Special Issue Article - Imaging in Medicine (2011) Volume 3, Issue 3
Dose prescription, reporting and recording in intensity-modulated radiation therapy: a digest of the ICRU Report 83
Vincent Gregoire1 & Thomas R Mackie†1,21Center for Molecular Imaging and Experimental Radiotherapy & Radiation Oncology Department, Université catholique de Louvain, St-Luc University Hospital, Avenue Hippocrate 10, B-1200 Brussels, Belgium
2University of Wisconsin – Madison, Departments of Human Oncology, Medical Physics, 600 Highland Avenue, Madison, WI 53792, USA
- Corresponding Author:
- Thomas R Mackie
Center for Molecular Imaging and Experimental Radiotherapy & Radiation Oncology Department
Université catholique de Louvain, St-Luc University Hospital
Avenue Hippocrate 10, B-1200 Brussels, Belgium
E-mail: trmackie@facstaff.wisc.edu
Abstract
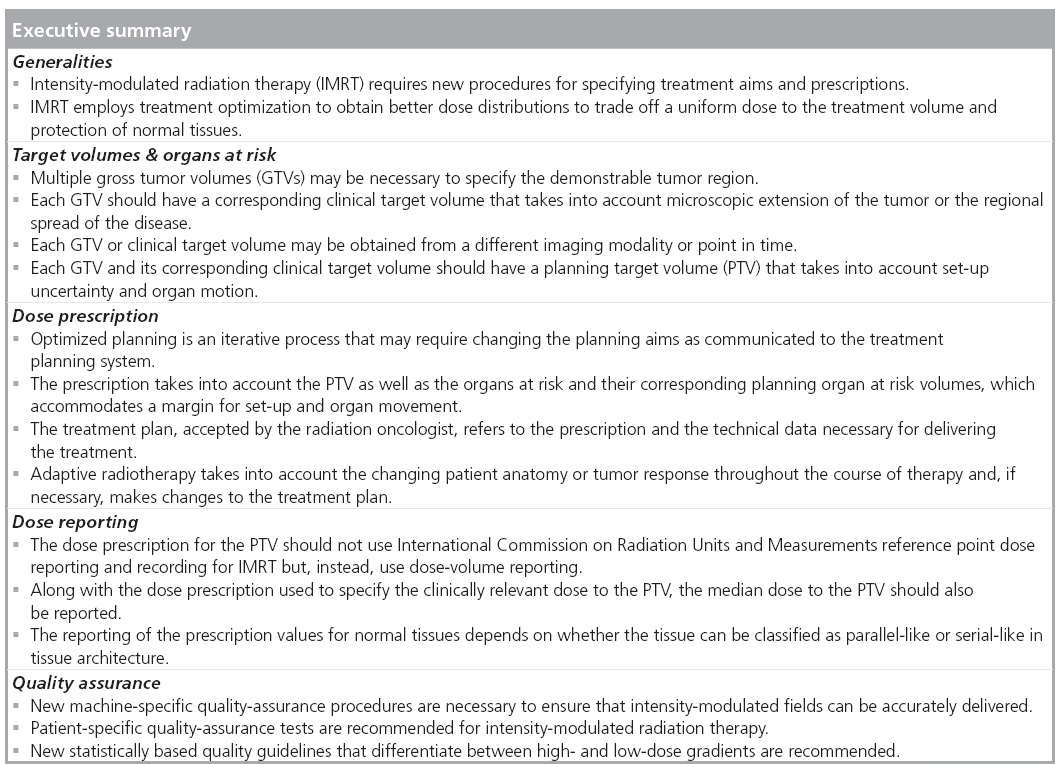
Rapid development in imaging techniques, including functional imaging, have fueled the drive to implement new methods of delivering 3D radiation therapy, such as intensity-modulated radiation therapy, with unprecedented accuracy. The International Commission on Radiation Units and Measurements (ICRU) Report 83 provides the information necessary to standardize techniques and procedures and to harmonize the prescribing, recording and reporting of intensity-modulated radiation therapy. Applicable concepts and recommendations in other International Commission on Radiation Units and Measurements reports concerning radiation therapy were adopted, and new concepts and recommendations were elaborated. In particular, additional recommendations were given on the selection and delineation of the target volumes and the organs at risk; concepts of dose prescription and dose-volume reporting have also been refined.
Keywords
clinical target volume ▪ dose constraint ▪ dose metric ▪ dose optimization ▪ gross tumor volume ▪ intensity-modulated radiation therapy ▪ organ at risk ▪ planning target volume ▪ radiation oncology
During the latter part of the last century, key innovations in radiotherapy technology, diagnostic imaging and computer science greatly modified the routine practice of radiotherapy, leading to substantial improvements in treatment delivery and outcome [1]. Before 1950, deeply seated tumors were treated with crossfired beams or rotation techniques to ensure an acceptably low dose to the normal tissues, especially skin, soft tissues and bone [2]. The introduction of deeply penetrating external photon beams, initially 60Co in the 1950s, and eventually, those from high-energy electron linear accelerators (linacs) in the 1960s, allowed the target dose to be increased without increasing normal-tissue morbidity.
During the 1970s and 1980s, treatment planning based on the use of planar diagnostic x-rays was widely implemented. A ‘simulator’, a specialized imaging system for radiotherapy employing an x-ray imaging system with the same geometry and degrees of freedom as a linac or rotational 60Co unit, became a widely used tool for planning treatment delivery. The bony anatomy was visible with planar x-rays, but the location of soft tissues, including tumors, was difficult to ascertain, and could often only be deduced from or correlated with bony landmarks, air cavities or contrast-enhanced images. The increasing use of x-ray CT in the 1980s, and MRI in the 1990s, enabled much more reliable 3D assessment of the location and extent of the disease. With these imaging improvements and advances in treatment- planning techniques, it became practical to design treatment fields that conformed more closely to the target volume.
Conventional radiotherapy was traditionally administered using a number of coplanar beams, usually of relatively uniform or smoothly varying intensity across the field. The use of low melting-point heavy cast-metal alloys allowed the treatment fields to be more easily custom shaped than with lead blocks. Multileaf collimators, designed to replace molded heavy metal blocks, made it easier to use multiple complexshaped fields, even in the same treatment session. Many linacs became equipped with electronic portal-imaging systems for verification of patient positioning, thus improving conformity between the planned and delivered doses. All of these technical innovations allowed more accurate treatment delivery to tumors, potentially allowing higher tumor doses, and thus increased local tumor control and/or reduced doses to the surrounding normal tissues.
When 3D planning techniques and special delivery systems to shape the field are used to reduce normal tissue damage close to the target volume, the technique is usually referred to as conformal radiotherapy or 3D-CRT. When compared with conventional approaches, 3D-CRT tends to use more treatment fields and a reduced dose to normal tissues abutting the target volume.
The concept of intensity-modulated radiation therapy (IMRT) arose because radiotherapy treatment-planning optimization algorithms predicted that the optimal radiation pattern from any single direction was typically nonuniform [3–5]. It was shown that a collective set of intensity-modulated beams from multiple directions could be designed to produce dose homogeneity similar to conventional radiotherapy within the tumor, but with superior conformality, especially for concave or other complexshaped target volumes, thereby sparing nearby normal tissues [6]. In addition, IMRT makes it easier to produce nonuniform dose distributions if required for treatment of a volume within another defined volume (also known as concomitant boost, or simultaneous integrated boost techniques) [7–9]. Rather than using uniform or constantly varying intensity distributions across each incident field, IMRT attempts to achieve more optimal dose distributions by varying the beam intensity (fluence) within each incident beam, usually by subdividing the beam into a number of smaller segments and modulating each to achieve its selected fluence contribution. Modulation of the beam is greatly facilitated by the use of multileaf collimators or binary collimators combined with a moving couch. The latter were specifically developed for IMRT.
In the context of radiotherapy delivery, the International Commission on Radiation Units and Measurements (ICRU) has been developing guidelines for prescribing, recording and reporting dose for radiation therapy. The first set of guidelines was published in 1978, and was subsequently updated in 1993 and 1999 to integrate the new development in radiotherapy, including electron and proton beams [10–15]. These documents recommended concepts and procedures for the delineation of the tumor, normal-tissue structures and margins to take into account potential tumor invasion, organ motion and set-up error. They also proposed recommendations for dose reporting and, to a lesser extent, for dose prescription and recording. With the wider use of IMRT, there was a need to update these reports to take into account the new opportunities offered by such a treatment modality [15].
Definition of target volume
As introduced in the previous ICRU Reports 50, 62, 71 and 78, several volumes related to both tumor and normal tissues have been defined for use in the treatment-planning and -reporting processes [11–14]. Selection and delineation of these volumes is an obligatory step in the planning process, as dose cannot be prescribed, recorded and reported without the specification of target volumes and volumes of normal tissue at risk.
The gross tumor volume (GTV) is the gross demonstrable extent and location of the malignant growth. It consists of the primary tumor, the regional lymph nodes or the distant metastases according to the clinical situation. The GTV can be delineated on anatomic (e.g., CT or MRI) or functional (e.g., PET with various tracers) imaging modalities; it can be delineated before the start of treatment and, eventually, during treatment to capture a change in target volume. More than one GTV can be specified. A nonambiguous annotation has been proposed to name such GTVs (e.g., GTV-tumor [MRIT 2, 0 Gy]) for a primary-tumor GTV delineated before treatment based on a T2-weighed MRI. It is known that tumors have the potential to microscopically infiltrate into the surrounding normal tissues and/or disseminate through the lymphatic network to reach the regional lymph nodes. In this framework, the clinical target volume (CTV) is a volume that contains a demonstrable GTV and/or subclinical malignant disease that must be eliminated. Over the last years, data on the incidence of regional tumor and lymph node infiltration have been compiled for various primary tumor sites, based on which recommendations for the definition of CTVs have been proposed [16–18]. Similar to the GTV, clear annotation should be used for the CTV (e.g., CTV-T [MRI-T2; 0 Gy]) for a primarytumor CTV associated to a GTV delineated before treatment based on a T2-weighed MRI. In addition, it should be emphasized that both the GTV and the CTV are oncological concepts and represent volumes that must be treated in order to achieve the aim of radical therapy.
After these volumes have been selected, before applying a particular radiation technique, one must consider different types of variations, uncertainties or even errors related to geometrical factors. Indeed, physiological factors (e.g., change in organ filling or breathing) may introduce movements of the CTV, and the whole patient could be slightly differently positioned from one session to another. Thus, these geometric factors require the addition of a margin around the CTV, composed of an internal margin (i.e., an internal target volume related to internal movement of the CTV) and a setup margin (i.e., related to variation in patient set-up). The internal target volume might be useful in clinical situations in which the internal movement of the target dominates the setup uncertainties. The planning target volume (PTV) is defined as the volume including the CTV and the surrounding margin. It is a geometrical concept used for treatment planning and defined to ensure that the prescribed dose is actually delivered to the CTV with a clinically acceptable probability. Recommendations have been published on how to calculate margins to delineate PTVs [19]. There may be more than one GTV and corresponding CTV specified. Each CTV should have a corresponding PTV. IMRT makes it relatively easy to specify different doses to each of the PTVs.
The organs at risk (OARs), or critical normal structures, are tissues, which, if irradiated, could suffer significant morbidity and, thus, might influence the treatment planning and/or the dose prescription. In principle, all nontarget tissues could be OARs. However, normal tissues considered as OARs typically depend on the location of the CTV and/or the prescribed dose. Care will have to be given to the delineation of OARs: for example, for ‘tubed’ organs (e.g., the rectum), the wall and not the full organ including the content will be delineated; also for finite normal tissues (e.g., the parotids and the lungs), the full organ will have to be delineated as the figures of merit to evaluate radiation toxicity in these organs (e.g., mean parotid dose, V20Gy for the lung) will have to be related to the full volume. Recent recommendations have been published regarding normal-tissue tolerance [20].
As is the case with the PTV, uncertainties and variations in the position of the OAR during treatment must be considered to avoid serious complications. For this reason, margins have to be added to the OARs to compensate for these uncertainties and variations using similar principles as for the PTV. This leads, in analogy with the PTV, to the concept of planning OAR volume (PRV). The selection of the margin will, however, depend on the structure of the OAR being more critical for organs such as the spinal cord or nerves than for organs such as the parotid glands or the lungs. In practice, for these latter organs, the OAR–PRV margin could be set to 0 mm.
Planning aims & treatment optimization
In IMRT, the distribution of dose to multiple volumes is prioritized and tailored through an iterative process, referred to as ‘optimization’. The process consists of three major components: the definition and description of the ‘planning aims’ using image-based information from which all of the volumes of interest (e.g., GTVs, CTVs, OARs, PTVs and PRVs) are delineated and the desired absorbed-dose levels are specified; a complex beam delivery optimization process to achieve and, if needed, modify the initial planning aims; and a complete set of finally accepted values, which becomes the ‘treatment prescription’ and, together with the required ‘technical data’, represents the ‘accepted treatment plan’.
The planning aims are dosimetric goals used to develop the treatment plan. These goals can be defined for any specified volume, including the PTVs and PRVs, for which constraints are needed. Typically, multiple constraints are defined, such as mean or median dose, dose to ‘x%’ of a volume (e.g., D2% or Dnear-maximum dose) or volume receiving at least an absorbed dose (e.g., V20Gy). Also in the optimization process, priority of one constraint over another and/or priority of one volume over another are specified. All of these constraints are defined in the planning protocol. To initiate the planning process, medical physicists or technologists sometimes use so-called artificial dose-volume constraints, which may be different from the desired ones or from clinically relevant dose constraints. The dose-volume constraints will then be modified iteratively to achieve the best plan.
When the optimized dose distribution is accepted by the physician, the prescription and technical data are finalized. The treatment plan includes the final prescription as well as all technical data required for treatment delivery. The prescription is a description of the volumes of interest, the dose and/or dose-volume requirements for the PTV, the fractionation scheme, the normal tissue constraints and the dose distribution(s) that have been planned. This final process is the responsibility of the treating physician. The prescription is then referred to as the finally accepted set of values of the modified planning aims in the treatment plan after an optimization process.
Dose-volume prescription, reporting & recording
The main reason for the use of dose-volume reporting and recording in IMRT is that the coverage of the PTV by a specific absorbed dose can be explicitly determined from a dose–volume histogram and be better controlled through optimized planning. The use of dose-volume reporting and recording instead of reporting and recording the more established absorbed dose at the ICRU reference point is predicated on the use of an adequate dose-calculation system. Recently, model-based dose-calculation algorithms, such as the convolution/superposition method, or Monte Carlo simulation, have been adopted and provide accurate absorbed-dose calculations even in situations of tissue heterogeneity such as the lung. The report recommends that the users of treatment-planning systems ensure that treatment-planning systems have the ability to compute the absorbed dose accurately for small fields, inhomogeneous tissues and in regions in which there is electronic disequilibrium. The absorbed dose in Gy to a small mass of water within the heterogeneous tissue is the relevant dose to compute. This means that direct computation of dose with Monte Carlo simulation to the tissue (including the correct atomic composition and density) must be converted to the dose of a small mass of water within the tissue type.
Prescription values for IMRT should be based on statistically meaningful dose-volume specifications, and not on specifying the dose only at a single point. The older specification of an ICRU reference point dose is not recommended for IMRT, and nor is the minimum dose to the PTV. This is because the minimum dose represents the dose to a single point likely at the boundary of the PTV and is far too susceptible to errors in delineation. A specific dose-volume prescription value to use is not prescribed but it should be clinically relevant, statistically meaningful and clearly described. For example, D98%, also called the near-minimum dose, may be an acceptable choice as it represents the dose that at least 98% of the PTV receives. Radiation oncologists should be aware that any change in the prescription protocol or dose-volume specification is likely to result in a change to the dose received by the patient. It is important when making changes to the prescription to evaluate the magnitude and extent of these changes by comparing the dose received by patients for the old and new protocols so that dose values specified can be adjusted if necessary. Whatever dose-volume prescription value is chosen, the median dose, represented by D50%, should also be reported and recorded as it represents a typical dose within the PTV and is usually nearest to the dose value of the more traditional ICRU reference point. The radiation oncologist should not rely solely on the dose–volume histogram for treatment evaluation but should also carefully inspect the absorbed-dose distributions slice-by-slice (or in 3D) to make sure that the PTV is being adequately irradiated and normal sensitive tissues avoided as best as possible.
The functional arrangement of normal-tissue cells has been described as parallel or serial [21]. For parallel-like structures it is recommended that more than one dose-volume specification be considered for reporting and recording. The mean absorbed dose in parallel-like structures can be a useful measure of absorbed dose in an OAR. Typically, because of highly non-uniform absorbed-dose distributions in OARs, the mean absorbed dose and the median absorbed dose are not similar in value, and so the median absorbed dose cannot be used as an accurate substitute for the mean. For parallel-like normal tissues, dose-volume reporting specifying VD, which is a volume that receives at least the absorbed dose, D, specified in Gy, is a concept that has been commonly used and can also be easily obtained from a dose-volume histogram.
The maximum absorbed dose as specified by a single calculation point (Dmax or D0%) has often been reported for serial-like structures; however, this is based on a single point and has great delineation uncertainty. This report instead recommends that D2% be reported. To obtain a true value of D2%, the entire organ should be delineated. When not possible (e.g., for the spinal cord), the anatomic description of the delineated regions should be described when reporting the D2 %. Care should be taken in changing from a maximum absorbed dose, D0%, or other maximum-like dose-volume specification to the near-maximum absorbed dose, D2%, with the dose constraints altered if necessary.
When organs are not clearly classified as serial-like or parallel-like structures, at least three dose-volume specifications should be reported and recorded. These would include Dmean, D2% and a third specification, VD, that correlates well with an absorbed dose, D, which, if exceeded within some volume, has a known high probability of causing a serious complication. Other specifications of risk, as deemed by the radiation oncologist to be relevant, may also be reported and recorded.
The reported and recorded dose prescriptions and technical data defining the accepted plan are only relevant if there is adequate quality control on the whole process of IMRT to ensure that the doses are being delivered accurately. Machinespecific quality-assurance tests on the planning and delivery system are sometimes more complex than for other forms of radiation therapy because the ability to plan and deliver the modulation of intensity must be specially measured. In addition to machine-specific tests, patient-specific quality assurance is also recommended. One or more of the following methods producing a statistically relevant set of comparisons can be used to verify that the intensity pattern will deliver the desired absorbed dose:
▪ Measurement of the intensity pattern from individual beams for a specific patient;
▪ Measurement of absorbed dose in a phantom of the beam-intensity pattern planned for a specific patient;
▪ Independent but equivalently accurate absorbed-dose ca lculations for the patient-specific beam-intensity pattern.
■ In vivo dosimetry
It is recommended that, for a low-gradient (<20% per cm) region, the one standard deviation difference between the measured (or independently computed) absorbed dose and the treatment-planning absorbed dose, normalized to the absorbed-dose prescription (e.g., D50%), should be no more than 3.5%. This means that approximately 85% of points should be within 5% of the desired value (normalized to the prescription absorbed dose). For high-gradient (>20% per cm) regions, the accuracy of distance to agreement of isodose lines should be within 3.5 mm, which means that 85% of the measurement or calculation samples should be within a 5-mm distance to agreement. Such a proposal is either based on comparison measured or on independently calculated absorbed dose. Investigative action is recommended if 85% of points of comparison fail to meet either the distance to agreement or absorbed-dose accuracy.
Conclusion
Intensity-modulated radiation therapy is characterized by nonuniform intensity distributions that have been optimized to collectively deliver an adequately homogenous dose to the target volume and spare normal tissues as much as possible. Usually, these intensity patterns are iteratively optimized by specifying dose and dose-volume constraints to the target volume and normal tissues. The optimization leads to an approved treatment plan, which is specified by the prescription (which also includes specifications for OARs as well as the target volume) and the technical data needed to deliver the plan. Treatment plans can be altered during the course of radiation therapy to take into account patient anatomy changes due to tumor shrinkage or weight loss. This so-called adaptive therapy can result in new target-volume and OAR delineations. ICRU Report 83 documents the specific differences between earlier ICRU reports for the specification of procedures for the prescribing, reporting and recording of IMRT treatments. In particular, additional recommendations were given on the selection and delineation of the target volumes and the OARs; concepts of dose prescription and dose-volume reporting have also been refined.
Future perspective
Today, approximately one patient out of two suffering from cancer benefits from radiotherapy given in one or several stages of their disease. This number is expected to rise owing to the aging of the population requiring cancer treatment, the need for more organ- and function-preserving treatment approaches and the fact that more and more patients cured from one cancer may experience another one (or other ones). Regarding radiotherapy delivery, it is anticipated that worldwide IMRT will be used in a majority of patients treated with curative intentions. Among these patients, some will even require frequent re-imaging and re-planning during IMRT treatment to adapt the dose distribution to the tumor evolution. Such adaptive radiotherapy could possibly lead to dose escalation on specific parts of the tumor volume, aiming at further increasing the treatment efficacy.
In this context, more so than ever, such treatment evolutions will require accurate and homogeneous dose prescription, reporting and recording, which will be greatly facilitated by the use of a unique set of recommendations, such as the one proposed by ICRU. It is likely that refinements of these recommendations will have to be elaborated to better integrate the possible evolution of adaptive radiotherapy or other delivery techniques (e.g., stereotactic treatment). However, as it has been for the last 30 years, the ICRU recommendations should remain the backbone for radiotherapy practice, as a unique common language aiming at facilitating and improving communication between radiation oncologists.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
- Bernier J, Hall EJ, Giaccia A: Radiation oncology: a century of achievements. Nat. Rev. Cancer 4, 737–747 (2004).
- Webb S: The Physics of Three-Dimensional Therapy: Conformal Therapy, Radiosurgery and Treatment Planning. Institute of Physics Publishing, Bristol, PA, USA (1993).
- Brahme A: Design principles and clinical possibilities with a new generation of radiation therapy equipment: a review. Acta Oncol. 26, 403–412 (1987).
- Brahme A: Optimization of stationary and moving beam radiation therapy techniques. Radiother. Oncol. 12, 129–140 (1988).
- Cormack AM: A problem in rotation therapy with x rays. Int. J. Radiat. Oncol. Biol. Phys. 13, 623–630 (1987).
- Intensity Modulated Radiation Therapy Collaborative Working Group: Intensity modulated radiation therapy: current status and issues of interest. Int. J. Radiat. Oncol. Biol. Phys. 51, 880–914 (2001).
- Brahme A, Ågren AK: Optimal dose distribution for eradiation of heterogenous tumors. Acta Oncol. 26, 377–385 (1987).
- Mackie, TR, Holmes TW, Swerdloff S et al.: Tomotherapy: a new concept in the delivery of dynamic conformal radiotherapy. Med. Phys. 20, 1709–1719 (1993).
- Weeks KJ, Arora VR, Leopold KA et al.: Clinical use of a concomitant boost technique using a gypsum compensator. Int. J. Radiat. Oncol. Biol. Phys. 30, 693–698 (1994).
- ICRU: Dose Specification for Reporting External Beam Therapy with Photons and Electrons. ICRU Report 29. International Commission on Radiation Units and Measurements, MA, USA (1978).
- ICRU: Prescribing, Recording and Reporting Photon Beam Therapy. ICRU Report 50. Oxford University Press, Oxford, UK (1993).
- ICRU: Prescribing, Recording and Reporting Photon Beam Therapy (Supplement to ICRU Report 50). ICRU Report 62. Oxford University Press, Oxford, UK (1999).
- ICRU: Prescribing, Recording and Reporting Electron Beam Therapy. ICRU Report 71, J. ICRU Vol. 4(1). Oxford University Press, Oxford, UK (2004).
- ICRU: Prescribing, Recording and Reporting Proton-Beam Therapy. ICRU Report 78, J. ICRU Vol. 7(2). Oxford University Press, Oxford, UK (2007).
- ICRU: Prescribing, Recording, and Reporting Photon-Beam Intensity-Modulated Radiation Therapy (IMRT). ICRU Report 83, J. ICRU, Volume 10(1). Oxford University Press, Oxford, UK (2010).
- Grégoire V, Coche E, Cosnard G et al.: Selection and delineation of lymph node target volumes in head and neck conformal radiotherapy. Proposal for standardizing terminology and procedure based on the surgical experience. Radiother. Oncol. 56(2), 135–150 (2000).
- Roels S, Duthoy W, Haustermans K et al.: Definition and delineation of the clinical target volume for rectal cancer. Int. J. Radiat. Oncol. Biol. Phys. 65(4), 1129–1142 (2006).
- Boehmer D, Maingon P, Poortmans P et al.: EORTC radiation oncology group. Guidelines for primary radiotherapy of patients with prostate cancer. Radiother. Oncol. 79(3), 259–269 (2006).
- van Herk M: Errors and margins in radiotherapy. Semin. Radiat. Oncol. 14, 52–64 (2004).
- Bentzen SM, Constine LS, Deasy JO et al.: Quantitative Analyses of Normal Tissue Effects in the Clinic (QUANTEC): an introduction to the scientific issues. Int. J. Radiat. Oncol. Biol. Phys. 76(3 Suppl.), S3–S9 (2010).
- Withers HR: Predicting late normal tissue responses. Int. J. Radiat. Oncol. Biol. Phys. 12, 693–698 (1986).


