Case Report - Imaging in Medicine (2025) Volume 17, Issue 1
Unveiling the Intersection: Post Traumatic Guyon's Canal Syndrome
- Corresponding Author:
- Zahra SM Husain
Department of Diagnostic Radiology, Dammam Medical Complex, Dammam, Saudi Arabia
E-mail: Zahra.4@live.com
Received date: 22-May-2024, Manuscript No. FMIM-24-141530; Editor assigned: 25-May-2024, PreQC No. FMIM-24-141530 (PQ); Reviewed: 14- June-2024, QC No. FMIM-24-141530; Revised: 11-January-2025, Manuscript No. FMIM-24-141530 (R); Published: 18- January-2025, DOI: 10.47532/1755-5191.2024.17(1).265-268
Abstract
Guyon’s canal syndrome, also known as ulnar tunnel syndrome or handlebar palsy, is an exceedingly rare peripheral ulnar neuropathy. It involves the compression of the distal ulnar nerve at the wrist as it passes through a space called Guyon’s canal. This canal is a triangular fibroosseous tunnel, approximately 1.5 cm long, located at the carpus. The syndrome can result from various causes, including compression due to ganglion cysts, occupational traumatic neuritis, musculotendinous arch issues, and ulnar artery disease. In this case, we describe an instance of post-traumatic Guyon’s canal syndrome secondary to a ruptured ganglion cyst and triquetrum fracture.
Keywords
Guyon’s canal • Ulnar nerve • Trauma • MRI • Ganglion cyst
Introduction
Guyon’s canal syndrome, though uncommon, occurs due to compression of the ulnar nerve as it traverses Guyon’s canal. The wrist is the second most common site for ulnar nerve entrapment, following the elbow. Diagnosis usually relies on clinical examination. However, due to varying clinical presentations, identifying the syndrome can be challenging, especially when sensory symptoms are atypical or absent. Additionally, pinpointing the exact compression site along the nerve course remains difficult based solely on clinical examination or electrophysiology.
Case Presentation
A previously healthy 35-year-old woman visited the orthopedic clinic due to a three-week history of pain and tingling in her right hand’s fourth and fifth fingers, along with the medial palm area. She had a history of falling on an outstretched hand but did not seek medical advice. Despite taking oral analgesics, her symptoms worsened.
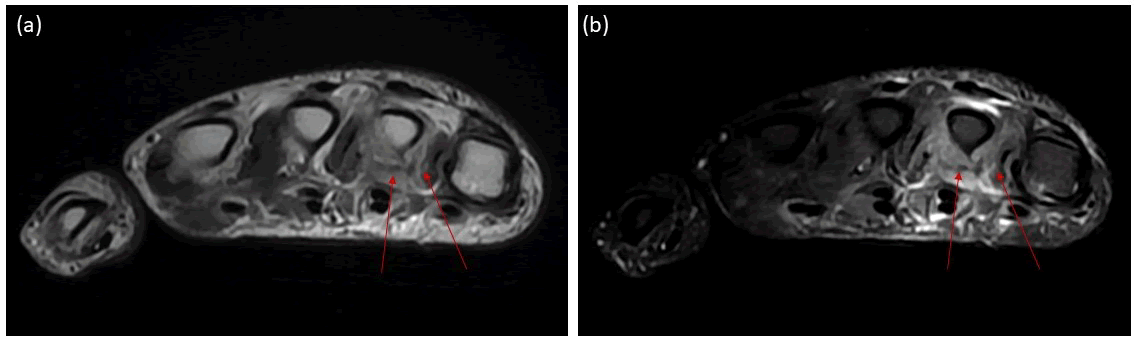
The patient underwent a hand MRI, which revealed denervation edema in the third and fourth lumbrical muscles (Figure 1). Ulnar nerve neuropathy was considered, prompting a wrist MRI to assess Guyon’s canal.
Figure 1. a) Hand MRI, axial T2 and b) T2 fat saturation sequence demonstrate atrophy and edematous signal in the third and fourth lumbrical muscles (arrows).
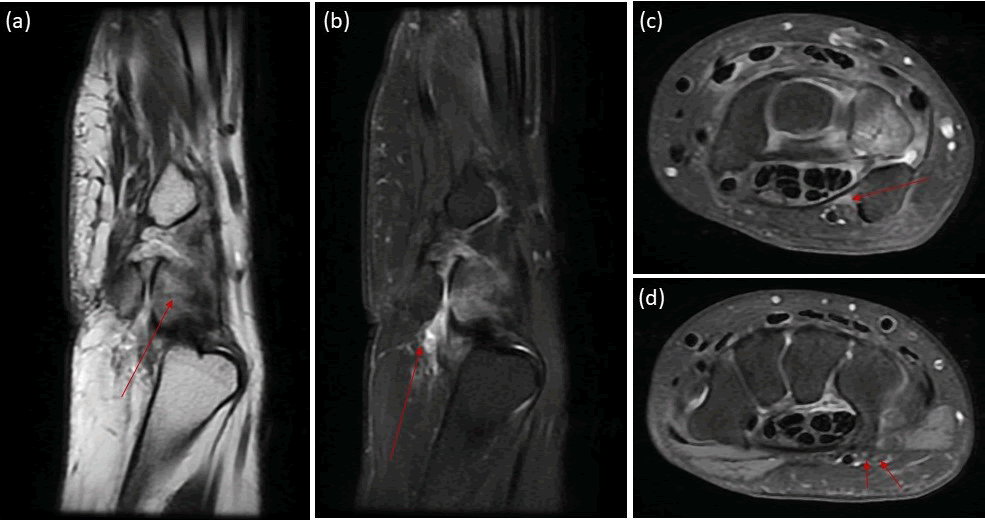
Wrist MRI revealed ruptured pisotriquetral joint ganglion cyst with surrounding free fluid extending to the proximal Guyon’s canal. The latter is compressing the proximal ulnar nerve (Zone I). There is bone marrow edema related to triquetrum with low signal intensity line suggesting fracture (Figure 2).
Figure 2. a) Wrist MRI, sagittal T1; b) sagittal PD fat saturation, c) axial PD fat saturation sequences at the level of proximal and d) distal Guyon’s canal. Triquetrum bone marrow edema with intramedullary low signal intensity line denoting fracture (arrow in (a)). Pisotriquetral ganglion cyst with surrounding free fluid and edematous changes denoting rupture (arrow in (b)). Free fluid noted in the proximal Guyon’s canal (zone I) causing mass effect on the ulnar nerve (arrow in (c)). The superficial and deep branches of the ulnar nerve demonstrate normal thickness and signal intensity (arrows in (d)).
While ganglion cysts and triquetrum fractures are established causes of ulnar nerve compression in Guyon’s canal, our case involves dual etiologies resulting from a traumatic event. Unlike typical Guyon’s canal syndrome, where the ganglion cyst is the primary cause, in our patient, ulnar nerve compression was due to free fluid that leaked from the cyst and extended into Guyon’s canal. Additionally, the triquetrum fracture compounded the trauma, leading to the patient’s symptoms.
Discussion
Guyon’s canal, also referred to as the ulnar-carpal canal, is anatomically defined by the proximal and medial borders formed by the pisiform bone and the lateral and distal borders formed by the hook of the hamate. The canal’s floor includes the transverse carpal ligament, while its roof is formed by the volar carpal ligament [1]. At the distal end of the canal’s floor lies the pisohamate hiatus, bordered superiorly by a concave musculotendinous arch and inferiorly by the pisohamate ligament [1-2].
Within Guyon’s canal, the ulnar artery and the ulnar nerve are situated. The ulnar nerve divides into branches, responsible for sensory innervation of the palmar surface of the little finger and the ulnar side of the index finger, as well as motor innervation of the palmaris brevis muscle. Additionally, the deep branch of the ulnar nerve innervates the hypothenar muscle and then passes through the pisohamate hiatus to supply the deep muscles of the third and fourth lumbricals, the interosseous muscles, the adductor pollicis, and the flexor pollicis brevis [3]. Notably, due to its superficial location, the ulnar nerve in Guyon’s canal is more sensitive to direct external compression than the median nerve within the carpal tunnel. Furthermore, the portion of the transverse carpal ligament covering Guyon’s canal is thinner than the part protecting the carpal tunnel [4].
Compression of the ulnar nerve inside Guyon’s canal can lead to sensorimotor, pure motor, or pure sensory deficits. Shea and McClain classified ulnar nerve lesions in Guyon’s canal into three types based on the anatomical site of compression at the wrist [5]:
• Type I: Involves the ulnar nerve proximal to or within Guyon’s canal. It presents with both motor and sensory abnormalities, including weakness in intrinsic hand muscles innervated by the ulnar nerve. Sensory deficits occur in the hypothenar eminence and the ulnar half of the ring finger, specifically on the palmar surface (not dorsally, which is innervated by the dorsal cutaneous nerve).
• Type II: Compression occurs along the deep branch of the ulnar nerve. This type manifests as weakness in muscles innervated by the deep branch. Depending on the location of compression, some hypothenar muscles may be spared.
• Type III: Compression is distal within the end of Guyon’s canal. Only sensory abnormalities are observed, affecting the palmar ulnar distribution. Notably, there is no motor deficit associated with this rare syndrome.
Shea and McClain recognized 19 distinct lesions responsible for ulnar nerve compression at the wrist and hand. The most common causes are ganglion cysts (28.7%), occupational neuritis (23.5%), lacerations (10.3%), ulnar artery disease (8.1%), and carpal bone fractures (5.9%). Among those lesions, 52% have been categorized as type II, 30% as type I, and 18% as type III. Congenital factors (such as anomalous muscles and accessory ossicles), trauma, rheumatoid arthritis, and mass lesions (both intrinsic and extrinsic) were implicated in ulnar nerve involvement near Guyon’s canal [5]. Georgiev et al., summarized various abductor digiti minimi variants associated with Guyon’s canal syndrome, including absence, origins from forearm fascia, palmaris longus, flexor carpi radialis fascia, intermuscular fascia, three origins, and fusion with the flexor digiti minimi brevis [6].
Diagnosing distal ulnar neuropathy relies on clinical criteria, but electromyography and neurological studies play a crucial role in assessing pain and nerve function. A comprehensive patient history, including work details, hobbies, and lifestyle, is essential. Conditions such as rheumatoid arthritis, scleroderma, and diabetes must be considered. Excluding abnormalities in the cervical spine, shoulder, and elbow is also important [7-9]. The symptoms resemble those of ulnar nerve involvement at the elbow, except for the absence of sensory loss in the dorsum of the hand due to the dorsal cutaneous branch leaving the forearm 5-8 cm proximal to the wrist [10]. Pain, if present, may worsen with tapping over the pisiform (Tinel’s sign) and can radiate up the forearm. The Palmaris brevis sign aids in diagnosis, distinguishing between ulnar nerve compression at the cubital tunnel versus the wrist. When the patient voluntarily abducts the little finger, simultaneous contraction of the Palmaris brevis occurs, absent in cubital tunnel entrapment but usually preserved when the ulnar nerve is compressed at the pisohamate hiatus [11-13].
Radiographs of the hand and wrist, including the carpal canal view, are essential to visualize possible fractures and bone displacement. MRI is recommended for patients with equivocal clinical findings, suspected mass lesions, or persistent symptoms after surgery. Ultrasound is valuable for ruling out space-occupying lesions. When the syndrome results from mechanical repetitive trauma (such as occupation, hobbies, or lifestyle), the approach involves avoiding pressure on the hypothenar eminence. Initial conservative therapy includes immobilization, discontinuing traumatic habits, and local cortisone injections. Surgical decompression may be necessary in refractory cases [14,15].
Surgical intervention is recommended for large lesions that cause pressure. Although small ganglia may not always be detectable through the skin, persistent signs of deep branch ulnar nerve impairment in Guyon’s canal warrant exploration. During surgical exploration, the ulnar nerve and artery can be released within Guyon’s canal. If a ganglion is present, it can be dissected and completely removed. In cases without an obvious mass lesion, constricting bands are divided, and the pisohamate hiatus is unroofed [16-18].
Conclusion
Guyon’s canal syndrome is less common than carpal tunnel syndrome or cubital tunnel syndrome. MRI plays a crucial role in diagnosing patients with symptoms of ulnar nerve compression and identifying the underlying cause before surgery. Dual etiologies can coexist in Guyon’s canal syndrome, necessitating thorough investigation and targeted treatment.
References
- Gross MS, Gelberman RH. The anatomy of the distal ulnar tunnel. Clin Orthop Relat Res. 196, 238-247 (1985).
[Google Scholar] [PubMed]
- Zeiss J, Jakab E, Khimji T et al. The ulnar tunnel at the wrist (Guyon's canal): Normal MR anatomy and variants. Am J Roentgenol. 158, 1081-1085 (1992).
[Crossref] [Google Scholar] [PubMed]
- Depukat P, Mizia E, Kuniewicz M et al. Syndrome of canal of guyon-definition, diagnosis, treatment and complication. Folia Med Cracov. 55, 17-23 (2015).
[Google Scholar] [PubMed]
- Scarborough A, MacFarlane RJ, Mehta N et al. Ulnar tunnel syndrome: Pathoanatomy, clinical features and management. Br J Hosp Med. 81, 1–9 (2020).
[Crossref] [Google Scholar] [PubMed]
- Shea JD, McClain EJ. Ulnar-nerve compression syndromes at and below the wrist. J Bone Joint Surg Am. 51, 1095-1103 (1969).
[Google Scholar] [PubMed]
- Georgiev GP, Jelev L, Surchev L. Undescribed variant muscle–“deep abductor-flexor” of the little finger, in relation to ulnar nerve compression at the wrist. Ann Anat. 189, 276-282 (2007).
[Crossref] [Google Scholar] [PubMed]
- Tottas S, Kougioumtzis I, Titsi Z et al. Ulnar nerve entrapment in Guyon’s canal caused by a ganglion cyst: Two case reports and review of the literature. Eur J Orthop Surg Traumatol. 29, 1565-1574 (2019).
[Crossref] [Google Scholar] [PubMed]
- Wang GH, Mao T, Chen YL et al. An intraneural ganglion cyst of the ulnar nerve at the wrist: A case report and literature review. J Int Med Res. 49, 701 (2021).
[Crossref] [Google Scholar] [PubMed]
- Quang VP, Quoc HH, Nguyen B et al. Guyon’s canal resulting from lipoma: A case report and review of the literature. Int J Surg Case Rep. 95, 107-182 (2022).
[Crossref] [Google Scholar] [PubMed]
- Rohilla S, Yadav R, Dhaulakhandi D. Lipoma of Guyon’s canal causing ulnar neuropathy. J Orthop Traumatol. 10, 101-103 (2009).
[Crossref] [Google Scholar] [PubMed]
- Shturman Sirota I, Olivares Ronces A. An atypical presentation of pacinian corpuscles on bilateral Guyon’s tunnel. Plast Reconstr Surg Glob Open. 6, 1946 (2018).
[Crossref] [Google Scholar] [PubMed]
- Aguiar PH, Bor-Seng-Shu E, Gomes-Pinto F et al. Surgical management of Guyon's canal syndrome, an ulnar nerve entrapment at the wrist: Report of two cases. Arq Neuropsiquiatr. 59, 106-111 (2001).
[Crossref] [Google Scholar] [PubMed]
- Pierre-Jerome C, Moncayo V, Terk MR. The Guyon's canal in perspective: 3-T MRI assessment of the normal anatomy, the anatomical variations and the Guyon's canal syndrome. Surg Radiol Anat. 33, 897-903 (2011).
[Crossref] [Google Scholar] [PubMed]
- Kaiser R, Houstava L, Brzezny R et al. The results of ulnar nerve decompression in Guyon's canal syndrome. Acta Chir Orthop Traumatol Cechoslov. 79, 243-248 (2012).
[Google Scholar] [PubMed]
- Hoogvliet P, Jh Coert, Jan Friden et al. How to treat Guyon's canal syndrome? Results from the European HANDGUIDE study: A multidisciplinary treatment guideline. Br J Sports Med. 47, 1063-1070 (2013).
[Crossref] [Google Scholar] [PubMed]
- Huang CW, Yin CY, Huang HK et al. Influential factors of surgical decompression for ulnar nerve neuropathy in Guyon's canal. J Chin Med Assoc. 84, 885-889 (2021).
[Crossref] [Google Scholar] [PubMed]
- Wang B, Zhao Y, Lu A et al. Ulnar nerve deep branch compression by a ganglion: A review of nine cases. Injury. 45, 1126-1130 (2014).
[Crossref] [Google Scholar] [PubMed]
- Cho YJ, Cho SM, Sheen SH et al. Simple decompression of the ulnar nerve for cubital tunnel syndrome. J Korean Neurosurg Soc. 42, 382-387 (2007).
[Crossref] [Google Scholar] [PubMed]