Research Article - International Journal of Clinical Rheumatology (2019) Volume 14, Issue 6
Diagnostic role of neuromuscular ultrasound in cubital tunnel syndrome
- Corresponding Author:
- Mona Hamdy
Rheumatology and Rehabilitation Department, Minia University, Egypt
E-Mail: dr.mona.hmdy@gmail.com
Abstract
Objective: We aim to evaluate the role of Ultrasonography (US) as a diagnostic tool for Cubital Tunnel Syndrome (CuTS) in comparison with the Nerve Conduction Study (NCS). Methods: Twenty elbows with CuTS and twenty asymptomatic controls were assessed by NCS and underwent ultrasonography of elbows. Patient and control data were compared to determine the diagnostic relationship in patients with CuTS and the degree of severity. Results: The NCS of the ulnar nerve, clinical parameters, and variable US measurements had a high degree of correlation. The CSA of the ulnar nerve was the most sensitive and 100% sensitive, 80% specific, and cut-off point of 9.5 mm2 behind the Medial Epicondyle. The diagnostic accuracy of the ulnar nerve ratio (UNR) was 95% sensitive and 85% specific. Conclusion: Ultrasonographic measurements of the ulnar nerve CSA and UNR are equivalent to noninvasive diagnostic measurements, which are an alternative method of CuTS assessment.
Keywords
cubital tunnel syndrome • neuromuscular • ultrasonography • nerve conduction • entrapment neuropathies
Introduction
Cubital Tunnel Syndrome (CuTS) is the second most common compressive neuropathy of the upper limb following carpal tunnel syndrome . It is the most common site for entrapment for the ulnar nerve [1,2]. Neuromuscular ultrasound (US) has been introduced in electro diagnostic laboratories as a complement to nerve conduction and electromyography studies for the diagnosis of a variety of nervous and muscular conditions [3].
The electrophysiological studies usually show the level of the lesion, but do not provide anatomical information about the nerve or its surroundings [4,5]. In the last few years, US, being inexpensive and non-invasive imaging modality, CTS diagnostic tools are useful, providing information on the surrounding structures and median nerve. It has become an adjunct to electro diagnostic studies in the evaluation of entrapment neuropathies [6,7].
The present study aimed to identify the efficacy of US measurements in a consecutive sample of patients with clinically diagnosed CuTS to analyze the correlation of US findings with electrophysiological abnormalities and clinical severity. Secondary causes for CuTS were excluded from the study e.g. elbow arthritis. Patients with associated roximal C8 root compression were also excluded.
Patients and Methods
Patients
Seventeen patients with twenty elbows were included in this study, and twenty controls were evaluated between May 2015 and January 2016.
Methodology
The clinical diagnosis of cubital tunnel syndrome was based on signs and symptoms of ulnar nerve distribution, such as intermittent paraesthesias, numbness and tingling in the small finger and ulnar half of the ring finger, elbow pain in the region of the cubital tunnel, non-specific complaints of hand clumsiness or weakness, grip weakness (e.g., difficulty opening bottles or jars), hand clumsiness (e.g., difficulty typing) or difficulty with precision pinch activities (e.g., buttoning buttons) [8]. An assessment Questionnaire for symptoms severity in ulnar neuropathy at the elbow was used [9].
Clinical severity of Ulnar Nerve Entrapment (UNE) was graded using a 1–4 ordinal scale: Grade-1: only subjective symptoms in territory innervated by the ulnar nerve; the symptoms may be intermittent (diurnal or nocturnal, correlate or otherwise with prolonged or uncomfortable elbow positions and repetitive elbow movements) without abnormal objective findings. Grade-2: sensory loss (by comparison of fifth and third fingers or, in the presence of CTS, with the radial aspect of the first finger). Grade-3: Weakness of ulnar nerve intrinsic muscles of the hand with or without hypotrophy. Grade-4: atrophy and absence of voluntary contraction of ulnar nerve intrinsic muscles of the hand [9].
Electro diagnostic studies were done according to 1999 recommendations of the American association of electro diagnostic medicine, American academy of the neurology, American academy of physical medicine and rehabilitation including Sensory and motor conduction studies and EMG study [10]. All neurophysiological studies were done using Neuropack S1, MEB- 9400K, four channels EMG/EP Measuring System; Nihon Kohden; Japan.
Patients divided into five severity classes based on the following neurophysiological classification [11]: Negative UNE: normal findings on all tests, Mild UAE: slowing of ulnar MNCV across elbow and normal ulnar SNAP, Moderate UNE: slowing of ulnar MNCV across elbow and reduced amplitude of ulnar SNAP; Severe UNE: absence of ulnar SNAP (fifth digit-wrist segment) and slowing of motor nerve conduction velocity (MNCV) across elbow; Extreme UNE; absence of hypothenar motor and sensory responses. Neuromuscular ultrasound evaluation: All US scans were performed using Siemens ACUSON P300 Ultrasound System (Siemens Healthcare, Boulevard, Malvern, USA) multi-frequency 10-18 MHz linear transducer for high detail resolution of superficial structures using the 18 MHz.
The patient was in supine position, and the arm abducted and flexed 90 at the elbow for evaluation of the nerve from the wrist to the axilla [12] (Figure 1).
To obtain a sagittal view, the transducer was placed in the ulnar groove. Then, rotated 90 degrees to get a cross-sectional view at the elbow. The transducer was then advanced distally to the mid-forearm and proximally to the mid-arm, for imaging of the nerve in the cubital tunnel, at the level of the medial epicondyle, and in the supracondylar region [12]. On using the automatic ellipse tool of the ultrasound machine, transversal scans of the ulnar nerve CSA were determined; nerves in which the shape was not well adapted to CSA measurements by mounting and ellipse were measured by direct tracing (Figure 2).
The ulnar nerve was scanned from the middle of the upper arm to the middle of the forearm. The size of the nerve was measured at the following levels: medial epicondyle, 2 cm proximal, 2 cm distal to this level, and in the middle of the upper arm and forearm.
Ulnar nerve upper arm and forearm swelling ratios were calculated by dividing the maximum ulnar nerve CSA at the elbow by the ulnar nerve CSA at the middle of the upper arm or forearm, respectively [13].
Results
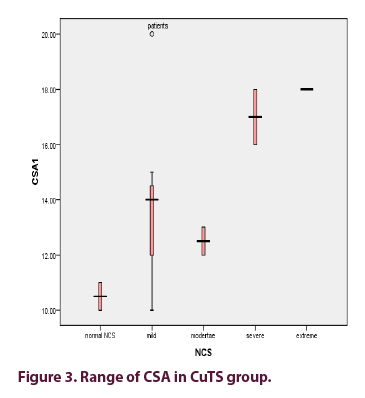
CuTS group; showed CSA at the medial epicondyle ranged from 10 to 20 mm2 with a mean of 13.95mm2 ± 2.95, while the CSA 2 cm proximal to the medial epicondyle ranged from 6 to 11 mm2 with a mean of 8.5 mm2 ± 1.85. The CSA 2 cm distal to the medial epicondyle ranged from 6 to 10 mm2 with a mean of 8.55 mm2 ± 1.39. The medial epicondyle /mid arm CSA ratio was found to be from 1.20 to 2.81 with a mean of 2.08± 0.50 while the medial epicondyle /midforearm CSA ratio as found to be from 1.50 to 4.50 with a mean of 2.78± 0.84. Power Doppler signals were found to be positive in 11 (55%) of cases. There was a difference in the CSA of the ulnar nerve at the medial epicondyle in controls (8.75 mm2) compared to those with UNE (13.95 mm2), which was statistically significant (P = 0.001) (Figure 3). The ulnar nerve ratios at the medial epicondyle and mid-arm and mid-forearm were also statistically significant with p<0.001 (Table 1).
| Elbows (No=20) | Control (No=20) | P-value | ||
|---|---|---|---|---|
| CSA at the medial epicondyle | Range | 10-20 | 8-10 | <0.001* |
| Mean ± SD | 13.95 ± 2.95 | 8.75 ± 0.79 | ||
| CSA 2 cm proximal to media epicondyle | Range | 6-11 | 6-8 | 0.001* |
| Mean ± SD | 8.5 ± 1.85 | 6.90 ± 0.79 | ||
| CSA 2 cm distal to media epicondyle | Range | 6-10 | 5-7 | <0.001* |
| Mean ± SD | 8.55 ± 1.39 | 5.95 ± 0.69 | ||
| medial epicondyle CSA/ arm ratio | Range | 1.20-2.81 | 0.80-1.33 | <0.001* |
| Mean ± SD | 2.08 ± 0.50 | 1.10 ± 0.19 | ||
| medial epicondyle CSA/ forearm Ratio | Range | 1.50-4.50 | 1-2 | <0.001* |
| Mean ± SD | 2.78 ± 0.84 | 1.53 ± 0.29 | ||
Table 1. Ultrasonographic findings in cubital tunnel syndrome group and control.
The NCS findings were positively correlated with the ultrasonographic parameters in CuTS group as regards CSA max, CSA 2 cm proximal to media epicondyle, CSA 2 cm distal to media epicondyle, CSA max / arm ratio, CSA max / forearm ratio, and vascularity (r=0.58, p= 0.007, r=0.71, p=0.001, r=0.52, p=0.02, r=0.48, p=0.03, r=0.51, p=0.02 and r=0.68, p=0.001 respectively).
CSA at the medial epicondyle was found to be the most sensitive parameter in the diagnosis of CuTS. It showed the highest sensitivity 100% and specificity 80% with 98.5% for the AUC at a cutoff point 9.5mm2, compared to other US parameters (Figure 4). Delta arm showed a sensitivity of 90% and a specificity of 85% at 1.3. Delta forearm had a sensitivity of 95% and a specificity of 85% at 1.7. Combined CSA at the medial epicondyle and ulnar nerve ratio add no more values to the sensitivity or specificity (Table 2).
| AUC | Sensitivity | Specificity | Cutoff value | P-value | |
|---|---|---|---|---|---|
| CSA at the medial epicondyle | 98.50% | 100% | 80% | 9.5 | <0.001* |
| CSA 2 cm proximal to medial epicondyle | 76% | 75% | 75% | 7.5 | 0.005* |
| CSA 2 cm distal to medial epicondyle | 94% | 90% | 80% | 6.5 | <0.001* |
| Medial epicondyle CSA/arm ratio | 95.50% | 90% | 85% | 1.29 | <0.001* |
| Medial epicondyle CSA/forearm ratio | 95% | 95% | 85% | 1.7 | <0.001* |
| Combined CSA at the med. Epicondyle and delta arm | 99% | 100 | 80% | 384.64 | <0.001* |
Table 2. Diagnostic value of ultrasonographic parameters in cubital tunnel syndrome.
Discussion
In most instances, the value of ancillary testing should be determined by the extent to which it affects the probability of the patient having the diagnosis that had been established clinically. Clearly, there are diagnoses that cannot be well established based on clinical criteria alone, and appropriate testing may have a substantial impact in these cases. On the other hand, when a diagnosis can be reliably established clinically, testing may simply add inconvenience, delay, discomfort, and expense to the diagnostic process [14]. Recently, US techniques came into advancement as a tool to complement the diagnosis of CuTS.
In the present study, the efficacy of ultrasound for the diagnosis of CuTS was evaluated. Electrodiagnostic studies were used as gold standard diagnostic procedures. Our findings from the ultrasound measurement at different levels around the elbow showed a significant correlation with NCS in concordant with Simon et al. [15]; Omejec and Podnar [16].
The CSA behind the medial epicondyle was found to be the site of maximum enlargement with the highest sensitivity and specificity (100% and 80% respectively) at 9.5 mm2 cut off value, and the AUC was 98.5%. This cut off value was in concordant with Pompe and Beekman [13], who concluded that the cut off value for CSA behind the medial epicondyle was 10 mm2, but they found a lower sensitivity 80% and specificity (80% and 72%, respectively) due to selection bias of their patients as the recruited all patients in the DD of UNE, then classified according to NCS, and so some of their patients was not truly CuTS. Another bias in that study was their control population; they studied patients control side, not healthy control as we did.
In one study [15] the CSA was measured the max CSA they found that CSA comparable to our results (13.0±1.4 vs. 13.95±2.95, respectively) and they found a significant difference to their control (p<0.01) with their range of CSA max was 10-20 mm2 which was the same range of our study. Also, data from Omejec and Podnar [16] concluded that CSA max was ranged from 10- 14mm2 compared to 10-20 of our data. As regards to the ulnar nerve ratios, Simon et al. [15] found that CSAmax divided CSA at the midarm ratio to be 2.2±0.2, which was significant regarding their control. These data were comparable to our results. Our data was 2.08±0.5, which was also highly significant regards to our controls. In terms of sensitivity and specificity, the ulnar nerve ratio (CSA at the ME divided by mid-arm point) was found to be 90% and 85% respectively at cut off value 1.29 which was comparable to results gained from Omejec and Podnar [16]; ratio was 1.65 with lower sensitivity (64%) and near-equal specificity (85%), this lower sensitivity due to different control selection. These data were comparable to previous data from Yoon et al. [17] with sensitivity and specificity of 100% and 97%, respectively.
Pompe and Beekman [13] concluded that ROCanalysis of their results did not show a cut-off point for the swelling ratio with much higher sensitivity (without loss of too much specificity). The lower specificity found in their study compared to our results may be explained by their control group, which consisted of disease, not healthy controls.
The AUC of The CSA mid-forearm ratio was found to be 95%. The sensitivity and specificity was 90% and 85% respectively, which was more than those found by 18; 88% and 66% respectively probably due to the lower number of controls compared to their patients (41 elbows vs. 21 healthy controls).
Furthermore, adding the CSA to the ratios did not add significant change to sensitivity and specificity, that was the same observations from previous studies, which concluded that the ratio measurement does not appear to be more accurate than the largest CSA [17,18]. Vascularity was a significant finding in the CuTS group. We could found vascularity in 7 cases of CuTS (35%). These findings were on line with data from [19].
Conclusion
The US is considered a new diagnostic modality in entrapment neuropathies of the ulnar nerve, and several cut off values are considered nowadays as diagnostic criteria for CuTS. Based on the above mentioned data neuromuscular ultrasound could be considered as a primary tool and a modality of 1st choice for the diagnosis of CuTS in order to select cases who are in need for further laboratory tests; NCS and EMG. For CuTS cases who was diagnosed based on clinical criteria, we recommend to proceed for NCS and EMG if the CSA > 9.5 mm2 and/or CSA behind medial epicondyle /forearm ratio >1.7.
Early cases presented by clinical CuTS who are already evaluated by NCS modality and results are negative, we strongly recommend for NMUS evaluation. Ultrasound evaluation for CuTS patients who are approved to their diagnosis clinically and laboratory is recommended as an adjuvant modality in order to gain more informative data before surgical procedures.
References
- Roberts G, Maclean A, Logan A. Ulna Nerve Decompression at the Elbow in Patients with Normal Nerve Conduction Tests. J. Hand. Surg. Am. 20(2), 260-265 (2015).
- Qing C, Zhang J, Wu S et al. Clinical classification and treatment of cubital tunnel syndrome. Exp. Ther. Med. 8(5), 1365-1370 (2014).
- Walker F, Cartwright M, Wiesler E et al. Ultrasound of nerve and muscle. Clin. Neurophysiol. 115(3), 495-507 (2004).
- Deniz F, Oksuz E, Sarikaya B et al. Comparison of the diagnostic utility of electromyography, ultrasonography, computed tomography, and magnetic resonance imaging in idiopathic carpal tunnel syndrome determined by clinical findings. Neurosurgery. 70(3), 610-616 (2012).
- Keles I, Kendi A, Aydn G et al. Diagnostic precision of ultrasonography in patients with carpal tunnel syndrome. Am. J. Phys. Med. Rehabil. 84(6), 443-450 (2005).
- Chiou H, Chou Y, Cheng S et al. Cubital tunnel syndrome: diagnosis by high-resolution ultrasonography. J. Ultrasound. Med. 17(10), 643-648 (1998).
- Ginn S, Cartwright M, Chloros G et al. Ultrasound in the diagnosis of a median neuropathy in the forearm: case report. J. Brachial. Plex. Peripher. Nerve. Inj. 2(1), 1 (2007).
- Palmer B, Hughes T. Cubital tunnel syndrome. J. Hand. Surg. Am. 35(1), 153-163 (2010).
- Mondelli M, Padua L, Giannini F et al. A self-administered questionnaire of ulnar neuropathy at the elbow. J. Neurol. Sci. 27(6), 402-411 (2006).
- American Association of Electrodiagnostic Medicine. Practice parameter for electrodiagnostic studies in ulnar neuropathy at the elbow: summary statement. Muscle. Nerve. 22(3), 408-411 (1999).
- Padua L, Aprile I, Mazza O et al. Neurophysiological classification of ulnar entrapment across the elbow. Neurol. Sci. 22(1), 11-16 (2001).
- Cartwright M, Walker F. Neuromuscular ultrasound in common entrapment neuropathies. Muscle. Nerve. 48(5), 696-704 (2013).
- Pompe S, Beekman R. Which ultrasonographic measure has the upper hand in ulnar neuropathy at the elbow? Clin. Neurophysiol. 124(1), 190-196 (2013).
- Graham B. The Value Added by Electrodiagnostic Testing in the Diagnosis of Carpal Tunnel Syndrome. J. Bone. Joint. Surg. Am. 90(12) (2008).
- Simon N, Ralph J, Poncelet A et al. A comparison of ultrasonographic and electrophysiologic ‘inching’in ulnar neuropathy at the elbow. Clin. Neurophysiol. 126(2), 391-398 (2015).
- Omejec G, Podnar S. Normative values for short‐segment nerve conduction studies and ultrasonography of the ulnar nerve at the elbow. Muscle. Nerve. 51(3), 370-377 (2015).
- Yoon J, Walker F, Cartwright M. Ultrasonographic swelling ratio in the diagnosis of ulnar neuropathy at the elbow. Muscle. Nerve. 38(4), 1231-1235 (2008).
- Bayrak A, Bayrak I, Turker H et al. Ultrasonography in patients with ulnar neuropathy at the elbow: Comparison of cross‐sectional area and swelling ratio with electrophysiological severity. Muscle. Nerve. 41(5), 661-666 (2010).
- Frijlink D, Brekelmans G, Visser L. Increased nerve vascularization detected by color Doppler sonography in patients with ulnar neuropathy at the elbow indicates axonal damage. Muscle. Nerve. 47(2), 188-193 (2013).