Research Article - Interventional Cardiology (2022)
Women with angina and myocardial SPECT perfusion defects but without significant epicardial coronary artery disease. Does a pathological SPECT result affect their long-term prognosis?
- Corresponding Author:
- Evangelos Lampas
Department of Cardiology,
Konstantopouleio General Hospital,
Athens,
Greece Agias Olgas 3-5,
PC 14233 Athens,
Greece,
E-mail: elampas@hotmail.com
Received date: 01-Aug-2022, Manuscript No. FMIC-22-59984; Editor assigned: 03-Aug-2022, PreQC No. FMIC-22-59984 (PQ); Reviewed date: 22-Aug-2022, QC No. FMIC-22-59984;Revised date: 29-Aug-2022, Manuscript No. FMIC-22-59984 (R);Published date: 05-Sep-2022, DOI: 10.37532/1755-5310.2022.14(S11).268
Abstract
Background: Women with angina and a positive SPECT for reversible ischemia but without CAD or NOCAD on ICA often pose a significant concern in terms of prognosis.
Objectives and methods: A retrospective single center study assessing cardiovascular morbidity, mortality, and MACE in women with the above-mentioned characteristics during a follow-up period of at least three years after ICA using a telephone questionnaire.
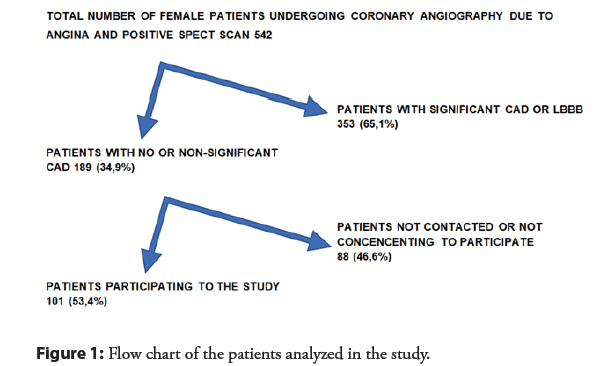
Results: We retrospectively studied women with angina and a positive SPECT for reversible ischemia that underwent ICA for a period of 7 years (from January 1, 2011 until December 31, 2017) in our hospital. Women that fulfilled the pre-specified criteria were 189. At the telephone survey, 101 (53.4%) were successfully contacted and agreed to participate. The mean age was 69.2 (SD=8.4) years and the mean followup time was 5.51 years (SD=1.69). Mortality rate was 0.99% (1 patient yet of noncardiac causes) and 0.99% rate of revascularization (also 1 patient). Eight (7.9%) were hospitalized for cardiac reasons and 13 (12.8%) patients reported symptoms of HF (no women with NYHA-Class above II). Eight (7.9%) had arrhythmic events and only one (0.99%) mild anginal symptoms. It was also noteworthy that the mortality rate in the not-contacted group derived by public security records (3 out of 88, 3,4%), did not differ significantly from the contacted group.
Conclusion: Women with angina, a positive SPECT for reversible ischemia and no CAD or non-obstructive CAD in ICA have very low risk for MACE and fatal events and an excellent long-term cardiovascular prognosis for at least 5 years.
Keywords
Women and pathological SPECT • False-positive SPECT interpretation • Coronary angiography •Coronary artery disease • Cardiac events
Abbrevations
MPI: Myocardial Perfusion Imaging; SPECT: Single-Photon Emission Computed Tomography; LBBB: Left Bundle Branch Block; CAD: Coronary Artery Disease; ECG: Electrocardiogram; HF-NYHA: Heart Failure-New York Heart Association; PCI: Percutaneous Coronary Intervention; CABG: Coronary-Aortic Bypass Surgery; NOCAD: Non-Obstructive Coronary Artery Disease; INOCA: Ischemia but Non-Obstructive Coronary Artery disease; MACE: Major Adverse Cardiac Events; CMD: Cardiovascular Coronary Dysfunction
Introduction
Lately an increasing interest has raised upon the impact of Ischemia and Non Obstructive Coronary Artery disease (INOCA) on long term prognosis of patients [1,2]. By definition, INOCA includes microvascular angina and Coronary Microvascular Dysfunction (CMD), the latter usually correlated with female sex, smoking habit, obesity, diabetes mellitus, hypertension and dyslipidemia. The prevalence of INOCA among patients with angina seems to be very high. In unselected populations referred to assessment less than 10% have obstructive CAD [3,4]. The prevalence of CMD ranges between 27 and 54% in several studies of patients with angina and NOCAD. Microvascular angina prevalence, on the other hand, varies significantly between different ethnic populations [5].
All the studies show a strong female preponderance of INOCA. A large US multi-center study showed that nearly 39% of the patients selected for coronary angiography because of suspected angina and/or positive stress test have non-obstructive CAD [6]. This frequency is higher among women (approximately 50%-70%), compared to men (30%-50%). In a retrospective registry from Eastern Denmark including 11223 patients with angina referred to coronary angiography between 1998 and 2009, 65% of women vs. 33% of men had non-obstructive CAD, with an increasing rate over the 10-year study period in both sexes, reaching up to 73% among women in 2009. Similarly, almost two-thirds (62%) of women referred to coronary angiography and enrolled in the National Heart, Lung, and Blood Institute sponsored Women’s Ischemia Syndrome Evaluation (WISE), did not have a significant obstructive stenosis [7].
The diagnostic algorithm of angina patients includes non-invasive evaluation with functional imaging [8] with several modalities available for this purpose. Myocardial Perfusion Scintigraphy (MPS) with Single Photon Emission Computed Tomography (SPECT) is a well-established diagnostic tool for ruling-in and ruling-out myocardial ischemia for patients with angina [9]. Defects in stress and rest images of a myocardial SPECT scan are considered indicative of impaired myocardial perfusion, usually due to stenosis or even total occlusion of coronary arteries [2]. The degree and level of epicardial coronary artery stenosis cannot be determined unless angiography is conducted. In angiography “normal”‐appearing coronary arteries are defined as having 0% or <20% luminal stenosis and Non–Obstructive CAD (NOCAD) is defined as coronary arteries with luminal stenosis >20% but <50%. Although traditional understanding of obstructive CAD was 70%, recent European Society of Cardiology and American College of Cardiology/American Heart Association (ACC/AHA) 269guidelines shifted to include stenosis of 50% to 70% if there is associated inducible ischemia or fractional flow reserve ≤ 0.80 when considering the physiological significance of stenosis and revascularization management in patients with stable CAD [10].
Several studies have shown a particularly high percentage of false positive SPECT scans for significant epicardial CAD, ranging from 25% up to more than 50% depending on the study, for patients with no or non-obstructive coronary artery disease [11-13]. Perfusion defects in SPECT scans of these patients may sometimes be artifacts caused by technical issues (attenuation of signal due to radiation absorption from adjacent tissues-like the diaphragm-being the most common cause) [14]. Yet there is also concern about existing pathologies in these patients (such as myocardial “bridges” or INOCA) associated with increased cardiovascular morbidity and poor prognosis in the following years, although we still have an important knowledge gap due to the absence of cardiovascular outcome trials, specifically in INOCA subjects [15-17].
In order to address these questions, we designed a study assessing the long-term prognosis of patients with angina and positive SPECT scans for reversible ischemia but no CAD or NOCAD. And since the prevalence of INOCA is higher in women we decided to focus only on female patients for this retrospective study.
Materials and Methods
Study population
A retrospective single center study was conducted, reviewing the database of the Catheterization Laboratory of a tertiary General Hospital carrying out approximately 1600-1700 catheterizations per year. Our initial search focused on women that underwent invasive coronary angiography with an indication of angina and a positive myocardial SPECT scan for reversible ischemia in at least three myocardial segments. The study’s period was seven years, finishing three years before the retrospective study was conducted, with an intention to extend the minimum follow-up period for every woman included in our study to more than three years. Women with an implanted device (pacemaker or defibrillator), LBBB morphology (due to concerns of a high probability of false positive SPECT results [18,19], history of cardiomyopathy, myocardial infarction, or myocardial revascularization with significant epicardial coronary artery disease and severe comorbidities, were excluded.
The final study group comprised women with no or non-obstructive epicardial CAD, symptoms of angina and a positive myocardial SPECT. We attempted contact telephone with the patients or their family and those that agreed to participate to the study answered a predesigned study questionnaire (Table 1). It included questions on MACE, cardiovascular morbidity, and mortality (death from any cause, cardiovascular death, hospitalization for any reason related to cardiovascular pathology, myocardial revascularization, angina, arrhythmias, and heart failure).
Moreover, for women who met the criteria but could not be contacted by telephone, we searched public records using their social security numbers and identified those who had died. That is how we created a “control group” for mortality, since we were concerned about significantly higher percentage of death in patients that could not be contacted. All other data for the deceased patients or patients that could not be contacted were not surveyed at all, since it was impossible to have consent for their inclusion in the study. The Ethics committee of our hospital had approved the protocol of the study, as well as the questionnaire used for the telephone interviews.
Myocardial perfusion scintigraphy
All SPECT studies were performed with the metastable nuclear isomer of technetium-99 (Tc-99m), radioisotope without implementation of a gated technique in most scans. Due to the retrospective nature of our study and lack of sufficient data for ischemia distribution, the SPECT results were solely classified as positive, if reversible ischemia was detected in at least three segments and negative for ischemia if <3 segments were involved.
Coronary angiography
Within a period of 3 months after the SPECT scans, ICAs were performed at the Hospital’s Catheterization Laboratory (Konstantopouleio Hospital Nea Ionia, Athens, Greece), using Philips Allura Xper FD20 X-ray system. Left heart catheterization was performed with the use of a standard Judkins technique, and images were obtained in multiple views. Angiographic results were analyzed anatomically by two experienced interventional cardiologists and significant stenosis was determined as narrowing of the vessel lumen by more than 50%. In case of any disagreement regarding the percentage of stenosis of the lesions, Invasive coronary angiography-based Quantitative Coronary Analysis (IQCA) was performed on each controversial stenotic lesion at the borderline of ~50%. Quantitative coronary analysis software on the workstation was then used to detect luminal edges, locate site of maximal stenosis, and quantify the degree of maximal stenosis. Manual edge tracing was performed, whenever automatic edge detection failed.
Statistical analysis
Variables with approximately symmetric distributions were summarized as mean and Standard Deviation (SD). For comparisons of proportions, chi-square tests were used. All p values reported are two-tailed. Statistical significance was set at 0.05 and analyses were conducted using SOFA-statistics software (version 1.5.3).
Results
We retrospectively analyzed data of all patients that underwent coronary angiography in the Catheterization Laboratory of the Konstantopouleio General Hospital of Nea Ionia, for a period of seven years (from January 1,2011 until December 31, 2017) searching for female patients that fulfilled criteria of angina and a positive myocardial SPECT scan for reversible ischemia. Women that met that criteria were 542 (from a total of 12536 angiographies). 353 of them had obstructive CAD and underwent reperfusion either with PCI or CABG, according to the ESC guidelines. The remaining 189 female patients had no or non-significant coronary artery disease and were studied further. In the subsequent telephone survey, 101 (53.4%) of them were successfully contacted, either personally or through a close relative who answered the call and agreed to participate in the study. The mean age of female patients included in the analysis was 69.2 years (SD ± 8.4) and the mean follow up time was 5.51 years (SD ± 1.69). At the time of telephone contact only one (0.99%) woman had died and from a non-cardiac cause. One (0,99%) female patient underwent revascularization (PCI) 6 years after the index coronary angiogram, and 5 patients (1,7%) had another coronary angiogram during the following years, yet without significant epicardial coronary artery disease and need for revascularization. A remarkable number of female patients had arrhythmic events in the following years, with a composite of new-onset atrial fibrillation or flutter, ablation for arrhythmias of any origin and pacemaker implantation in 8 (7.9%) patients. One woman (0.99%) reported symptoms of angina (CCS class I). The total number of hospitalized patients for cardiovascular reasons during follow up was 8 female patients (7.9%), and one woman with pulmonary oedema. Another 13 women (12.8%) reported symptoms of heart failure during follow up period, but with a mean NYHA class value of only 1.3 and no patients in NYHA class more than II. Another important finding is that the mortality rate in the group of women that could not be contacted (3 patients out of 88, 3,4%) did not differ significantly from that of the contacted patients (X2 (1, N=189 1.3283. p-value=0.249104)). Finally, the total mortality rate including contacted and not contacted group was 2.1% (4 women). The flowchart of the study is depicted in Figure 1 and the results are depicted in Table 2.
| Follow-up period from the coronary angiography | ||||||
|---|---|---|---|---|---|---|
| Demographic data | ||||||
| Age | ||||||
| Death | YES | NO | ||||
| Cause of death | Cardiac | Non-Cardiac | ||||
| Admission of the patient in a cardiology department | YES | NO | ||||
| If YES give further details | ||||||
| Coronary angiography during the follow up period | YES | NO | ||||
| Results-consultation | PCI | |||||
| CABG | ||||||
| No intervention-conservative treatment | ||||||
| No Intervention-non-obstructive CAD | ||||||
| Symptoms during the follow up period | ||||||
| Angina | No | Yes | (CCS CLASS….) | |||
| Heart failure | No | Yes | (ΝΥΗΑ CLASS….) | |||
| New atrial fibrillation-flutter | No | Yes | ||||
| Implantable device | No | Yes | PACEMAKER | ICD | CRT | |
Abbreviations: PCI: Percutaneous Coronary Intervention; CABG: Coronary-Aortic Bypass Surgery; CAD: Coronary Artery Disease; NYHA: New York Heart Association; ICD: Implantable Cardioverter-Defibrillator; CRT: Cardiac Resynchronization Therapy
Table 1: Study questionnaire.
| Number of women contacted (101) | |
|---|---|
| Mean Age years (standard deviation) | 69.22 (8.4) |
| Follow up years after angiography (standard deviation) | 5.51yrs (1.69) |
| Deaths (none of them of cardiac origin) | 1 (0.99%) |
| Revascularization (PCI/CABG+valve) | 1 (0.99%) |
| Angina (CCS class I) | 1 (0.99%) |
| Angiography-no serious CAD | 5 (1.7%) |
| Hospitalization for cardiovascular reasons (ACS, PCI, Arrhythmic events and ablation, Device implantation) | 8 (7.9%) |
| Arrhythmic events/Interventions | 8 (7.9%) |
| NYHA symptoms | 13 (12.8%) I-II class |
| Valve replacement | None |
| Number of women not contacted (88) | |
| Deaths of unknown origin (data derived from public records) | 3 (3.4%) |
| Total Deaths (contacted or not) | 4 (2.1%) |
Abbreviations: CAD: Coronary Artery Disease; ACS: Acute Coronary Syndrome; PCI: Percutaneous Coronary Intervention; CABG: Coronary-Aortic Bypass Surgery; NYHA: New York Heart Association
Table 2: Study Results of female patients with no or non- significant coronary artery disease (total number 189).
Discussion
This was a small retrospective single-center study that showed women with angina and a SPECT scan indicative of reversible ischemia but no CAD or NOCAD have very low cardiovascular morbidity and mortality and an excellent long-term prognosis in the following years. The particularly long average follow-up time of the study, more than 5.5 years, with no cardiac deaths and a very low rate of revascularization during the follow-up period enhance the value of our results. The fact that the rate of death in the “lost to follow-up” female patients did not differ significantly from the contacted women could be considered as indices of similarity between the two groups, at least for major outcomes. The rate of hospitalization for cardiovascular reasons during the follow-up period is quite low and the majority is related to arrhythmic events and conduction disturbances rather than acute coronary syndromes. A significant percentage of women reported symptoms of heart failure but most of them in NYHA class I and with no related hospitalizations reported. The particularly low number of patients complaining about persistent angina is interesting and raises questions about the true percentage of women with INOCA in our study group. The lack of data about the use of anti-anginal medication after the initial assessment of our female population and the fact that the questionnaire used is not validated for adequately assessing anginal symptoms could perhaps explain this inconsistency with previously published data [1].
It is undoubtful that our study lacks sufficient data to identify how many of our patients had true dynamic macro- or microvascular impairment, which could explain the positive SPECT scan results, and how many were just “victims” of artifacts of the SPECT study. None of the women in our study population underwent vasoreactivity tests during angiography that could answer such questions. Yet, the very low overall rate of dismal outcomes in the majority of women during a long follow up period probably renders such a quest unnecessary.
Our study had a low total rate of false positive interpretations of myocardial SPECT scans. Such rates are reported in early performance studies of MPS for the diagnosis of coronary artery disease, with a significant number of gated SPECT scans and supine and prone acquisitions [20]. Yet later “real world” series report significantly higher rates of false positive scans above 50%, raising questions on the accuracy of the method in ruling-in patients for coronary artery disease and the subsequent cost of such a strategy. An explanation for our low rate of false positive interpreted scans could be the fact that we excluded from analysis all patients that had an LBBB morphology at rest ECG before coronary angiogram. Furthermore, recent literature suggests that this morphology could be a source of increased falsely positive SPECT scans and subsequently misdiagnosis, leading to unnecessary coronary angiograms [18].
Our study has numerous limitations. First, the retrospective nature of the study and the lack of thorough clinical information, medical history and medication of our female population when they underwent the SPECT scan, and the index coronary angiography deprives us of data regarding the etiology of the false positive results of SPECT scans. Second, the considerable number of women that could not be contacted raises suspicion of a higher mortality/morbidity and cardiovascular events rate in that group. Yet the fact that the data derived from public social security records did not differ significantly as far as mortality irrespectively of the etiology is concerned is reassuring. Follow up via telephone contact with a non-validated questionnaire is another limitation and could question the accuracy of answers, particularly when quantitative data like NYHA score are assessed.
Limitations regarding the SPECT results include the lack of data regarding the percentage of exercise stress versus vasodilator stress SPECT scans in our sample and the low percentage of gated SPECT scans. The limited SPECT scan data regarding the amount and distribution of area at risk in non-revascularized patients, yet with a diagnosis of “positive SPECT”, may have contributed to the minuscule cardiovascular morbidity and mortality in the years following the index coronary angiography.
Finally, we observed a very low morbidity and mortality rate in our women population during more than 5 years follow up. This result is not in accord with other INOCA studies. For example, the National Heart, Lung, and Blood Institute-sponsored Women’s Ischemia Syndrome Evaluation (WISE) study, depicted that the prognosis of patients with INOCA is far from benign [1]. Since no 272reactivity tests were performed to determine the cause for falsely positive SPECT scan results (artifacts, INOCA or others) may be one of the reasons for this discrepancy with previous data.
Conclusion
Women are the majority of patients with symptoms of angina and a diagnosis of INOCA after a positive imaging functional test like SPECT and a coronary angiography with no or non-significant CAD. In this small retrospective study, we showed that the long-term prognosis for female patients with angina and a positive SPECT scan for reversible myocardial ischemia with no or non-obstructive epicardial coronary artery disease is excellent as far as cardiovascular morbidity and mortality are concerned, irrespective of the definite diagnosis of INOCA or other pathology. We also depicted that the exclusion of patients with an LBBB morphology in resting ECG can improve the diagnostic accuracy of myocardial SPECT scans regarding detection of significant CAD.
Acknowledgments
We gratefully acknowledge the help of the staff of the Catheterization Laboratory of Konstantopouleio General Hospital Nea Ionia, Athens, Greece.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing Interest
All authors have no conflicts of interest to declare.
References
- Kunadian V, Chieffo A, Camici PG, et al. An EAPCI expert consensus document on ischaemia with non-obstructive coronary arteries in collaboration with European Society of Cardiology working group on coronary pathophysiology and microcirculation endorsed by coronary vasomotor disorders international study group. Eur Heart J. 41(37): 3504-3520 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Schuijf JD, Matheson MB, Ostovaneh MR, et al. Ischemia and No Obstructive Stenosis (INOCA) at CT angiography, CT myocardial perfusion, invasive coronary angiography, and SPECT: The CORE320 study. Radiology. 294(1): 61-73 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Reeh J, Therming CB, Heitmann M, et al. Prediction of obstructive coronary artery disease and prognosis in patients with suspected stable angina. Eur Heart J. 40(18): 1426-1435 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Douglas PS, Hoffmann U, Patel MR, et al. Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med. 372: 1291-1300 (2015).
[CrossRef] [Google Scholar] [PubMed]
- Shimokawa H, Suda A, Takahashi J, et al. Clinical characteristics and prognosis of patients with microvascular angina: an international and prospective cohort study by the Coronary Vasomotor Disorders International Study (COVADIS) Group. Eur Heart J. 42(44): 4592-4600 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Pepine CJ, Anderson RD, Sharaf BL, et al. Coronary microvascular reactivity to adenosine predicts adverse outcome in women evaluated for suspected ischemia results from the National Heart, Lung and Blood Institute WISE (Women’s Ischemia Syndrome Evaluation) study. J Am Coll Cardiol. 55(25): 2825-2832 (2010).
[CrossRef] [Google Scholar] [PubMed]
- Sharaf B, Wood T, Shaw L, et al. Adverse outcomes among women presenting with signs and symptoms of ischemia and no obstructive coronary artery disease: Findings from the National Heart, Lung, and Blood Institute-sponsored Women’s Ischemia Syndrome Evaluation (WISE) angiographic core laboratory. Am Heart J. 166(1): 134-141 (2013).
[CrossRef] [Google Scholar] [PubMed]
- Miller TD, Askew JW, Anavekar NS. Noninvasive stress testing for coronary artery disease. Cardiol Clin. 32(3): 387-404 (2014).
[CrossRef] [Google Scholar] [PubMed]
- Sakata K, Iida K, Kudo M, et al. Prognostic value of I-123 metaiodobenzylguanidine imaging in vasospastic angina without significant coronary stenosis. Circ J. 69(2): 171-6 (2005).
[CrossRef] [Google Scholar] [PubMed]
- Herscovici R, Sedlak T, Wei J, et al. Ischemia and No Obstructive Coronary Artery Disease (INOCA): What is the risk? J Am Heart Assoc. 7(17): e008868 (2018).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Knuuti J, Ballo H, Juarez-Orozco LE, et al. The performance of non-invasive tests to rule-in and rule-out significant coronary artery stenosis, in patients with stable angina: A meta-analysis focused on post-test disease probability. Eur Heart J. 39: 3322-3330 (2018).
[CrossRef] [Google Scholar] [PubMed]
- Silva T, Ramos R, Rio R. False positive results of SPECT-we should minimize the unnecessary referrals to invasive coronary angiography. P5336 | BEDSIDE European Cardiology Congress. (2013).
- Escandarian R, Razavi MR, Safaei S, et al. Evaluation of the correlation between myocardial perfusion scan findings and invasive coronary angiography results. Middle East J Rehabil Health. 4(2): e45216 (2017).
- Burrell S, MacDonald A. Artifacts and pitfalls in myocardial perfusion imaging. J Nucl Med Technol. 34: 193-211 (2006).
[Google Scholar] [PubMed]
- Vallejo E, Morales M, Sánchez I, et al. Myocardial perfusion SPECT imaging in patients with myocardial bridging. J Nucl Cardiol. 12(3): 318-23 (2005).
[CrossRef] [Google Scholar] [PubMed]
- Sakata K, Iida K, Kudo M, et al. Prognostic value of I-123 metaiodobenzylguanidine imaging in vasospastic angina without significant coronary stenosis. Circ J. 69(2): 171-6 (2005).
[CrossRef] [Google Scholar] [PubMed]
- Soman P, Dave D, Udelson J, et al. Vascular endothelial dysfunction is associated with reversible myocardial perfusion defects in the absence of obstructive coronary artery disease. J Nucl Cardiol. 13(6): 756-60 (2006).
[CrossRef] [Google Scholar] [PubMed]
- Higgins JP, Williams G, Nagel JS, et al. Left bundle-branch block artifact on single photon emission computed tomography with technetium Tc 99m (Tc-99m) agents: Mechanisms and a method to decrease false-positive interpretations. Am Heart J. 152(4): 619-26 (2006).
[CrossRef] [Google Scholar] [PubMed]
- Koepfli P, Wyss CA, Gaemperli O, et al. Left bundle branch block causes relative but not absolute septal underperfusion during exercise. Eur Heart J. 30(24): 2993-9 (2009).
[CrossRef] [Google Scholar] [PubMed]
- Berman DS, Kang X, Nishina H et al. Diagnostic accuracy of gated Tc-99m sestamibi stress myocardial perfusion SPECT with combined supine and prone acquisitions to detect coronary artery disease in obese and non-obese patients. J Nucl Cardiol. 13(2): 191-201 (2006).
[CrossRef] [Google Scholar] [PubMed]