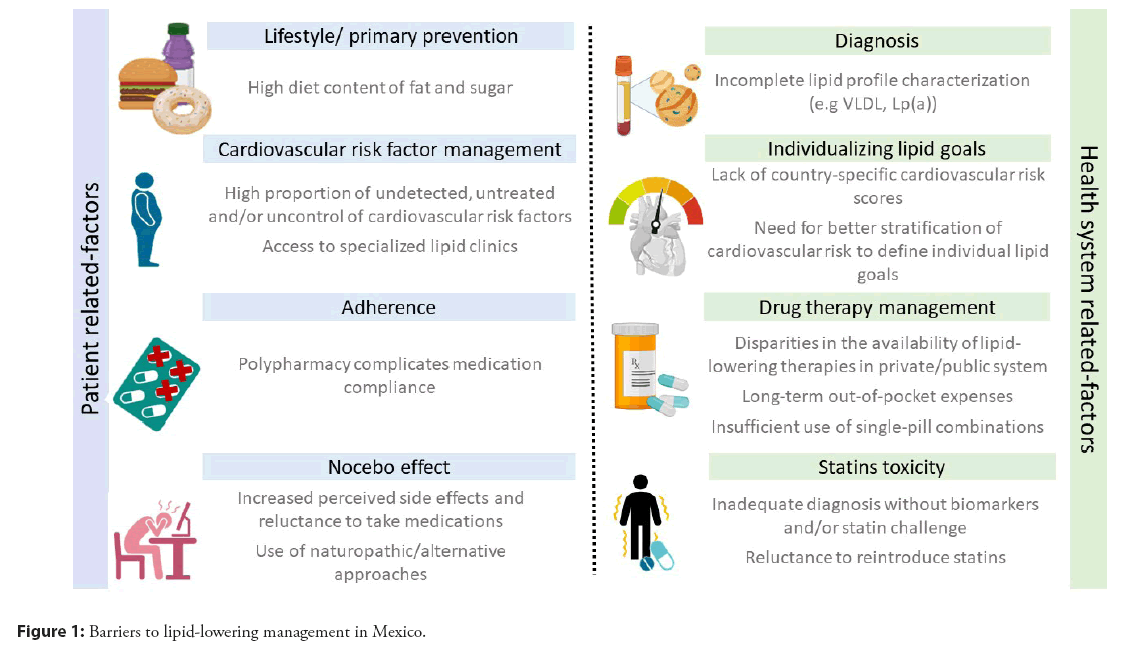
A recent report of LLT in the Mexican population showed that only one-third (33.4%) of the patients with ASCVD attending for the first time to specialized cardiovascular clinics were on LDL-c treatment goals (14.1% achieved LDL-c 70-55 mg/dL and 19.3% achieved a more strict goal of LDL-c<55 mg/dL). The failure to achieve LDL-c goals was substantial even among patients receiving moderate and high-intensity statins, justifying the need for more potent LLT in a meaningful proportion of patients. Furthermore, 29.9% of this high-risk population were not on any LLT at the time of the visit. The principal barriers to achieving lipid control in Mexico are summarized in Figure 1.
Lifestyle and cardiovascular risk factors in Mexico
Previously reported data showed a high prevalence of patients presenting a high cardiovascular risk in Mexican population [2,6]. Different factors contribute to these results.
Firstly non-medical determinants of health play an important role, while tobacco consumption in Mexico is relatively low (7.4%) [18]. Compared with other countries (e.g. 9.4% USA, 14.5% UK, 19.8% Spain), obesity and overweight represent one of the major problems in our population. Mexico has one of the highest rates of obesity globally shown in the Table 1, 74.1% of the Mexican population is overweight or obese and this problem is extending to earlier stages in life with a historic increase in child obesity [18- 20]. This is of special interest in the topic as it has been proven that atherosclerosis starts in childhood and risk factor control in the early stages of the disease has an important impact on future outcomes [2]. While diet and lifestyle play a crucial role, other non-modifiable factors such as genetics aggravate this condition.
| Japan | Belgium | United Kingdom | Mexico | |
|---|---|---|---|---|
| Smokers (%) | 16.7 | 15.4¥ | 14.5* | 7.4* |
| Overweight or obese population (%) | 27.2 | 55.4¥ | 64.2 | 74.1* |
| Total fat supply (Grams per capita per day) | 89.2 | 173.4 | 138.7 | 102.1 |
| Total calories supply (Kilocalories per capita per day) | 2691 | 3800 | 3395 | 3163 |
| Total protein supply (Grams per capita per day) | 88 | 100.3 | 106.2 | 91.7 |
| Sugar supply (Kilos per capita per day) | 26.4 | 60.5 | 38.5 | 44.2 |
| Vegetables supply (Kilos per capita per day) | 96.7 | 135.9 | 79.3 | 66.5 |
Note: *Data form 2020, ¥Data from 2018
Table 1: Smoking, overweight/obesity and diet data distribution in different countries.
Another concerning matter is the increase in the prevalence of classical cardiovascular risk factors reported from 2012 to 2018. A prevalence of 10.3% to 21.4% of Diabetes Mellitus (DM) and 18.4% to 42.6% of hypertension have been reported in different national surveys [5,21]. Higher prevalence has been observed in selected populations, and more alarming are the low rates of awareness, treatment, and control [17,22,23]. Another factor associated with lipid control is the presence of Non-Alcoholic Fatty Liver Disease (NAFLD). Few reports have found an increased risk for NAFLD in Mexican population due to lifestyle and genetic factors. NAFLD has been related to hepatic overproduction of very low-density lipoprotein particles and dysregulated clearance of lipoproteins from the circulation, which makes diet management and LLT fundamental among these patients [24-27].
Some other particular characteristics among the Mexican population include an increased prevalence of metabolic syndrome and DM compared with other populations. Interestingly, the lipid profile also presents a distinctive pattern, previous small reports have suggested that Latin American countries have a higher prevalence (12.9% to 24.7%) of increased triglycerides, low HDL-c, elevated Non-HDL-c, and normal or mildly elevated LDL-c which may contribute to residual CVD risk [17,28-30]. Gender also plays a role, as lower HDL-c levels have been detected among Hispanic/Latin women [2].
Individualizing Lipid goals: Current guidelines/ recommendations
Due to the importance of the topic many countries and societies are continuously updating their recommendations regarding lipid management. A summary of current guidelines and recommendations is provided in Table 2.
| Mexican clinical practice guideline | ACC/AHA guideline | ESC guideline | |||||
|---|---|---|---|---|---|---|---|
| CV risk calculator used | Globorisk | ASCVD Risk Estimator | SCORE 2 & SCORE2-OP | ||||
| Lab risk calculator | Office risk calculator | ||||||
| Elements required for CV risk calculator | Demografics | Country Gender Age |
Country Height* Weight* Gender Age |
Sex Age Race |
Sex Country |
||
| Laboratory | Total-cholesterol | Total-cholesterol HDL-cholesterol | Non HDL-cholesterol | ||||
| Office | Systolic Blood pressure | Systolic Blood pressure | Systolic Blood pressure | Systolic Blood pressure | |||
| Medical History | Smoker Diabetic | Smoker | Diabetic Smoker Treatment for HTN | Smoker | |||
| Applicable age | 40-80 years | 40-79 years | 40-89 years | ||||
| Risk calculator interpretation | Low risk | Globorisk <10% | ASCVD Risk<5% | <50 y | 50-69 y | = 70 y | |
| “Low to moderate” SCORE2<2.5% | “Low to moderate” SCORE2 <5% | “Low to moderate” SCORE2-OP <7.5% | |||||
| Moderate risk | Globorisk 10-19% | “Intermediate” ASCVD Risk 7.5-<20% | |||||
| High risk | Globorisk 20-29% | ASCVD Risk >20% | SCORE2 2.5 to<7.5% | SCORE2 5 to<10% | SCORE2-OP 7.5 to<15% | ||
| Very high risk | Globorisk 30-39% | SCORE2 = 7.5% | SCORE2 = 10% | SCORE2-OP = 15% | |||
| Extreme high risk | Globorisk = 40% | ||||||
| Comments | Exclude patients with history of coronary artery disease and stroke | Intended for patients with LDL-C<190 mg/dL (4.92 mmol/L), without ASCVD, not on LDL-C lowering therapy | Intended for apparently healthy patients without ASCVD, diabetes, CKD or FH Adjusted tables for low, medium, high and very high risk Fatal and non-fatal events | ||||
Note: ASCVD: Atherosclerotic Cardiovascular Disease, SCORE2: Systematic Coronary Risk Estimation 2 SCORE2-OP: Systematic Coronary Risk Estimation 2-Older Persons, CKD: Chronic Kidney Disease, FH: Familial Hypercholesterolemia. *For BMI calculation which substitute the laboratory data
Table 2: Summary of Mexican clinical practice guidelines, ACC/AHA and ESC guidelines, and cardiovascular risk recommendations for lipid lowering management.
In brief, LDL-c reduction is now recommended by all international guidelines, with more intense treatment goals recommended for those at higher risk [3,4,31]. Consistently with the European Society of Cardiology (ESC) and the American College of Cardiology/American Heart Association (ACC/AHA) guidelines, the Mexican lipid control guidelines recommend stratification according to risk categories and Cardiovascular (CV) risk estimation [2-5,31,32]. Different LDL-c goals are defined based on the risk category to achieve the best risk/benefit ratio [2- 4,31,33]. The 2018 ACC/AHA guidelines recommend<70 mg/dL as a goal for patients with Atherosclerotic Cardiovascular Disease (ASCVD) [2], while the 2019 ESC guidelines recommend<55 mg/dL with a stepwise approach [3]. In 2022, the American College of Cardiology published an expert consensus, which equalizes with the European criteria and recommends an LDL-c goal<55 mg/dL in patients with clinical ASCVD at very high risk [34]. The Mexican guideline makes a distinction between stable chronic ASCVD (LDL-c goal<70 mg/dL) and recent ASCVD (Acute coronary syndrome<1 year), ASCVD complicated with diabetes and/or extensive/diffuse ASCVD, these patients to be considered at extremely high risk (LDL-c goal<55 mg/dL) [5]. This distinction has important pharmaco-economic implications, extremely high-risk profile corresponds to subpopulations that have been shown to benefit the most with more potent therapies (iPCSK9) [5], hence insurance policies can justify the addition of these therapies if necessary.
The risk estimation calculator also varies across guidelines (Table 2). Although international datasets and national registries across the globe have contributed to the development of the risk calculators used in the current guidelines [2-4,31], Mexico does not have a country-specific risk estimator.
Recently, the Mexican Society of Cardiology updated its guidelines recommending the use of Globorisk as the preferred tool to evaluate CV risk for Mexico. Globorisk was calibrated in Mexican population, however, it is important to mention, this CV risk calculator was derived from US studies including a proportion of the Hispanic/Latin population and was calibrated with national surveys, the risk score was developed for an age break of 40-80 years and only evaluates fatal cardiovascular disease. In this context, the recently published 2021 ESC Guidelines on CVD prevention in clinical practice have introduced the new SCORE2 and SCORE2-Older People (SCORE2-OP) with CV risk thresholds according to age, which was re-calibrated to estimate both fatal and non-fatal CV risk [4]. SCORE2-OP takes into account the increase of non-CVD mortality risk associated with age and provides a more accurate risk estimation in older people that may help to reduce the excessive use of medication in this vulnerable population [4,35]. However, it was developed for European population. The SCORE2 should not be used in young patients (<40 years), which is an important limitation as in recent years there has been an increase in ASCVD in younger populations. The ACC/AHA guideline uses the ASCVD risk estimator; this score can be used in an age between 40-79 years. This calculator was derived from community-based studies in the US to estimate 10-year risk hard outcomes (MI and stroke, both fatal and nonfatal), and also provide a lifetime ASCVD risk [2]. A more extensive/ detailed comparison between guidelines is beyond the scope of this review. It is important to recognize that most of the data used to build the risk scores derived from studies in selected populations and thus the impact of other baseline factors influencing risk, including genetics and risk enhancing factors are not well established. This draws attention to the importance of long-term real-world registries from different regions.
Medical professionals should be familiarized with the evaluation of cardiovascular risk and implement said evaluation in their regular practice as it is an inexpensive tool and may help weigh the risks with the expected benefits associated with more potent LLT. Unfortunately, in many cases, this critical clinical step is omitted in primary care due to patient overload and restricted consultation time. This oversight results in inappropriate CV risk stratification. The exclusive use of the reference values provided by the laboratory to norm the clinical strategy without individualizing target goals according to risk (higher risk=lower LDL-c goals) can result in an insufficient treatment [36].
Importantly, regardless the guideline of choice, lifestyle changes and LDL-c reduction ( ≥ 50%) in patients with established ASCVD are well-established recommendations as it has proven substantial benefit in clinical outcomes, hence more potent strategies should be considered for these patients to achieve the LDL-c goal. It is important to underline that the risk stratification and the therapeutic recommendations used should correspond to the same guideline.
Diagnosis and follow-up
Early diagnosis and accurate characterization of the type of dyslipidaemia (e.g. polygenic, familial hypercholesterolemia, hypolipoproteinemia (a), hyperalphalipoproteinemia, among others) are fundamental for proper management. These phenotypes require a complete lipid profile for their detection, it is recommended that lipid measurements include total cholesterol, HDL-c, Non-HDL-c, LDL-c (direct laboratory measurement should be preferred to the calculated method) and triglycerides. Additional measurement of ApoA1, ApoB, VLDL-c and lipoprotein (a) are valuable to detect atherogenic dislipoproteinemia and should be performed if possible, in particular in patients with suboptimal LDL-c lowering response to statins [2-5]. Unfortunately, many centers in Mexico only perform basic lipid profiles and in many cases, LDL-c determination is calculated rather than measured.
The use of additional tests is still a matter of debate. Coronary Artery Calcium (CAC) score and/or carotid ultrasound can help to detect subclinical disease and re-stratified the risk. Given dyslipidaemias are in general asymptomatic, determining the extension of the disease could be relevant in patients with moderate risk and to evaluate the progression of the disease [2-5]. However, it is limited in primary care and in the public health system as they required specialized centers and can represent out-of-pocket expenses.
Other non-classical tests/biomarkers such as high-sensitivity C-reactive protein, homocysteine, extracellular vesicles, pulse wave velocity, growth differentiation factor-15, fibrinogen, ankle- brachial index, and uric acid have been related to cardiovascular risk [37-41]. These tests may provide useful information and complement the evaluation in selected cases where initiating therapy may be considered borderline. However, their use in clinical practice is controversial since many of them have not demonstrated yet net benefit in improving clinical outcomes, security and cost-effectiveness.
While the state-of-the-art tests are important to understand the underlying pathophysiology and future therapies, in the context of developing countries where the availability and costs play an important role, their clinical value needs to be considered. Hence, extensive testing is not recommended routinely and clinical reasoning based on medical history and physical examination must prevail when making medical decisions.
Importantly, patients need to be advised of the importance of follow up, even if lipid control is achieved, dyslipidaemia requires constant monitoring as LLT is a dynamic issue. A proportion of patients with previous control will present lipid levels above thresholds at follow-up, many patients will have an initial consultation and only schedule a follow-up visit if symptoms are present when the progression of the disease has extended, this is predominately challenging when patients do not understand the chronicity and the implications of the disease. A study focusing on lipid management programs and patient education demonstrated a benefit of personalizing the therapy and empowering the patient on lipid level improvement [42]. Consequently, a detailed discussion with the patient is fundamental for long-term management.
Diet management and naturopathic
Lifestyle changes are recommended as first-line therapy for CVD risk factor management [2-4,31], supported by studies demonstrating the beneficial impact of physical activity and diet on cardiovascular risk [43-50]. Moderate to intense aerobic physical activity is advised for lipid control 3-4 times per week. Additionally, different diets have proven to be effective in lowering lipid levels such as Mediterranean diet, the USDA Food Pattern, and the AHA Diet, among others [2]. The general recommendation is to limit the intake of sweets, fats, and red meats, and increase vegetables, fruits and non-tropical vegetable oils (such as olive oil), nuts, poultry, blue fish, and whole grains [2,3,47,50]. However, it has to be recognized the difficulty in achieving appropriate lipid control with lifestyle changes alone. Successful management most frequently will require specific and consistent dietary/exercise programs and/or the assistance of other health professionals such as dietitians, nutritionists, or exercise physiologists. Mexican cultural food has a high content of fat and sugar and the recent overload with convenient low-price fast food aggravates the issue. The Mexican socioeconomic setting also represents a challenge for the implementation of these measurements, as the appropriate diets include products that can increase cooking expenses and the extensive working hours leave restricted time for the required physical activity.
The aforementioned issues cause lifestyle changes to be difficult to implement, being more challenging with older age as lifestyle patterns are already installed. In the sub-analysis of the REMECAR registry, only 1.7% of the population self-reported to be taking any dietary measures [17]. Although lifestyle change recommendations are fundamental for all patients, in low-risk patients and mild dyslipidaemias lifestyle management alone can be attempted, whereas in more severe cases (e.g. secondary prevention, CV enhancers) LLT should not be delayed. While many physicians will initially recommend additional LLT, a growing proportion of patients are showing personal preferences to avoid drug therapy and use naturopathic approaches. Even though, some natural/ dietary strategies have shown an effect in lowering LDL-C (e.g. Berberine, red rice yeast) [51-53], it needs to be remembered that these strategies are not as effective as LLT and despite their natural properties they are not exempt from possible side effects and interactions. Consequently, they should only be used in cases where there is a definitive contraindication of LLT or as coadjutants.
It is important to emphasize that only a few strategies have been scientifically studied in this context and they should not be confused with natriuretic products that lack scientific evidence. Unfortunately, in Mexico these products are not often regulated and/or approved by proper medical authorities, the ingredients might not be disclosed, and patients might not disclaim their use during their medical history which makes it more difficult to monitor their use, side effects, and interactions that can be unpredictable.
Medication availability and adherence
Medication adherence continues to be one of the most important barriers to achieving lipid goals. Many factors are involved in not having correct medication compliance (polypharmacy, cost, side effects). It is not uncommon that patients present multiple comorbidities in addition to lipid alterations. This is especially the case in older age, when the debut of new chronic disease makes polypharmacy a constant and increasing barrier. Every medication added to a patient’s chronic treatment represents additional pills to remember, additional costs, and an increase in the risk of side effects/interactions that could result in treatment discontinuation. Single combination pills are a useful tool to minimize poor adherence in chronic diseases [54]. However, these medications can be limited as one of the main barriers in Mexico is medication costs and availability in the public health system.
Mexico has a fractionated healthcare system composed of private and public systems. The public health system provides its beneficiaries with a range of medications; however, it is limited to medications and brands approved within the annual budget and supply. In terms of LLT, while the efficiency of using combined or more potent therapies is evident (e.g., high-intensity statins+ezetimibe, PCSK9 inhibitors), these medications most frequently are not included in public health insurance. Some public health systems exclusively cover selected single combination pills (simvastatin- ezetimibe) and several patients will require stronger therapies to achieve lipid control. Only some public health systems have approved the use of evolocumab for selected patients. Nonetheless, patients require to complete a strict screening and fulfill certain conditions to be eligible (e.g. extremely high-risk) and could be restricted to monthly availability.
On the other hand, a very low proportion of the population has insurance with medication coverage, hence most cases these medications represent an out-of-pocket expense, which is a notable barrier to implementing these therapies. The REMECAR registry reported a very low proportion (0.5%) of patients receiving PCSK9 inhibitors after visiting specialized cardiovascular clinics, even within patients with ASCVD only in ~1.3% were prescribed these types of therapies despite two-thirds of the population did not achieve the LDL-c treatment goals [17]. The limited access and the expense associated with more potent therapies increase the non-adherence to medication and the use of other alternatives resulting in inadequate control.
The use of generic medications is a common solution as they are more economically accessible, however, long-term comparisons of hard outcomes between these products are not frequently evaluated and this must be considered when making clinical decisions.
Side effects vs. nocebo-effect
Another factor contributing to the reluctance in using LLT is the risk of developing side effects (e.g. statin-associated muscle symptoms, new-onset type 2 diabetes mellitus, hepatotoxicity) [53]. The major concern in lipid management is statin-associated muscle symptoms which are considered the most prevalent side effect and one of the principal reasons for statin discontinuation.
Its presentation varies in severity from diffuse myalgias to its most severe presentation, rhabdomyolysis. Although these side effects have been well described in the literature, the incidence varies between 1%-5% in controlled randomized trials and 5%-10% in observational data [5,53,55]. While some populations are more prone to present these side effects, sensitivity to statin dosage has not been demonstrated in Hispanic/Latino population [2].
Even though statin intolerance could severely impact lipid management, it must be distinguished from the so-called nocebo effect caused by negative expectations about treatment side effects. Unfortunately, the unregulated information distributed by internet search and social media can be misleading and patients might wrongly attribute another condition as an adverse event, leading to higher reports of side effects. In our setting, this nocebo effect has particular importance, as it has caused an increase in the reluctance to use statins and to try natural solutions. Physicians need to conduct a detailed interrogation (directed questionnaires such as Statin-Associated Muscle Symptom Clinical Index) and examination (e.g., use of biomarkers) to determine real statin intolerance and determine the appropriate treatment modifications [53,56].
It is important to remember that patients shouldn’t be left untreated especially high and very high-risk patients. Algorithms have been developed to help reintroduce statin therapy, involving reassessment and rechallenge of statins (unless side effects are severe) by modifying the dosing regimen or using an alternative statin. For example hydrophilic statins have less muscle penetration as lipophilic statins are non-selective and can diffuse into extrahepatic tissues [2,53,56]. Clinicians need to reassess, review past adverse events and possible contributing factors and then rediscuss in detail the potential risk-benefit of the reintroduction of statin therapy to be able to make a shared decision [36,53]. Alternatively, newer medication targeting other systems can be attempted if available.
Future Perspectives
The growing numbers in CVD across the world and studies demonstrate the urgent need to improve lipid management. Current efforts are focused in finding new alternatives to traditional statin therapy. A detailed description of these investigations is not the goal of the present review, it is however briefly worth mentioning the therapies that are currently being explored and/or that might become suitable alternatives for certain clinical scenarios in the near future. First, Bempedoic acid has shown LDL-c reductions between 17% and 25%. Bempedoic acid is a small molecule that acts in the same pathway as statins; however, it blocks ATP-Citrate Lyase (ACL) and has a selective activation in hepatocytes resulting in a favorable safety profile for muscle symptoms and diabetes. In this context the CLEAR (Cholesterol Lowering via Bempedoic Acid, an ACL-Inhibiting Regimen) Tranquility trial confirmed lipid reduction and safety in among hypercholesterolemic patients with statin intolerance, providing new treatment options for patients with this profile [57,58]. A second approach involves small interfering RNAs (siRNAs) to selectively inhibit the production of specific proteins. An example is Inclisiran, an anti-PCSK9 with a long-standing effect of 3-6 months. Phase I studies with Inclisiran showed a reduction of PCSK9 levels and, in parallel, a corresponding decrease in LDL-C [57,59,60]. The ORION-1 trial revealed a maximum reduction in LDL-C of 52.6% (300 mg two-dose) at 180 days, additionally, Inclisiran also promoted reduction of other lipid components (non-HDL-C, triglycerides, apolipoprotein B, and lipoprotein (a)) [60,61]. The long term effect of Inclisiran and its impact on major adverse cardiovascular events is currently under investigation (ORION-3;ORION-4). Olpasiran in another siRNA directed to decrease Lp(a) has shown us that Lp(a) an independent risk factor and primarily genetically determined [57]. Other therapies being investigated include anti- sense oligonucleotides (Vupanorsen which inhibits ANGPTL3 production, Volanesorsen targeting apolipoprotein C-III and Pelacarsen to decrease Lp(a)) [57,59].
Conclusions
Mexico has some of these molecules available as part of clinical trials, which provide clinicians with early experience on their use and the possible challenges to expect in our population. Even though some of them represent a promising alternative to improve LLT and provide more personalized therapy, evidence of their benefit/security is still to be determined and their use will still be limited due to their cost.
Mexico’s socioeconomic situation in addition to the globally recognized challenges in LLT makes lipid control a big health burden for patients, clinicians, and the health system. Real-world data provided by national surveys and longitudinal registries including clinical outcomes are essential in understanding the sociodemographic, medical, and healthcare characteristics that impact LLT among different populations. Identifying the barriers to achieving proper lipid control according to the country-specific settings can help to determine specific strategies and national recommendations.
It is evident that income level and out-of-pocket costs is a fundamental barrier, however, it is not comparable with the economic expenses associated to cardiovascular events. Improving prevention and achieving cardiovascular risk control represents the best cost/benefit strategy. While cost barriers could be unavoidable due to the patient’s means, patient education (empowerment and awareness) and continuous medical training in the topic are essential to overcome other non-system related barriers.
References
- Ference BA, Ginsberg HN, Graham I, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the european atherosclerosis society consensus panel. Eur Heart J. 38:2459-2472 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APHA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: Executive summary: A report of the American college of cardiology/American heart association task force on clinical practice guidelines. J Am Coll Cardiol. 73:3168-3209 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk: The task force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur Heart J. 41:111-188 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Visseren FLJ, Mach F, Smulders YM, et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice: Developed by the task force for cardiovascular disease prevention in clinical practice with representatives of the european society of cardiology and 12 medical societies With the special contribution of the European Association of Preventive Cardiology (EAPC). Eur Heart J. 42:3227-3337 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Pavía-López AA, Alcocer-Gamba MA, Ruiz-Gastelum ED, et al. Guía de práctica clínica mexicana para el diagnóstico y tratamiento de las dislipidemias y enfermedad cardiovascular aterosclerótica. Arch Cardiol Mex. 92:1-62 (2022).
[CrossRef] [Google Scholar] [PubMed]
- Hajifathalian K, Ueda P, Lu Y, et al. A novel risk score to predict cardiovascular disease risk in national populations (Globorisk): A pooled analysis of prospective cohorts and health examination surveys. Lancet Diabetes Endocrinol. 3:339-355 (2015).
[CrossRef] [Google Scholar] [PubMed]
- Kotseva K, De Backer G, De Bacquer D, et al. Lifestyle and impact on cardiovascular risk factor control in coronary patients across 27 countries: Results from the European society of cardiology ESC-EORP Euroaspire V registry. Eur J Prev Cardiol. 26:824-835 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Kotseva K, De Backer G, De Bacquer D, et al. Primary prevention efforts are poorly developed in people at high cardiovascular risk: A report from the European society of cardiology EUR Observational research programme EUROASPIRE V survey in 16 European countries. Eur J Prev Cardiol. (2020).
[CrossRef] [Google Scholar] [PubMed]
- Kotseva K, Investigators E. The EUROASPIRE surveys: Lessons learned in cardiovascular disease prevention. Cardiovasc Diagn Ther. 7:633-639 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Ray KK, Molemans B, Schoonen WM, et al. EU-wide cross-sectional observational study of lipid-modifying therapy use in secondary and primary care: The DA VINCI study. Eur J Prev Cardiol. 28:1279-1289 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Klimchak AC, Patel MY, Iorga ŞR, et al. Lipid treatment and goal attainment characteristics among persons with atherosclerotic cardiovascular disease in the United States. Am J Prev Cardiol. 1:100010 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Carrillo-Larco RM, Benites-Moya CJ, Anza-Ramirez C, et al. A systematic review of population-based studies on lipid profiles in Latin America and the Caribbean. Elife. 18(9):e57980 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Vrablik M, Seifert B, Parkhomenko A, et al. Lipid-lowering therapy use in primary and secondary care in central and eastern europe: DA VINCI observational study. Atherosclerosis. 334:66-75 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Cífková R, Bruthans J, Wohlfahrt P, et al. 30-year trends in major cardiovascular risk factors in the czech population, czech MONICA and czech post-MONICA, 1985-2016/17. PLoS One. 15:e0232845 (2020).
- Dyrbus K, Gasior M, Desperak P, et al. Characteristics of lipid profile and effectiveness of management of dyslipidaemia in patients with acute coronary syndromes-data from the TERCET registry with 19,287 patients. Pharmacol Res. 139:460-466 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Reiner Ž, De Backer G, Fras Z, et al. Lipid lowering drug therapy in patients with coronary heart disease from 24 European countries-findings from the EUROASPIRE IV survey. Atherosclerosis. 246:243-250 (2016).
[CrossRef] [Google Scholar] [PubMed]
- De los Ríos-Ibarra MO, Leiva-Pons JL, Rodríguez-Reyes H, et al. Risk stratification and lipid evaluation in mexican patients, evidence of lipid and cardiovascular analysis in REMECAR. The mexican registry of cardiovascular diseases (REMECAR group). Atheroscler Plus. 50:32-39 (2022).
[CrossRef] [Google Scholar] [PubMed]
- OECD. Non-medical determinants of health. (2016).
- OECD. Overweight or obese population (indicator). (2019).
- OECD. Health at a Glance. (2021).
- Garcia-Garcia G, Aviles-Gomez R, Luquin-Arellano VH, et al. Cardiovascular risk factors in the Mexican population. Ren Fail. 28:677-687 (2006).
[CrossRef] [Google Scholar] [PubMed]
- Meaney A, Ceballos-Reyes G, Gutiérrez-Salmean G, et al. Cardiovascular risk factors in a Mexican middle-class urban population. The Lindavista Study. Baseline data. Archivos de Cardiología de México. 83:249-256 (2013).
- Meaney E, Lara-Esqueda A, Ceballos-Reyes GM, et al. Cardiovascular risk factors in the urban Mexican population: The FRIMEX study. Public Health. 121:378-384 (2007).
[CrossRef] [Google Scholar] [PubMed]
- Garcia DO, Morrill KE, Lopez-Pentecost M, et al. Nonalcoholic fatty liver disease and associated risk factors in a community-based sample of Mexican-origin adults. Hepatol Commun. 6:1322-1335 (2022).
[CrossRef] [Google Scholar] [PubMed]
- Bernal-Reyes R, Castro-Narro G, Malé-Velázquez R, et al. The Mexican consensus on nonalcoholic fatty liver disease. Rev Gastroenterol Mex (Engl Ed). 84:69-99 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Chatrath H, Vuppalanchi R, Chalasani N, et al. Dyslipidemia in patients with nonalcoholic fatty liver disease. Semin Liver Dis. 32:22-29 (2012).
- Martins I. Unhealthy nutrigenomic diets accelerate nafld and adiposity in global communities. J Mol Genet Med. 9:162 (2015).
- Practical recommendations for the management of cardiovascular risk associated with atherogenic dyslipidemia, with special attention to residual risk. Spanish adaptation of a european consensus of experts. Clin Investig Arterioscler. 29:168-177 (2017).
- Pedro-Botet J, Mantilla-Morató T, Díaz-Rodríguez Á, et al. The role of atherogenic dyslipidaemia in clinical practice guidelines. Clin Investig Arterioscler. 28:65-70 (2016).
- Ponte-Negretti CI, Isea-Perez JE, Lorenzatti AJ, et al. Atherogenic dyslipidemia in Latin America: Prevalence, causes and treatment: Expert's position paper made by The Latin American Academy for the Study of Lipids (ALALIP) endorsed by the Inter-American Society of Cardiology (IASC), the South American Society of Cardiology (SSC), the Pan-American College of Endothelium (PACE), and the International Atherosclerosis Society (IAS). Int J Cardiol. 243:516-522 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Catapano AL, Graham I, De Backer G, et al. 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J. 37:2999-3058 (2016).
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: Executive summary: A report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation. 140:e563-e595 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Mach F, Baigent C, Catapano ALet al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk: The task force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). European Heart Journal. 41:111-188 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Lloyd-Jones DM, Morris PB, Ballantyne CM, et al. 2022 ACC expert consensus decision pathway on the role of nonstatin therapies for ldl-cholesterol lowering in the management of atherosclerotic cardiovascular disease risk: A report of the american college of cardiology solution set oversight committee. J Am Coll Cardiol. 80:1366-1418 (2022).
[CrossRef] [Google Scholar] [PubMed]
- Cooney MT, Selmer R, Lindman A, et al. Cardiovascular risk estimation in older persons: Score O.P. Eur J Prev Cardiol. 23: 1093-1103 (2016).
[CrossRef] [Google Scholar] [PubMed]
- Morales-Villegas EC, Rodriguez-Martinez HA. We do not need more guidelines, or more drugs, or more combinations! the priority is a medical ecosystem that favors evidence-based medicine, personalization, empowerment, access, and reflection. (2022).
- Lugo-Gavidia LM, Nolde JM, Carnagarin R, et al. Association of circulating platelet extracellular vesicles and pulse wave velocity with cardiovascular risk estimation. Int J Mol Sci. 23 (2022).
[CrossRef] [Google Scholar] [PubMed]
- Vlachopoulos C, Aznaouridis K, Stefanadis C, et al. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: A systematic review and meta-analysis. J Am Coll Cardiol. 55:1318-1327 (2010).
[CrossRef] [Google Scholar] [PubMed]
- Barter PJ, Rye KA. Homocysteine and cardiovascular disease: Is HDL the link? Circ Res. 99:565-566 (2006).
[CrossRef] [Google Scholar] [PubMed]
- Carnagarin R, Nolde JM, Ward NC, et al. Homocysteine predicts vascular target organ damage in hypertension and may serve as guidance for first-line antihypertensive therapy. J Clin Hypertens (Greenwich). 23:1380-1389 (2021).
- Wang J, Tan GJ, Han LN, et al. Novel biomarkers for cardiovascular risk prediction. J Geriatr Cardiol. 14: 135-150 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Morales-Villegas EC, Vega-Velasco A, Moreno-Virgen G, et al. LDL-cholesterol lowering efficacy of atorvastatin® in primary prevention. Real-world experience in a developing country; a program based on evidence, personalization, and empowerment. (2021).
- Hupin D, Roche F, Gremeaux V, et al. Even a low-dose of moderate-to-vigorous physical activity reduces mortality by 22% in adults aged ≥ 60 years: A systematic review and meta-analysis. Br J Sports Med. 49:1262-1267 (2015).
[CrossRef] [Google Scholar] [PubMed]
- Sacks FM, Lichtenstein AH, Wu JHY, et al. Dietary fats and cardiovascular disease: A presidential advisory from the american heart association. Circulation. 136:e1-e23 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Threapleton DE, Greenwood DC, Evans CE, et al. Dietary fibre intake and risk of cardiovascular disease: Systematic review and meta-analysis. Bmj. 347:f6879 (2013).
[CrossRef] [Google Scholar] [PubMed]
- Wang X, Ouyang Y, Liu J, et al. Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: Systematic review and dose-response meta-analysis of prospective cohort studies. Bmj. 349:g4490 (2014).
[CrossRef] [Google Scholar] [PubMed]
- Estruch R, Ros E, Salas-Salvadó J, et al. Primary prevention of cardiovascular disease with a mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med. 378:e34 (2018).
[CrossRef] [Google Scholar] [PubMed]
- Sofi F, Abbate R, Gensini GF, et al. Accruing evidence on benefits of adherence to the Mediterranean diet on health: An updated systematic review and meta-analysis. Am J Clin Nutr. 92:1189-1196 (2010).
[CrossRef] [Google Scholar] [PubMed]
- Martínez-González M, Hershey MS, Zazpe I, et al. Transferability of the mediterranean diet to non-mediterranean countries. What is and what is not the mediterranean diet. Nutrients. 9(11):1226 (2017).
- de Lorgeril M, Salen P, Martin JL, et al. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: Final report of the lyon diet heart study. Circulation. 99:779-785 (1999).
[CrossRef] [Google Scholar] [PubMed]
- Becker DJ, Gordon RY, Halbert SC, et al. Red yeast rice for dyslipidemia in statin-intolerant patients: A randomized trial. Ann Intern Med.150:830-839 (2009).
[CrossRef] [Google Scholar] [PubMed]
- Becker DJ, French B, Morris PB, et al. Phytosterols, red yeast rice, and lifestyle changes instead of statins: A randomized, double-blinded, placebo-controlled trial. Am Heart J. 166:187-196 (2013).
[CrossRef] [Google Scholar] [PubMed]
- Ward NC, Watts GF, Eckel RH, et al. Statin toxicity. Circ Res. 124:328-350 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Corrao G, Parodi A, Zambon A, et al. Reduced discontinuation of antihypertensive treatment by two-drug combination as first step. Evidence from daily life practice. J Hypertens. 28:1584-1590 (2010).
[CrossRef] [Google Scholar] [PubMed]
- Collins R, Reith C, Emberson J, et al. Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet. 388:2532-2561 (2016).
[CrossRef] [Google Scholar] [PubMed]
- Stroes ES, Thompson PD, Corsini A, et al. Statin-associated muscle symptoms: Impact on statin therapy-european atherosclerosis society consensus panel statement on assessment, aetiology and management. Eur Heart J. 36:1012-1022 (2015).
[CrossRef] [Google Scholar] [PubMed]
- Tokgözoğlu L, Libby P. The dawn of a new era of targeted lipid-lowering therapies. Eur Heart J. 43:3198-3208 (2022).
[CrossRef] [Google Scholar] [PubMed]
- Colivicchi F, Di Fusco SA, Scicchitano P, et al. Updated clinical evidence and place in therapy of bempedoic acid for hypercholesterolemia: ANMCO position paper. J Cardiovasc Med (Hagerstown). 22:162-171 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Raal FJ, Kallend D, Ray KK, et al. Inclisiran for the treatment of heterozygous familial hypercholesterolemia. N Engl J Med. 382:1520-1530 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Scicchitano P, Milo M, Mallamaci R, et al. Inclisiran in lipid management: A literature overview and future perspectives. Biomed Pharmacother. 143:112227 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Ray KK, Landmesser U, Leiter LA, et al. Inclisiran in patients at high cardiovascular risk with elevated LDL cholesterol. N Engl J Med. 376:1430-1440 (2017).
[CrossRef] [Google Scholar] [PubMed]