Research Article - Diabetes Management (2017) Volume 7, Issue 6
Inpatient diabetes mellitus: Institutional progress in management of an emerging hospital epidemic
- *Corresponding Author:
- Curtiss B. Cook
Mayo Clinic, Division of Endocrinology
Scottsdale, Arizona
E-mail: cook.curtiss@mayo.edu
Abstract
Objective: Assess changes in glycemic control and basal-bolus insulin use over 4 years in an academic teaching hospital. Methods: Point-of-care glucose and insulin administration data were obtained from electronic health records for patients with diabetes mellitus (DM) discharged from 2011 through 2014. Changes in patient-stay mean glucose, frequency of hyperglycemic measurements, and basal-bolus insulin therapy were evaluated. Results: There were 5,386 discharges with a DM diagnosis. No demographic differences were detected across the 4 years. The frequency of hyperglycemia and patient-stay mean glucose both declined significantly (P ≤ .02). Among patients in the highest tertile of hyperglycemia frequency, basal-bolus insulin therapy increased (P<.01) only among surgical patients. Increasing age, HbA1c, frequency of hyperglycemia, steroid use, and basal-bolus insulin therapy positively correlated with patient-stay mean glucose, whereas year of discharge was associated with lower values. Age, case-mix index, HbA1c, female sex, hyperglycemia frequency, and year of discharge all increased the odds of basal-bolus insulin therapy. Conclusions: This analysis provided insight into one institution’s progress in hospital DM care over time. Considerable study is still needed in the area to better understand how best to organize and deliver care to assure the best results for the patient and the health care system.
Keywords
diabetes mellitus, inpatient, hospitalization, hospital internal medicine, surgery
Introduction
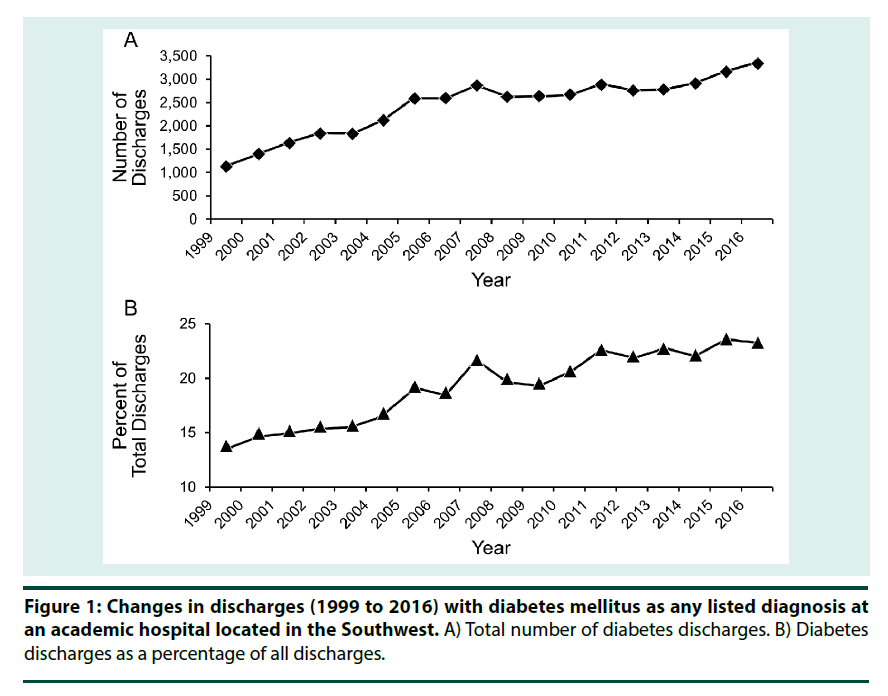
Diabetes mellitus (DM) is an emerging inpatient epidemic that has a considerable impact on the hospital system in the United States. During a 21-year period (1988 to 2009), the number of hospital discharges associated with DM nearly doubled—from 2.8 million to 5.5 million [1]. Parallel to this national trend, the authors’ institution saw a surge in the volume of inpatient DM cases, increasing from 1,117 discharges in 1999 to 3,305 in 2016, with DM now representing 23% of all hospital discharges (Figure 1). For patients with DM, hospital stays represent about 40% of the direct medical expenses attributable to DM [2], and the diagnosis of DM is also associated with a greater risk of readmissions [3,4]. Inpatient management of hyperglycemia has been an important focus of research. There is general agreement that patients with sustained hyperglycemia in the hospital have worse outcomes (e.g, increased surgical-site infections, higher mortality) [5,6]. Inpatient hypoglycemia and glucose variability are other factors that have been linked to poorer outcomes [7-13]. Consensus guidelines from various sources stress the importance of inpatient hyperglycemia management, suggest target glucose levels, and advocate for development of quality improvement programs that can optimize glucose control without increasing hypoglycemia [5,6,14]. Care of hospitalized patients with DM encompasses many issues above and beyond just glycemic control, however, and should be included in the discussion on care. For instance, proper timing of mealtime insulin, assuring inpatient diabetes self-management education, and discharge planning are also essential components of care. The topics of quality and safety with regard to inpatient DM have been the subjects of extensive study and review. A number of institutions and societies have published descriptions of their quality improvement programs and have reported on various methods and provided guidelines aimed at enhancing management of inpatient DM [5,6,15-17]. The authors of this study first published an overview of their hospital’s inpatient DM care in 2007 [18]. Subsequently, they have been characterizing the care of subsets of inpatients with DM with a focus on glucose management and insulin use, including care of patients who are postoperative and perioperative and patients who have solid organ transplants and solid organ malignancies [19-22]. In addition, provider attitudes and barriers to inpatient DM care have been studied, and care processes have been developed and analyzed for patients given inpatient insulin pump therapy [23-26]. Notwithstanding the large body of work in the literature regarding inpatient DM care, how successful have hospitals been in improving glycemic control or in the use of effective insulin therapies to treat hyperglycemia? Little longitudinal data have been published in answer to this question. Rather than focusing on a subset of inpatients here as they have previously done, the authors instead return to providing an updated assessment of overall institutional care over time. Specifically analyzed were longitudinal changes in glycemic control and insulin use over a 4-year period that occurred within the context of institutional efforts to improve oversight of inpatient DM care.
Methods
▪ Facility description
The authors’ academic teaching hospital is a 268-bed facility located in the metropolitan Phoenix, Arizona. All adult general medical and surgical specialties are represented, including solid organ and bone marrow transplantation programs. The hospital does not provide inpatient care for obstetric or pediatric patients. Numerous accredited residency and fellowship programs are represented, and the facility serves as a training site for several allied health schools.
▪ Oversight of inpatient DM-related policies and practices
Beginning in 2006, a steering committee was formed to provide oversight of the hospital’s inpatient DM activities. In 2011, the committee became recognized by the institution and was granted subcommittee status, reporting to the institution’s hospital practice subcommittee. It is a multidisciplinary group with representation from endocrinology (including DM nurse educators), hospital internal medicine, general surgery, nutrition services, informatics, laboratory medicine, pharmacy, intensive and nonintensive care nursing, patient and staff education, and quality personnel. The charge of the Inpatient Diabetes Subcommittee (IDSC) has been to promote standards of care and safety and to improve outcomes and transitions of hospitalized patients with DM. The IDSC accomplishes its charge via a number of activities, including developing, implementing, and measuring the impact of strategies to enhance care; providing staff education; monitoring of clinical practice and regulatory guidelines; and oversight and development of policies and procedures.
▪ Policies and procedures for managing quality and safety of inpatient DM care
Multiple policies and procedures have been implemented to standardize management of inpatient care for DM and to assure patient safety at the authors’ institution. For instance, a number of policies have been written for glucose monitoring, hypoglycemia detection and treatment, insulin administration, and use of insulin pump and continuous glucose monitoring systems in the hospital. Insulin and bedside glucose monitoring are ordered electronically. Additionally, the electronic health record links bedside glucose monitors directly to the laboratory information system. Allied health education pertaining to DM is conducted regularly. Finally, any changes in procedures are transmitted electronically via newsletters. The IDSC monitors and analyzes high-risk scenarios, such as insulin administration errors and develops corrective action plans to mitigate events.
▪ Case selection
This analysis employed previously published methods for case selection, evaluation of glucose control, and assessment of insulin use in the hospital [18,21,27]. Briefly, we examined electronic hospital data for the calendar years from 2011 through 2014. This timeframe was selected because a new electronic health record was introduced in 2010; and after 2014, a new point-of-care technology was implemented to measure bedside glucose levels. Patients discharged with an International Classification of Diseases, 9th Revision, Clinical Modification diagnosis code for diabetes (Code 250.xx) were identified from the hospital’s electronic billing records. In keeping with our previous methods, this analysis included only patients who did not require a stay in the intensive care unit. Data collected included patients’ demographic characteristics, use of glucocorticoids, and casemix index as a measure of case complexity. The case-mix index used by the authors’ hospital is a measure of the relative cost or resources needed to treat the mix of patients and is calculated on the basis of the principal and secondary diagnoses, age, procedures performed, the presence of comorbidities and/or complications, discharge status, and sex [28]. Additionally, the primary inpatient service caring for the patient was obtained and categorized into 3 groups: hospital internal medicine (HIM), surgical, and other (e.g, neurology, internal medicine subspecialties, transplant).
▪ Assessment of glycemic control
Retrieval and analyses of inpatient glycemic data followed previously described methods [18- 22,27]. To summarize, point-of-care bedside glucose (POC-BG) data were analyzed as the means to assess inpatient glycemic control. The POC-BG values for the cases selected, as described above, were obtained from the linked laboratory information system. Measurements were performed with standardized instrumentation (Accucheck Inform, Roche Diagnostics). Commercial software (Medical Automation Systems) facilitates the interfacing of glucometer data with the electronic laboratory file. The patient-stay mean POC-BG was calculated for the entire length of stay for each patient. The percentages of hyperglycemic (glucose >180 mg/dL) and hypoglycemic (glucose<70 mg/dL) values in the POC-BG data were calculated by dividing the number of values per patient by the total number of bedside measurements per patient and then multiplying by 100 as previously described [18,19,21,22,27]. Hemoglobin A1c [HbA1c] was included when available.
▪ Assessment of inpatient insulin use
The best approach to managing hyperglycemia in noncritically ill inpatients is via a basal-bolus insulin program. This regimen uses a combination of long- or intermediate-acting insulin with a short- or rapid-acting insulin given with meals, supplemented by correction doses for high glucose values [29-32]. Use of correction insulin only (ie, sliding-scale insulin) without basal insulin results in ineffective glycemic control [29-33]. To analyze inpatient insulin use for various levels of hyperglycemia, the authors used previously published methods [18,19,21,22,27]. Only insulin actually administered to the patient was evaluated and was determined by linking to data in the inpatient electronic pharmacy records. The insulin types on formulary at the authors’ hospital were used in the analysis: basal, or long-acting insulin therapy (glargine or [neutral protamine Hagedorn] NPH); and short-acting, or rapid- or short-acting insulin (regular or aspart), if given as a prandial dose or as a correction dose, or both. Patterns of insulin administration were then classified as none, basal only, short-acting only, or basal plus short-acting. When identified in the data, premixed insulin was categorized as basal plus short-acting. As the value of intensifying insulin therapy is unclear in patients with short hospital stays, analysis was restricted as per the authors’ prior convention to cases where length of stay was 3 days or longer [18,19,21,22,27].
▪ Data analysis
The primary objective of this analysis was to provide a longitudinal assessment of inpatient DM care. Therefore, frequencies and proportions for categorical variables were determined. Mean (SDs) were calculated for continuous variables; and univariate analyses were conducted to compare the outcomes and demographic characteristics according to year of admission. Comparisons between the groups were based on the independence assumption, using the nonparametric Kruskal-Wallis test for continuous variables and the Pearson χ2 test for categorical variables. Insulin use was assessed overall. Insulin use was also specifically assessed in the patient group whose hyperglycemia frequency fell into the highest tertile of measurements because these cases should have had the greatest use of basal-bolus insulin therapy. Results with P<.05 were considered significant. The authors were interested in examining variables associated with patient- stay mean glucose. Additionally, variables that predicted use of basal-bolus insulin therapy were evaluated. These comparisons were tested, as was done previously, by using a generalized estimating equation (GEE) model to account for potential multiple observations (ie, hospitalizations) for a person [27]. Statistical analyses were performed using the software packages SAS Studio 3.4 (SAS Institute Inc) and R version 3.1.2 (The R Foundation).
Results
▪ Patient characteristics
There were 5,386 hospitalizations analyzed for DM patients who met the inclusion criteria (noncritically ill, length of stay ≥ 3 days). The mean patient age was 67 years, and most patients were men and white (Table 1). The mean case-mix index was approximately 2, length of stay was 8 days, and HbA1c was 6.9%. Glucocorticoids were administered to 39% of patients. Most patients were cared for on the HIM services, about 25% by one of the surgical specialties and the remainder by other inpatient specialties. The population remained stable over the 4-year analytic period, with no differences across years in age, sex, race, case-mix index, length of stay, or use of glucocorticoids. There was variation in HbA1c levels. The distribution of the inpatient services varied over time, although HIM did remain the principal service caring for DM patients in each year (Table 1).
| Year of Discharge | ||||||
|---|---|---|---|---|---|---|
| 2011 (N=1,320) | 2012 (N=1,354) | 2013 (N=1,354) | 2014 (N=1,358) | Total (N=5,386) | ||
| Characteristics | P Value | |||||
| Age, mean (SD), y | 67 (14.0) | 67 (14) | 67.0 (13) | 67 (13) | 67 (14) | 0.5 |
| Men, % | 61 | 61 | 61 | 62 | 61 | 0.94 |
| White, % | 87 | 89 | 86 | 88 | 87 | 0.74 |
| Case-mix index | 2.1 (1.7) | 2.2 (1.8) | 2.2 (1.7) | 2.2 (1.7) | 2.2 (1.7) | 0.54 |
| Length of stay, mean (SD), d | 7.9 (5.9) | 8.3 (6.6) | 7.9 (5.9) | 7.8 (5.4) | 8.0 (6.0) | 0.14 |
| Hemoglobin A1c, % | 6.8 (1.4) | 6.9 (1.2) | 6.8 (1.3) | 7.0 (1.4) | 6.9 (1.3) | 0.03 |
| Glucocorticoids, % | 38 | 37 | 41 | 39 | 39 | 0.46 |
| Inpatient service, % | <.01 | |||||
| Hospital internal medicine | 44 | 40 | 43 | 38 | 41 | |
| Surgical | 24 | 26 | 24 | 30 | 26 | |
| All others | 32 | 34 | 33 | 32 | 33 | |
| a Data are mean (SD) or no. (%), as applicable. | ||||||
Table 1. Characteristics of Inpatients with diabetes mellitus according to year of hospital dischargea (n=5,386 discharges)
▪ Changes in glycemic control
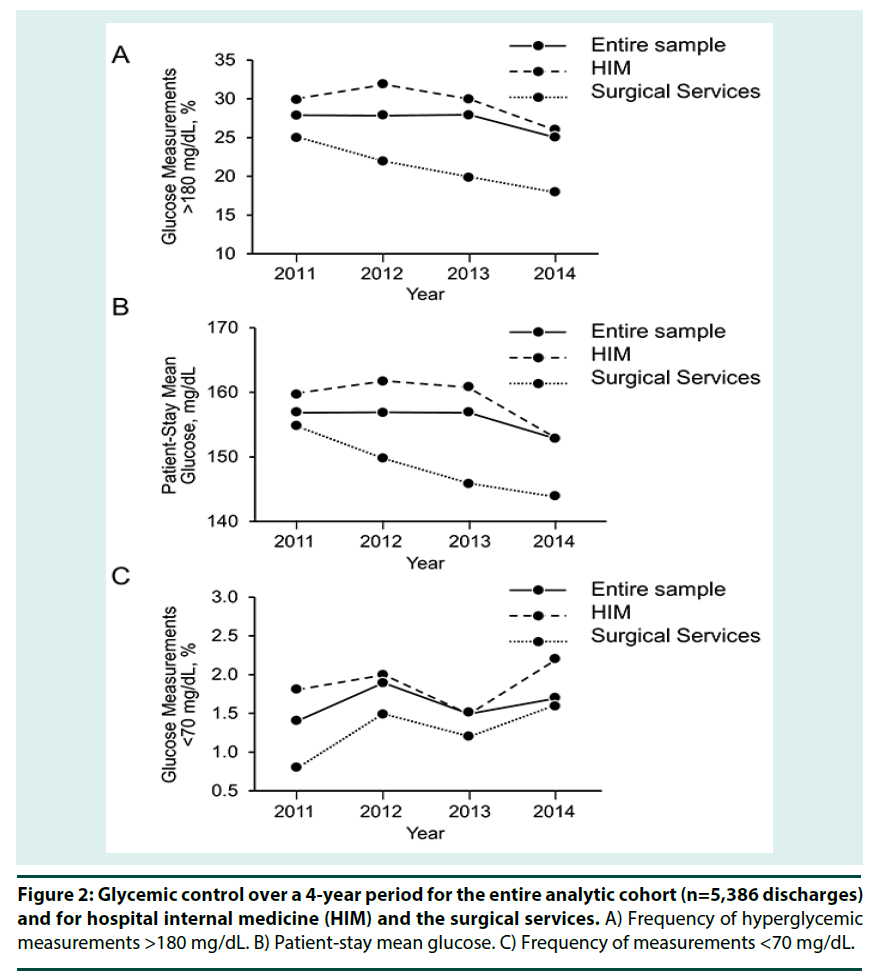
For the entire cohort, the frequency of hyperglycemia (percent of measurements that were >180 mg/dL) decreased from 28% in 2011 to 25% in 2014 (P=.02) (Figure 2A). Because HIM and surgical patients represented nearly two-thirds of inpatients with DM, the remainder of the analysis excluded patients on other services. For patients cared for on the HIM services, the percentage of values >180 mg/dL decreased from 30% to 26% (P=.02), and in the surgical services, the frequency decreased from 25% to 18% from 2011 through 2014 (P=.01). When patient-stay mean glucose values were analyzed, changes occurred in parallel with those seen with hyperglycemic frequency. For all patients and all years combined, a slight but significant decrease was noted from 2011 through 2014 (Figure 2B). In 2011, mean (SD) glucose was 157 mg/dL; and by 2014, it was 153 mg/ dL (P=.01). Among patients cared for on the HIM services, a significant decrease was seen: mean glucose was 160 mg/dL in 2011, declining to 153 mg/dL by 2014 (P<.01). Patient-stay mean glucose also improved significantly over time for the surgical services, decreasing from 155 mg/dL in 2011 to 144 mg/dL in 2014 (P<.01). Finally, the frequency of hypoglycemia (the percentage of POC-BG measurements <70 mg/dL) in the data was determined (Figure 2C). Hypoglycemia frequency varied during the 4-year period, and no definite patterns were seen. Significant variations in hypoglycemia data were seen for the entire cohort (P=.04). No change in hypoglycemia frequency was detected in the HIM data (P=.15). Hypoglycemic events were higher but not significantly so in the surgical patients, increasing from 0.8% to 1.6% (P=.07).
Figure 2: Glycemic control over a 4-year period for the entire analytic cohort (n=5,386 discharges) and for hospital internal medicine (HIM) and the surgical services. A) Frequency of hyperglycemic measurements >180 mg/dL. B) Patient-stay mean glucose. C) Frequency of measurements <70 mg/dL.
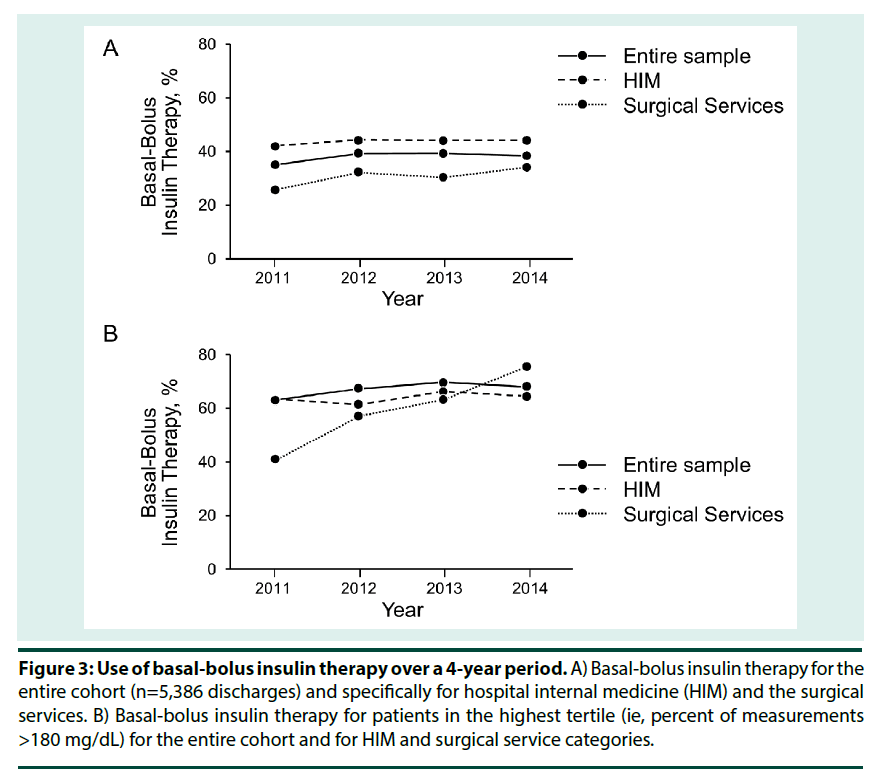
▪ Insulin use
There were no changes (P=.20) in basal-bolus insulin use over the 4 years for the entire cohort selected for analysis. No differences in use of basal-bolus insulin therapy were detected within the 4 years of data in either the HIM or surgical services (all, P ≥ .60) (Figure 3A). Use of basal-bolus insulin therapy was next evaluated in patients who had the most frequent occurrence of hyperglycemic measurements—those who were in the highest tertile of measurements (>180 mg/dL) (Figure 3B). These patients would have been candidates for more aggressive use of basal-bolus insulin treatment. In the entire sample set, the frequency of basal-bolus insulin use increased from 63% in 2011 to 69% in 2014, but the change was not significant (P=.33). In this subset of patients, no significant changes in use of basal-bolus insulin therapy were detected for the HIM patients (P=.57). However, in the surgical services, basal-bolus insulin therapy increased from 41% to 76% (P < .01).
Figure 3: Use of basal-bolus insulin therapy over a 4-year period. A) Basal-bolus insulin therapy for the entire cohort (n=5,386 discharges) and specifically for hospital internal medicine (HIM) and the surgical services. B) Basal-bolus insulin therapy for patients in the highest tertile (ie, percent of measurements >180 mg/dL) for the entire cohort and for HIM and surgical service categories.
▪ Variables associated with patient-stay mean glucose
GEE linear regression modeling was conducted to determine variables associated with patient-stay mean glucose among the HIM and surgical patients (Table 2). Increasing age, HbA1c, and frequency of glucose measurements >180 mg/dL were positively correlated with higher patient-stay mean glucose. Additionally, glucocorticoid use and use of basal-bolus insulin therapy were positively associated. Year of analysis was negatively associated with patient-stay mean glucose so that by 2014 mean glucose was significantly lower than in 2011. Case-mix index, race/ethnicity, and sex were not significantly correlated (Table 2).
| Characteristic | Estimate | SE | 95% CI | P Value |
|---|---|---|---|---|
| Age, y | 0.07 | 0.03 | 0.02 to 0.12 | <.01 |
| Case-mix index | −0.12 | 0.17 | −0.46 to 0.21 | 0.47 |
| Hemoglobin A1c, % | 0.74 | 0.29 | 0.17 to 1.31 | <.01 |
| Glucose measurements >180, % | 1.32 | 0.02 | 1.28 to 1.36 | <.01 |
| White (vs. other) | 0.67 | 1.08 | −1.45 to 2.80 | 0.53 |
| Women (vs. men) | −1.13 | 0.66 | −2.43 to 0.17 | 0.09 |
| Glucocorticoids (vs. none) | 2.22 | 0.73 | 0.79 to 3.66 | <.01 |
| Basal-bolus insulin (vs. other therapy) | 8.71 | 1.32 | 6.12 to 11.31 | <.01 |
| Year of discharge (vs. 2011) | ||||
| 2012 | −1.49 | 0.92 | −3.30 to 0.31 | 0.1 |
| 2013 | −1.10 | 0.91 | −2.88 to 0.68 | 0.22 |
| 2014 | −2.14 | 0.89 | −3.89 to −0.39 | 0.02 |
| Surgery (vs. hospital internal medicine) | 1.08 | 0.62 | −0.14 to 2.30 | 0.08 |
Table 2. Variables associated with patient-stay mean glucose
▪ Variables associated with use of basalbolus insulin therapy
GEE logistic regression modeling was used to evaluate for variables associated with the use of basal-bolus insulin therapy among the HIM and surgical patients (Table 3). Each year increase in age resulted in a very slight but significant decrease in use of basal-bolus insulin. Every unit increase in case-mix index increased the odds of treatment by 8%. Each HbA1c increase of 1% was associated with a 98% increase in the use of basal-bolus insulin treatment. Every 1% increase in the frequency of glucose measurements >180 mg/dL increased the use by 3%. Women also had a 26% lower chance of receiving basal-bolus insulin. After adjusting for the other variables in (Table 3), basal-bolus insulin therapy increased over time, such that by the year 2014, the odds of administration rose by 45% compared to 2011. After adjusting the other variables in the table, the odds of basal-bolus insulin therapy were 39% less in the surgical services compared with HIM.
| Characteristic | Odds Ratio | 95% CI | P Value |
|---|---|---|---|
| Age, y | 0.99 | 0.98-0.99 | <.01 |
| Case-mix index | 1.08 | 1.01-1.16 | 0.02 |
| Hemoglobin A1c, % | 1.98 | 1.78-2.21 | <.01 |
| Glucose measurements >180, % | 1.03 | 1.02-1.03 | <.01 |
| White (vs. other) | 0.88 | 0.62-1.25 | 0.47 |
| Women (vs. men) | 0.74 | 0.59-0.93 | 0.01 |
| Glucocorticoids (vs. none) | 1.23 | 0.99-1.53 | 0.06 |
| Year of discharge (vs. 2011) | |||
| 2012 | 1.33 | 1.00-1.77 | 0.05 |
| 2013 | 1.28 | 0.96-1.71 | 0.09 |
| 2014 | 1.45 | 1.08-1.95 | 0.01 |
| Surgery (vs. hospital internal medicine) | 0.61 | 0.49-0.76 | <.01 |
Table 3. Variables associated with use of basal-bolus insulin therapy
Discussion
DM, which is epidemic in US hospitals [1], has a considerable financial impact on hospital systems and accounts for a substantial number of inpatient hospital days [2]. Additionally, inpatient DM care is complex and must include provisions for glucose monitoring and control, hypoglycemia risk management, proper application of insulin therapy, discharge planning, patient and staff education, and developing processes for high-risk and unusual scenarios (eg, use of insulin pump therapy in the hospital). Quality improvement measures and care must also align with clinical practice guidelines that have emerged over recent years. Although all of the above factors must be considered in the care of hospitalized patients with DM, hyperglycemia has been a major focus of conversations about management. Numerous societies have recommended protocols for effective management of hyperglycemia, and consensus advocates good glucose control in the hospital to optimize patient outcomes [5,6,14,34]. The Joint Commission has developed guidelines to assist hospitals in achieving certification in inpatient DM care [35]. Although many institutions—including that of the authors of this report—have published descriptions of their quality improvement efforts, little is known about the success of these initiatives, and institutions need to begin the process of assessing the effectiveness of their glucose management programs over time. Since the last published analysis, the authors’ hospital has made strides toward developing high-level oversight of its inpatient population with DM [18]. A multidisciplinary committee endorsed by the institution was formed; and policies and guidelines related to glucose monitoring, insulin administration, and hypoglycemia management were reviewed and updated. Computerized order entry was established, provider attitudes towards inpatient DM care were evaluated, and attention was focused on care of populations with specific diagnoses (eg, transplant or cancer). In this analysis, the authors returned to examining overall glycemic control and insulin management at the institutional level as a means to assess institutional progress. This report summarizes 4-year data regarding changes in glucose control and insulin use in noncritically ill patients. Additionally, data from HIM and surgical services were examined, and variables associated with both glycemic control and basal-bolus insulin therapy were evaluated.
To our knowledge, this is the first analysis that has assessed demographic characteristics, glycemic control, or insulin use over time for inpatients with DM. During the 4 years, there was some variation in HbA1c, but otherwise age, sex, race/ ethnicity, case-mix index, and glucocorticoid use remained constant. There were some differences in the relative proportions in the services to which patients were assigned, but throughout the analytic period, nearly two-thirds of patients with DM were consistently cared for either by HIM or one of the surgical services. The overall stability in demographic characteristics and disease severity indicates that at least for now, adaptive redesign of inpatient DM education or care processes to accommodate a changing patient demographic may not be required. For glycemic control, slight but significant decreases in hyperglycemia frequency and in patient-stay mean glucose were seen over time. After adjusting for other variables and limiting the analysis to just HIM and surgical patients, a significant decrease in patient-stay mean glucose was confirmed by year 2014. Although significant, these modest improvements in glucose control may not have an impact on outcomes such as length of stay, surgical site-infection rates, or mortality. The improvements in glycemic control occurred without a simultaneous, excessive increase in the risk of hypoglycemic events by 2014. Mean glucose and hyperglycemic values remained well below benchmark data [36]. The data here indicate that the institution as a whole is moving in a positive direction with glycemic control for inpatients with DM. No changes in overall use of basal-bolus insulin therapy occurred over the 4 years. When only those patients who had the highest frequency of hyperglycemic measurements were considered, a significant increase in use of this regimen was observed for the surgical patients. This increase was very likely due to interventions that specifically targeted these services, beginning in 2011 [22,37]. However, after adjusting for other variables, the odds of basal-bolus insulin therapy were still significantly lower for surgical than for HIM patients, indicating that efforts to improve care in the surgical services must continue. In adjusted analysis, variables associated with patient-stay mean glucose included increasing age, higher HbA1c at admission, frequency of hyperglycemia, and use of glucocorticoids. The observation that basal-bolus insulin therapy positively correlated with mean glucose is an indication that practitioners were responding to observed hyperglycemic episodes. In addition to the service type and year of discharge, other variables positively associated with basal-bolus insulin therapy were case-mix index (a reflection of complexity of patient care), HbA1c (a reflection of historical outpatient glycemic control), and the frequency of hyperglycemic measurements >180 mg/dL. Increasing age was associated with slightly less use of basal-bolus insulin, but the difference was small and may not be clinically important. The observation that women were provided less access to recommended treatment requires further investigation. It should be noted that approximately 40% of patients overall with the highest frequency of hyperglycemia still did not receive basal-bolus insulin. The above results could be used to develop care pathways that anticipate the need for more intensive hyperglycemic therapy earlier in the hospital stay. For instance, it should be anticipated that patients who present with greater acuity, the need for glucocorticoids, or higher HbA1c levels would need basal-bolus insulin, which could then be started earlier in the hospitalization. There are limitations to the current analysis. First, it represents data from a single institution, so observations derived cannot be generalized to other facilities. Second, this analysis addressed only the noncritically patient population, and additional study is needed on how DM care is being delivered in the critically ill population. Third, data on outpatient DM therapy was not readily available and could have provided additional information as to the need for inpatient insulin treatment. Finally, the authors cannot say yet whether the time and investment made in developing a program of overseeing care for the general inpatient DM population has yielded any positive dividends on outcomes, including lower costs and patient and staff satisfaction with the care delivered. Despite the limitations, few institutions have reported longitudinal data on the status of their inpatient glucose control efforts. This study provides insight into various aspects of DM care at the authors’ hospital over time, including demographic characteristics, glycemic control, and insulin-use data. Considerable study is still needed in the area of inpatient DM care to better understand how best to organize and deliver care to assure the best results for the patient and the health care system.
References
- Centers for Disease Control and Prevention. Age-adjusted percentage, adults with diabetes http://www.cdc.gov/diabetes/statistics/dmany/index.htm
- Matt Petersen. Economic costs of diabetes in the US in 2012. American Diabetes Association. Diabetes. Care. 36(4), 1033–1046 (2013).
- Jiang HJ, Stryer D, Friedman B et al. Multiple hospitalizations for patients with diabetes. Diabetes. Care. 26(5), 1421–1426 (2003).
- Dungan KM. The effect of diabetes on hospital readmissions. J. Diabetes. Sci. Technol. 6(5), 1045-52 (2012).
- Society of Hospital Medicine. Glycemic control implementation toolkit [Internet] http://www.hospitalmedicine.org/ResourceRoomRedesign/GlycemicControl.cfm
- American Association of Clinical Endocrinologists. AACE diabetes resource center [Internet] [cited 2017 Jul 12]. Available from: http://resources.aace.com/
- Finfer S, Chittock DR, Su SY et al. NICE-SUGAR StudyInvestigators. Intensive versus conventional glucose control in critically ill patients. N. Engl. J. Med. 360(13),1283–1297 (2009).
- Kalfon P, Giraudeau B, Ichai C et al. Tight computerized versus conventional glucose control in the ICU: a randomized controlled trial. Intensive. Care. Med. 40(2), 171–181 (2014).
- Akirov A, Grossman A, Shochat T et al. Mortality among hospitalized patients with hypoglycemia: insulin related and noninuslin related. J. Clin. Endocrinol. Metab. 102(2), 416–424 (2017).
- Krinsley JS. Glycemic variability and mortality in critically ill patients: the impact of diabetes. J. Diabetes. Sci. Technol. 3(6), 1292–1301 (2009).
- Krinsley JS. Glycemic variability: a strong independent predictor of mortality in critically ill patients. Crit Care Med. 36(11), 3008–3013 (2008).
- Egi M, Bellomo R. Reducing glycemic variability in intensive care unit patients: A new therapeutic target? J. Diabetes. Sci. Technol. 3(6), 1302–1308 (2009).
- Dungan KM, Binkley P, Nagaraja HN et al. The effect of glycaemic control and glycaemic variability on mortality in patients hospitalized with congestive heart failure. Diabetes. Metab. Res. Rev. 27(1), 85–93 (2011).
- Umpierrez GE, Hellman R, Korytkowski MT et al. Endocrine Society. Management of hyperglycemia in hospitalized patients in non-critical care setting: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 97(1), 16–38 (2012).
- Munoz M, Pronovost P, Dintzis J et al. Implementing and evaluating a multicomponent inpatient diabetes management program: putting research into practice. Jt. Comm. J. Qual. Patient. Saf. 38(5), 195–206 (2012).
- Mathioudakis N, Pronovost PJ, Cosgrove SE et al. Modeling inpatient glucose management programs on hospital infection control programs: an infrastructural model of excellence. Jt Comm J. Qual. Patient. Saf. 41(7), 325–336 (2015).
- Golden SH, Hager D, Gould LJ et al. A gap analysis needs assessment tool to drive a care delivery and research agenda for integration of care and sharing of best practices across a health system. Jt Comm. J. Qual. Patient. Saf. 43(1), 18–28 (2017).
- Cook CB, Castro JC, Schmidt RE et al. Diabetes care in hospitalized non-critically ill patients: more evidence for clinical inertia and negative therapeutic momentum. J. Hosp. Med. 2(4), 203–211 (2007).
- Chakkera HA, Weil JE, Castro J et al. Hyperglycemia during the immediate posttransplant period after kidney transplantation. Clin. J. Am. Soc. Nephrol. 4(4), 853–859 (2009).
- Werner KT, Mackey PA, Castro JC et al. Hyperglycemia during the immediate period following liver transplantation. Future. Sci. OA. 2(1), FSO97 (2016).
- Karlin NJ, Cheng M-R, Castro JC et al. Hyperglycemia among hospitalized cancer patients with coexisting diabetes mellitus. Diabetes. Manag. 5(6), 441–448 (2015).
- Cook CB, Apsey HA, Habermann EB et al. Update on a quality initiative to overcome clinical inertia in the postoperative care of inpatients with diabetes mellitus. Endocr Pract. 23(4), 498–500 (2017).
- Cook CB, McNaughton D, Braddy C et al. Management of inpatient hyperglycemia: assessing perceptions and barriers to care among resident physicians. Endocr. Pract. 13(2), 117–24 (2007).
- Cook CB, Jameson KA, Hartsell ZC et al. Beliefs about hospital diabetes and perceived barriers to glucose management among inpatient midlevel practitioners. Diabetes. Educ. 34(1), 75–83 (2008).
- Mackey PA, Thompson BM, Boyle ME et al. Insulin pump therapy use during surgery: an update on a quality initiative. J. Diabetes. Sci. Technol. 9(6), 1299–1306 (2015).
- Cook CB, Beer KA, Seifert KM et al. Transitioning insulin pump therapy from the outpatient to the inpatient setting: a review of 6 years' experience with 253 cases. J. Diabetes. Sci. Technol. 6(5), 995–1002 (2012).
- Mackey PA, Boyle ME, Walo PM et al. Care directed by a specialty-trained nurse practitioner or physician assistant can overcome clinical inertia in management of inpatient diabetes. Endocr. Pract. 20(2), 112–119 (2014).
- State of California, Office of Statewide Health Planning and Development. Case Mix Index https://www.oshpd.ca.gov/documents/HID/CaseMixIndex/ExampleCalculation.pdf
- Theilen BM, Gritzke KA, Knutsen PG, et al Inpatient glycemic control on the vascular surgery service. Endocr. Pract. 14(2), 185–191 (2008).
- Umpierrez GE, Smiley D, Hermayer K et al. Randomized study comparing a basal-bolus with a basal plus correction insulin regimen for the hospital management of medical and surgical patients with type 2 diabetes: basal plus trial. Diabetes. Care. 36(8), 2169–2174 (2013).
- Umpierrez GE, Smiley D, Jacobs S et al. Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes undergoing general surgery (RABBIT 2 surgery). Diabetes. Care. 34(2), 256–261 (2011).
- Umpierrez GE, Smiley D, Zisman A et al. Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes (RABBIT 2 trial). Diabetes. Care. 30(9), 2181-2186 (2007).
- Queale WS, Seidler AJ, Brancati FL. Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus. Arch. Inter. Med. 157(5), 545–452 (1997).
- American Diabetes Association. Diabetes care in the hospital. Diabetes. Care. 39(1), S99–S104 (2016).
- The Joint Commission. Certification in inpatient diabetes [Interent] http://www.jointcommission.org/certification/inpatient_diabetes.aspx
- Mackey PA, Boyle ME, Walo PM et al. Care directed by a specialty-trained nurse practitioner or physician assistant can overcome clinical inertia in management of inpatient diabetes. Endocr. Pract. 20(2), 112–119 (2014).
- Mackey PA, Boyle ME, Walo PM et al. Care directed by a specialty-trained nurse practitioner or physician assistant can overcome clinical inertia in management of inpatient diabetes. Endocr. Pract. 20(2), 112–119 (2014).