Case Report - Interventional Cardiology (2022) Volume 14, Issue 1
Transcoronary pacing for transient CHB during PTCA: A novel salvage
- Corresponding Author:
- Akshay A Bafna
Department of Cardiology,
Rajarshi Chhatrapati Shahu Maharaj Government Medical College and CPR Hospital,
Kolhapur,
Maharashtra,
India
E-mail: drbafnaakshay@gmail.com
Received date: 11-Oct-2021, Manuscript No. FMIC-21-44303; Editor assigned: 13-Oct-2021, PreQC No. FMIC-21-44303 (PQ); Reviewed date: 25-Oct-2021, QC No. FMIC-21-44303; Revised date: 28 Oct-2021, Manuscript No. FMIC-21-44303 (R); Published date: 04-Nov-2021, DOI: 10.37532/1755-5310.2022.14(1).432
Abstract
We describe a case of emergency Transcoronary Pacing (TCP) for the management of transient complete heart block during Percutaneous Transluminal Coronary Angioplasty (PTCA). A 60-year-old woman with a past medical history of angioplasty for Left Anterior Descending (LAD) and Right Coronary Artery (RCA) stenosis presented with chest pain and sweating. Her electrocardiography showed NSTEMI (Non-ST Segment Elevation Myocardial Infarction) with ST depression in V5-V6, I and aVL leads. Coronary angiography revealed 80% stenosis at The Left Circumflex Artery (LCX) and 30% In-Stent Restenosis (ISR) in RCA. During PTCA, as the guiding wire advanced to the Left Circumflex Artery (LCX) and the balloon inflated at 8 atm, Complete Heart Block (CHB) developed with a heart rate of 40 beats per minute. The intravenous rescue therapy with atropine was ineffective. An emergency TCP was successfully performed using a guiding wire as a pacing wire. The ventricle rhythm was reversed after 15-20 minutes of TCP initiation, and PTCA was completed uneventfully. We demonstrate that TCP can be a safe and effective technique for emergency management of heart block during PTCA and may be a suitable alternative to transvenous pacing.
Keywords
Angioplasty • Complete Heart Block (CHB) • Guidewire • Left Circumflex Artery (LCX) • PTCA • Transcoronary pacing (TCP) • Transvenous pacing
Introduction
Temporary cardiac pacing is occasionally required to manage bradyarrhythmias during Percutaneous Coronary Intervention (PCI) [1]. Unfortunately, the predictability for cardiac pacing in a patient during the PCI is still poor. Thus, many interventional cardiologists adopt a prophylactic temporary pacemaker placement strategy in highrisk patients [1,2].
Placement of temporary transvenous pacing catheter into the right ventricle is the commonly used approach for pacing during PCI [3].However, the use of temporary transvenous pacing catheters in all PCI patients creates an unnecessary expenditure. It may also be associated with complications like bleeding, disruption of tricuspid apparatus and ventricle perforation [1,4,5]. Moreover, if emergency pacing is required and the transvenous pacemaker is not appropriately placed for prophylaxis use, delay in placement can be detrimental [1].
In 1985, Meier, et al. [6] reported a safe and effective use of coronary guidewire as the pacing wire for temporary cardiac pacing. Nevertheless, this technique is not widely used [1]. We are presenting a case of successfully achieved temporary transcoronary pacing (TCP) for the management of transient Complete Heart Block (CHB) during Percutaneous Transluminal Coronary Angioplasty (PTCA) (Table 1).
| Time | Event |
|---|---|
| 2016: Medical history | History of angioplasty in LAD and right coronary artery |
| 21 Feb 2021: At the time of admission | Patient admitted with chest pain and sweating |
| 21 Feb 2021: At the time of emergency investigations |
|
| 21 Feb 2021: At the time of angioplasty |
|
| 21 Feb 2021: During intervention | Ventricle rhythm reversed after 15-20 minutes of transcoronary pacing initiation and angioplasty completed uneventful |
| 21 Feb 2021: Post intervention | Post-operative electrocardiogram revealed a normal rhythm and clinical improvement |
Abbreviations: LAD: Left Anterior Descending coronary artery; ECG: Electrocardiogram: NSTEMI: Non ST Elevated Myocardial Infarction; LVEF: Left Ventricular Ejection Fraction; CPK-MB: Creatine Phosphokinase-MB; ISR: In-Stent Restenosis; LCX: Left Circumflex Artery; RCA: Right Coronary Artery; CHB: Complete Heart Block; HR: Heart Rate
Table 1: Timeline of events for this case study.
Case Presentation
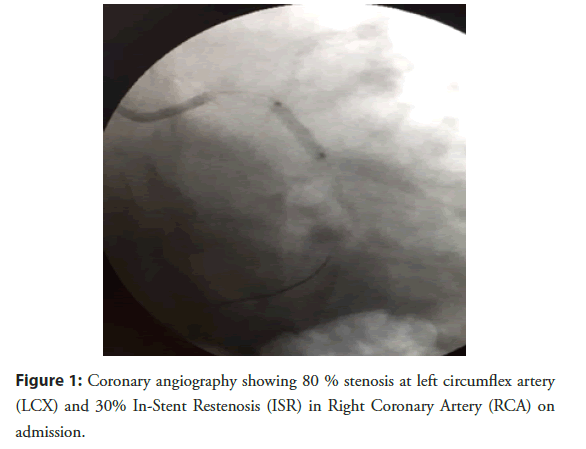
A 65-years-old female was hospitalised with a complaint of chest pain with sweating on Feb 21, 2021 at Rajarshi Chhatrapati Shahu Maharaj Government Medical College, Kolhapur. She had a medical history of the Left Anterior Descending artery (LAD) and Right Coronary Artery (RCA) angioplasty in 2016. Her electrocardiogram showed Non-ST Elevated Myocardial Infarction (NSTEMI) with ST depression in V5-V6, I and aVL leads. The routine blood investigations showed CPK-MB 101 U/L and Troponin-I 1.1 ng/mL. The echocardiography reported Left Ventricular Ejection Fraction (LVEF) 55% with no regional wall motion abnormality. Coronary angiography demonstrated 80% stenosis in the Left Circumflex Artery (LCX) and 30% In-Stent Restenosis (ISR) in RCA. The LAD stent was patent without any stenosis (Figure 1).
Figure 1: Coronary angiography showing 80 % stenosis at left circumflex artery (LCX) and 30% In-Stent Restenosis (ISR) in Right Coronary Artery (RCA) on admission.
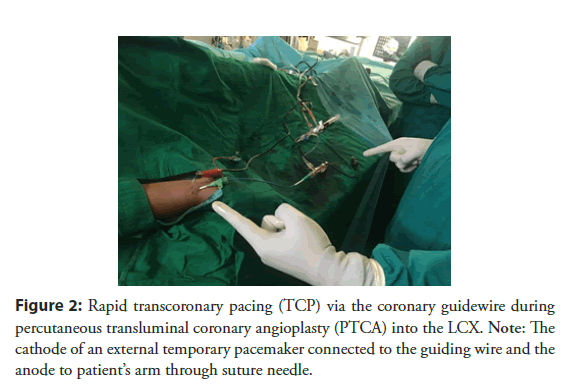
Percutaneous transluminal coronary angioplasty was planned to LCX on Feb 21, 2021. Prior to PTCA, aspirin 300 mg PO, ticagrelor 90 mg PO, atorvastatin 80 mg PO, Unfractionated Heparin (UFH) 6500 units, and cefotaxime 1 gm were administered intravenously. After cannulation for the coronary artery, the occlusion of the LCX was crossed with the use of angioplasty guiding wire (0.014” Fielder FC J tipped PTCA guidewire) and Boston Scientific balloon with predilated size 2.0 × 10 nm. As the guiding wire advanced to LCX and balloon inflated at 8 atm, CHB developed with heart rate of 40 beats per minute. Intravenous atropine 2 cc could not able to recover ventricle rhythm. Transcoronary pacing was performed immediately to manage CHB. The cathode of a temporary external pacemaker (Medtronic, India) was connected to the guiding wire and anode to the patient’s arm through a suture needle (Figure 2).
Figure 2: Rapid transcoronary pacing (TCP) via the coronary guidewire during percutaneous transluminal coronary angioplasty (PTCA) into the LCX. Note: The cathode of an external temporary pacemaker connected to the guiding wire and the anode to patient’s arm through suture needle.
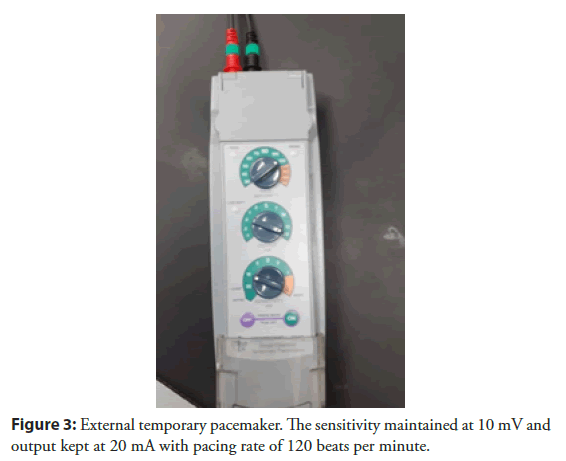
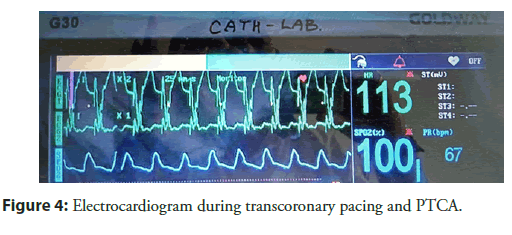
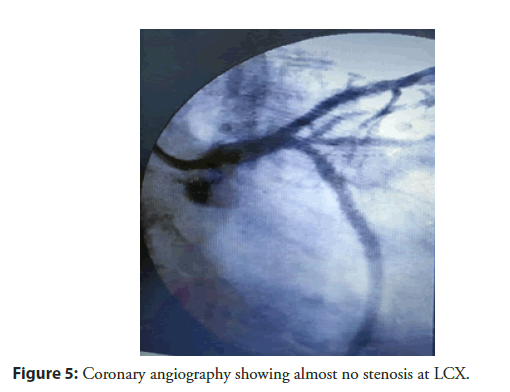
With a pulse of 120 beats per minute, TCP began with pacing threshold (sensitivity) maintained at 10 mV and output at 20 mA (Figures 3 and 4). Angioplasty was completed, and ventricle rhythm was revived after 15-20 minutes. The LCX stenosis was reduced from 80-90 to 0 percent on the visual estimate (Figure 5). The coronary artery segment was found normal after removal of the catheter. The angioplasty was completed successfully, and the further course was uneventful. A post-operative electrocardiogram revealed a normal rhythm and clinical improvement was observed. All the Timeline of events for this case study are mentioned in Table 1.
Figure 5: Coronary angiography showing almost no stenosis at LCX.
Results and Discussion
We presented a case of TCP, which successfully managed transient complete heart block during PTCA.
Meier, et al. [6] are the first to demonstrate the emergency use of coronary angioplasty guidewire as a pacing wire during PTCA. A subsequent report on 300 patients supported the feasibility of this technique [7]. Although this technique has been demonstrated long time back in 1985, still it has limited application. This may be perhaps due to the infrequent need for temporary cardiac pacing during PCI. The commonly used technique utilizes a transvenous pacemaker associated with complications like bleeding at the vascular site, ventricle perforation, and others. The concomitant use of anticoagulants during transvenous pacemaker and PTCA may increase the risk of bleeding is well reported.
Mixon and co-workers, reported use of temporary coronary guidewire pacing during PCI in 26 patients [1].They suggested using a subcutaneously placed metal suture to connect to the pacemaker’s anode end instead of a long cutaneous electrode. This subcutaneously placed metal suture reduces the resistance during cardiac pacing. In our case, we placed a suture needle near arterial, subcutaneous tissue and connected it to the anode end of the pacemaker.
Further, the guidewire tip shall be located distally or dip in the myocardium for effective pacing. In our case, the guide wire tip was placed at circumflex, which lies at atrioventricular grooves and is suitable for effective transcoronary pacing. Serna, et al. reported 3% failure rate of temporary coronary guidewire pacing during PCI in 300 patients study [7]. This failure was demonstrated due to pacing attempted at the infarcted area. The pacing location thus plays a critical in the success of temporary coronary guidewire pacing. In our case, the placement of the guidewire tip in the noninfarcted area of the circumflex tip is responsible for successful and uneventful pacing. Using guidewire, temporary transcoronary pacing during PTCA is feasible, safe, and effective and may provide a suitable alternative to transvenous pacing.
The bradycardia and conduction defects during coronary angioplasty are rare and known to occur in about 2 percent of patients [8].
Conclusion
In the present case, the risk of heart block seemed negligible, and heart block was not reversed with pharmacological management. The TCP system was kept readily available to manage any unforeseeable complications during angioplasty. The emergency use of TCP was safe and effective in this case. Transcoronary pacing can be used in an emergency to manage transient complete heart block during PTCA.
Acknowledgement
Nil
Consent
Patient’s consent was obtained to publish clinical information and images.
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- Mixon TA, Cross DS, Lawrence ME, et al. Temporary coronary guidewire pacing during percutaneous coronary intervention. Catheter Cardiovasc Interv. 61(4): 494-500 (2004).
[CrossRef] [Google scholar] [PubMed]
- Harvey JR, Wyman RM, McKay RG, et al. Use of balloon flotation pacing catheters for prophylactic temporary pacing during diagnostic and therapeutic catheterization procedures. Am J Cardiol. 62(13): 941-4 (1988).
[CrossRef] [Google scholar] [PubMed]
- Weinstein J, Gnoj J, Mazzara JT, et al. Temporary transvenous pacing via the percutaneous femoral vein approach: A prospective study of 100 cases. Am Heart J. 85(5): 695-705 (1973).
[CrossRef] [Google scholar] [PubMed]
- Mandak JS, Blankenship JC, Gardner LH, et al. Modifiable risk factors for vascular access site complications in the IMPACT II trial of angioplasty with versus without eptifibatide. Integrilin to minimize platelet aggregation and coronary thrombosis. J Am Coll Cardiol. 31(7): 1518-24 (1998).
[CrossRef] [Google scholar] [PubMed]
- Blankenship JC, Hellkamp AS, Aguirre FV, et al. Vascular access site complications after percutaneous coronary intervention with abciximab in the Evaluation of c7E3 for the Prevention of Ischemic Complications (EPIC) trial. Am J Cardiol. 81(1): 36-40 (1998).
[CrossRef] [Google scholar] [PubMed]
- Meier BE, Rutishauser WI. Coronary pacing during percutaneous transluminal coronary angioplasty. Circulation. 71(3): 557-61 (1985).
[CrossRef] [Google scholar] [PubMed]
- de La Serna F, Meier B, Pande AK, et al. Coronary and left ventricular pacing as standby in invasive cardiology. Cathet Cardiovasc Diagn. 25(4): 285-9 (1992).
[CrossRef] [Google scholar] [PubMed]
- Dorros G, Cowley MJ, Simpson J, et al. Percutaneous transluminal coronary angioplasty: Report of complications from the National Heart, Lung and Blood Institute PTCA Registry. Circulation. 67(4): 723-30 (1983).
[CrossRef] [Google scholar] [PubMed]