Research Article - Imaging in Medicine (2021) Volume 13, Issue 8
Vascular abnormalities in patients with COVID-19 pneumonia
Elias El-Haddad1,2*, Najib Pascal Chalhoub1,2, Mohammad Rida1,2, Samer Abi-Khalil1,2, Tonine Younan1,2, Sami Slaba1,2, Soha Haddad- Zebouni1,2
1Medical Imaging Department, Hôtel-Dieu de France Hospital, Alfred- Naccache Avenue, Achrafieh, BP 16- 6830, Beirut, Lebanon
2Department of Medicine, Saint Joseph University, Damascus Road, Riad El Solh, BP 11-5076, Beirut, Lebanon
- Corresponding Author:
- Elias El-Haddad
Department of Medicine
Saint Joseph University
Damascus Road
Riad El Solh
BP 11-5076
Beirut
Lebanon
E-mail: haddad.elias@gmail.com
Abstract
Purpose: Describe CT findings in patients with COVID-19 pneumonia, focusing on the vascular aspects, during the novel coronavirus pandemic.
Materials and methods: In this prospective single-institutional study we included patients admitted to the emergency department between March 1 and April 4, 2020 with a SARS-CoV-2 pneumonia. We report findings on chest CT from 59 patients (35 men, 24 women, mean age 52.54 years).
Results: Among the symptoms found: fever (78%), cough (42.4%), dyspnea (39%) and headache (6.8%). Initial reverse transcriptase polymerase chain reaction (RT-PCR) was positive in 81.4%, becoming positive on retesting. Intensive care unit (ICU) admission rate was 23.7%. A total of 59 scans were obtained, describing distribution: left (8.7%) right (32.6%) or bilateral (58.7%) with the most common localization being the right lower lobe (84.8%). Findings included focal ground glass opacities (GGO) (10.9%) or multiple GGO (89.1%), consolidation (37%), crazy paving (32.6%), reversed halo sign (17.4%) and traction bronchiectasis (76.1%).
We reported vascular aspects such as enlargement (78.3%), irregularities (58.7%) and distortion (58.7%). A severity score based on lung involvement was estimated over a score of 25 with a mean of 6.4 (range: 0 to 22) and it was correlated with age (p<0.05). Other correlations included abnormal CT findings and male sex (p=0.001). Vascular angulation and traction were correlated with multifocal GGO, traction bronchiectasis, crazy paving, reversed halo sign and male sex (p<0.05).
Conclusion: Those signs can raise the possibility of concomitant vasculitis in patients with COVID-19 pneumonias.
Keywords
COVID-19 ▪ thorax ▪ tomography ▪ X-Ray Computed ▪ pneumonia ▪ vasculitis
Introduction
The SARS-CoV-2, from the family of the Coronaviridae, is the seventh zoonotic infection to affect humans after the Severe Acute Respiratory Syndrome (SARS) in 2002-2003 and the Middle East Respiratory Syndrome (MERS) in 2012 [1,2]. It was first reported in December 2019 during a large outbreak in Wuhan, Hubei Province, China. It has since spread rapidly worldwide until the first case was declared in Lebanon by the ministry of public health on February 21, 2020 [3].
The on-going pandemic of the novel coronavirus has raised international concerns in more than 190 nations, affecting more than 200 million individuals and responsible for more than 4 million deaths. In December 2020, the first dose of a fully tested vaccine manufactured by Pfizer/BioNTech was administered. By the date of submission of this article, more than 4 billion doses of Covid-19 vaccines were administered worldwide [1].
Chest CT-scan was found to be a rapid and practical modality, playing an important role in the diagnosis and management of the COVID-19 [4] and has been largely used during the outbreak as it raised public health concerns for early diagnosis and management. Several studies described typical or usual aspects of the COVID-19 pneumonia as bilateral and peripheral predominant Ground-Glass Opacity (GGO), consolidation or both and less frequently crazy paving, reverse halo sign and bronchial distortion [2,4,5]. Chest CT images have been reported to provide 98% sensitivity in screening for SARS-CoV-2 infections [6]. In a recent study done by Ai et al, chest CT scan had higher sensitivity in diagnosing COVID-19 compared with initial reverse transcriptase polymerase chain reaction (RT-PCR) [5] with a nasal swabs sensibility around 53.6% to 73.3% [7]. Therefore, patients with COVID-19 pneumonia may have CT findings but an initially negative RT-PCR. This highlights the importance of using multiple detection methods to ensure accurate patient diagnosis.
“Vascular enlargement sign” was one of the few radiological aspects reported; in fact, Haiying et al. found this sign prevalent in 67% of the cases, supporting a promising role for Vascular enlargement sign in identifying pneumonia caused by coronavirus [8].
In this study, our aim is to report chest CT findings in patients with COVID-19 pneumonia and describe particularly vascular aspects on imaging.
Materials and Methods
▪ Study design and patients recruitment
This is a prospective, single-institutional, observational study, conducted at the radiology department of Hôtel-Dieu de France university hospital in Beirut, Lebanon, from March 1 to April 4, 2020. It included all individuals who were admitted to the emergency department of the hospital for symptoms suspicious of COVID-19 infection, and were therefore tested by RT-PCR for SARS-CoV-2 and underwent chest CT-scan imaging. The study was approved by the Ethical Committee of the Saint Joseph University and informed consent was waived.
Inclusion criteria were:
1. Confirmed positive RT-PCR for SARSCoV- 2
2. Suspicion of lower respiratory tract infection with SARS-CoV-2 after being in contact with a positive patient or after coming back from abroad even with a negative initial RT-PCR. The latter became positive on subsequent testing (patients were retested due low sensitivity of the RT-PCR in this setting).
Exclusion criteria were the absence of chest CT scan or a second negative RT-PCR.
▪ CT-scan protocol
All chest CT images were acquired on GE LightSpeed VCT64 with the following parameters: (a) Supine position with maximum inspiration and breath-holding; (b) Adaptive tube current, 1.25 mm section thickness, 1.25 mm interval and 120 kVp. Post treatment of the images was done on GE Advantage Windows 4.X.
▪ Image analysis
Each scan was read by three different radiologists; one had 20 years’ experience in interpreting chest CT and the two others were radiology fellows. They reviewed all images and described the distribution of the lesions (unique or multiple, affected lobe) and aspects of pneumonias (GGO, consolidation, crazy paving, reversed halo, bronchial traction). Pulmonary vessel abnormalities were reported either as vascular enlargement (abnormal augmented vessel size in a peripheral area or within the GGO compared to another vessel at the same level), vessel irregularities (e.g. ectasia and stenosis within the GGO compared to another vessel at the same level) or vessel distortion (vessel angulation with the affected area) after volume rendering.
We used the semi-quantitative scoring system developed by F Pan et al. to assess the involvement based on the percentage of pathologic parenchyma [9]. Each lobe was scored from 0 to 5 as follows: 0, no involvement; 1, <5% involvement; 2, 5% to 25% involvement; 3, 26% to 49% involvement; 4, 50% to 75% involvement; 5, >75% involvement. The total CT score was the sum of the individual lobar scores and ranged from 0 (no involvement) to 25 (maximum involvement).
▪ Statistical analysis
Continuous variables were described by their mean and categorical variables by the numbers (N) and percentages (%) of each category. All continuous variables were analyzed as such and not categorized. Pearson correlation was used for the evaluation of the relationship between two continuous variables, t- test was used when evaluating the difference in the mean of two independent groups, and Chi-square test were used for the comparison of categorical variables between groups. All tests were two-tailed and considered statistically significant for p<0.05. SPSS Statistics version 25.0 (IBM Corporation, New York, USA) was used for statistical analysis.
Results
A total of 59 patients were recruited; 35 were men (59.3%) and 24 were women (40.7%). Patients were aged between 22 and 87 years old, with a mean age of 52.5 years. Among the clinical symptoms at presentation, fever was present in 46 patients (78%), cough in 25 cases (42.4%), dyspnea in 23 (39%), while headache was observed in 4 (6.8%) patients. Fourteen patients (23.7%) had a severe infection and were admitted to the Intensive Care Unit (ICU) (TABLE 1).
| Characteristics | COVID-19 |
|---|---|
| Patients(N=59) | |
| Age(y) | |
| Mean | 52.54 |
| Range | 22-87 |
| Sex, no (%) of patients | |
| Male | 35(59.3) |
| Female | 24(40.7) |
| Positive initial RT-PCR | 81.40% |
| ICU admission | 14(23.7) |
| Chest CT | |
| Abnormal | 46(78%) |
| Normal | 13(22%) |
| Symptoms at presentation, no (%) of patients | |
| Fever | 46(78%) |
| Cough | 25(42.4) |
| Dyspnes | 23(39%) |
| Headache | 4(6.8) |
TABLE 1: Patients’ characteristics in the study. Percentages may not add up to 100 because of rounding
Initial RT-PCR for SARS-CoV-2 was positive in 81.4% of the cases. Negative patients had a history of confirmed contact with a positive patient or came back from highly epidemic areas with suggestive findings on chest CT scan and later became positive on retesting, hence they were added to our population.
Of the 59 patients, 46 (78%) had abnormalities on chest CT-scan and 13 (22%) had normal findings. Among the abnormalities all patients had GGO: 5 (10.9%) had single focal GGO and 41(89.1%) had multifocal GGO. Other findings included 17 (37%) with consolidation, 15 (32.6%) with crazy paving, 8 (17.4%) with reversed halo sign and 35 (76.1%) with traction bronchiectasis (TABLE 2).
| CT findings | No (%) of patients (N=46) |
|---|---|
| GGO* | |
| Focal GGO* | 5(10.9) |
| Multiple GGO* | 41(89.1) |
| Consolidation | 17(37) |
| Crazy paving | 15(32.6) |
| Reverse Halo sign | 8(17.4) |
| Traction bronchiectasis | 35(76.1) |
| Vascular abnormalities | |
| Vessel enlargement | 36(78.3) |
| Vessel irregularities | 27(58.7) |
| Vessel distortion (angulation) | 27(58.7) |
*Note: GGO: ground-glass opacities.
TABLE 2: CT findings of 46 patients with confirmed SARS-CoV-2 infection. Percentages may not add up to 100 because of rounding
In terms of lesion distribution, it was predominantly peripheral in 36 patients (78.3%) peripheral and central in 10 patients (21.7%) cases, and none with central abnormalities. 27 patients (58.7%) had bilateral disease, 15 (32.6%) only right findings and 4 (8.7%) only left findings. Lobe distribution was as following: 24 (52.2%) in the right upper lobe, 18 (39.1%) in the middle lobe, 39 (84.8%) in the right lower lobe, 20 (43.5%) in the left upper lobe and 27 (58.7%) in the left lower lobe. Of the 5 patients with a single lesion, three (60%) had lesions that were initially located in the right lower lobe; and the other two had lesions in the right upper and middle lobes each (TABLE 3).
| Distribution | No (%) of patients (N=46) |
|---|---|
| Peripheral | 36(78.3) |
| Peripheral and central | 10(21.7) |
| Bilateral | 27(58.7) |
| Left lung | 4(8.7) |
| Right lung | 15(32.6) |
| Left | |
| Left upper lobe | 20(43.5) |
| Left lower lobe | 27(58.7) |
| Right | |
| Right upper lobe | 24(52.2) |
| Middle lobe | 18(39.1) |
| Right lower lobe | 39(84.8) |
TABLE 3: Lesions’ distribution in 46 patients with COVID-19 pneumonia. Percentages may not add up to 100 because of rounding.
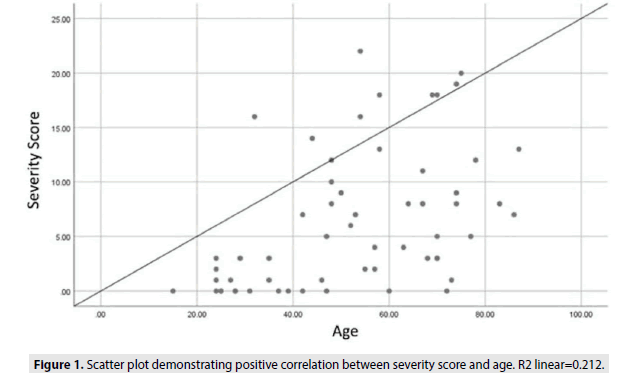
Severity score of chest CT ranged from 0 to 22, with a mean score of 6.4. We noted a positive correlation between the age and the severity score, with older individuals having higher scores (p<0.05) as reported in the scatterplot (FIGURE 1).
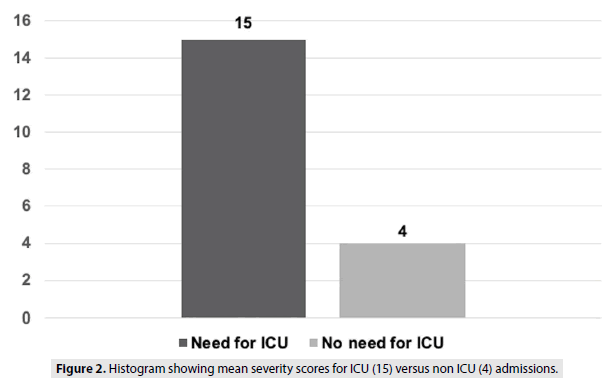
On the other hand, 85% of the patients admitted to the ICU had a severity score above 10 (only 2 patients had a score of 6 and 8 each) with a mean score of 15. Among patients that did not require an ICU admission, the mean severity score was 4 (FIGURE 2).
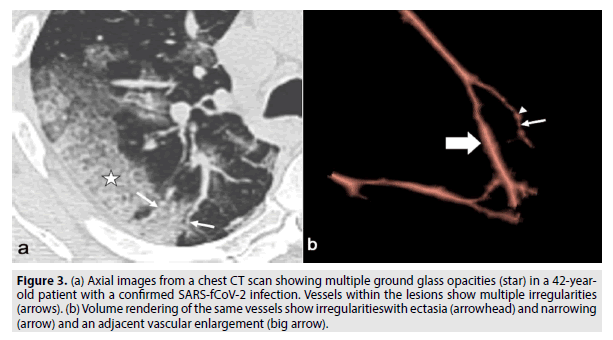
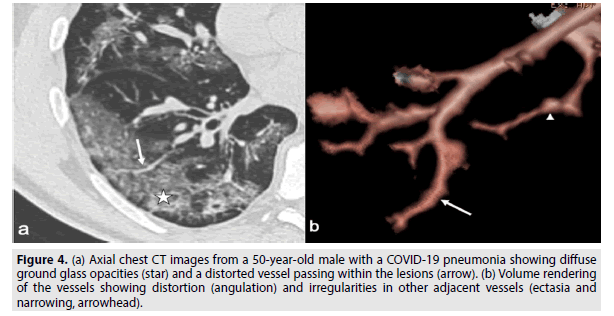
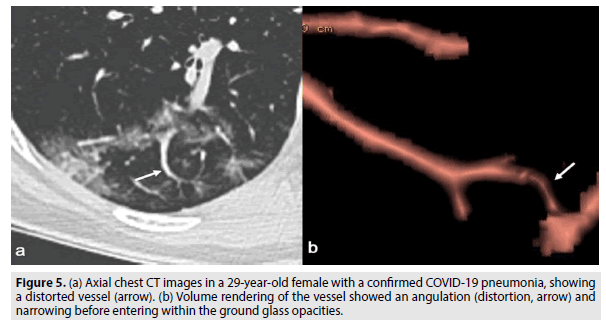
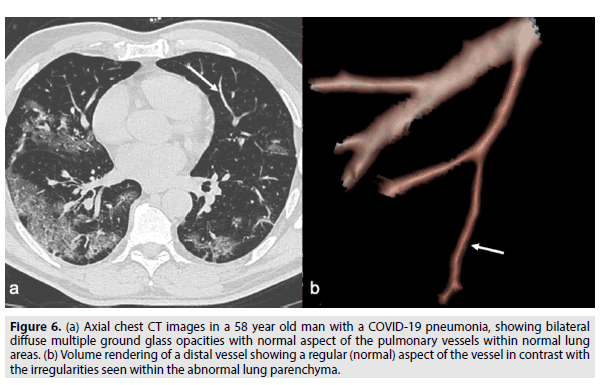
All images were interpreted, and volume rendered on GE Advantage Window 4.X to interpret pulmonary vascular aspects showing enlargement, irregularities and angulation, as seen in Figures 3-5 in contrast with the normal vessel seen in figure 6 (FIGURES 3-6).
FIGURE 3: (a) Axial images from a chest CT scan showing multiple ground glass opacities (star) in a 42-yearold patient with a confirmed SARS-fCoV-2 infection. Vessels within the lesions show multiple irregularities (arrows). (b) Volume rendering of the same vessels show irregularitieswith ectasia (arrowhead) and narrowing (arrow) and an adjacent vascular enlargement (big arrow).
FIGURE 4: (a) Axial chest CT images from a 50-year-old male with a COVID-19 pneumonia showing diffuse ground glass opacities (star) and a distorted vessel passing within the lesions (arrow). (b) Volume rendering of the vessels showing distortion (angulation) and irregularities in other adjacent vessels (ectasia and narrowing, arrowhead).
FIGURE 6: (a) Axial chest CT images in a 58 year old man with a COVID-19 pneumonia, showing bilateral diffuse multiple ground glass opacities with normal aspect of the pulmonary vessels within normal lung areas. (b) Volume rendering of a distal vessel showing a regular (normal) aspect of the vessel in contrast with the irregularities seen within the abnormal lung parenchyma.
One of the main signs reported were vascular abnormalities: 36 (78.3%) had vascular enlargement, 35 (76.1%) had vessel traction, 27 (58.7%) had vessel irregularities and distortion and 27 (58.7%) had vessel angulation.
Although no significant correlation was noted between scan abnormalities and positive RTPCR (p=0.1), we found a statistical difference with patients who were admitted to the ICU and imaging (p=0.026) as well as those with fever (p=0.027) and headache (p=0.03) but neither with cough nor dyspnea (p>0.05).
Of the 59 patients, abnormal CT findings were more seen in men than women with 33 males and 13 females having abnormal findings while 2 males and 11 females had a normal exam, with a statistical significance (p=0.001).
Our analysis was mainly focused on vascular abnormalities and their correlations with other variables. There was no correlation between unifocal GGO and any vascular finding. Vessel angulation was almost always seen with multifocal GGO and traction bronchiectasis and frequently associated with crazy paving, reversed halo sign and male sex (p<0.05). Vessel distortion and irregularities were associated with multifocal GGO, reversed halo sign and bronchial traction (p<0.05) but not with crazy paving (p=0.07) nor sex (p=0.1). Moreover, vessel traction was correlated with multifocal GGO, consolidation, crazy paving, reversed halo, bronchiectasis and male sex (p<0.05).
Discussion
In our cohort, the initially positive RT-PCR’s rate was 81.4% with the rest turning positive on later testing. 19.6% of patients who had a negative RT-PCR at admission later became positive. Therefore, we can conclude that many parenchymal aspects described above can be suggestive of COVID-19 pneumonia especially in the setting of a pandemic and consider patient isolation even before RT-PCR results.
Initial chest CT was normal in 13 patients with confirmed positive RT-PCR. There was a statistical significance between sex (11 women and 2 men). We concluded that women with a positive RT-PCR have usually less CT findings than men, however most of these women were hospital staff (nurses, orderlies) that were diagnosed early with mild symptoms, or just dyspnea later explained by their anxious state.
Our model showed correlation between CT findings with fever and headache but not cough or dyspnea. The latter signs being very subjective and usually noted in patients, many of whom were hospital staff. Therefore, with many healthcare workers on the frontline with the virus causing occupational health risks [10], we suggest massive RT-PCR testing and a CT scan in asymptomatic healthcare workers (especially males) or in case of fever of headache, especially with the lack of sufficient Personal Protective Equipment (PPE) and awareness of personal protection [11].
We then analyzed correlation between ICU admission and CT findings, and the difference was significant, which is coherent with the fact that ICU admission in the setting of COVID-19 is primarily caused by pulmonary involvement objectified by lung abnormalities on CT. 85% of the patients admitted to the ICU had a severity score above 10 (only 2 patients had a score of 6 and 8 each), so we can consider 10 as a cutoff value, in addition to clinical status, to assess patient’s admission to the ICU.
While 13 patients had normal CT findings, 46 had signs suggestive of a COVID-19 infection. The most frequent sign being peripheral ground glass opacities in all of them. Ten of these patients had concomitant central GGO. Other findings included consolidation, crazy paving and reversed halo sign, similar to those described by Li et al (2). We also realized that there was a pattern in the laterality in the distribution of the abnormalities notably the GGO with greater involvement of the right lung compared to the left. The right lower lobe being most involved, this can be explained by the anatomical more obtuse angulation of the right lower lobar bronchus that can participate in the predominant infection in the lower right lobe via the inhalation of the virus containing droplets.
Our focus in this study is the aspect of the pulmonary arteries vasculature on CT in the setting of COVID- 19 infection. The most commonly seen sign was the vascular angulation or distortion. Its association with the multifocal GGO, traction bronchiectasis and crazy paving may be due to the high inflammatory state in the lung parenchyma with the involvement with the lung interstitium [12]. It is responsible for the distortion of the lung parenchyma thus the bending of the vessels. Histologic studies of COVID-19 affected lung parenchyma showed clusters of focal fibrin with inflammatory cellular infiltration and multinucleated giant cells suggesting early fibrosis [13] and may explain the traction bronchiectasis close to the GGO areas that may contain early stages of fibrotic changes.
Vascular enlargement was frequent in our population, as described already by many other authors [2,12,14] is a dilatation of the pulmonary vasculature within or around the lesions seen on CT. This manifestation may be due to alveolar damage impairing oxygen flow, increasing the surface of air exchange, increased blood supply to the inflammatory area and most probably due to local Nitric Oxide (NO) secretion.
Another vascular finding is the vessel irregularity, which is an alternation of narrowing and ectasia of the vascular lumen. It was observed in the vessels passing through the ground glass opacities. This distortion is seen in vasculitic changes. Lumen narrowing and distal ectasia involving pulmonary vasculature is seen in Granulomatosis with polyangiitis, causing necrotizing vasculitis [15]. Infections are a cause of secondary vasculitis [16] which supports our hypothesis especially that viral infections are known to be incriminated with immune mediated vasculitis. Kawazaki disease was associated in 2004 to infection by The New-Haven Coronavirus HCovNH [17] which also supports our hypothesis of vasculitic changes in pulmonary vessels in the COVID-19.
Both vascular changes (irregularities and angulation) were associated in our study with the male sex. In fact, the female population, as cited before, has a high rate of normal CT findings which makes it more probable for men to have more abnormal CT findings. In addition, men are most likely to get infected by the COVID-19 [18], and it is also found in our cohort, which makes it more likely to find vascular abnormalities in chest CT compared to women in the setting of a COVID infection.
To enhance our hypothesis, we tried to compare our vascular findings with the scleroderma renal crisis in which we find increased vascular permeability, activation of coagulation cascade, and renin secretion, that may lead to the acute renal failure manifesting as prominent small vessel involvement and thrombotic microangiopathy on pathology [19]. During the outbreak in China, many reports described an increase in the coagulation state of COVID-19 patients [20,21]. In the nephrogram of renal scleroderma, vascular signs seen arteriographically were pronounced proximal arterial ectasia and severe interlobular arterial narrowing [22]. The scleroderma renal crisis is known to be triggered by corticosteroids and during this pandemic of COVID-19, some studies showed that corticosteroids may lead to severe and adverse reactions and deterioration of the disease [23-26]. This lead us to point out that the similarities of both diseases on imaging (vascular irregularities) and pathophysiology (hypercoagulopathy and worsened by corticosteroids) can be taken into consideration to emphasize on the possible “vasculitis” associated with the COVID-19.
One possible type of bias is the experimenter bias where the knowledge of the status of the RT-PCR could influence the interpretation of CT-scan results. In fact, during this global pandemic, there is a trend among radiologists to search more for and describe the lesions that could be related to COVID-19 pneumonia which could be sometimes misleading and could be leading to missing other alternative diagnoses. Therefore, although COVID-19 pneumonia should be suspected and looked for in every suspicious patient, physicians should always keep in mind other differentials presenting with similar symptomatology. On a last note, the vascular abnormalities associated with COVID-19 pneumonia raise the possibility of concomitant vasculitis especially with many treatments were tested in COVID-19 patients such as hydroxychloroquine, azithromycin and Ivermectin which are known to have immunomodulation properties. More studies need to be conducted in order to explore the histological and immunological pathways in these vasculitic changes seen on imaging and perhaps help to find a targeted treatment.
Conclusion
To sum up, the most frequent aspect of the COVID-19 pneumonia was peripheral ground glass opacities. Concerning the vascular aspects - which are our focus in this study - the most commonly seen sign was the vascular angulation or distortion. Vascular enlargement sign was frequent in our population. Another vascular finding was the vessel irregularity, the alternation of narrowing and ectasia of the vascular lumen. The latter finding is seen in some vasculitis raising the possibility of concomitant vasculitis. More studies need to be conducted in order to explore the histological and immunological pathways in these vasculitic changes seen on imaging and perhaps help to find a targeted treatment.
Acknowledgements
The authors would like to express their appreciation for all of the nurses, doctors and hospital staff for their efforts to combat the COVID-19 outbreak.
References
- Novel Coronavirus (2019-nCoV) situation reports (2021).
- Li Y, Xia L. Coronavirus disease 2019 (COVID-19): Role of chest CT in diagnosis and management. AJR Am J Roentgenol. 214(6), 1280-1286 (2020).
- Lebanese Ministry of Public Health website (2020).
- Wang Y, Dong C, Hu Y et al. Temporal changes of CT findings in 90 patients with COVID-19 pneumonia: A longitudinal study. Radiology. 296(2), E55-E64 (2020).
- Ai T, Yang Z, Hou H et al. Correlation of chest CT and RT-PCR testing for coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases. Radiology. 296(2), E32-E40 (2020).
- Fang Y, Zhang H, Xie J et al. Sensitivity of chest CT for COVID-19: Comparison to RT-PCR. Radiology. 296(2), E115-E117 (2020).
- Yang Y, Yang M, Shen C et al. Evaluating the accuracy of different respiratory specimens in the laboratory diagnosis and monitoring the viral shedding of 2019-nCoV infections. 1-17 (2020).
- Lv H, Chen T, Pan Y et al. Pulmonary vascular enlargement on thoracic CT for diagnosis and differential diagnosis of COVID-19: a systematic review and meta-analysis. Ann Transl Med. 8(14), 878 (2020).
- Pan F, Ye T, Sun P et al. Time course of lung changes at chest CT during recovery from coronavirus disease 2019 (COVID-19). Radiology. 295(3), 715-721 (2020).
- Gan WH, Lim JW, Koh D. Preventing intra-hospital infection and transmission of coronavirus disease 2019 in health-care workers. Saf Health Work. 11(2), 241-243 (2020).
- Wang J, Zhou M, Liu F. Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp Infect. 105(1), 100-101 (2020).
- Zhou S, Wang Y, Zhu T, Xia L. CT features of coronavirus disease 2019 (COVID-19) pneumonia in 62 patients in Wuhan, China. AJR Am J Roentgenol. 214(6), 1287-1294 (2020).
- Tian S, Hu W, Niu L et al. Pulmonary pathology of early-phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. J Thorac Oncol. 15(5), 700-704 (2020).
- Jain A, Patankar S, Kale S, Bairy A. Imaging of coronavirus disease (COVID-19): a pictorial review. Pol J Radiol. 86, e4-e18 (2021).
- Hur JH, Chun EJ, Kwag HJ et al. CT features of vasculitides based on the 2012 international chapel hill consensus conference revised classification. Korean J Radiol. 18(5), 786-798 (2017).
- Belizna CC, Hamidou MA, Levesque H, Guillevin L, Shoenfeld Y. Infection and vasculitis. Rheumatology (Oxford). 48(5), 475-482 (2009).
- Esper F, Shapiro ED, Weibel C et al. Association between a novel human coronavirus and Kawasaki Disease. J Infect Dis. 191(4), 499-502 (2005).
- Guan W, Ni Z, Hu Y et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. (2020).
- Stein LB. Coagulopathy associated with COVID-19. NEJM J WATCH. (2020).
- Zhang Y, Xiao M, Zhang S et al. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med. 382(17), e38 (2020).
- Batal I, Domsic RT, Medsger TA, Bastacky S. Scleroderma renal crisis: A pathology perspective. Int J Rheumatol. (2010).
- Winograd J, Schimmel DH, Palubinskas AJ. The spotted nephrogram of renal scleroderma. AJR Am J Roentgenol. 126(4), 734-738 (1976).
- Zhang W, Zhao Y, Zhang F et al. The use of anti-inflammatory drugs in the treatment of people with severe coronavirus disease 2019 (COVID-19): The Perspectives of clinical immunologists from China. Clin Immunol. 214, (2020).
- Gautret P, Lagier JC, Parola P et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 56(1), (2020).
- Heidary F, Gharebaghi R. Ivermectin: a systematic review from antiviral effects to COVID-19 complementary regimen. The Journal of Antibiotics. 73, 593-602 (2020).
- Kory P, Meduri GU, Varon J, Iglesias J, Marik PE. Review of the emerging evidence demonstrating the efficacy of ivermectin in the prophylaxis and treatment of COVID-19. Am J Ther. 28(3), e299–e318 (2021).