Research Article - Interventional Cardiology (2018) Volume 10, Issue 5
The Role of the Retrograde Approach in Percutaneous Coronary Interventions for Chronic Total Occlusions : Insights from the Japanese Retrograde Summit Registry
- Corresponding Author:
- Makoto Sekiguchi
Department of Cardiology, Fukaya Red Cross Hospital, Fukaya, Japan
Tel: +81(0)48-571-1511
Fax: +81(0)48-573-5351 E-mail: makoto-s@qj8.so-net.ne.jp
Received date: August 14, 2018 Accepted date: September 04, 2018 Published date: September 11, 2018
Abstract
Background: Percutaneous coronary intervention for chronic total occlusion (CTO-PCI) success rates have increased with adoption of the retrograde approach. We evaluated the role of the retrograde approach in CTO-PCI from the analysis of the Japanese Retrograde Summit Registry. Methods and Findings: We analysed 3,229 consecutive PCIs in 56 Japanese centres and included in this registry in January 2012–December 2013. We analysed background characteristics and procedure outcomes of the following groups: A, succeeded using only the antegrade approach; R, succeeded using the retrograde approach; RA, succeeded using the antegrade approach after failure of the retrograde approach; F, failed. Success in initial approach was obtained in 2,854 procedures (88.4%). Procedure numbers and rates in each group were: A, n=2,016 (62.4%); R, n=658 (20.4%); RA, n=180, 5.6%); Group F, n=375 (11.6%). J-CTO scores were 1.24 ± 0.95, 2.16±1.06, 1.69±1.04, and 2.00±1.07, respectively (p<0.0001). Average procedure time was >180 minutes and average air kerma >5 Gy. Overall in-hospital MACCE rate was 0.53%, and was high in Groups R and F (P<0.0001). Conclusions: Procedure success was achieved using only the antegrade approach in many cases. The retrograde approach succeeded even in difficult CTO-PCI cases. Limitations included large amounts of contrast agent, high-dose fluoroscopy, and high complication rate. Therefore, further developments are still required.
Abbreviations
CABG: Coronary Artery Bypass Grafting, CART: Controlled Antegrade And Retrograde Subintimal Tracking, CC grade: Collateral Channel Filling Grade, CTO: Chronic Total Occlusion, CTO-PCI: Percutaneous Coronary Intervention for Chronic Total Occlusion, GW: Guidewire, IVUS: Intravascular Ultrasound, LCX: Left Circumflex Artery, MACCE: Major Adverse Cardiovascular and Cerebrovascular Events, PCI: Percutaneous Coronary Intervention, STAR: Subintimal Tracking and Re-Entry
Introduction
There has been a great deal of progress in the development of new devices to perform percutaneous coronary intervention for chronic total occlusion (CTO-PCI), such as specialized guidewires, microcatheters, and re-entry devices, as well as treatment techniques, such as the parallel wire technique, intravascular ultrasound (IVUS)-guided wiring, and subintimal tracking and re-entry (STAR). However, favourable outcomes have only been obtained in some centres and by some operators [1-4].
The success rate of CTO-PCI with the conventional antegrade approach is generally about 70% [5-7], with the main reason for failure being inability of the guidewire to reach the distal coronary artery. Recently, the success rate of CTO-PCI has increased with the development and widespread adoption of the retrograde approach and controlled antegrade and retrograde subintimal tracking (CART) technique proposed by Kato et al. [8,9]. The Japanese Retrograde Summit Group implemented a registry for CTO cases, in which PCI was performed with a retrograde approach in many centres in Japan from 2009, and reported the usefulness and safety of this approach [10,11]. In many CTO lesions, however, high success rates can be expected only with the antegrade approach [12]. These reports discussed CTO cases treated only with the retrograde approach and did not evaluate the requirement, efficacy, or safety of a retrograde approach in total CTO-PCI. The Japanese Retrograde Summit Group increased the number of centres to be included, and registered all CTO-PCI cases regardless of the antegrade or retrograde approach. We analysed the role of application of the retrograde approach in recent actual clinical practice of CTO-PCI.
Methods
Study population and study protocol
We registered all cases of CTO-PCI performed between January 2012 and December 2013 at 56 centres approved to participate in the registry. The presences of related symptoms and/or ischemia at the territory of CTO were taken as indications for PCI, and cases in which it was impossible to take an antiplatelet agent were excluded. All patients at each centre provided informed consent for inclusion in the registry.
Aspirin and thienopyridine as antiplatelet agents were administered preoperatively in all cases. The dosage of heparin calculated based on body weight was administered during the operation, with additional administration to maintain activated clotting time >300 s. Coronary angiography on both sides was performed simultaneously at the beginning of the procedure, and PCI difficulty level expected from the morphology of the CTO lesion was evaluated based on the J-CTO score [12]. We determined the score regarding the morphology at CTO entry, presence of calcification, presence of bending (≥45°) within the occlusion, longer lesion (≥20 mm), and previous attempt, and lesions were categorized as easy (0), intermediate (1), difficult (2), or very difficult (≥3).
All procedures, including the initial use of the antegrade or retrograde approach and changes in approach during the procedure, were decided by each centre and at the operator’s discretion. Drug-eluting stent placement was applied as the standard treatment after successful guidewire crossing unless contraindicated.
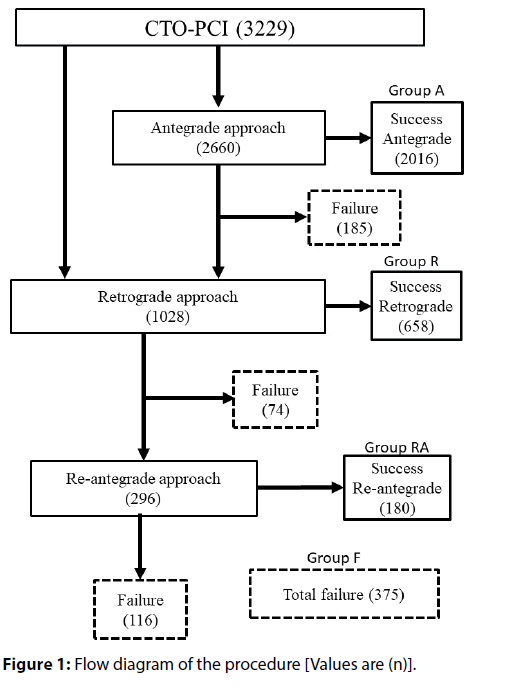
Cases were classified into groups according to the procedure outcome as follows: Group A, succeeded using the antegrade approach; Group R, succeeded using retrograde approach; Group RA, succeeded using the antegrade approach after failure of the retrograde approach; Group F, failed.
A procedure was deemed as implementing the retrograde approach when an attempt was made for the guidewire to cross a collateral channel. Patients and lesion characteristics, J-CTO score, assessment of collaterals, occurrence of in-hospital complications, procedure time, and amounts of contrast agent used, and fluoroscopy dose were compared between groups.
Definitions
CTO was defined as TIMI flow grade 0 and occlusion period >3 months as determined from patient symptoms, changes in anginal symptoms, history of myocardial infarction, or prior coronary angiography. Major collateral channel injury was defined as perforation and rupture requiring tissue or coil embolization or surgical treatment. Major adverse cardiac and cerebrovascular events (MACCE) were defined as death during hospitalization, Q-wave myocardial infarction, stroke, emergency CABG, and revascularization of target vessels. Continuous changes on the electrocardiogram, increasing by >3× the CK-MB value, were defined as myocardial infarction, and Q-wave myocardial infarction or non-Q-wave myocardial infarction were distinguished by the presence of absence of Q-wave, respectively. Measurement of CK-MB after the procedure was not required in cases with no further symptoms or changes in neither the electrocardiogram nor in haemodynamic status. The success of treatment was defined as blood flow with TIMI grade 3 on the target vessel and <50% residual stenosis.
Data collection
Joining of the registry in centres was performed on a voluntary basis, but the entry of all CTO-PCI performed during the period of the registration was required. Data was entered from each centre through the internet and we collected basic patient information, lesion characteristics, basic procedure information, detailed information for antegrade and a retrograde approach and also in-hospital events.
Statistical analysis
Continuous variables are expressed as the means ± Research Article Sekiguchi M, Muramatsu T, Kashima Y, et al. standard deviation, while categorical variables are expressed as frequencies. Student’s t test or the nonparametric Mann–Whitney U test was used for numerical comparisons between groups. The chi-square or Fisher’s exact test was used to compare categorical variables expressed as frequencies. To evaluate the influence of clinical, angiographic, and procedural variables on retrograde procedural success, odds ratios were estimated using univariate and multivariate logistic regression.
Results
A total of 3,229 consecutive PCIs were registered in a period of 24 months. Of these, 2,660 PCIs (82.4%) were started from an antegrade approach and 2,016 PCIs (75.8%) were successful (Group A). A total of 459 of 644 PCIs in which the antegrade approach failed were changed to a retrograde approach. The retrograde approach was performed in 1,028 PCIs (31.8%), including 569 PCIs where a retrograde approach was selected from the beginning of the procedure, and 658 PCIs (64.0%) were successful (Group R). The antegrade approach was used again in 296 of 370 PCIs in which the retrograde approach failed, and 180 of these PCIs (60.8%) were successful (Group RA). Group F consisted of 375 PCIs that ended in failure. A total of 2,854 PCI s (88.4%) were successful overall (Figure 1).
With regard to patient characteristics, the rate of a history of myocardial infarction was high in Group R. The rate of a history of CABG was low in Group A and high in Group F. The rate of a history of PCI was high in Group R and Group F. The rates of impaired kidney function (eGFR<30) and haemodialysis to end-stage renal failure were high in Group F. The rate of lower left cardiac function (LVEF<35%) was high in Group R and Group F (Table 1).
| Group A (n = 2016) |
Group R (n = 658) |
Group RA (n = 180) |
Group F (n = 373) |
p value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Male | 1666 | (82.8) | 582 | (88.7) | 140 | (78.2) | 300(80.0) | 0.0001 | |
| Age (years) | 67.9 ± 10.6 | 66.6 ± 10.1 | 68.4 ± 9.9 | 68.6 ± 9.9 | 0.0087 | ||||
| Previous MI | 733 | (37.7) | 285 | (44.6) | 63 | (57.3) | 163 | (45.0) | 0.0022 |
| Previous PCI | 115o | (57.7) | 444 | (68.1) | 103 | (57.5) | 250 | (67.0) | < 0.0001 |
| Previous CABG | 111 | (5.6) | 87 | (13.5) | 21 | (11.9) | 55 | (14.9) | < 0.0001 |
| Multi-vessel disease | 1221 | (61.2) | 388 | (60.2) | 103 | (57.5) | 254 | (68.5) | 0.0251 |
| Diabetes mellitus | 877 | (44.3) | 300 | (46.4) | 81 | (45.8) | 151 | (41.5) | 0.4826 |
| Hypertension | 1587 | (79.6) | 511 | (78.9) | 136 | (76.0) | 316 | (85.2) | 0.0336 |
| Hyperlipidemia | 1374 | (69.0) | 279 | (74.3) | 131 | (73.2) | 258 | (69.8) | 0.0666 |
| Smoking | 858 | (46.4) | 337 | (54.9) | 63 | (39.1) | 162 | (46.0) | 0.0002 |
| Family history of CAD | 263 | (17.5) | 86 | (17.9) | 27 | (20.6) | 42 | (16.0) | 0.7252 |
| Hemodialysis | 130 | (6.4) | 30 | (4.6) | 6 | (3.3) | 48 | (12.8) | < 0.0001 |
| eGFR < 30 | 9.6 | (9.6) | 7.9 | (7.9) | 8.7 | (8.7) | 15.4 | (15.4) | 0.0012 |
| EF < 35% | 173 | (9.1) | 81 | (12.8) | 11 | (6.4) | 46 | (13.0) | 0.0046 |
| Target vessel | |||||||||
| RCA | 819 | (40.6) | 428 | (65.0) | 100 | (55.6) | 198 | (52.8) | < 0.0001 |
| LAD | 678 | (33.6) | 170 | (25.8) | 58 | (32.2) | 89 | (23.7) | |
| LCx | 518 | (25.7) | 56 | (8.5) | 21 | (11.7) | 87 | (23.2) | |
| LMCA | 1 | (0.0) | 4 | (0.6) | 1 | (0.6) | 1 | (0.3) | |
| Reference diameter < 3.0 mm | 849 | (44.4) | 164 | (26.1) | 59 | (34.1) | 137 | (39.5) | < 0.0001 |
| Occlusion period < 1 year | 170 | (8.4) | 42 | (6.4) | 17 | (9.4) | 17 | (4.5) | 0.2362 |
| ISR-CTO | 354 | (18.0) | 54 | (8.5) | 14 | (8.0) | 44 | (12.1) | < 0.0001 |
| J-CTO score variables | |||||||||
| Entry shape – Blunt | 872 | (43.9) | 449 | (69.4) | 112 | (62.9) | 250 | (68.3) | < 0.0001 |
| Calcification | 572 | (28.7) | 306 | (46.9) | 64 | (35.6) | 201 | (55.2) | < 0.0001 |
| Bending ≥ 45° | 98 | (4.9) | 89 | (13.5) | 15 | (8.4) | 57 | (16.5) | < 0.0001 |
| Length ≥ 20 mm | 857 | (50.9) | 434 | (76.1) | 93 | (65.5) | 181 | (66.5) | < 0.0001 |
| Re-try lesion | 103 | (5.2) | 144 | (22.2) | 21 | (11.8) | 57 | (15.5) | < 0.0001 |
| J-CTO score | 1.24 ± 0.95 | 2.16 ± 1.06 | 1.69 ± 1.04 | 2.00 ± 1.07 | < 0.0001 | ||||
| J-CTO score category | |||||||||
| easy (0) | 472 | (23.4) | 33 | (5.0) | 21 | (11.7) | 24 | (6.4) | < 0.0001 |
| intermediate (1) | 805 | (39.9) | 141 | (21.4) | 57 | (31.7) | 107 | (28.5) | |
| difficult (2) | 547 | (27.1) | 242 | (36.8) | 68 | (37.8) | 123 | (32.8) | |
| very difficult (≥3) | 192 | (9.5) | 242 | (36.8) | 34 | (18.9) | 121 | (32.3) | |
Values are n (%) or mean + SD CABG = Coronary artery bypass grafting, CAD = Coronary artery disease, EF = Ejection fraction, MI = Myocardial infarction, PCI = Percutaneous coronary intervention, ISR = In-stent restenosis, J-CTO = Multicenter CTO Registry of Japan, LAD = Left anterior descending coronary artery, LCX = Left circumflex artery, LMCA = Left main coronary artery, RCA = Right coronary artery
Table 1. Patient characteristics and Lesion characteristics
With regard to lesion characteristics, the rate of diseased vessels in the left circumflex artery (LCX) was low in Group R and Group RA. With regard to each parameter of J-CTO score, the rates of long lesion ≥20 mm, blunt type occlusion morphology, lesion calcification, and lesion bending were low in Group A and that of re-attempted lesion was high in Group R and Group F (Table 1).
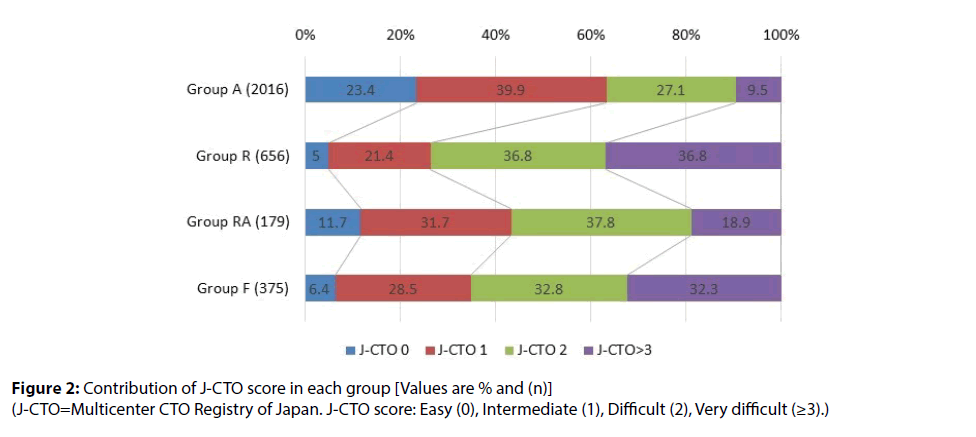
Based on the J-CTO score, there was many Easy (0) and Intermediate (1) cases in Group A, accounting for more than 60% of the total. On the other hand, the rate of Easy (0) and Intermediate in J-CTO was low in Group R and Group F, and the rate of Difficult (2) and Very difficult (≥3) was >60%. The rate of Very difficult (≥3) in Group RA was lower than those in Group R and Group F (Table 1 and Figures 2).
Procedure time was less than 120 minutes in Group A but ≥180 minutes in the other three groups. Fluoroscopy time was also <50 minutes in Group A, but almost 100 minutes in the other groups. Air kerma was low in Group A. The rate of in-hospital MACCE was significantly high in Group R and Group F. There were more cases of emergent CABG in Group F. Cardiac tamponade and collateral channel injury rates were high in Group RA and Group F (Table 2).
| Group A (n = 2016) |
Group R (n = 658) |
Group RA (n = 180) |
Group F (n = 373) |
p value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Procedure related variables | |||||||||
| - Number of GW used for CTO approach | 2.4 ± 1.4 | 5.1 ± 2.9 | 4.8 ± 2.3 | 5.2 ± 2.7 | < 0.0001 | ||||
| - Stent deployment | 1798 | (95.6) | 635 | (99.8) | 173 | (99.4) | 10 | (2.7) | < 0.0001 |
| - Total stent length, (mm) | 47.7 ± 23.9 | 68.6 ± 27.2 | 59.4 ± 25.5 | 32.2 ± 22.9 | < 0.0001 | ||||
| - Procedure time, (min) | 113.7 ± 61.0 | 211.0 ± 3.1 | 211.5 ± 5.8 | 191.1 ± 4.4 | < 0.0001 | ||||
| - Contrast dose, (ml) | 205.8 ± 91.2 | 262.3 ± 111.2 | 292.9 ± 118.9 | 248.3 ± 122.8 | < 0.0001 | ||||
| - Fluoroscopic time, (min) | 49.0 ± 31.4 | 99.8 ± 50.0 | 97.8 ± 40.8 | 92.7 ± 49.8 | < 0.0001 | ||||
| - Air Kerma, (mGy) | 3872.4 ± 97.9 | 6233.9 ±168.5 | 7025.3 ± 329.7 | 6151.4 ± 225.0 | < 0.0001 | ||||
| MACCE | 2 | (0.1) | 7 | (1.1) | 0 | (0.0) | 6 | (1.6) | < 0.0001 |
| - Cardiac death | 1 | (0.0) | 1 | (0.2) | 0 | (0.0) | 2 | (0.5) | 0.1003 |
| - Non cardiac death | 1 | (0.0) | 1 | (0.2) | 0 | (0.0) | 0 | (0.0) | 0.7398 |
| - QMI | 0 | (0.0) | 1 | (0.2) | 0 | (0.0) | 1 | (0.4) | 0.1901 |
| - Non QMI | 0 | (0.0) | 2 | (0.3) | 0 | (0.0) | 0 | (0.0) | 0.0499 |
| - Stroke / non- bleeding | 0 | (0.0) | 2 | (0.3) | 0 | (0.0) | 1 | (0.3) | 0.0929 |
| - CABG | 0 | (0.0) | 0 | (0.0) | 0 | (0.0) | 2 | (0.5) | 0.0016 |
| Other procedural adverse event | |||||||||
| - Transient cerebral ischemia attack | 1 | (0.0) | 0 | (0.0) | 0 | (0.0) | 1 | (0.3) | 0.3753 |
| - Contrast induced nephropathy | 2 | (0.1) | 2 | (0.3) | 0 | (0.0) | 0 | (0.0) | 0.4394 |
| - Coronary perforation | 12 | (0.6) | 37 | (5.6) | 11 | (6.1) | 38 | (10.1) | < 0.0001 |
| - Cardiac tamponade | 2 | (0.1) | 3 | (0.5) | 3 | (1.7) | 3 | (0.8) | 0.0015 |
| - Stent thrombosis | 3 | (0.1) | 2 | (0.3) | 1 | (0.6) | 1 | (0.5) | 0.6459 |
| Retrograde approach related adverse event | |||||||||
| - Donor artery trouble | 0 | (0.0) | 0 | (0.0) | 2 | (0.3) | 0.0016 | ||
| - Collateral channel injury | 48 | (7.3) | 21 | (11.7) | 28 | (7.5) | < 0.0001 | ||
| - Treatment required channel injury | 15 | (2.3) | 7 | (3.9) | 14 | (3.7) | < 0.0001 | ||
Values are n (%) or mean + SD CABG = Coronary artery bypass grafting, CTO = Chronic total occlusion, GW = Guidewire, J-CTO = Multicenter CTO Registry of Japan, MACCE = Major adverse cardiovascular and cerebrovascular events, MI = Myocardial infarction
Table 2. Procedural outcomes
Discussion
This was a retrospective, multi-centre observational study to evaluate the role of the retrograde approach in CTO-PCI. Table 3 summarizes our previous reports and recent multicentre registry reports. Galassi et al [13] reported that the relative number of retrograde procedures increased over time, reaching 25.1% of all CTOs in 2012. Kampaliotis et al. [14] reported that the extensive experience of the participating operators and the hybrid algorithm of PCI for CTO [15] increased utilization of the retrograde approach. The overall procedure success rate was 88.4%, indicating a generally favourable outcome. The retrograde approach related findings were similar to recent multi-centre registries.
| Yamane et al [10] (n = 378) |
Tsuchikane et al [11] (n = 801) |
Kampaliotis et al [14] (n = 1301) |
Galassi et al [13] (n= 9589) |
Present study (n = 3229) |
|
|---|---|---|---|---|---|
| Enrolled Period, year | 2009 | 2009 - 2010 | 2012 - 2015 | 2008 - 2012 | 2012 - 2013 |
| Retrograde procudure, % (n) | 100% (378) | 100% (801) | 41.4% (539) | 16.5% (1582) | 31.8% (1028) |
| Successful Collateral Channel Crossing by GW, % | 81.7% | 82.3% | 75.2% | Unknown | 77.0% |
| Retrograde Procedural Success, % | 70.4% | 71.2% | 62.3% | Unknown | 64.0% |
| Switch to Antegrade after Retrograde Failure, % (n) | 76.8% (86/112) | 77.1% (178/231) | Unknown | Unknown | 80.8% (296/370) |
| Antegrade Success After Retrograde Failure, % (n) | 58.1% (50/86) | 61.2% (109/178) | Unknown | Unknown | 60.8% (180/296) |
| MACE in Retrograde Procedures, % | 0.5% | 1.6% | 4.3% | 0.8% | 1.1% |
| Overall Procedural Success, % | 83.6% | 84.8% | 88.6% | 75.3% | 88.4% |
GW = guidewire, PCI= percutaneous coronary intervention, MACE = major adverse cardiovascular event *Only retrograde procedures were enrolled
Table 3. Previous reports of Japanese Retrograde Summit Group and latest multicenter registry
Although, the retrograde approach has been widely adopted; the antegrade approach was used at the beginning of the procedure in almost all cases and the procedure was successful in >75% of PCIs (Group A). More than half of the cases in Group A were classified as Easy (0) or Intermediate (1) based on the J-CTO score. These cases showed high procedure success rates with only the antegrade approach.
The J-CTO score of Group R was high, and 70% of cases were classified as difficult (2) or very difficult (≥3). Tsuchikane et al. also reported that the procedure success rate was high, even in cases with failure-related lesion characteristics, such as long occlusion (≥20 mm), lesion bending, and blunt morphology of occlusion entry [11]. We suggest that the retrograde approach procedure led many cases with higher J-CTO scores to successful CTO-PCIs. However, the success rate of the procedure with the retrograde approach was only 64% in this registry. The retrograde approach cannot be performed if the retrograde guidewire cannot cross the collateral channels. The success rate of collateral channel crossing with guidewires was 77.0% in this registry (Table 3). Therefore, whether the collateral channels can be crossed by the retrograde guidewire has a marked effect on the success rate of the procedure with the retrograde approach. It is interesting to note that the rate of CTO in the LCX was significantly low in Group R. Anatomically, septal collateral channels are not developed for occlusion in the LCX, and the retrograde route is confined to epicardial collateral channels. This may lead to not selecting a retrograde approach or difficulty in collateral channel crossing with a guidewire. Christopulos et al. also reported Circumflex CTO was a predictor of procedural failure in recent CTO-PCIs [16].
The retrograde approach cannot always be performed in all cases depending on the conditions, such as developed collateral channels. The procedural success rates of the antegrade approach after failure of the retrograde approach were not enough in recent multicentre registries including this registry (Table 3). To further improve the overall procedural success rate, it is important to achieve success with an antegrade approach in cases where a retrograde approach is difficult. For CTO treatment, it is necessary for the operator to learn advanced techniques [17], such as IVUS-guided wiring [18]. Use of a BridgePoint device is necessary, although it was approved in Japan for this study period. However, many problems remain to be resolved in that the BridgePoint device is influenced by the distal coronary artery morphology and long-term outcome are not still clear [19].
With regard to Group R, many patients had complex backgrounds, such as a history of PCI, history of CABG, multi-vessel disease, impairment of kidney function, and low left cardiac function, and J-CTO score was also high. However, about 35% of cases were classified as Easy (0) and Intermediate (1), and we feel that current assessment based on the CTO characteristics has limitations. New indicators, including assessment of “interventional” collateral channels required for the retrograde approach and morphology of the distal cap of the occlusion required for the antegrade approach, are necessary.
Complications caused by non-Q wave myocardial infarction (N-QMI) may be underestimated as a blood exam is not mandatory after a procedure in this registry, but the total rate of in-hospital MACCE was <1%. Therefore, the outcome seems to have been favourable. Lee et al reported similar initial results and complications of the retrograde approach [20]. The MACCE occurrence rate was high in Group R and Group F. The occurrence rates of coronary perforation, cardiac tamponade, and donor artery problems were significantly high in Group RA and Group F, and it was likely that the procedure was complicated and many cases had complex lesion characteristics. One issue caused by these complications is ceasing the retrograde approach and failure of the procedure. The retrograde approach is potentially useful for success even in complex CTO-PCI, but its indications must be considered carefully. Procedure time, fluoroscopy time, air kerma, and amounts of contrast agent were high in all except Group A. Especially, air kerma was >6 Gy on average, and there are concerns regarding radiation-induced skin injury [21]. It is assumed that combined use of the complex retrograde approach was responsible for this result except in Group A. It is necessary to decrease the fluoroscopy frame rate and restrict cineangiography as well as reducing the amounts of contrast agent used and air kerma by shortening the procedure time. Recently, the relationship between stress and atrial arrythmia was reported [22]. With regard to the treatment of coronary artery disease, post operational atrial arrythmia of the catheter-based procedure should be assessed to be compared with openchest cardiac surgery. Unfortunately, post operational atrial arrythmia has not been investigated in this study.
Limitations
This study had some limitations. This was a retrospective, multi-centre observational study. Therefore, the treatment policy was decided by each centre and operator, regardless of operator experience. This study is not analysed in the core laboratory. Only initial outcomes were covered through procedure success and in-hospital complications. Mid- and long-term outcomes after treatment have not been investigated.
Conclusions
The retrograde approach was used for cases with higher J-CTO scores. The retrograde approach procedures showed good initial results, despite application in more difficult CTO-PCI. However, limitations included large amounts of contrast agent, high-dose fluoroscopy, and high complication rate. Therefore, further developments are still required.
Funding
Japanese Retrograde Summit Registry was founded by Boston Scientific Japan and Asahi Intecc.
Conflict of interest
Etsuo Tsuchikane is a consultant for Abbott Vascular Japan, Boston Scientific Japan, and Asahi Intecc. Toshiya Muramatsu received speaking honoraria from Abbott Vascular, Boston Scientific Japan, Medtronic, and Terumo. Masahisa Yamane received speaking honoraria from Abbott Vascular, Asahi Intecc, Boston Scientific Japan, and Medtronic. The other authors have no conflicts of interest to declare.
References
- Horisaki T, Surmely JF, Suzuki T. Contact wire technique: a possible strategy for parallel wire technique. J Invasive Cardiol. 19: E263-264 (2007).
- Ito S, Suzuki T, Ito T, et al. Novel technique using intravascular ultrasound guide wire cross in coronary intervention for uncrossable chronic total occlusions. Circ J. 68: 1088-1092 (2004).
- Matsubara T, Murata A, Kanyama H, et al. IVUS-guided wiring technique: promising approach for the chronic total occlusion. Catheter Cardiovasc Interv. 61: 381-386 (2006).
- Colombo A, Mikhail GW, Michev I et al. Treating chronic occlusions using subintimal tracking and re-entry: the STAR technique. Catheter Cardiovasc Interv. 64: 407-411 (2005).
- Seuro JA, Marso SP, Jones PG, et al. Procedural outcomes and long-term survival among patients undergoing percutaneous coronary intervention of a chronic total occlusion in native coronary arteries: a 20-year experience. J Am Coll Cardiol. 38: 409-414 (2001).
- George S, Cockburn J, Clayton TC, et al. on behalf of the British Cardiovascular Intervention Society and the National Institute for Cardiovascular Outcome Research. Long-term follow-up of elective chronic total coronary occlusion angioplasty. Analysis from the U.K. central cardiac adult database. J Am Coll Cardiol. 64: 235-243 (2014).
- Namazi MH, Serati AR, Vakili H, et al. A Novel Risk Score in Predicting Failure or Success for Antegrade Approach to Percutaneous Coronary Intervention of Chronic Total Occlusion: Antegrade CTO Score. Int J Angiol. 26: 89-94 (2017).
- Surmely JF, Tsuchikane E, Katoh O, et al. New concept for CTO recanalization using controlled antegrade and retrograde subintimal tracking: the CART technique. J Invasive Cardiol. 18: 334-338 (2006).
- Tsuchikane E, Katoh O, Kimura M, et al. The first clinical experience with a novel catheter for collateral channel tracking in retrograde approach for chronic coronary total occlusions. J Am Coll Cardiol Intv. 3: 165-171 (2010).
- Yamane M, Muto M, Matsubara T, et al. Contemporary retrograde approach for the recanalization of coronary chronic total occlusion: on behalf of the Japanese retrograde summit group. EuroIntervention. 9: 102-109 (2013).
- Tsuchikane E, Yamane M, Mutoh M, et al, for the Retrograde Summit Investigators. Japanese multicenter registry evaluating the retrograde approach for chronic coronary total occlusion. Catheter Cardiovasc Interv. 82: E654-661 (2013).
- Morino Y, Abe M, Morimoto T, et al, for the J-CTO Registry Investigators. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO score as a difficulty grading and time assessment tool. J Am Coll Cardiol Intv. 4: 213-21 (2014).
- Galassi AR, Sianos G, Werner GS, et al. Retrograde recanalization of chronic total occlusions in Europe, procedural, in-hospital, and long-term outcomes from the multicenter ERCTO registry. J Am Coll Cardiol 65: 2388-2400 (2015).
- Karmpaliotis D, Karatasakis A, Alaswad K, et al. Outcomes with the use of the retrograde approach for coronary chronic total occlusion interventions in a contemporary multicenter US registry. Circ Cardiovasc Interv. 9: e003434 (2016).
- Brilakis ES, Grantham JA, Rintret S, et al. A percutaneous treatment algorithm for crossing coronary chronic total occlusions. J Am Coll Cardiol Intv. 5: 367-379 (2012).
- Christopoulos G, Kandzari DE, Yeh RW, et al. Development and validation of a novel scoring system for predicting technical success of chronic total occlusion percutaneous coronary interventions: the PROGRESS CTO (Prospective Global Registry for the Study of Chronic Total Occlusion Intervention) Score. J Am Coll Cardiol Intv. 9: 1-9 (2016).
- Muramatsu T. Current technical and clinical features of the antegrade and retrograde approaches to percutaneous transluminal coronary intervention for chronic total occlusion - 2013 version. The Egyptian Heart Journal. 66: 1–10 (2014).
- Okamura A, Iwakura K, Date M, et al. Navifocus WR is the promising intravascular ultrasound for navigating the guidewire into true lumen during the coronary intervention for chronic total occlusion. Cardiovasc Interv Ther. 29: 181-186 (2014).
- Whitlow PL, Burke MN, Lombardi WL, et al, for the FAST-CTO Trial Investigators. Use of a novel crossing and re-entry system in coronary chronic total occlusions that have failed standard crossing techniques. J Am Coll Cardiol Intv. 5: 393-401 (2012).
- Lee CK, Chen YH, Lin MS, et al. Retrograde Approach is as Effective and Safe as Antegrade Approach in Contemporary Percutaneous Coronary Intervention for Chronic Total Occlusion: A Taiwan Single-Center Registry Study. Acta Cardiol Sin. 33: 20-27 (2017).
- Klein LW, Miller DL, Balter S, et al. Occupational health hazards in the interventional laboratory: Time for a safer environment. Catheter Cardiovasc Interv 73: 432-438 (2009).
- Yan J, Thomson JK, Zhao W, et al. Role of Stress Kinase JNK in Binge Alcohol-Evoked Atrial Arrhythmia. J Am Coll Cardiol. 71: 1459-1470 (2018).