Review Article - Interventional Cardiology (2012) Volume 4, Issue 6
Examining the appropriateness of radial or femoral access: evidence from the RIVAL trial and clinical practice
- Corresponding Author:
- Tift Mann
Wake Heart & Vascular Associates
3000 New Bern Avenue, Suite G100
Raleigh, NC 27610, USA
Tel: +1 919 231 8253
Fax: +1 919 231 8186
E-mail: tiftmann@bellsouth.net
Abstract
Keywords
acute coronary syndromes, anticoagulants, coronary artery revascularization interventions, stents, transradial access
Currently more than 4 million percutaneous coronary interventions (PCIs) are performed each year in the world [Boston Scientific, Pers. Comm.]. Multiple studies over the past 20 years have shown that transradial access for PCI may have a distinct advantage over the transfemoral approach, in that access-site bleeding complications are virtually eliminated. As a result, transradial access has been accepted worldwide as a preferred strategy for PCI. Although there have been significant advances in antithrombotic therapy and interventional technique, bleeding complications remain a significant source of morbidity and mortality in patients undergoing PCI from femoral access. The purpose of the present paper is to review the evolution of contemporary femoral PCI techniques, and evaluate the role of transradial access in improving results.
Consequences of PCI-related bleeding
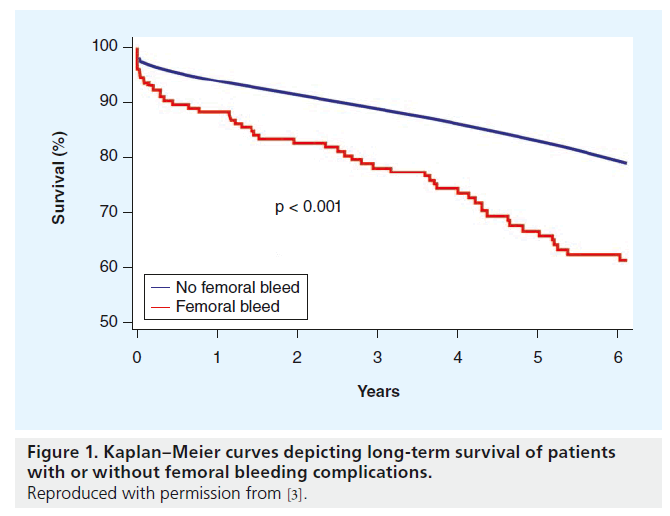
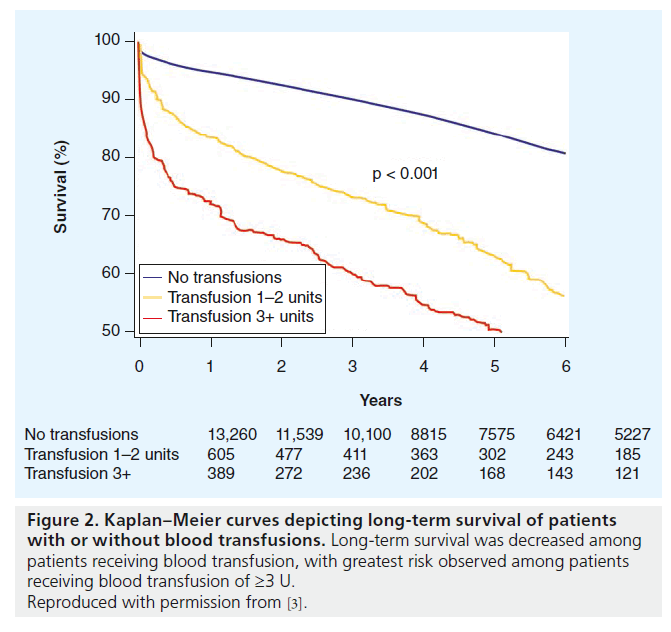
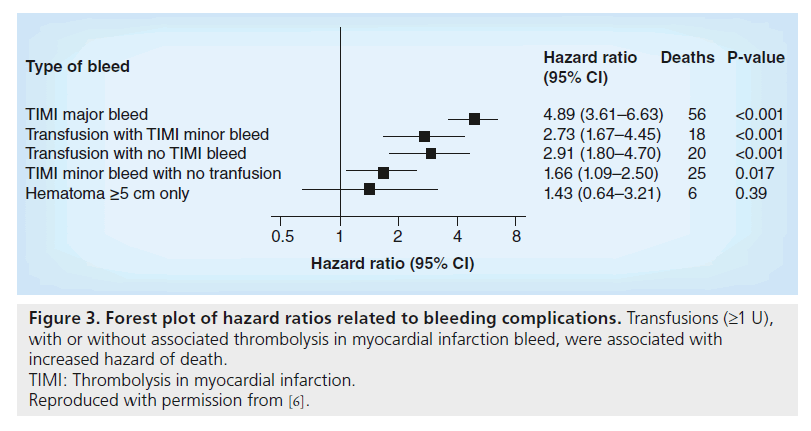
Pooled data from several major trials have demonstrated that bleeding complications in patients undergoing PCI are associated with long-term mortality. There is a two- to eight-fold increase in subsequent mortality in patients with acute coronary syndromes (ACS) undergoing PCI who experience major bleeding [1–5]. Survival actually continues to decline in these patients even weeks and months after the initial bleeding event (Figure 1). Transfusions themselves are an independent predictor of mortality, perhaps in part due to more adverse baseline characteristics in these patients [6–8]. Furthermore, there is a direct relationship between the number of transfusions and subsequent death (Figures 2 & 3).
Figure 1. Kaplan–Meier curves depicting long-term survival of patients with or without femoral bleeding complications.
Reproduced with permission from [3].
Figure 2. Kaplan–Meier curves depicting long-term survival of patients with or without blood transfusions. Long-term survival was decreased among patients receiving blood transfusion, with greatest risk observed among patients receiving blood transfusion of ≥3 U.
Reproduced with permission from [3].
Figure 3. Forest plot of hazard ratios related to bleeding complications. Transfusions (≥1 U), with or without associated thrombolysis in myocardial infarction bleed, were associated with increased hazard of death.
TIMI: Thrombolysis in myocardial infarction.
Reproduced with permission from [6].
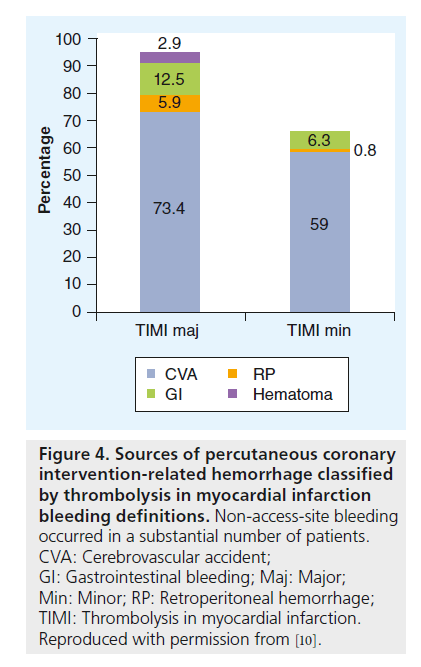
The femoral access site has been the major source of bleeding in these patients undergoing PCI. The source of bleeding may also be remote from the access site in 30–80% of patients (most commonly the gastrointestinal tract [Figure 4]) [9–11]. This non-access-site bleeding is also an important cause of mortality, with a higher hazard ratio than access bleeding [12]. While strategies that diminish bleeding risk have reduced the incidence of bleeding complications over the past decade, bleeding complications at the access site in particular, along with the mortality associated with them, remain a significant problem for the interventionalist.
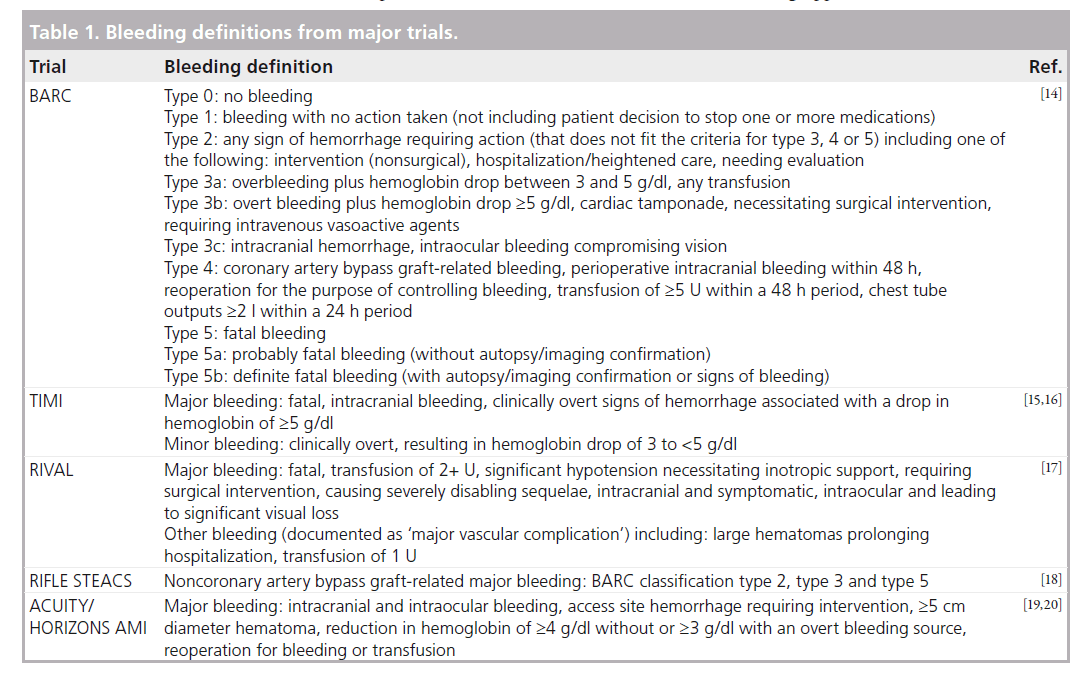
The assessment of bleeding risk and benefits of strategies to reduce bleeding has been impaired by the significant variation in the definition of bleeding between studies [13,14]. The different definitions are shown in Table 1 [14–20]. Thus, a ‘major’ bleed in one study may not qualify as ‘major’ in another. Furthermore, many studies have focused solely on mortality and have ignored the nonfatal sequelae of bleeding, including patient morbidity, prolongation of hospital length of stay, and the substantial increase in cost.
Figure 4. Sources of percutaneous coronary intervention-related hemorrhage classified by thrombolysis in myocardial infarction bleeding definitions. Non-access-site bleeding occurred in a substantial number of patients.
CVA: Cerebrovascular accident; GI: Gastrointestinal bleeding; Maj: Major; Min: Minor; RP: Retroperitoneal hemorrhage; TIMI: Thrombolysis in myocardial infarction. Reproduced with permission from [10].
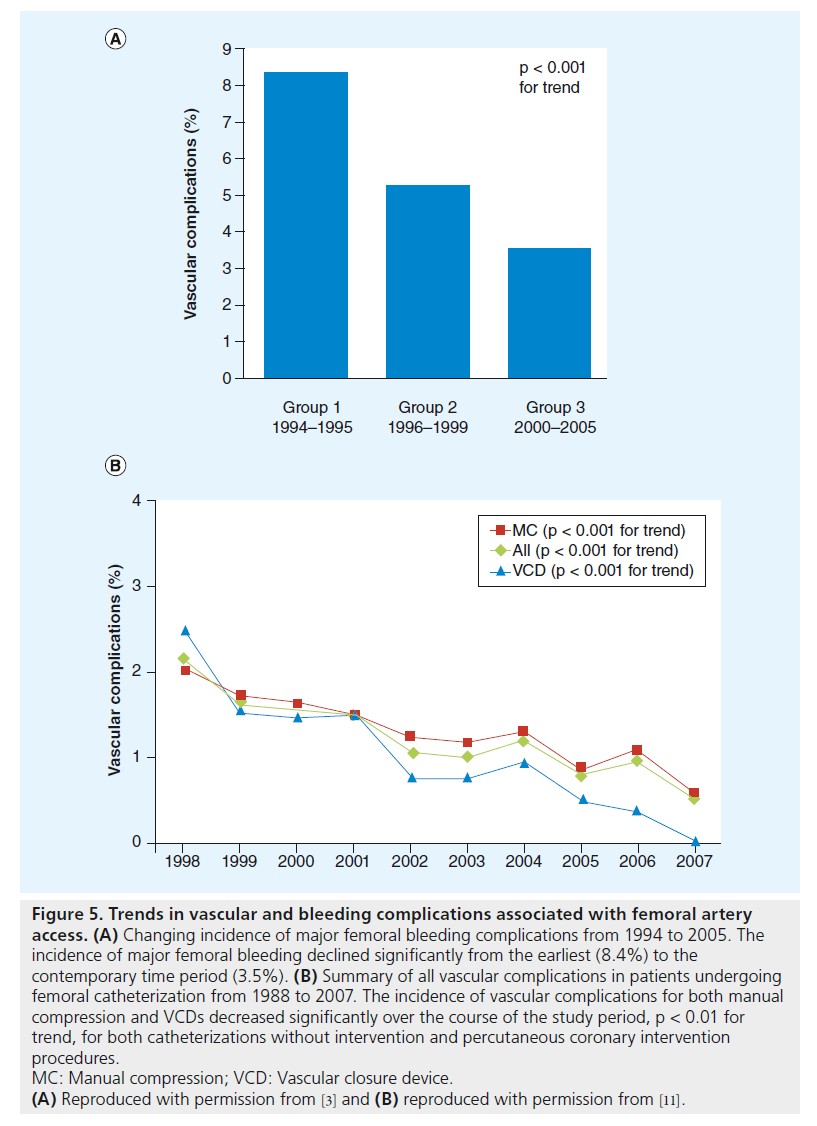
The introduction of the transradial technique for PCI stemmed from a desire to decrease these bleeding risks. The evolution of this technique has occurred during a period when there has also been an evolution in other strategies to reduce PCI-associated hemorrhage. Clearly, the implementation of bleeding avoidance strategies has had a beneficial effect in this regard (Figure 5A & B) [21]. The worldwide adoption of the transradial technique should thus be reviewed in the context of concurrent refinements in anticoagulation therapy and improvements in femoral access techniques.
Figure 5. Trends in vascular and bleeding complications associated with femoral artery access. (A) Changing incidence of major femoral bleeding complications from 1994 to 2005. The incidence of major femoral bleeding declined significantly from the earliest (8.4%) to the contemporary time period (3.5%). (B) Summary of all vascular complications in patients undergoing femoral catheterization from 1988 to 2007. The incidence of vascular complications for both manual compression and VCDs decreased significantly over the course of the study period, p < 0.01 for trend, for both catheterizations without intervention and percutaneous coronary intervention procedures.
MC: Manual compression; VCD: Vascular closure device.
(A) Reproduced with permission from [3] and (B) reproduced with permission from [11].
Anticoagulation therapy
Cardiologists now have a larger armamentarium available for interventional procedures, and selection of an optimal regimen is the cornerstone. Atherosclerotic plaque rupture with thrombosis is the pathophysiologic hallmark of ACS, and it is generally agreed that more potent antithrombotic regimens are required in these patients. However, ischemic protection has been obtained with the high price of bleeding complications, and these complications are a strong predictor of increased mortality and other major adverse coronary events.
There has been a significant reduction in bleeding complications over the past decade due to alterations in adjuvant antithrombotic and antiplatelet therapies [9–11,21–23]. Perhaps the most important has been a reduction in the use of intravenous glycoprotein IIb/IIIa inhibitors and high-dose unfractionated heparin. Although current European and American guidelines recommend initiation of dual antiplatelet therapy (aspirin plus clopidogrel, prasugrel or ticagrelor) as soon as possible after the diagnosis of ACS and preferably prior to catheterization, intravenous glycoprotein IIb/IIIa use has been replaced in many patients by oral antiplatelet agents [23]. However, it should be emphasized that the risk of femoral access bleeding is increased with any antiplatelet therapy.
A second major factor in the reduction of access-site bleeding complications has been the increasing use of bivalirudin. A metanalysis of four randomized studies performed before the widespread use of clopidogrel pretreatment (n = 11,638) showed a significant reduction in the combined event rate of death, myocardial infarction, revascularization and major bleeding with bivalirudin compared with heparin plus a glycoprotein IIb/IIIa inhibitor (7.8 vs 10.8%; p < 0.001) [24]. As a result of this and other studies, most interventions in the USA are currently performed using bivalirudin anticoagulation [25]. Other strategies have been evaluated worldwide to reduce bleeding complications. These include lower heparin dosing, reversal of heparin with protamine at the conclusion of the interventional procedure, and other drugs such as bivalirudin, enoxaparin and fondaparinux [26–29].
Improvements in femoral access
Technological improvements have also played a role in reducing the incidence of femoral bleeding complications. Reduction in the size of interventional devices allows the use of smaller guide catheters with a resultant smaller arteriotomy and less bleeding. In the USA, the use of access-site closure devices has been evaluated over the past decade. It has now become clear that the use of the access-site closure devices in procedures performed via the femoral artery result in faster hemostasis, shorter duration of bed rest and improved patient comfort. However, these devices have introduced a set of complications themselves, and whether they reduce the incidence of bleeding complications is controversial [21,22]. Indeed, current guidelines state that access-site closure devices should not be used routinely for the specific purpose of reducing femoral vascular complications [30].
Pre-RIVAL trial use of transradial access
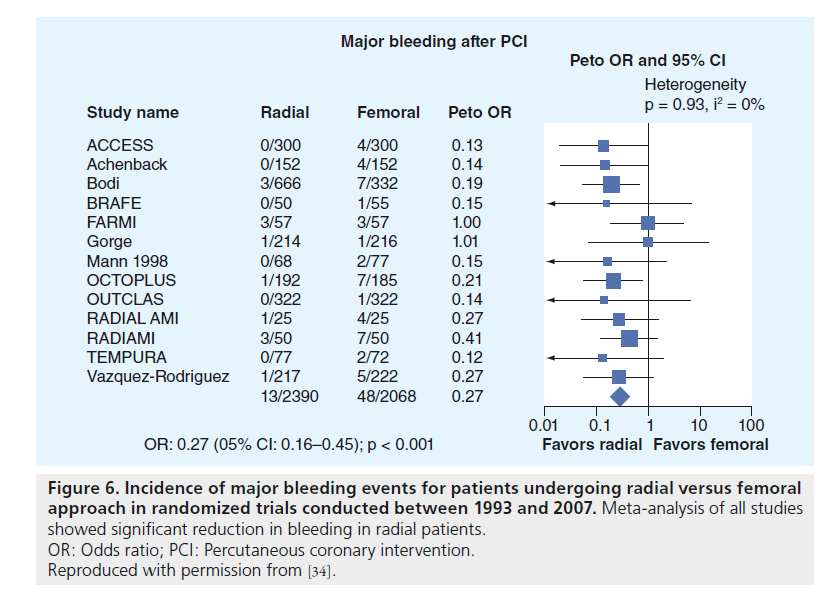
Since the first transradial interventional cases in the early 1990s, there has been a strong push by proponents of this access site for more widespread recognition of the value of this approach. Within several years of the first transradial interventions, prospective studies revealed a significant reduction in access-site complications with its use compared with femoral access (Figure 6) [31–34]. However, femoral access was the standard of care, and the significant learning curve associated with transradial access was a hurdle to general acceptance of the technique. Indeed, early studies suggested that this learning curve may be over 100 cases. Compounding this problem was the lack of available training, as very few fellowship programs taught the technique. It was the demonstration that femoral bleeding complications were associated with reduced survival that led operators to look seriously at the advantages of radial access.
Figure 6. Incidence of major bleeding events for patients undergoing radial versus femoral approach in randomized trials conducted between 1993 and 2007. Meta-analysis of all studies showed significant reduction in bleeding in radial patients.
OR: Odds ratio; PCI: Percutaneous coronary intervention.
Reproduced with permission from [34].
With experienced radial operators, procedural success was the same as from femoral access. With miniaturization of interventional tools, complex procedures could be carried out through the smaller catheters necessary with radial access. Even cases traditionally performed through large bore catheters, such as bifurcation stenting, left main stenting, saphenous vein graft stenting, and rotational atherectomy were safely performed transradially. Emergency procedures could be performed without prolongation of door-to-balloon times, and multiple early studies have demonstrated a reduction in mortality in patients undergoing transradial access for ST segment elevation myocardial infarction (STEMI) [35–42]. The reduction in vascular complications has been demonstrated in a large spectrum of other high-risk classes, such as women [43], obese patients [44] and octogenarians [45,46].
It also became apparent that the advantages of the transradial approach extended beyond the reduction of access bleeding. The ability of patients to ambulate immediately after the procedure as opposed to necessary bed rest after femoral procedures resulted in reduced morbidity of catheterization procedures. Quality-oflife studies revealed an overwhelming patient preference for the arm approach [47]. Early mobility and the absence of access complications resulted in reduced hospital length of stay and reduced cost [33,48]. Economic benefits alone (again paired with equality of procedural success) seemed to make the radial approach an obvious choice in the current age of controlling healthcare costs. Other advantages included reduced postprocedure requirements for nursing care and the possibility of outpatient procedures [49–53]. These benefits of transradial access have been acknowledged in the American College of Cardiology/American Heart Association guidelines [54], and recommendations regarding adoption of radial artery procedures and suggestions regarding training and adoption have recently been published by the Society for Cardiovascular Angiography and Intervention [55]. The transradial approach is now accepted worldwide as an access for PCI, and there has been a recent ground swell of support in the USA.
The problems and complications of the transradial approach have been clarified. Radial artery spasm was an early deterrent, but this problem has largely been eliminated with intraarterial pharmacological agents, especially verapamil, prior to catheter insertion [56,57]. Postprocedure radial artery occlusion is virtually always asymptomatic, but the access site is lost for future procedures. It can largely be prevented by attentiveness to procedural details. All patients must receive adequate anticoagulation, even elective catheterizations, as low heparin doses are associated with an excessive incidence of radial occlusion [58,59]. Hemostasis devices should be applied using patent hemostasis and removed as quickly as possible [60,61]. Ulnar compression may reverse early radial occlusion [62]. Increased operator radiation exposure during radial procedures was an early concern, but numerous studies have shown no difference when compared with femoral procedures after completion of the learning curve [63,64].
The learning curve for transradial procedures is an issue, especially for interventionalists primarily trained from femoral access. However, worldwide meetings and numerous transradial courses provide learning opportunities. Most centers have now incorporated radial access as part of their training programs. Left radial access is associated with shorter fluoroscopy times, particularly for new operators [65]. Although access may be awkward, catheter manipulation is similar to femoral access when the procedure is performed from the right side of the table using Jutkins curves.
RIVAL trial
After almost 20 years of research in the area of transradial PCI, there was a need for a larger, multicenter, prospective, randomized trial. The potential bias of previous registries, single-center trials and retrospective metanalyses left a gap in the body of evidence supporting transradial intervention.
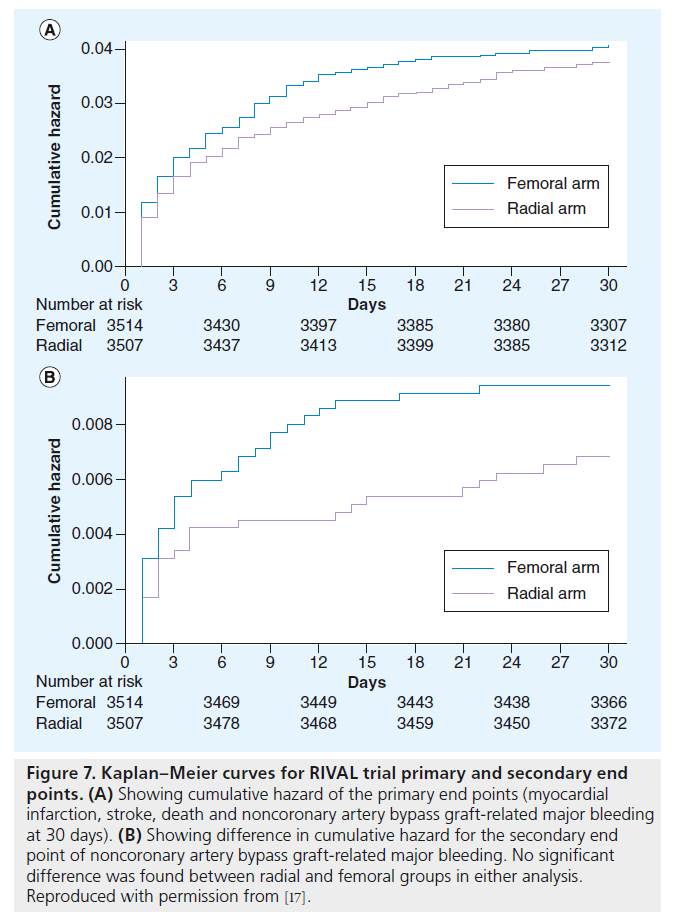
The purpose of the RIVAL trial was to determine whether radial access was superior to femoral access in patients with ACS who were undergoing coronary angiography with possible intervention [17]. Patients with STEMI and non- ST segment elevation ACS were randomized to have their procedure performed from radial or femoral access (1:1). The primary outcome was a composite of death, myocardial infarction, stroke, or non-coronary artery bypass graft (CABG)-related major bleeding at 30 days. Secondary outcomes were death, myocardial infarction, stroke and non-CABG-related major bleeding at 30 days. A total of 7021 patients were randomized in this large, multicenter, worldwide trial.
No significant difference in the primary outcome was observed in the study (3.7% radial group vs 4.0% femoral group, p = 0.50). There was a significant reduction in major vascular complications in the radial group (1.4% radial vs 3.7% femoral; p < 0.0001). These differences are shown in Figure 7. Access site crossover was higher in the radial group (7.6 vs 2.0% femoral, p = 0.0001). The authors concluded that radial and femoral approaches were both safe and effective for PCI, but that the lower rate of local vascular complications may be an indication for the radial approach in ACS patients.
Figure 7. Kaplan–Meier curves for RIVAL trial primary and secondary end points. (A) Showing cumulative hazard of the primary end points (myocardial infarction, stroke, death and noncoronary artery bypass graft-related major bleeding at 30 days). (B) Showing difference in cumulative hazard for the secondary end point of noncoronary artery bypass graft-related major bleeding. No significant difference was found between radial and femoral groups in either analysis. Reproduced with permission from [17].
The RIVAL trial has been the subject of substantial postpresentation scrutiny. The lack of significant reduction in the primary end point with radial access was contrary to previous studies, and some explanations have been proposed. One is the restrictive definition of major bleeding employed in the trial. Second, contemporary bleeding avoidance strategies used in the trial have reduced femoral access complications. Indeed, the incidence of femoral bleeding was low even in the presence of a relatively low percentage use of bivalirudin (most patients were treated with heparin), a 25% incidence of the use of IIb/IIIa inhibitors, and a 23% incidence of the use of closure devices. The authors themselves attributed this low incidence of femoral access bleeding to several factors, including the rigorous definition of bleeding used in the trial, a relatively low incidence of access-site bleeding compared with other sites (gastrointestinal, intracranial and pericardial constituted 60% of the major bleeding), as well as the relatively high-volume operators participating in the trial.
The RIVAL definition of major bleeding warrants further discussion. Major bleeding was defined as that which was: fatal; resulted in transfusion of two or more units of red blood cells; caused sufficient hypotension with need for inotropic support; needed surgical intervention; caused severely disabling sequelae; or was intracranial and symptomatic or intraocular and leading to significant visual loss. Less severe access bleeding, including that which required only one transfusion, was classified as a “major vascular complication”. The latter complications were significantly reduced in the trial (1.4% radial vs 3.7% femoral; p < 0.0001). An interesting post hoc analysis carried out by RIVAL investigators showed significantly less bleeding in the radial arm when the ACUITY trial major bleeding definition (Table 1) was applied. While this difference may be merely anecdotal, it validates the speculation that the bleeding definition contributed to the surprising results of the trial. Furthermore, since mortality from PCI-related hemorrhage may be late, it is likely that significant bleeding events that resulted in mortality after 30 days were not included in the primary end point.
Subgroup analysis revealed two important observations. First, there was a significant reduction in the primary end point (1.6% radial vs 3.2% femoral; p = 0.021) in centers with the highest radial volume (>142 radial PCI per operator per year). In these centers, major vascular complications occurred in only 0.7% of 1129 patients in the radial group (vs 4% in the femoral arm; p = 0.019). Secondly, in the 1958 patients with STEMI, the primary outcome was significantly reduced in the radial group (1.3% radial vs 3.2% femoral; p < 0.006). This observation makes clinical sense, since these patients are the most intensely anti-coagulated and should benefit from transradial access.
Several procedural characteristics were also evaluated. Although fluoroscopy time was significantly longer in the radial group, PCI procedural time, PCI contrast volume, length of stay in the hospital, and persistent pain at the access site greater than 2 weeks were the same in both groups. Access site crossover was higher in the radial arm (7.6% radial vs 2.0% femoral; p < 0.0001), but crossover occurred in only 4.4% in the highest tertile radial PCI group. A higher percentage of patients preferred radial access for their next procedure (90% radial vs 51% femoral; p < 0.0001).
Debates at major meetings have focused on interpretation of the results of the RIVAL trial. Proponents of the femoral approach have argued that it is not necessary to learn the transradial technique because of the low incidence of major bleeding in the femoral group. Radialists have countered, emphasizing the reduction in “major vascular complications”, as well as the subgroup analyses demonstrating radial benefit, particularly in patients with STEMI. A weakness in the latter argument is that an operator needs to be proficient in the technique to show benefit. Thus, like many major trials, the results of RIVAL have raised as many questions as it answered.
RIFLE trial
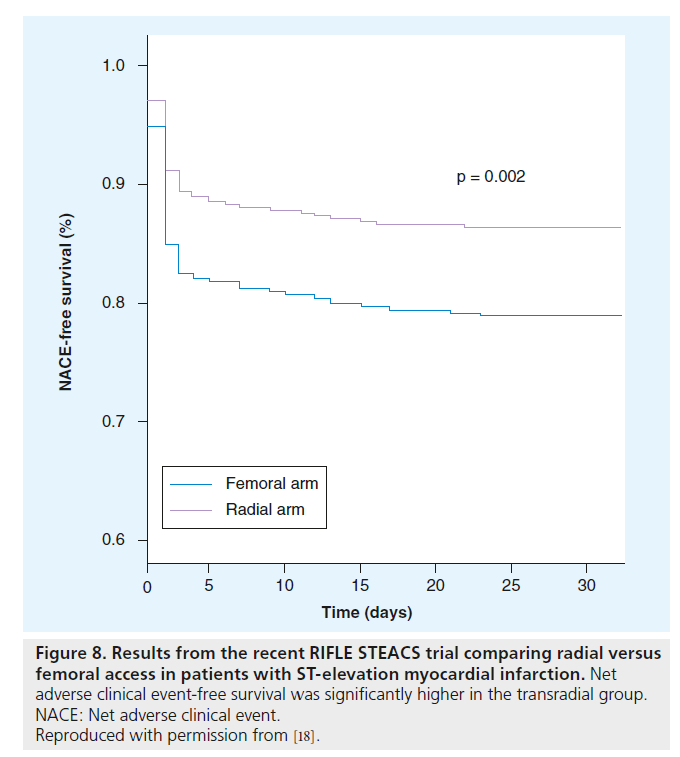
The recently presented RIFLE trial was a prospective, randomized study evaluating radial versus femoral patients in STEMI [18]. A total of 1001 patients were enrolled at four Italian centers. Major adverse cardiac events plus non- CABG bleeding were determined at 30 days. In this study, non-CABG-related bleeding was defined as type 2, 3 and 5 of the BARC classification, rather than the more restrictive definition in the RIVAL trial. Both MACCE and non-CABG-related bleeding were significantly reduced in the trial, and survival was significantly higher in the radial arm (Figure 8). Most importantly, cardiac death was reduced from 9.2% in the femoral group to 5.2% in the radial group (p = 0.02). There was a 47% reduction in access-site-related bleeding complications (6.8% femoral vs 2.6% radial; p = 0.002).
Figure 8. Results from the recent RIFLE STEACS trial comparing radial versus femoral access in patients with ST-elevation myocardial infarction. Net adverse clinical event-free survival was significantly higher in the transradial group. NACE: Net adverse clinical event. Reproduced with permission from [18].
The operators in the RIFLE trial were experienced radialists, and the results support the substudy observations of the RIVAL trial. Crossover from radial to femoral was required in 4.7% of patients. Evaluation of adjunctive pharmacology reveals a low use of bivalirudin similar to RIVAL. However, an important difference was the more frequent use of glycoprotein IIb/IIIa inhibitors (68.6% RIFLE vs 32.8% RIVAL). On the basis of these two studies, as well as the previous nonrandomized trials, radial access has the potential to reduce access-site bleeding complications, and also mortality, in patients with STEMI.
Operator experience
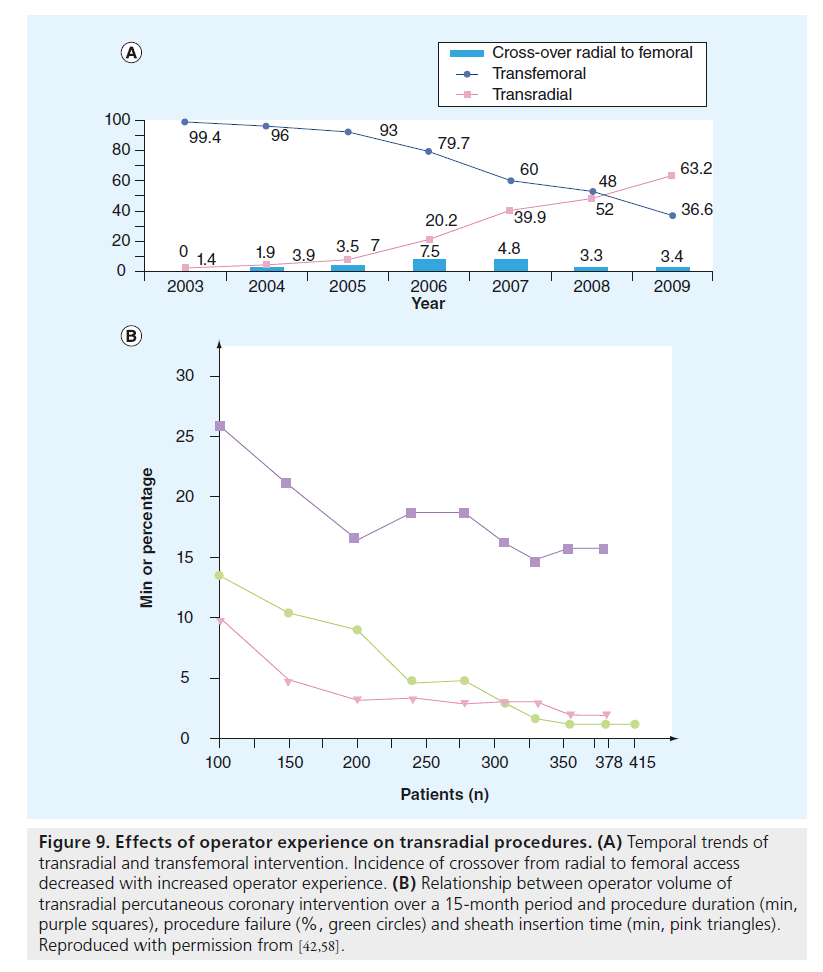
A huge variable in all transradial trials is operator experience. Radial access involves a unique set of skills, and operators must complete a learning curve before becoming skilled with the technique. The length of the learning curve has been debated, and patients with ACS, especially STEMI, present a particularly challenging population. Proficiency with the transradial technique is required to realize its maximal benefits, and it may take years for an institution (or region) to transition from default femoral to radial access [36]. While the number of required cases for expertise is variable, the eventual decrease in crossover rate is a marker of operator experience (Figure 9A & B) [42].
Figure 9. Effects of operator experience on transradial procedures. (A) Temporal trends of transradial and transfemoral intervention. Incidence of crossover from radial to femoral access decreased with increased operator experience. (B) Relationship between operator volume of transradial percutaneous coronary intervention over a 15-month period and procedure duration (min, purple squares), procedure failure (%, green circles) and sheath insertion time (min, pink triangles). Reproduced with permission from [42,58].
The importance of operator experience was clearly demonstrated in the RIVAL trial, as a significant reduction in the primary outcome was seen only in the highest tertile PCI volume group. The access site crossover rate is a useful indicator of radial proficiency. Thus, in the RIVAL trial, crossover occurred in 4.4% of patients in the highest tertile group, as opposed to 9.7% in the intermediate tertile and 8% in the lowest tertile. In the RIFLE trial, crossover from radial to femoral occurred in only 4.7% of patients, reflecting the radial experience of these operators.
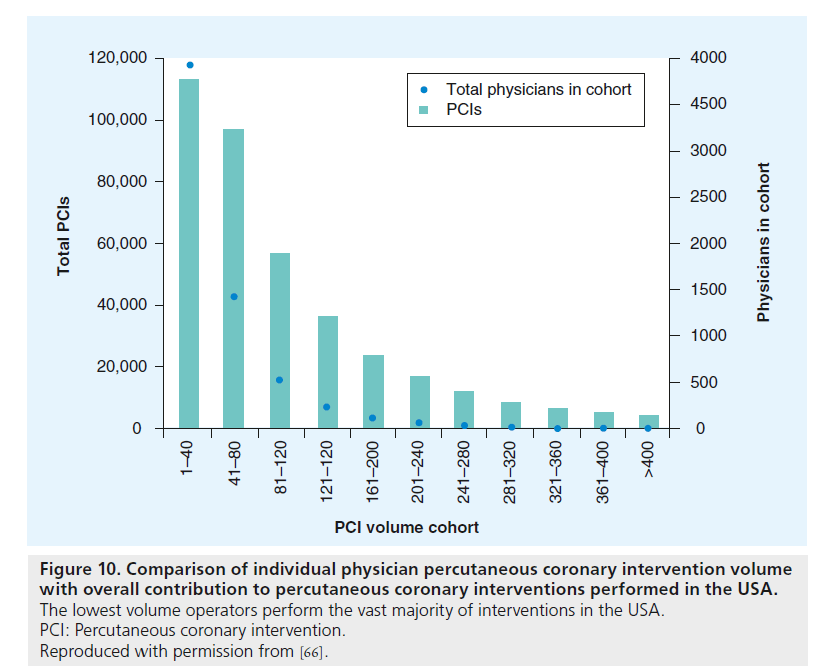
These data raise important issues for interventionalists in the USA. Although transradial training has now been adopted as part of many fellowship programs, most interventionalists in the USA have limited transradial experience. Indeed, less than 1% of these interventionalists perform greater than 40% of cases via the radial artery [9]. This is further compounded by the relatively low individual operator volume in this country (Figure 10) [66]. As research continues to demonstrate transradial benefit in many important subgroups undergoing PCI (ACS, women, advanced age and low BMI), more interventionalists should become experienced, high-volume radial operators. In the USA, a commitment must be made to develop a physician training system that appropriately rewards both clinical outcomes and reduced costs. The adoption of the transradial approach should be a goal of all interventional practices.
Figure 10. Comparison of individual physician percutaneous coronary intervention volume with overall contribution to percutaneous coronary interventions performed in the USA. The lowest volume operators perform the vast majority of interventions in the USA. PCI: Percutaneous coronary intervention. Reproduced with permission from [66].
Future perspective
An important area for future research will be to expand relationships between patients with STEMI, high-volume centers, and transradial intervention. The state of North Carolina has implemented a STEMI program entitled ‘Reperfusion of Acute Myocardial Infarction in North Carolina Emergency Departments’. This program developed out of a need to streamline and standardize STEMI patient care with an eye for reducing time to treatment [67]. Within the first 3 months of its initiation, the program showed significant decreases in reperfusion time in almost all areas currently studied [68]. While the program was not created with radial specialists in mind, the flow of patients from low-volume to high-volume centers may be the perfect opportunity for this subset of patients to be brought to the most experienced transradial operators.
Another variable that warrants further clarification is the role of access-site selection in patients receiving contemporary anti-coagulation, specifically oral thienopyridines and bivalirudin.
Whether the transradial benefit seen in RIVAL and RIFLE can be demonstrated with the use of these drugs remains uncertain [69]. The results of the ongoing MATRIX trial should provide further answers regarding bivalirudin monotherapy [101]. The effectiveness of transradial access with bivalirudin in reducing all PCI-related bleeding is being tested in the ongoing EASY B2B trial [102]. Although the use of glycoprotein IIb/IIIa inhibitors has decreased in the past decade, there are clearly patient subsets in which their use is indicated, and radial access should be preferred in these cases [23].
Conclusion
Over the past 20 years, transradial access has moved from a controversial niche procedure to a potentially lifesaving technique. While the benefits of this approach are debatable in patients undergoing elective PCI, a definite mortality benefit is realized when the procedure is performed by experienced operators in patients with ACS, especially patients with STEMI.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Executive summary
Consequences of percutaneous coronary intervention-related bleeding
▪ Femoral access-site bleeding is a major risk of percutaneous coronary intervention (PCI) and is associated with increased mortality, especially in patients requiring transfusion.
Anticoagulation therapy
▪ Improved anticoagulant strategies in acute coronary syndrome patients, including the increased use of bivalirudin, have reduced PCI-associated bleeding in recent years.
Improvements in femoral access
▪ Technological advances with smaller guide catheters have reduced femoral access bleeding. The use of access-site closure devices remains controversial.
Pre-RIVAL trial use of transradial access
▪ Transradial becomes an accepted alternative access site for PCI that reduces bleeding complications, especially in patients with acute coronary syndromes.
RIVAL trial
▪ The RIVAL trial demonstrates no significant difference in the primary end point between radial and femoral access, but major vascular complications are reduced significantly in radial group. The subgroup analyses show intriguing trends for further study.
RIFLE trial
▪ Confirms previous observations that transradial access reduces mortality in acute myocardial infarction when the procedure is performed by experienced operators.
Operator experience
▪ There is a definite learning curve with the transradial approach, and maximum benefits are not realized without experience.
Future perspective
▪ Current data suggests the necessity for more experienced transradial operators in the USA.
References
Papers of special note have been highlighted as:
▪▪ of interest
- Eikelboom JW, Mehta SR, Anand SS, Xie C, Fox KAA, Yusuf S. Adverse impact of bleeding on prognosis in patients with acute coronary syndromes. Circulation 114, 774–782 (2006).
- Rao SV, Jollis JG, Harrington RA et al. Relationship of blood transfusions and clinical outcomes in patients with acute coronary syndromes. JAMA 292, 1555–1562 (2004).
- Doyle JB, Ting HH, Bell MR et al. Major femoral bleeding complications after percutaneous coronary intervention: incidence, predictors, and impact on long-term survival among 17,901 patients treated at the Mayo Clinic from 1994 to 2005. J. Am. Coll. Cardiol. Interv. 1, 202–209 (2008).
- Manoukin SV, Feit F, Mehran R et al. Impact of major bleeding on 30day mortality and clinical outcomes in patients with acute coronary syndromes: an analysis from the ACUITY trial. J. Am. Coll. Cardiol. 49, 1362–1368 (2007).
- Yatskar L, Selzer F, Cohen HA, Jacobs AK, Williams DO, Slater J. Access site hematoma requiring blood transfusions predicts mortality in patients undergoing percutaneous coronary intervention: data from the National Heart, Lung, and Blood Institute Dynamic Registry. Catheter Cardiovasc. Interv. 69, 961–966 (2007).
- Mehran R, Pocock S, Nikolsky E et al. Impact of bleeding on mortality after percuntaneous coronary intervention: results from a patient-level pooled analysis of the REPLACE-2 (randomized evaulation of PCI linking angiomax to reduced clinical events), ACUITY (acute catheterization and urgent intervention triage strategy), and HORIZONS-AMI (harmonizing outcomes with revascularization and stents in acute myocardial infaction) trials. J. Am. Coll. Cardiol. Interv. 4(6), 654–664 (2011).
- Kinnaird TD, Stabile E, Mintz GS et al. Incidence, predictors, and prognistic complications of bleeding and blood transfusions following percutaneous coronary interventions. Am. J. Cardiol. 92, 930–935 (2003).
- Nikolsy E, Mehran R, Sadeghi HM et al. Prognostic impact of blood transfusion after primary angioplasty for acute myocardial infarction: analysis from the CADILLAC (controled abciximab and device investigations to lower late angioplasty complications) trial. J. Am. Coll. Cardiol. 2(7), 624–632 (2009).
- Rao SV, Ou FS, Wang TY et al. Trends in the prevalence and outcomes of radial and femoral approaches to percutaneous coronary intervention: a report from the National Cardiovascular Data Registry. JACC Cardiovasc. Interv. 1, 379–386 (2008).
- Rao SV, Cohen MG, Kandzari DE et al. The transradial approach to percutaneous coronary intervention: historical perspective, current concepts, and future directions. J. Am. Coll. Cardiol. 55(20), 2187–2195 (2010).
- Applegate RJ, Sacrinty MT, Kutcher MA et al. Trends in vascular complications after diagnostic cadiac catheterization and percutaneous coronary intervention via the femoral artery. J. Am. Coll. Cardiol. Interv. 1(3), 317–326 (2008).
- Verheught FWA, Steinhubl SR, Hamon M et al. Incidence, prognostic impact, and influence of antithrombotic therapy on access and nonaccess site bleeding in percutaneous coronary intervention. JACC Cardiovasc. Interv. 4(2), 191–197 (2011).
- Steinhubl SR, Kastrati A, Berger PB. Variation in the definitions of bleeding in clinical trials of patients with acute cornary syndromes and undergoing percutaneous coronary interventions and its impact on the apparent safety of antithrombotic drugs. Am. Heart J. 154, 3–11 (2007).
- Mehran R, Rao SV, Bhatt DL et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the bleeding academic research consortium. Circulation 123, 2736–2747 (2011).
- Chesebro JH, Knatterud R, Roberts J et al. Thrombolysis in myocardial infarction (TIMI) trial, phase I: a comparison between intravenous tissue plasminogen activator and intravenous streptokinase. Clinical findings through hospital discharge. Circulation 76, 142–154 (1987).
- Bovill EG, Terrin ML, Stump DC et al. Hemorrhagic events during therapy with recombinant tissue-type plasminogen activator, heparin, and aspirin for acute myocardial infarction: results of the Thrombolysis in myocardial infarction (TIMI), Phase II Trial. Ann. Intern. Med. 115, 256–265 (1991).
- Jolly SS, Niemela K, Xavier D et al. Design and rationale of the RadIal Vs. femorAl access for coronary intervention (RIVAL) trial: a randomized comparison of radial versus femoral access for coronary angiography or intervention in patients with acute coronary syndromes. Am. Heart J. 161, 254–260 (2011).
- Romagnoli E, Biondi-Zoccai G, Sangiorgi G et al. Radial versus femoral randomized investigation in ST elevation acute coronary syndrome: the RIFLE-STEACS (Radial Versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome) study. J. Am. Coll. Cardiol. doi:10.1016/j. jacc.2012.06.017 (2012) (Epub ahead of print).
- Stone GW, Bertrand M, Colombo A et al. Acute catheterization and urgent intervention triage strategy (ACUITY) trial: study design and rationale. Am. Heart J. 148, 746–775 (2004).
- Mehran R, Brodie B, Cox DA et al. The harmonizing outcomes of revascularization and stents in acute myocardial infarction (Horizons-AMI) trial: study design and rationale. Am. Heart J. 156, 44–56 (2008).
- Marso SP, Amin AP, House JA et al. Associations between use of bleeding avoidance strategies and risk of periprocedural bleeding among patients undergoing percutaneous coronary intervention. JAMA 303, 2156–2164 (2010).
- Dauerman HL, Rao SV, Resnic F, Applegate RJ. Bleeding avoidance strategies: consensus and controversy. J. Am. Coll. Cardiol. 58(1), 1–10 (2011).
- Hanna EB, Rao S, Manoukian SV, Saucedo JF. The evolving role of glycoprotein IIb/IIIa inhibitors in the setting of percutaneous coronary interventions: strategies to minimize bleeding risk and optimize outcomes. J. Am. Coll. Cardiol. Interv. 3(12), 1209–1219 (2010).
- Stone GW, McLaurin BT, Cox DA et al. Bivalirudin for patients with acute coronary syndromes. N. Engl. J. Med. 355, 2203–2216 (2006).
- Stone GW, White HD, Ohman EM et al. Bivalirudin in patients with acute coronary syndromes undergoing percutaneous coronary intervention: a subgroup analysis from the Acute catheterization and urgent intervention triage strategy (ACUITY) trial. Lancet 369, 907–919 (2007).
- Yusuf S, Mehta SR, Chrolavicius S et al. Comparison of fondaparinux and enoxaparin in patients with acute coronary syndromes. N. Engl. J. Med. 354, 1464–1476 (2006).
- Mehta SR, Granger CB, Eikelboom JW et al. Efficacy and safety of fondaparinux versus enoxaparin in patients with acute coronary syndromes undergoing percutaneous coronary intervention: results from the OASIS-5 trial. J. Am. Coll. Cardiol. 50, 1742–1751 (2007).
- Parodi G, Migliorini A, Valenti R et al. Comparison of bivalirudin and unfractionated heparin plus protamine in patients with coronary heart disease undergoing percutaneous coronary intervention (from the Antithrombotic Regimens aNd Outcome [ARNO] trial). Am. J. Cardiol. 105, 1053–1059 (2010).
- Montalescot G, White HD, Gallo R et al. Enoxaparin versus unfractionated heparin in elective percutaneous coronary intervention. N. Engl. J. Med. 355, 1006–1017 (2006).
- Patel MR, Jneid H, Derdyn CP et al. Arteriotomy closure devices for cardiovascular procedures: a scientific statement from the American Heart Association. Circulation 122, 188–1893 (2010).
- Kiemeneij F, Laarman GJ, Odekerken D, Slagboom T, van der Wieken R. Randomized comparison of percutaneous transluminal coronary angioplasty by the radial, brachial and femoral approaches: the Access study. J. Am. Coll. Cardiol. 29(6), 1269–1275 (1997).
- Mann T, Cubeddu G, Bowen J et al. Stenting in acute coronary syndromes: a comparison of radial versus femoral access sites. J. Am. Coll. Cardiol. 32, 572–576 (1998).
- Mann T, Cowper PA, Petersen ED et al. Transradial coronary stenting: comparison with femoral access closed with an arterial suture device. Catheter Cardiovasc. Interv. 49, 150–156 (2000).
- Jolly SS, Amlani S, Hamon M, Yusuf S, Mehta SR. Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am. Heart J. 157, 132–140 (2009).
- Saito S, Tanaka S, Hiroe Y et al. Comparative study on transradial approach vs. transfemoral approach in primary stent implantation for patients with acute myocardial infarction: results of the test for myocardial infarction by prospective unicenter randomization for access sites (TEMPURA) trial. Catheter Cardiovasc. Interv. 59, 26–33 (2003).
- Philippe F, Larrazet F, Meziane T et al. Comparison of transradial vs. transfemoral approach in the treatment of acute myocardial infarction with primary angioplasty and abciximab. Catheter Cardiovasc. Interv. 61, 67–73 (2004).
- Chase AJ, Fretz EB, Warburton WP et al. Association of the arterial access site at angioplasty with transfusion and mortality: the M.O.R.T.A.L study (Mortality benefit Of Reduced Transfusion after percutaneous coronary intervention via the Arm or Leg). Heart 94, 1019–1025 (2008).
- Cantor WJ, Puley G, Natarajan MK et al. Radial versus femoral access for emergent percutaneous coronary intervention with adjunct glycoprotein IIb/IIIa inhibition in acute myocardial infarction – the RADIALAMI pilot randomization trial. Am. Heart J. 150, 543–549 (2005).
- DeCarlo D, Borelli G, Gistri R et al. Effectiveness of the transradial approach to reduce bleedings in patients undergoing urgent coronary angioplasty with GPIIb/IIIa inhibitors for acute coronary syndromes. Catheter Cardiovasc. Interv. 74, 408–415 (2009).
- Hetherington SL, Adam Z, Morley R et al. Primary percutaneous coronary intervention for acute ST-segment elevation myocardial infarction: changing patterns of vascular access, radial versus femoral artery. Heart 95(19), 1612–1618 (2009).
- Johnman C, Pell JP, Mackay DF et al. Clinical outcomes following radial versus femoral artery access in primary or rescue percutaneous coronary intervention in Scotland: Retrospective cohort study of 4534 patients. Heart 98, 552–557 (2012).
- Valgimigli M, Saia F, Guastaroba P et al. Transradial versus transfemoral intervention for acute myocardial infarction: a propensity score-adjusted and -matched analysis from the REAL (REgistro regionale AngiopLastiche dell’Emilia-Romagna) multicenter registry. J. Am. Coll. Cardiol. Interv. 5(1), 23–35 (2012).
- Pristipino C, Pelliccia F, Granatelli A et al. Comparison of access-related bleeding complications in women versus men undergoing percutaneous coronary catheterization using the radial versus femoral artery. Am. J. Cardiol. 99, 1216–1221 (2007).
- Cox N, Resnic FS, Popma JJ et al. Comparison of the risk of vascular complications associated with femoral and radial access coronary catheterization procedures in obese versus nonobese patients. Am. J. Cardiol. 94, 1174–1177 (2004).
- Caputo RP, Simons A, Giambartolomei A et al. Transradial cardiac catheterization in elderly patients. Catheter Cardiovasc. Interv. 51, 287–290 (2000).
- Achenbach S, Roper D, Kallert L et al. Transradial versus transfemoral approach for coronary angiography and intervention in patients above 75 years of age. Catheter. Cardiovasc. Interv. 72, 629–635 (2008).
- Cooper CJ, El-Shiekh RA, Cohen DJ et al. Effect of transradial access on quality of life and cost of cardiac catheterization: a randomized comparison. Am. Heart J. 138(3 Part 1), 430–436 (1999).
- Roussanov O, Wilson SJ, Henley K et al. Cost-effectiveness of the radial versus femoral artery approach to diagnostic cardiac catheterization. J. Invasive Cardiol. 19, 349–353 (2007).
- Amoroso G, Sarti M, Belluci R et al. Clinical and procedural predictors of nurse workload during and after invasive coronary procedures: The potential benefit of a systematic radial access. Eur. J. Cardiovasc. Nurs. 4, 234–241 (2005).
- Bertrand OF, De Larochelliere R, Rodes- Cabau J et al. A randomized study comparing same day home discharge and abciximab bolus only to overnight hospitalization and abciximab bolus and infusion after transradial coronary stent implantation. Circulation 114, 2636–2643 (2006).
- Dery JP, Simard S, Barbeau GR. Reduction of discomfort at sheath removal during transradial coronary procedures with the use of a hydrophilic-coated sheath. Catheter Cardiovasc. Interv. 54, 289–294 (2001).
- Gilchrist IC, Nickolaus MJ, Momplaisir T. Same-day transradial outpatient stenting with a 6-hr course of glycoprotein IIb/IIIa receptor blockade: A feasibility study. Catheter Cardiovasc. Interv. 56, 10–13 (2002).
- Jabara R, Gadesam R, Pendyala L et al. Ambulatory discharge after transradial coronary intervention: preliminary US single-center experience (Same-day TransRadial intervention and discharge evaluation, the STRIDE study). Am. Heart J. 156, 1141–1146 (2008).
- Levine GN, Bates ER, Blankenship JC et al. 2011 ACCF/AHA/SCAI guidelines for percutaneous coronary intervention. Catheter Cardiovasc. Interv. 58(24), e44–122 (2011).
- Caputo RP, Tremmel J, Rao S et al. Transradial arterial access for coronary and peripheral procedures: Executive summary by the transradial committee of the SCAI. Catheter Cardiovasc. Interv. 78, 823–839 (2011).
- Kiemeneij F, Vajifer B, Eccleshall S, Laarman G, Slagboom T, van der Wieken R. Evaluation of a spasmolytic cocktail to prevent radial artery spasm during coronary procedures. Catheter Cardiovasc. Interv. 58, 261–284 (2003).
- Varenne O, Jegou A, Cohen R et al. Prevention of arterial spasm during percutaneous coronary interventions through radial artery: the SPASM study. Catheter Cardiovasc. Interv. 58, 261–284 (2003).
- Spaulding C, Lefevre T , Funck F et al. Left radial approach for coronary angiography: results of a prospective study. Cathet. Cardiovasc. Diagn. 39, 365–370 (1996).
- Stella PR, Kiemeneij F, Laarman G, Odekerken D, Slagboom T, van der Wieken R. Incidence and outcome of radial artery occlusion following transradial artery coronary angioplasty. Cathet. Cardiovasc. Diagn. 40, 156–158 (1997).
- Sanmartin M, Gomez M, Rumoroso JR et al. Interruption of blood flow during compression and radial artery occlusion after transradial catheterization. Cathet. Cardiovasc. Interv. 70, 185–189 (2007).
- Pancholy S, Coppola J, Patel T, Roke-Thomas M. Prevention of radial artery occlusion – patent hemostasis evaluation trial (PROPHET study): a randomized comparison of traditional versus patency documented hemostasis after transradial catheterization. Cathet. Cardiovasc. Interv. 72, 335–340 (2008).
- Bernat I, Bertrand OF, Rokyta R et al. Efficacy and safety of transient ulnar artery compression to recanalize acute radial artery occlusion after transradial catheterization. Am. J. Cardiol. 107(11), 1698–1701 (2011).
- Neill J, Douglas H, Richardson G et al. Comparison of radiation dose and the effect of operator experience in femoral and radial arterial access for coronary procedures. Am. J. Cardiol. 106, 936–940 (2010).
- Bertrand OF, Arsenault J, Mongrain R. Operator vs. patient radiation exposure in transradial and transfemoral coronary interventions. Eur. Heart J. 29, 2577–2578 (2008).
- Sciahbasi A, Romagnoli E, Burzotta F et al. Transradial approach (left vs right) and procedural times during percutaneous coronary procedures: TALENT study. Am. Heart J. 161(1), 172–179 (2011).
- Maroney JM, Khan S, Powell W, Klein LW. Current operator volumes of invasive coronary procedures in Medicare patients: implications for future manpower needs in the catheterization laboratory. Catheter Cardiovasc. Interv. doi:10.1002/ccd.24366 (2012) (Epub ahead of print).
- Jollis JG, Mehta RH, Roettig ML, Berger PB, Babb JD, Granger CB. Reperfusion of acute myocardial infarction in North Carolina emergency departments (RACE): study design. Am. Heart J. 185, 851.e1–851.e11 (2006).
- Jollis JG, Roettig ML, Aluko AO et al. Implementation of a statewide system for coronary reperfusion for ST-segment elevation myocardial infarction. JAMA 298(20), 2371–2380 (2007).
- Hamon M, Rasmussen LH, Manoukian SV et al. Choice of arterial access site and outcomes in patients with acute coronary syndromes managed with an early invasive strategy: the ACUITY trial. EuroIntervention 5, 115–120 (2009).
▪▪ Large study clearly demonstrating that femoral access bleeding complications reduce survival postpercutaneous coronary intervention.
▪▪ Comprehensive summary of transradial research trends, from its inception as a technique to current research.
▪▪ Landmark trial demonstrating reduced access bleeding complications with transradial approach.
▪▪ Important meta-analysis confirming reduced access bleeding with the transradial access.
▪▪ First study demonstrating transradial efficacy in acute myocardial infarction.
101. Valgimigli M. Minimizing adverse haemorrhagic events by transradial access site and systemic implementation of angioX (Matrix). Sponsor: Italian Society of Invasive Cardiology; currently enrolling. http://clinicaltrials.gov/ct2/show/NCT01433627
102. Bertrand O. Early discharge after transradial stenting of coronary arteries in high-risk patients of bleeding (EASY-B2B). Sponsor: Laval University; currently enrolling. http://clinicaltrials.gov/ct2/show/NCT01084993