Case Report - International Journal of Clinical Rheumatology (2021) Volume 16, Issue 1
Multiple exostosis disease
- Corresponding Author:
- Kawtar Nassar
1Department of Rheumatology
IbnRochd University Hospital Center, Morocco
E-mail: kawtarnassar@yahoo.fr
Abstract
Multiple exostosisdisease is a rare condition. It is characterized by the proliferation and the development of numerous bone swellings in the metaphysis of long bones with a possible abnormality in their shape and length. It preferentially affects the knees, shoulders, ankles and wrists. These lesions remain clinically asymptomatic, but the pain is the main complaint of patients. The phenotype of this disease varies greatly between patients. All bones that develop through endochondral ossification can be affected like long bones. Some localizations are rare but potentially serious such as the ribs, the spine or the pelvis due to the proximity to important structures. The most feared, although rare, complication is the transformation into chondrosarcoma, requiring a close monitoring. The treatment can be conservative or surgical. The treatment and excisional surgery may be indicated in the event of functional disorders or deformities.The greater knowledge of the pathophysiology of the disease makes it possible to consider potential therapeutic targets. We report a rare case with iliac bone localization, discovered in adolescence rather than childhood.
Keywords
multiple cartilaginous exostoses ● skeletal dysplasia ● ulna lengthening ● osteochondromas
Introduction
Multiple exostosis disease, also known as familial ostechondromatosis or diaphyseal aclasis, is a rare genetic disease with an autosomal dominant disorder, characterized by the presence of multiple osteochondromas (exostoses) [1]. It is mainly caused by loss of function mutations in two genes: exostosin-1 (EXT1) and exostosin-2 (EXT2) and not appear to have a sexual predominance. This benign tumoraffects1 in 50,000 births. Osteochondromas form in the first decade of life and stop growing at puberty. In the majority of cases, they are asymptomatic [1,2]. The most common location is at the lateral side of the most active growth plate of a long bone. Clinical problems include pain and functional impairment. Additionally, growth deformities of bones and short stature are considerably present. Malignant degeneration of osteochondroma is a rare but important complication [3].Sacrum localization is not usual. We report a case of a 20-year-old female patient who has anunhabitual localization in iliac bone, discovered in adolescence age.
Case Report
A 20-year-old female patient and the patient is the youngest of five siblings. There was no family history of bone disorder, nor consanguineous marriage or a similar case in the family. In her past medical history, she reports slip full on the pelvis at the age of fourteen causing a transient pain. Since three years a painful and progressive swelling in right buttock were of a dull and painful nature exacerbated when she walk. The patient reports also the presence of other swelling since childhood in the right forefoot and the upper limbs not annoying or painful.Her main complaint for which she consulted was the painful right pelvic swelling.
Clinical exam
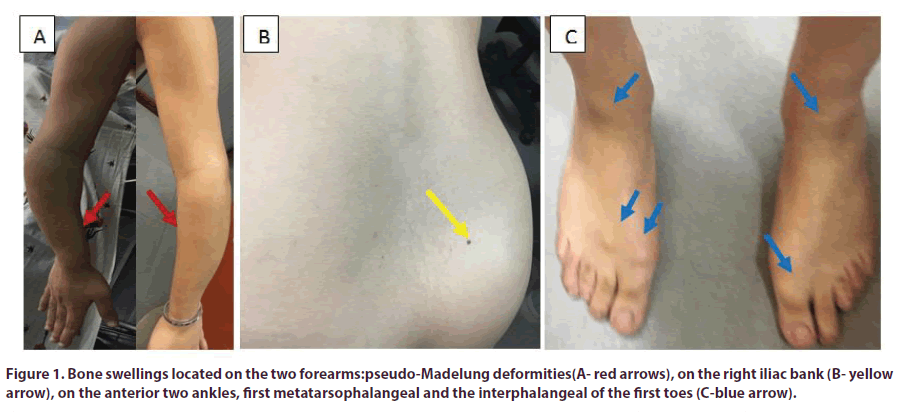
Clinical exam found the patient with short stature; the height was at 151 cm, and weight 58 kg. Ulnar shortening with deformity of the upper limb focusing on bayonet hand or pseudo-Madelung deformities (Figure 1A). Significant swelling of the right buttocks, measuring 10 cm in length, hard and fixed to the deep plane (Figure 1B), painful on pressure: the pain returned at 7/10. The clinical exam finds also other swelling having the same characteristics but of variable sizes, in anterior face of the two ankles, bilateral first metatarsophalangeal and the interphalangeal of the two first toes (Figure 1C).
Radiographic examination
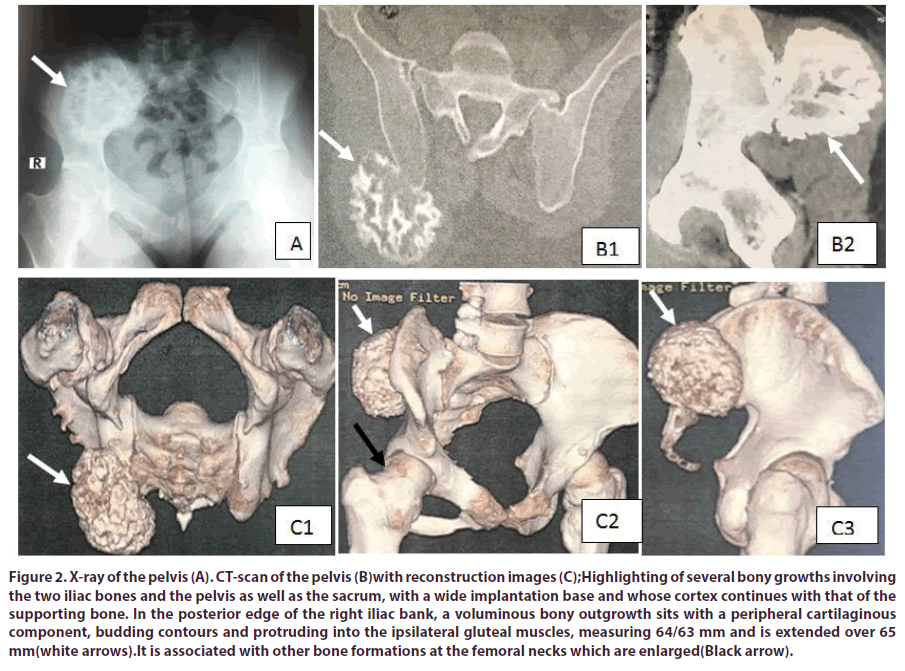
Radiographic examination revealed several pedunculated or sessile metaphyseal bone growths involving the humerus, the radius, the distal tibias bone, the forefeet and the first toes, of varying size, which the biggest is located at the level of the posterior edge of the iliac bank of the right sacroiliac joint, measuring 64/63 mm. The CT-scan of the pelvis with the reconstruction images confirms the bone growth (Figure 2), involving the two iliac bones and the pelvis as well as the sacrum, with a wide implantation base and whose cortex continues with that of the supporting bone. In the posterior edge of the right iliac bank, there is a voluminous bony outgrowth sits with a peripheral cartilaginous component, budding contours and protruding into the ipsilateral gluteal muscles, measuring 64/63 mm and is extended over 65 mm. It is associated with other bone formations at the femoral necks which are enlarged.
Figure 2: X-ray of the pelvis (A). CT-scan of the pelvis (B)with reconstruction images (C);Highlighting of several bony growths involving the two iliac bones and the pelvis as well as the sacrum, with a wide implantation base and whose cortex continues with that of the supporting bone. In the posterior edge of the right iliac bank, a voluminous bony outgrowth sits with a peripheral cartilaginous component, budding contours and protruding into the ipsilateral gluteal muscles, measuring 64/63 mm and is extended over 65 mm(white arrows).It is associated with other bone formations at the femoral necks which are enlarged(Black arrow).
Laboratory investigations
Laboratory investigations results showed normal routine serum chemistry. Serum calcium at 91 mg/l, serum phosphorus at 33 mg/l, serum alkaline phosphatase at 108 UI/l, creatinin 12 mg/l, urine calcium 315 mg/24hr, urin phosphorus 1208 mg/24 hr, parathormon 57 pg/ml, 25 (OH)vitamin D insufficiency 22,30 ng/ ml. C-reactive protein and sedimentation rate at 1 mg/l and 5 mm/1th hour, respectively. The biopsy of the pelvic voluminous bony outgrowth confirmed itsosteochondromas origin.
A diagnosis of hereditary multiple exostosiswas made according to the clinical, radiological and histological findings. In this case, there were no signs of bone weakness or signs of malignant transformation. The analgesic treatment has been instituted, and a surgical approach of the pelvic bone growthisplanned.
Discussion
Multiple exostosisdisease or hereditary multiple exostosisalso known as familial ostechondromatosis or diaphyseal aclasis a rare genetic disease characterized by the presence of multiple benign exostoses[1]. It’s an autosomal dominant disorder caused by loss of function mutations in two genes: exostosin-1 and exostosin-2 that are linked to heparan sulfate synthesis.The specific molecular mechanism of the disruption of the cartilage structure and exostosesformation is still not known [2]. This condition affects 1 in 50,000 births, such values are probably underestimated because the asymptomatic lesions. In approximately 50% of individuals, multiple osteochondromas are initially diagnosed before 3,5 years of age. In more than 80%, it is diagnosed before the end of the first decade [2]. Otherwise, some studies found a significant correlation between male sex and severe clinical presentations, like pain and sensitivomotor deficits, even deformities of the limbswhich can be explain by hormonal differences between genders, or genetic cause [3].
Most patients present most than 6 exostoses witch they can be clearly visible and palpable. The habituallocalization includes the distal femur (90%), proximal tibia (84%), fibula (76%), and humerus (72%) but they are often first discovered on the ribs and the proximal tibia. They are rarely located in carpal and tarsal bones, and never in the facial bones because they develop by intramembranous ossification [3]. Knees, shoulders, ankles and wrists are the most involved joints during diagnosis.
Exostosescancause disturbances in the growing diaphysis occasioning deformities and functional limitations. A clinical classification system determine the burden and life limitations secondary to the disease classifying the patients on three groups according to the number of involved segments [4]. The typical deformitity on the upper member is ulnar shortening and deformity focusing on bayonet hand or pseudo-Madelung deformities; and in the lower limbs the “Erlenmeyer flask”.The hip joint of the patients could be a “coxavalga” and the knee joint with genu valgum with early knee arthritis and patella subluxation. Spinal exostoses could lead to severe and acute neurological syndromes. The lesion can become bigger and causes more problems [5].The most serious complication is the transformation into secondary peripheral chondrosarcoma, which occurs in 0.5 to 5% of cases [6].
Conventional radiographs are able to focus osteochondromas in the appendicular skeleton. Computerized tomography can be considered for regions that are difficult to visualize (thorax, spine, pelvis). Magnetic resonance imaging can determine the cartilage thickness and the effect of the lesion on surrounding soft tissue structures, detectingthe malignant transformation. The positron emission tomography and cintigraphydcan be usedsuch as alternative [5,7,8]. In the absence of genetic proof, the diagnosticis based on clinical and radiological data. Like the case of our patients.
There is no specific treatment which is symptomatic and surgical. The excisional surgery may be indicated in the event of functional disorders or deformities. The conservative treatment is indicatingif there are no clinical problems to avoid. The spontaneous regression of the lesions has been documented in single cases during childhood and adolescence [9]. Excision is associatewith low morbidity. A role for adjuvant radiotherapy and chemotherapy has not been proved in secondary chondrosarcomas. The prognosis of secondary chondrosarcomas is good, since these tumours rarely metastasise: the 5-year survival is estimated to be 90% [10].
Conclusion
Multiple Exostoses Disaese is a chronic and rare disorder that requires a careful follow-up to avoid many possible complications. It is considered a difficult disease to manage and has variable presentation between each patient. This case highlighted the importance of monitoring of patients with HME and how changes in bone structure can lead to deformities and pain. The originality of this case report is the pelvic localization, age of diagnosis and the rarity of the disease.
Conflicts of interest
The authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or nonfinancial interest.
Authors’ contributions
Kawtar Nassar compiled this case report and performed the necessary literature review with the redaction and who continues to follow this patient.
Saadia Janani revised then approved this case report.
We thank our colleague Doctor Watik Asmaa for havind referred us the patient for hospital care and hospital collaboration with other disciplines.
References
- Wells M, Birchard Z. A 40-Year-Old Male Presenting with Hereditary Multiple Exostosis: Management and Considerations. Case. Rep. Orthop. (2019).
- Porter DE, Lonie L, Fraser M et al. Severity of disease and risk of malignant change in hereditary multiple exostoses. J. Bone. Joint. Surg. Br. 86(7), 1041–1046 (2004).
- Beltrami G, Ristori G, Scoccianti G et al.Hereditary Multiple Exostoses: a review of clinical appearance and metabolic pattern. Clin. Cases. Miner. Bone. Metab. 13(2), 110–118 (2016).
- D’Arienzo A, Andreani L, Sacchetti F et al. Hereditary Multiple Exostoses: Current Insights. Orthop. Res. Rev. 11, 199–211 (2019).
- Maurizio Pacifici. Hereditary Multiple Exostoses: New Insights into Pathogenesis, Clinical Complications, and Potential Treatments. Curr.Osteoporos. Rep. 15(3), 142–152 (2017).
- Robin F, RoparsM, Violas P et al. Hereditary multiple exostosis. Revue. Du. Rhumatisme. Monographies. 86, 84–91 (2019).
- Kane BS, Niasse M, Akpo G et al. Disseminated masses. La. Revue. De. Médecine. Interne. 38(8), 562–563 (2016).
- EL-Sobky TA, Samir S, Atiyya AN et al. Current paediatricorthopaedic practice in hereditary multiple osteochondromas of the forearm: a systematic review. SICOT-J. 4, 10 (2018).
- Gigi R, Kurian BT,Cole A et al.Late presentation of spinal cord compression in hereditary multiple exostosis: case reports and review of the literature. J. Child .Orthop. 13, 463–470 (2019).
- Pacifici M. Hereditary multiple exostoses: are there new plausible treatment strategies? Expert. Opin. Orphan. Drugs. 6(6), 385–391 (2018).