Case Report - International Journal of Clinical Rheumatology (2021) Volume 16, Issue 1
Coexistence of relapsing polychondritis and remitting seronegative symmetrical synovitis with pitting odema (RS3PE) syndrome
- Corresponding Author:
- Dilek Tezcan
Division of Rheumatology
Faculty of Medicine, Selcuk University, Konya, Turkey
E-mail: dr_dilekturan@hotmail.com
Abstract
Relapsing Polychondritis (RP) is an autoimmune disease characterized by recurrent and progressive inflammation and destruction of cartilaginous and other proteoglycan-rich tissue with multisystematic manifestations. Remitting Seronegative Symmetrical Synovitis with Pitting Edema (RS3PE), is a rare disorder characterized by pitting edema, onset of acute polyarthritis and negative rheumatoid factor. A 46-year-old female patient who developed RS3PE after RP symptoms developed. This case, being an RS3PE syndrome accompanying RP and being a rare association, is presented to contribute to the literature.
Keywords
remitting seronegative ● symmetrical synovitis with pitting edema syndrome ● relapsing polychondritis
Introduction
Relapsing Polychondritis (RP) is an autoimmune disease characterized by recurrent and progressive inflammation and destruction of cartilaginous and other proteoglycan-rich tissue with multi-systematic manifestations. Although the first case was reported in 1923[1], the current definition of RP was proposed in 1960 by Pearson et al. [2]. It is a rare disease with an estimated incidence of 3.5 cases per million/year. It affects both genders with a mild female predominance. The median age of onset is between the fourth and the fifth decade of life, but it can occur at any age.Diagnosis of RP is generally based on clinical findings, while laboratory data have only a supportive contribution. Especially the cartilaginous structures of ear, nose, joints and respiratory tract are affected. Cardiovascular and respiratory complications have a high mortality and morbidity rate [3]. Remitting Seronegative Symmetrical Synovitis with Pitting Edema (RS3PE) is a disease characterized by the onset of acute polyarthritis with pitting edema, negative rheumatoid factor, absence of joint erosion on radiographs, synovitis detected by USG/ MRI, and good response to low dose steroids. RS3PE was first described by McCarty in 1985 [4]. It is mostly seen in the elderly population, particularly over 60 years of age and predominantly in men. It is known to be associated with other rheumatological diseases and may represent a paraneoplastic syndrome in a variety of situations. This case, being an RS3PE syndrome accompanying RP and being a rare association, is presented to contribute to the literature.
Case report
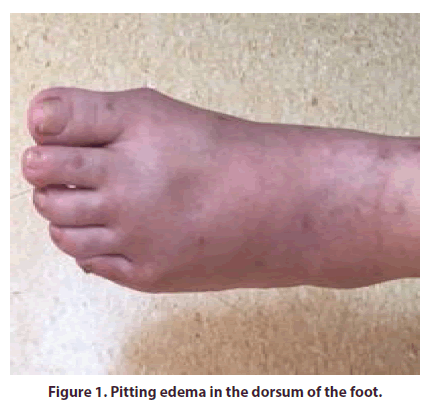
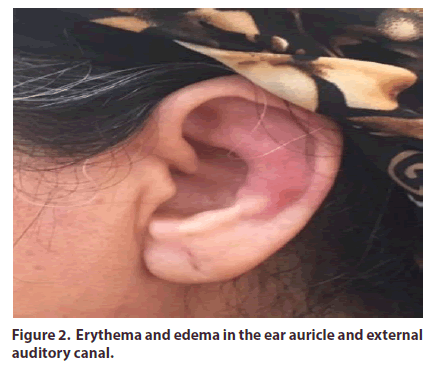
A 46-year-old female patient was given antibiotic and inhaler treatments at the health centers she previously applied with complaints of hoarseness, shortness of breath, widespread joint pain, and fever that started about 6 months ago. The patient's complaints progressed in the following days and additional clinical findings developed. The patient applied to our outpatient clinic due to the complaints of swelling in the dorsum of the left foot, pain in the ankle, swelling, pain in the hand joints, and stiffness. The patient, whose morning stiffness lasted for more than an hour, had no history of systemic and rheumatologic disease other than known diabetes mellitus. There was no smoking or alcohol use history. Systemic physical examinations were normal on. In her rheumatological examination, there was pitting edema in the dorsum of the left foot (Figure 1). There was swelling and tenderness in the right hand metacarpophalangeal joints. The left ankle joint was extremely sensitive and both passive and active wrist movements were restricted due to pain. Ear, Nose and Throat (ENT) examination revealed widespread erythema and edema in the left ear auricle and external auditory canal. The soft part of the auricle that did not contain cartilage was normal (Figure 2). In addition, Nasal dorsum saddle-nose deformity was detected. In laboratory tests, C reactive protein (CRP): 36.1 mg/dl (N: 0-8) and sedimentation (ESR ): 68 mm/s. Thyroid, kidney and liver function tests, total protein, albumin, uric acid, serum electrolyte levels and tumor indicators were found within normal limits. Rheumatoid Factor (RF), anti-Cyclic Citrullinated Peptide antibody (AntiCCP), Antinuclear Antibodies (ANA) and Antineutrophil Cytoplasmic Antibodies (ANCA) were negative. Erosive changes were not observed in the joints in the radiological examination. In the abdominal and pelvis ultrasonography performed for malignancy screening, liver, spleen, and kidneys were found in normal size and structure, there was no lymphadenopathy or mass. Neck ultrasound and mammography were found to be normal. ENT and chest diseases department were consulted with. There were restrictive findings in respiratory function tests. First degree insufficiency and diastolic dysfunction in the mitral and aortic valves were seen in the echocardiographic examination. In thoracic CT, long segment diffuse thickening was observed in the trachea and left main bronchial wall, and the posterior membranous structure was preserved. A significant narrowing of the lumen was noted due to the thickening of the trachea and left main bronchial wall. Bronchoscopy was performed in the patient whose dispnea increased, and findings compatible with CT were found. The pathology result sent from bronchoalveolar lavage came as chronic inflammation. The patient was diagnosed with "RP" in line with the clinical, histopathological and radiological findings. The patient was diagnosed with RS3PE, with the patient having arthritis accompanied by asymmetric pitting edema, seronegative, and with the absence of erosion on graphy. 48 mg/day methylprednisolone treatment was started orally in the patient who was thought to have RP and RS3PE coexistence. Methotrexate 15 mg/week and inhaler treatment was added. In the follow-up, the steroid was discontinued by reducing the monthly dose by 20%. Swelling in the dorsum of the foot, arthritis in the ankle and redness in the ear improved markedly on the 15th day of treatment. The patient's acute phase reactants regressed. No activation was observed during the patient’s outpatient clinic follow-ups.
Discussion
RP is a rare and less studied disease. Diagnostic criteria defined by Mc Adam et al. are used for RP. Our case was diagnosed with RP according to Mc Adam criteria. There is no specific laboratory or imaging tests. Auricular chondritis develops most frequently (90%) and nasal chondritis is the second most common (54- 70%). Auricular chondritis is present in most patients, with inflammation limited to the cartilaginous portion of the pinna and characteristic sparing of the lobule. Pain, discolouration or tenderness of the pinna is the initial symptom in most patients. Recurrent episodes of chondritis can lead to decomposition and fibrosis in normal cartilage tissue, leading to a cauliflower-like appearance in the ear and nasal collapse or saddle nose deformity. In our case, there was a saddle-nose deformity that developed in the last 3 months. The patient's ANCA test was negative and kidney function tests were normal. No findings suggesting GPA was found in thorax CT and ENT examination. Arthritis is the second most common presenting symptom of RP (52-85%). Classically it is an episodic, self-remitting, asymmetric, usually migratory, non-erosive and nondeforming polyarthritis. Pitting edema does not accompany. In our case, arthritis and pitting edema were together [5,6].
Recently, the possibility of dividing patients with RP into three distinct clinical phenotypes has been suggested: the hematological form representing less than 10% of patients, essentially older men with associated myelodysplasia and poor prognosis, the respiratory form representing about 25% of patients with predominant tracheobronchial involvement, and the mild and most frequent form, representing 65% of patients, with a favorable prognosis with the possibility of remission without treatment in 16% [7]. Our case is included in the second group. Laryngotracheal incidence is one of the most important causes of morbidity and mortality in RP. As in our case, laryngeal chondritis typically presents as hoarseness and dysphonia.
Initial treatment of RP with high doses of steroids is necessary to achieve symptom control, and sometimes long-term use is required to prevent relapses. Cyclophosphamide, cyclosporine, azathioprine, and methotrexate have been used alone or in addition to steroids in the event of life-threatening disease. It is imperative to recognize this unusual picture, as early diagnosis of RP and rapid initiation of immunosuppressive therapy can prevent long-term complications.
The etiopathogenesis is still unclear. Studies have shown the association of both cellular immunity changes and abnormal autoantibody response in RP. Studies have shown that 33 % of patients with RP had circulating antibodies to type II collagen in the active phase of the disease and their titres also corresponded to disease activity. As many as 37% of patients with RP have an associated hematologic disorder, connective tissue disease, vasculitis, dermatologic disorder, or other autoimmune disease.These concomitant diseases may precede, occur after RP, or be present at the same time. The most commonly reported relationship is Myelodysplastic syndrome (MDS) (6-11%). RP’s relation with Sjögren's syndrome (3-12%), RA(2-7%), systemic lupus erythematosus(1-5%), autoimmune thyroiditis(2-5%), spondyloarthritis, and chronic inflammatory bowel has been identified [5,6].
When the literature is reviewed, RS3PE and RP association was presented as a case accompanied by MDS in 2001 by Manganelli et al.[8]. The case is a 72-year-old male with MDS, a few months after the simultaneous diagnosis of RS3PE and MDS, the patient presented a clinical and pathological picture compatible with RP. When RP and RS3PE are examined separately, although the relationship between MDS is well known, RS3PE cases developing after RP have not been reported. In the case presented by Manganelli et al. these two diseases may be associated with MDS. In our case, there was only association of RP and RS3PE without hematological malignancy. In addition, unlike the other case, it is a young female patient who developed RS3PE after RP symptoms developed. Although RS3PE is known to be a disease of the elderly population, it is also seen in young age groups, but it is extremely rare. Systemic vasculitis, autoimmune diseases, and malignancy accompany in 30% of RS3PE patients [9,10].
Conclusion
Since it is a case where only two diseases are together and there is no accompanying disease, it is important in the literature. The diagnosis of both diseases is made clinically and there may be a delay in diagnosis. Early recognition of these cases and patient follow-up after diagnosis is important.
Funding
This study did not require any funding
Conflict of interest
All the authors are no conflicts of interest related to this manuscript.
Ethics
This article does not contain any studies with human participants or animals performed by any of the authors. This is a case report, and thepatient was informed and fully consents to publication.
References
- Jaksch-Wartenhorst R. Polychondropathia. Wien. Arch. Inn. Med. 6, 93–100 (1923).
- Pearson CM, Kline HM, Newcomer VD. Relapsing polychondritis. N. Engl. J.Med. 263, 51–58 (1960).
- VitaleA, Sota J, Rigante D et al.Relapsing Polychondritis:an Update on Pathogenesis, Clinical Features, Diagnostic Tools, and Therapeutic Perspectives. Curr. Rheumatol. Rep. 18(1), 3 (2016).
- McCarty DJ, O'Duffy JD, Pearson L et al. Remitting seronegative symmetrical synovitis with pitting edema. RS3PE syndrome. JAMA. 254, 2763–2767 (1985).
- Borgia F, GiuffridaR, Guarneri F et al. Relapsing Polychondritis: An Updated Review. Biomedicines. 6(3), 84 (2018)
- Kent PD, Michet Jr CJ, Luthra HS. Relapsing polychondritis. Curr. Opin. Rheumatol. 16(1), 56–61 (2004).
- Dion J, LerouxG, MouthonL et al. Relapsing polychondritis: What's new in 2017? Rev. Med. Interne.39(6), 400–407 (2018).
- ManganelliP, Delsante G, Bianchi G et al. Remitting seronegative symmetrical synovitis with pitting oedema in a patient with myelodysplastic syndrome and relapsing polychondritis. Clin. Rheumatol. 20(2), 132–135 (2001).
- Dd Joseph A, KumananT, Aravinthan N et al. An unusual case of remitting seronegative symmetrical synovitis with pitting edema: Case report and literature review. SAGE. Open. Med. Case. Rep. 8, 2050313X20910920 (2020).
- Lakhmalla M, Dahiya DS, KichlooA et al. Remitting seronegative symmetrical synovitis with pitting edema: a review. J. Investig. Med. (2020).