Editorial - Interventional Cardiology (2010) Volume 2, Issue 1
The left main coronary artery deserves more than a quick look
- Corresponding Author:
- Bernard De Bruyne
Cardiovascular Center Aalst, OLV Hospital, Moorselbaan, 164, B-9300 Aalst, Belgium
Tel: +32 53 72 44 39
Fax: +32 53 72 41 85
E-mail: bernard.de.bruyne@ olvz-aalst.be
Abstract
Keywords
Significant left main coronary artery (LMCA) stenosis is generally defined as the presence of a more than 50% stenosis at angiography. It is found in approximately 4% of patients undergoing diagnostic coronary angiography [1]. It is widely accepted that a significant narrowing of the LMCA puts a patient at high risk, as the stenosis jeopardizes almost the entire left ventricle. The current guidelines categorize the use of coronary artery bypass graft (CABG) for revascularization of patients with unprotected LMCA disease as a class IA recommendation, while they categorize the use of percutaneous coronary interventions (PCIs) as a class IIb or III recommendation [2,3]. Moreover, according to the existing guidelines, any stenosis of the LMCA of more than 50% should be treated surgically, regardless of the presence of symptoms or objective signs of ischemia [4]. These recommendations are based on studies conducted several decades ago when medical and surgical treatment practices were markedly different from current practice [5–7]. In addition, PCI has emerged as an alternative form of revascularization and its role in the treatment of LMCA stenoses is currently being investigated in prospective randomized trials. Yet, relatively little attention is paid to what should be the very first step of a patient-centered decision-making process: the precise diagnosis. The debate rages on how to treat prior to defining what exactly should be treated.
LMCA & noninvasive testing
We have been taught at medical school that a stable patient with suspected coronary artery disease should first undergo noninvasive testing to ascertain the presence of reversible ischemia prior to submitting the patient to a coronary angiogram. In reality, even though novel non-invasive testing is proposed every day, the vast majority of patients undergoing PCI have never undergone any stress testing, not to speak of their results [8]. Even in stable patients it appears that only a minority are submitted to a noninvasive stress test [9]. Ironically, it appears that the older the physician and the larger his case load, the lower the likelihood of asking for noninvasive stress testing. Noninvasive testing – and in particular myocardial perfusion imaging (MPI) – has proven to be highly sensitive and specific in detecting and localizing ischemia in patients with one-vessel disease and normal left ventricular function [10]. Yet, the presence of a LMCA stenosis is one of the numerous clinical situations in which the usefulness of MPI is less well established. The assessment of ‘ischemia’ at MPI is based on the difference in myocardial perfusion between ‘normal’ and ‘abnormal’ territories. Differences of approximately 20% are required to result in a positive perfusion imaging modality [11]. The balanced reduction in perfusion during stress in the presence of LMCA stenosis might be responsible for false-negative findings. In addition, since LMCA stenoses are rarely isolated, MPI will be of little help for guiding revascularization owing to its limited spatial accuracy. In a recently published study with 508 patients, the combination of a three-vessel pattern on single-photon emission computed tomography (SPECT) together with lung uptake of radiotracers, resulted in sensitivity of only 52% in the detection of LMCA disease [12]. In another study that included 101 patients with angiographically significant LMCA disease, quantitative SPECT assessment of perfusion data on top of qualitative assessment showed high-risk defects in only 59% of the total patient population [13]. Yet, the problem with all of these studies on the accuracy of noninvasive imaging for the detection of ‘significant coronary artery disease’ is that angiography is considered the gold standard. This is even more problematic in the case of stenosis of the LMCA.
LMCA & angiography
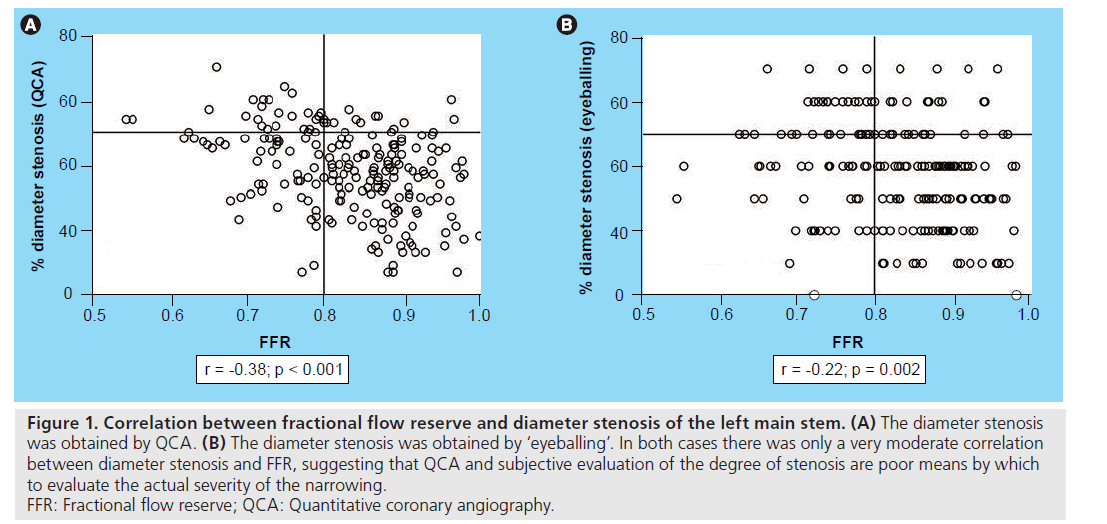
In the ‘real world’, decisions regarding revascularization in individual patients are often taken merely on the basis of the angiogram using the battered gold standard of 50% diameter stenosis as assessed by eyeballing. While it is common place to state that the angiogram is a poor predictor of the actual stenosis severity, this is particularly true in the case of LMCA stenosis. The investigators of the Coronary Artery Surgery Study (CASS) – a study that is still today, is considered the cornerstone of the treatment strategy in patients with LMCA disease – acknowledged an enormous intra- and inter-observer variability in the evaluation of LMCA stenoses [14,15]. In a recently published study, 213 patients with equivocal LMCA disease were estimated angiographically both visually by two independent observers and by quantitative coronary angiography (QCA) [16]. Fractional flow reserve (FFR) was measured in all patients to assess the actual severity of the LMCA lesion. Angiographic assessment of the lesions, either by QCA or by visual estimation failed to correctly identify the stenosis significance in almost a third of the total patient population (Figure 1). Moreover, interobserver concordance was only 52%. Of the patients, 23% had a LMCA stenosis less than or equal to 50% at angiography while the FFR was less than 0.80. If the decision concerning revascularization had been taken solely on the angiogram, the latter patients might have been denied CABG despite the presence of a hemodynamically significant stenosis. It should be observed that in the large trials (CASS, VA trial and European trial on CABG) on LMCA stenosis, patients were only included (and randomized) if they had a stenosis of more than 50%. It is very likely that many patients have been denied revascularization on the basis of a stenosis that was considered angiographically nonsignificant.
Figure 1: Correlation between fractional flow reserve and diameter stenosis of the left main stem. (A) The diameter stenosis was obtained by QCA. (B) The diameter stenosis was obtained by ‘eyeballing’. In both cases there was only a very moderate correlation between diameter stenosis and FFR, suggesting that QCA and subjective evaluation of the degree of stenosis are poor means by which to evaluate the actual severity of the narrowing. FFR: Fractional flow reserve; QCA: Quantitative coronary angiography.
“There are several reasons for the discrepancy between angiographic and hemodynamic assessment, especially in the case of left main coronary artery lesions...”
There are several reasons for the discrepancy between angiographic and hemodynamic assessment, especially in the case of LMCA lesions: overlapping of the catheter with the LMCA, spillover of contrast medium and incomplete mixing of blood and contrast medium in the proximal part of the LMCA may render the evaluation of an ostial lesion difficult; the LMCA is generally short and, when present, atherosclerosis is often diffusely distributed so that a normal segment is lacking. This leads to an underestimation of the ‘reference’ segment and, thus, to an underestimation of LMCA stenoses by both visual estimation and QCA; the myocardial mass that depends on the LMCA is large and, thus, the amount of blood that flows through it is great. Substantial trans-stenotic flow, in turn, induces large pressure gradients, especially during hyperemia. This explains why the relationship between angiography and FFR is different in LMCA stenoses as compared with most other segments of the coronary tree in which the angiogram often tends to overestimate the actual lesion severity. Accordingly, revascularization strategies based solely on the angiogram are likely to be inappropriate in patients with a LMCA stenosis.
LMCA & intravascular ultrasound
Intravascular ultrasound (IVUS), another morphologic approach, is often advocated to evaluate the LMCA stenosis. A minimal cross-sectional area (CSA) of 6–8 mm2 is often proposed as the threshold to identify a significant LMCA stenosis. Theoretically, IVUS should share the same limitation as angiography in gauging the physiologic repercussions of a LMCA stenosis. It is important to remember that the physiologic severity of a stenosis depends on the metrics of the stenotic segments, and also on the mass of myocardium perfused (and hence the transstenotic flow) by that given segment. For this reason, a given CSA will have a completely different physiologic meaning in the LMCA and in the second obtuse marginal branch. For the same reason, a minimal CSA of 6 mm2 in the LMCA will have a completely different significance in a 30‑year-old American football player than in an 80‑year-old frail lady. Nevertheless, IVUS has two immense advantages over angiography: its accuracy (and hence its reproducibility) in measuring not only the lumen but also plaque size and the capability to assess the composition of the vessel wall. This makes IVUS a very appreciable help when evaluating LMCA stenosis when PCI is considered. The currently available data come from four relatively small studies, from which three have correlated their IVUS findings with clinical events at follow-up [17–20].
“A substantial change in our general beliefs concerning left main coronary artery stenoses is needed.”
Abizaid et al. demonstrated that minimal CSA was the most important predictor of cardiac events at 1‑year in 122 patients with moderate LMCA disease [17]. Jasti et al. found a relatively good correlation between morphological evaluation by IVUS and physiological assessment with FFR of ambiguous LMCA lesions in 55 selected patients [18]. In 214 patients with angiographically indeterminate LMCA stenosis, Fassa et al. reported that an IVUS-guided treatment strategy may help to safely defer revascularization in patients with a nonsignificant LMCA stenosis [19]. Accordingly, these authors reported no benefit of revascularization in patients with a minimum lumen area (MLA) of 7.5 mm2 or greater while deferral of revascularization for patients with an MLA of less than 7.5 mm2 was associated with a very poor prognosis, emphasizing the need for an accurate assessment of LMCA stenosis severity.
“...revascularization strategies based solely on the angiogram are likely to be inappropriate in patients with a left main coronary artery stenosis.”
LMCA & fractional flow reserve
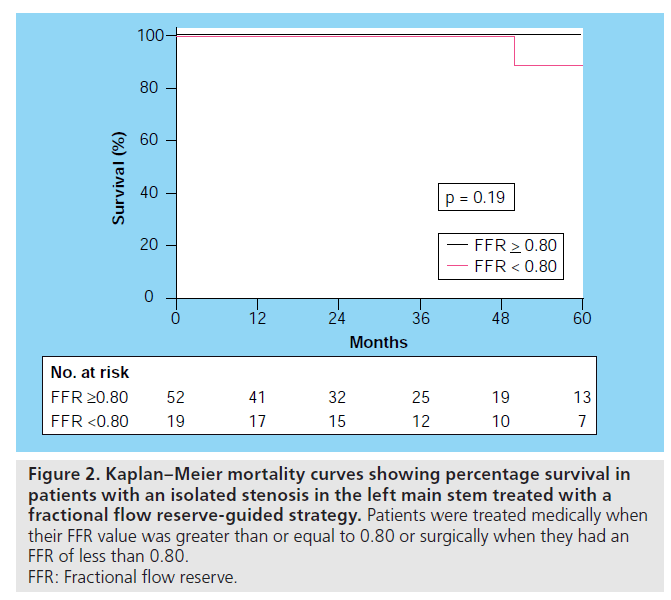
The pressure-derived FFR provides the physician with exactly the same information as myocardial perfusion imaging except FFR is quantified as percentage of normal maximal flow, is more accurate in intermediate stenoses, has a much better spatial resolution, and – most importantly – is available in the catheterization laboratory, the very place where the treatment can be applied. Recent data indicate that the additional doses of radiation, time and contrast medium required to obtain FFR after a diagnostic angiogram are so low that an ‘all-in-one’ approach can reasonably be contemplated in patients with suspected coronary artery disease (i.e., the combination a full anatomic [angiography] and functional [FFR] diagnostic work-up and – only when needed – ad hoc revascularization [PCI]) [21]. A recently published study demonstrated that a FFR-guided revascularization strategy can safely be applied in patients with LMCA stenosis: after a mean follow- up of 5 years, the mortality was surprisingly low in patients with a LMCA stenosis at angiography but in whom no CABG was performed on the basis of an FFR 0.80 or greater across the LMCA stenosis [16]. There was no difference in clinical outcome (mortality and major adverse cardiac events) in patients with an isolated LMCA stenosis who were treated medically or by CABG based on FFR measurements (Figure 2). A number of caveats of FFR measurements in LMCA should be kept in mind when performing these measurements, which can have major implications for the patient: isolated LMCA stenoses are relatively rare. Coexisting stenoses in the left anterior descending (LAD) artery or in the left circumflex artery (LCx) will tend to increase the FFR measured across the LMCA stenosis. The influence of a LAD and/or LCx lesion on the FFR value of the LMCA will depend on the severity of this distal stenosis but, even more, on the size of the vascular territory supplied by this vessel. To partially overcome this, a pullback curve should always be obtained in the case of lesions in the LAD or LCx in order to allow complete functional mapping of the epicardial coronary vasculature. The hyperemic stimulus should preferably be given intravenously and, in any case, the guiding catheter should be disengaged from the ostium when performing the measurements. In case of associated occlusion of the right coronary artery with collaterals from the left coronary artery, FFR will tend to be lower than if these collaterals were absent. This is not a pitfall or an erroneous measurement. It is simply the expression that FFR takes into account the total mass of perfused myocardium (in this case the territory normally supplied by the LMCA and that supplied by the right coronary artery).
Figure 2: Kaplan–Meier mortality curves showing percentage survival in
patients with an isolated stenosis in the left main stem treated with a
fractional flow reserve-guided strategy. Patients were treated medically when
their FFR value was greater than or equal to 0.80 or surgically when they had an
FFR of less than 0.80.
FFR: Fractional flow reserve.
Conclusion
Discussions regarding LMCA stenoses have focused on the question ‘how to revascularize?’ The essential question (i.e., should we revascularize?) is amazingly rarely discussed. This relates to the conviction that all angiographically visible stenoses of more than 50% should be revascularized while all stenoses of less than 50% should not. Recent data, however, indicate that:
▪ Unlike other segments of the coronary tree, angiography is highly inaccurate in evaluating the severity of LMCA stenoses;
▪ In contrast to all other segments of the coronary tree, this inaccuracy at the level of the LMCA mainly translates into an underestimation of lesion severity;
▪ Medium- to long-term clinical outcome is excellent in patients with a LMCA stenosis at angiography and in whom CABG is not performed on the basis of an FFR value larger than 0.80.
A substantial change in our general beliefs concerning LMCA stenoses is needed. A large randomized trial is about to start to compare the optimal revascularization modality (CABG vs drug-eluting stents) in patients with LMCA stenoses. Proper identification of patients who are likely to benefit from these treatments is indispensable so as not to cloud the results by including patients in whom nothing can be expected from revascularization.
Financial & competing interests disclosure
This work was supported by the Meijer Lavino Foundation for Cardiac Research. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed. No writing assistance was utilized in the production of this manuscript.
References
- Noto TJ Jr, Johnson LW, Krone R et al.: Cardiac catheterization 1990: a report of the Registry of the Society for Cardiac Angiography and Interventions (SCA&I). Cathet. Cardiovasc. Diagn. 24, 75–83 (1991).
- Kushner FG, Hand M, Smith SC Jr et al.: 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 54(23), 2205–2241 (2009).
- Silber S, Albertsson P, Avilés FF et al.; Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology: Guidelines for percutaneous coronary interventions. The Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology. Eur. Heart J. 26(8), 804–847 (2005).
- Eagle KA, Guyton RA, Davidoff R et al.: ACC/AHA 2004 guideline update for coronary artery bypass graft surgery: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 110, 1168–1176 (2004).
- Chaitman BR, Fisher LD, Bourassa MG et al.: Effect of coronary bypass surgery on survival patterns in subsets of patients with left main coronary artery disease. Report of the Collaborative Study in Coronary Artery Surgery (CASS). Am. J. Cardiol. 48, 765–777 (1981).
- European Coronary Surgery Study Group: Prospective randomised study of coronary artery bypass surgery in stable angina pectoris. Second interim report by the European Coronary Surgery Study Group. Lancet 2, 491–495 (1980).
- Kroncke GM, Kosolcharoen P, Clayman JA, Peduzzi PN, Detre K, Takaro T: Five-year changes in coronary arteries of medical and surgical patients of the Veterans Administration Randomized Study of Bypass Surgery. Circulation 78, I144–I150 (1988).
- Topol EJ, Ellis SG, Cosgrove DM et al.: Analysis of coronary angioplasty practice in the United States with an insurance-claims data base. Circulation 87, 1489–1497 (1993).
- Lin GA, Dudley RA, Lucas FL, Malenka DJ, Vittinghoff E, Redberg RF: Frequency of stress testing to document ischemia prior to elective percutaneous coronary intervention. JAMA 300, 1765–1773 (2008).
- Go V, Bhatt MR, Hendel RC: The diagnostic and prognostic value of ECG-gated SPECT myocardial perfusion imaging. J. Nucl. Med. 45, 912–921 (2004).
- Aarnoudse WH, Botman KJ, Pijls NH: False-negative myocardial scintigraphy in balanced three-vessel disease, revealed by coronary pressure measurement. Int. J. Cardiovasc. Intervent. 5(2), 67–71 (2003).
- Berman DS, Kang X, Slomka PJ et al.: Underestimation of extent of ischemia by gated SPECT myocardial perfusion imaging in patients with left main coronary artery disease. J. Nucl. Cardiol. 14, 521–528 (2007).
- Shiba C, Chikamori T, Hida S et al.: Important parameters in the detection of left main trunk disease using stress myocardial perfusion imaging. J. Cardiol. 53, 43–52 (2009).
- Fisher LD, Judkins MP, Lesperance J: Reproducibility of coronary arteriographic reading in the coronary artery surgery study (CASS). Cathet. Cardiovasc. Diagn. 8, 565–575 (1982).
- Taylor HA, Deumite NJ, Chaitman BR, Davis KB, Killip T, Rogers WJ: Asymptomatic left main coronary artery disease in the Coronary Artery Surgery Study (CASS) registry. Circulation 79, 1171–1179 (1989).
- Hamilos M, Muller O, Cuisset T et al.: Long-term clinical outcome after fractional flow reserve-guided treatment in patients with angiographically equivocal left main coronary artery stenosis. Circulation 120, 1505–1512 (2009).
- Abizaid AS, Mintz GS, Abizaid A et al.: One-year follow-up after intravascular ultrasound assessment of moderate left main coronary artery disease in patients with ambiguous angiograms. J. Am. Coll. Cardiol. 34, 707–715 (1999).
- Jasti V, Ivan E, Yalamanchili V, Wongpraparut N, Leesar MA: Correlations between fractional flow reserve and intravascular ultrasound in patients with an ambiguous left main coronary artery stenosis. Circulation 110(18), 2831–2836 (2004).
- Fassa AA, Wagatsuma K, Higano ST et al.: Intravascular ultrasound-guided treatment for angiographically indeterminate left main coronary artery disease: a long-term follow-up study. J. Am. Coll. Cardiol. 45, 204–211 (2005).
- Ricciardi MJ, Meyers S, Choi K, Pang JL, Goodreau L, Davidson CJ: Angiographically silent left main disease detected by intravascular ultrasound: a marker for future adverse cardiac events. Am. Heart. J. 146, 507–512 (2003).
- Ntalianis A, Trana C, Muller O et al.: Radiation, contrast medium and time needed for fractional flow reserve assessment after a left heart catheterization. Circulation 120, S927 (2009).