Research Article - International Journal of Clinical Rheumatology (2022) Volume 17, Issue 2
The Efficacy of Platelet Rich Plasma in Treating Symptomatic Cases with MRI-Confirmed Degenerative Medial Meniscal Lesions
Guoyou Zou*
Department of Orthopaedics, The Fourth Affiliated Hospital of Nantong University, Yancheng, 224005, PR China
- *Corresponding Author:
- Guoyou Zou
Department of Orthopaedics, The Fourth Affiliated Hospital of Nantong University, Yancheng, 224005, PR China
E-mail: zgy01rq@163.com
Received: 07-Feb-2022, Manuscript No. fmijcr-22-53753; Editor assigned: 08-Feb-2022, PreQC No. fmijcr-22-53753(PQ); Reviewed: 22-Feb-2022, QC No. fmijcr-22-53753; Revised: 25-Feb-2022, Manuscript No. fmijcr-22-53753(R); Published: 28-Feb-2022, DOI: 10.37532/1758-4272.2022.17(2).027-031
Abstract
Objects: To observe the efficacy and imaging changes after autologous platelet rich plasma intra-articular injection for symptomatic degenerative meniscal lesions.
Methods: From December 2019 to May 2021, 68 knee pain outpatients over 50 years old whose diagnoses were also confirmed by MRI which showing I-III degree meniscus degenerative lesions underwent a series of intra-articular injection of autologous platelet rich plasma (PRP), 3 sequential injections with 7-day intervals. All patients were followed-up and evaluated by Lysholm Knee Scoring Scale at the time of the 1st and 6th month post-treatment. MRI was rearranged for all patients at the time of the sixth month after treatment to observe if there were changes of the meniscal lesion as well as the edema of the MCL and the adjacent bone marrow. Results: The Lysholm scores of 68 patients were all significantly improved post-treatment and there was no significant difference between one month and six months after treatment. MRI showed that after 6 months of PRP treatment the bone marrow edema areas were dramatically decreased and even totally disappeared in some patients (15/25). Meanwhile, MRI imaging also showed in 83.3% (65/78) of the patients that the edema around the medial collateral ligament (MCL) disappeared completely while others presented significant diameter-decrease of their primary edema areas.
Conclusions: Good clinical outcomes were achieved in patients with symptomatic degenerative medial meniscus lesions after intra-articular injection of PRP. MRI showed the primary edema area of the medial collateral ligament and the bone marrow both decreased and, in some cases, even disappeared at the sixth month post-treatment.
Keywords
meniscus • platelet rich plasma • MRI • degenerative lesions • medial collateral ligament
Introduction
Meniscus is generally considered of functional in knee joint protection and intact meniscus can prevent knee osteoarthritis [1]. With the increase of age, degenerative injury appears inside meniscus which is mainly manifested by the change of its internal structures, and horizontal tear is the main type of injury on MRI images [2]. Degenerative lesion of menisci is considered of the early stage of the knee osteoarthritis [3,4]. And literature statistics showed that 90% of symptomatic osteoarthritis patients’ had positive meniscus lesions on their MRI pictures [5] and osteoarthritis-related medial gonarthrosis is much more frequent than the lateral [3].
Clinically, we observed that many adult patients with knee pain (early stage) showed medial side or posteromedial pain mainly and their MRI showed medial meniscus injury changes and edema area inside or around the MCL and the adjacent medial tibial plateau or the medial femoral condyle bone marrow. Therefore, we choose this kind of patients who majorly manifesting medial side pain with positive medial meniscus lesion confirmed by MRI into our clinical study to probe how to relief the knee symptoms and to prevent or protect the symptomatic knee from further deteriorating, which is an important point in preventing osteoarthritis progression.
Platelet-rich plasma (PRP) has already been widely used in treating knee osteoarthritis [6,7]. In our study, patients with symptomatic degenerative meniscus lesion were treated with PRP and the therapeutic effects were observed accordingly. Furthermore, by observing the healing changes of degenerative meniscus itself and the edema changes of surrounding tissues on MRI study, we discussed, on a preliminary level, the corresponding factors related to the pain symptoms and presumed that meniscus itself might not be the real or major cause of pain.
Materials and methods
Clinical data
From December, 2019 to May, 2021, 68 outpatients of knee pain who were over 50 years old and whose medial meniscal I-III tear was confirmed by MRI were treated with PRP injection. Two radiologists evaluated the MRI data separately. All patients were confirmed that there was no other injury that compromising the knee stable structures thus surgical intervention might needed. There were 24 males and 44 females in our group, with an average age of 60.5 years (50-75 years), all of whom had no clear history of joint trauma. All these patients were underwent MRI examination in the same hospital. Nearly 30% of the patients earlier received other unsuccessful conservative treatments, such as rest, oral non-steroidal anti-inflammatory analgesics (NSAIDs), glucocorticoid injection into the knee joint, etc. The inclusion criteria of this study are: (1) Knee joint pain; (2) Age over 50 years old; (3) MRI showed I-III degree horizontal tear of meniscus. Exclusion criteria: (1) III-IV knee osteoarthritis; (2) knee ligament rupture, fracture and other diseases requiring surgery; (4) Rheumatoid arthritis and gout; Diabetes, blood diseases, severe cardiovascular diseases, infections.
Informed consent of patients
This study has been permitted by the Ethics Committee of Yancheng First People's Hospital. Before treatment, patients were informed that: (1) PRP is a new treating method and the author has widely used this in the treatment of knee joint diseases and tendinous disorders with satisfactory results; (2) PRP was a product of autologous venous blood centrifugation thus no serious complications were found in clinical application; (3) Sign the informed consent form.
PRP preparation and joint cavity injection
By drawing 20 mL of peripheral venous blood into two 15 mL BD sterile centrifugal tubes each containing 1 mL of anti-coagulant and shaking them slightly and evenly to avoid blood coagulation, we put them into a routine centrifugation with the rotating speed of 1100 r/min and the centrifugal radius 13.5 cm. The whole blood was divided into three layers after 10 minutes centrifuging. From each tube we took of about 5ml of white blood cells and plasma layer just above the red blood cell layer, and then combined them into a new tube for a new round of centrifuging, 2200 r/min for 10 min. Then the serum layer above was removed, and about 3-5 mL of PRP --a mixture of the white-bloodcell layer and the plasma just above it was ready for use [8]. After a thorough sterile of the affected knee joint, this PRP was injected into the medial compartment of the knee, using a anterior-medial approach. The patient was asked to do a gentle flexing and extending of his or her knee and was informed that daily activities not strictly limited but strenuous exercises avoided within one week. The treatment was on a 7-day-interval basis, three times in total. NSAIDs and analgesic medication could be taken orally during the treatment in case of joint pain. Those patients with both sides symptoms were too told to have a 3 times treatment on their severe knee first, and then turn to another knee if the first knee showing nice.
Follow-up and the evaluation of clinical results
Patients were followed up and assessed before treatment and at the 1st and 6th month after the first treatment. At each follow-up, the knee joint was evaluated by physical examination and by Lysholm scoring system. At the 6th month, MRI was reexamined to observe if there’s meniscus healing as well as any changing of its surrounding tissues. Two radiologists independently evaluated MRI data before and after treatment.
Statistical analysis
All data analyses were performed using SPSS 13.0 software (IBM Corp., Armonk, NY, USA). The Lysholm scores at the various time points are presented as mean and standard deviation and were compared by one way analysis of variance using Bonferroni test. The difference was statistically significant with P<0.05.
Results
All patients had fulfilled three treatments and a 12 months follow-up. No knee joint infection happened. For these 68 patients, a total number of 90 knees underwent the PRP treating procedure. Among them, 78 knees were double examined by MRI before and after the treatment and their first MRI all showed medial meniscus lesions and accompanying inflammatory edema around the medial collateral ligament (MCL). There was also co-existed bone marrow edema in 25 joints of these 78 knees.
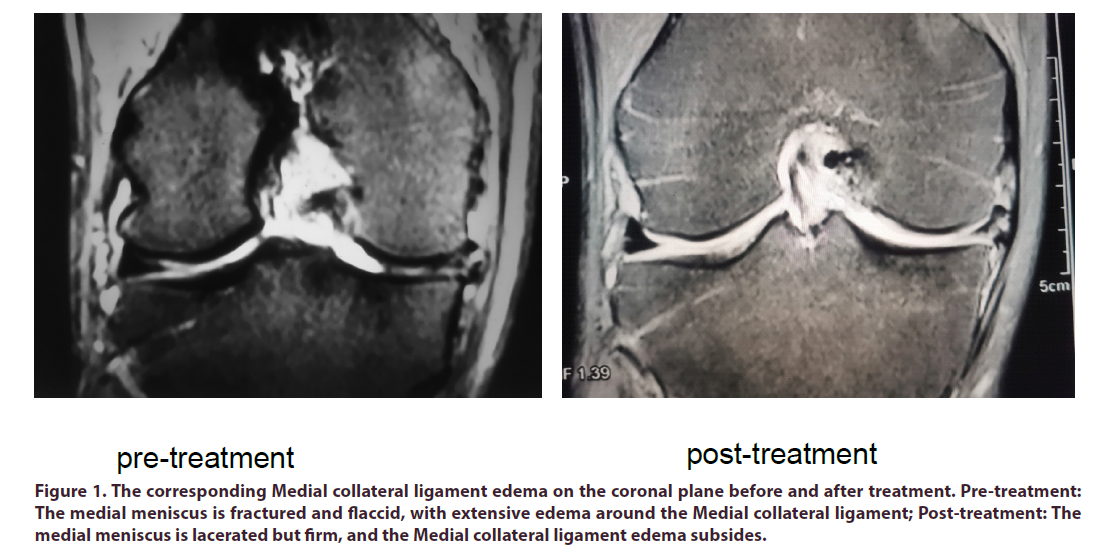
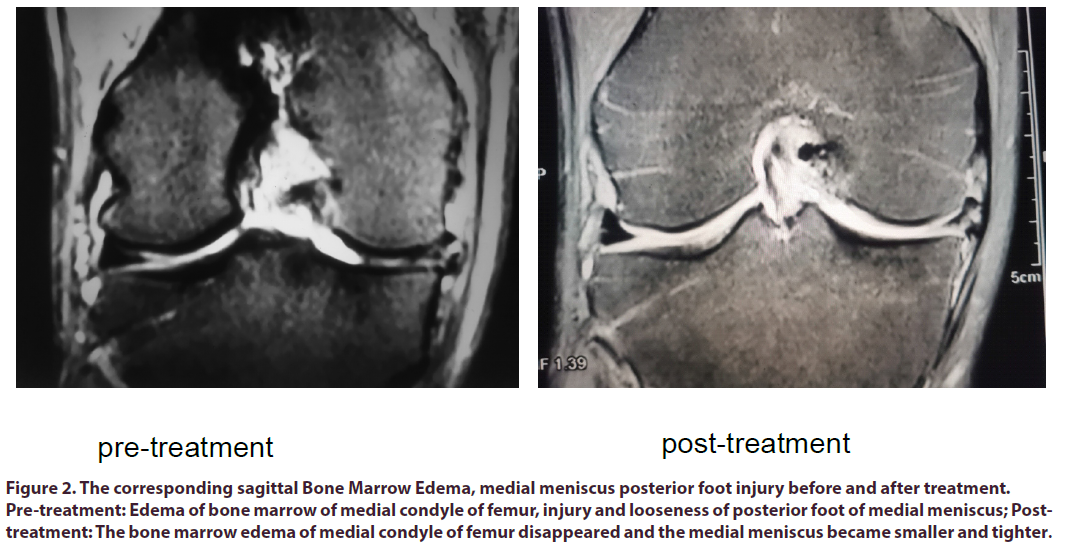
Lysholm score of these 68 patients before treatment, 1st month, 6th month and 12th month was 51.94±14.04, 77.83±12.68, 79.27±11.61 and 74.65±12.41, respectively. A significant difference was shown between before and after the treatment (Table 1). However, no significant difference was shown between the 1st, 6th and 12th month after treatment (Table 1). Three patients underwent arthroscopic surgery and one patient underwent total knee replacement surgery eventually due to their unalleviated symptoms. MRI reexamination six months after treatment showed as followed: in 83.3% of patients, the inflammatory edema around the MCL subsided completely; and in others, the edema diameter reduced significantly decreased compared with their 1st MRI pictures (Figure 1); for those 25 knees with bone marrow edema there were 15 cases of complete disappearance and 10 cases of significantly decrease of the edema area (Figure 2). These imaging observations mentioned above, were evaluated independently and separately by two radiologists. And their observing results were of highly consistent, no difference. For menisci, to which we prospectively expected some healing phenomenon might presented, the major aftertreatment- change was, if any, the affected meniscus seemed reduced in size and more compacted in shape (Figures 1 and 2).
Figure 1. The corresponding Medial collateral ligament edema on the coronal plane before and after treatment. Pre-treatment: The medial meniscus is fractured and flaccid, with extensive edema around the Medial collateral ligament; Post-treatment: The medial meniscus is lacerated but firm, and the Medial collateral ligament edema subsides.
Figure 2. The corresponding sagittal Bone Marrow Edema, medial meniscus posterior foot injury before and after treatment. Pre-treatment: Edema of bone marrow of medial condyle of femur, injury and looseness of posterior foot of medial meniscus; Posttreatment: The bone marrow edema of medial condyle of femur disappeared and the medial meniscus became smaller and tighter.
| Time | Lysholm score |
|---|---|
| pre-treatment | 51.94±14.04 |
| 1 month post-treatment | 77.83±12.68 |
| 6 months pos-ttreatment | 79.27±11.61 |
| 12 months post-treatment | 74.65±12.41 |
| F | 206 |
| P | 0 |
Table 1. Comparison of lysholm scores before and after PRP treatment.
Discussion
All the cases we recruited into this study were symptomatic patients whose major symptom was related to medial or posteromedial knee pain. MRI examination was choose as the best and unified measure for confirming diagnosis, assessing the pain source and evaluating post-treatment changes. We found a common phenomenon in all the MRI-examined 78 knees that medial meniscus degenerative lesion was almost always accompanied by a co-existing MCL edema, which we thought of coherent with its biomechanical character. The MCL is an important medial side stable structure and its deep fibers blend with the medial capsule tightly so the MCL is prone to be affected by sustained stress and strains, especially the valgus and external rotating loads. The author of this study had previously used PRP local injection in treating Achilles tendinitis and found that the edema around the tendon subsided down completely afterward [9] .This previous experience provided a practical basis for PRP treatment as a method for patients with degenerative medial meniscus injury and accompanied inflammatory edema of the MCL. The patients in this study all had medial knee tender point by palpation, which was coherent with the inflammatory edema site of the MCL. After treatment, medial knee pain greatly relieved in most patients. The- 6th-month-MRI showed that the edema of the MCL subsided completely in 85% of our patients and others also got their previous edema obviously reduced. On the contrary, meniscus repair phenomenon was rarely observed in this study, indicating that the medial knee pain might be more related to the inflammatory edema of the MCL than to meniscus itself.
Against what we primarily expected, no direct MRI imaging evidence of meniscus repair was found in this study, much similar to the result of D. Guenoun’s research [10], which also showed no evidence of meniscal repair in his research of applying PRP to treat meniscal injury. Of course, it should be noted that rather than conducting a medium or a long-term study, both D. Guenoun’s research and our study only took one after-treatment-MRI reexamination at the time of the 6th month. Interestingly, in another study, a very thorough case report, J.P. Betancourt exhibited the MRI of a meniscal degenerative injury case at the time of 12 months after PRP treatment [11] and found that no obvious repair of meniscal lesion could be seen though the patient’s symptom disappeared. Strangely, the same MRI showed that some immature tissue appeared in the meniscal lesion area. Similar phenomenon were also found in some of our cases as mentioned above, which we presumed to be a abscission and absorption of the ruptured meniscal tissues--a kind of “melt down”--for we had observed after PRP treatment the meniscus had become smaller and more compacted in these cases. Literature reveals the close relationship between degenerative meniscal injury and the development of knee osteoarthritis [12], and mainstream opinions have considered the arthroscopic treatment approaches to degenerative meniscus injury of ineffective or useless [13]. So comes one question that many of us might to ask: is there any real effective alternative to fill the big gap between the early onset of the-degenerative-meniscusstage and severe osteoarthritis stages that requiring knee replacement? During this long period, patients may demonstrate different symptoms but they all need some way to alleviate their pain or even stop their knee osteoarthritis progression. Though the current clinical outcomes varied (which may be due to the degree of osteoarthritis of patients selected by various studies) in treating osteoarthritis with PRP worldwide [14,15] , it is widely agreed that PRP can relieve the joint pain for many patients [16,17].
The author of this study had also previously found the similar phenomenon that after PRP injection the pain greatly relieved and bone morrow edema significantly reduced in knee osteoarthritis cases [18]. Now in this study, among the 78 knee joints examined by MRI, 25 knees manifested medial meniscus degenerative lesion and coexisting bone marrow edema. Jeffrey B. Driban et al [19] holds the opinion that bone marrow edema is related to the occurrence of knee osteoarthritis, and the regression or partial regression of bone marrow edema is directly related to the delay or termination of the osteoarthritis natural course. This viewpoint seems to be somewhat confirmed by our study-- out of the 25 knees with bone marrow edema there were 15 cases of edema complete vanished and 10 cases of edema significantly subsided (Figure 2), and their symptoms greatly alleviated.
Conclusion
In summary, this study confirmed the good result of using autologous platelet rich plasma in the treatment of symptomatic degenerative medial meniscus injury of knee joint. Although one of our primary goals was aimed at any objective evidence of damaged meniscal tissue repairing alone with the pain relief after PRP treatment, instead, we found more direct improvement in tissues around the meniscus itself, like the MCL. So we reasonably hypothesize that as least a considerable amount of the clinical efficacy came from the regression of MCL edema, as well as the regression or reduction of the adjacent bone marrow edema after PRP treatment.
The deficiency of our study is as followed: no control group was set up and the clinical follow-up period was relatively short, which needs to be improved in the future research.
References
- Ding C, Martel-Pelletier J, Pelletier JP. Meniscal tear as an osteoarthritis risk factor in a largely non-osteoarthritic cohort: c cross sectional study. J Rheumatolo. 34,776-784 (2007).
- Englund M, Guermazi A, Gale D et al. Incidental meniscal fifindings on knee MRI in middle-aged and elderly persons. N Engl J Med. 359,1108-1115 (2008).
- Seitz AM, Osthaus F, Schwer J et al. Osteoarthritis-Related Degeneration Alters the Biomechanical Properties of Human Menisci Before the Articular Cartilage. Front Bioeng Biotechnol. 9,659989 (2021).
- Jarraya M, Roemer FW, Englund M et al. Meniscus morphology: Does tear type matter? A narrative review with focus on relevance for osteoarthritis research. Semin Arthritis Rheum. 46(5),552-561 (2017).
- Englund M, Guermazi A, Lohmander LS. The meniscus in knee osteoarthritis. Rheum Dis Clin North Am. 35(3),579-90 (2009).
- John W Belk , Matthew J Kraeutler, Darby A Houck et al. Platelet-Rich Plasma Versus Hyaluronic Acid for Knee Osteoarthritis: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Am J Sports Med. 49(1),249-260 (2021).
- McLarnon M, Heron N. Intra-articular platelet-rich plasma injections versus intra-articular corticosteroid injections for symptomatic management of knee osteoarthritis: systematic review and meta-analysis. BMC Musculoskelet Disord. 22: 550 (2021).
- Aw AA, Leeu JJ, Tao X et al. Comparing the efficacy of dual Platelet-Rich Plasma (PRP) and Hyaluronic Acid (HA) therapy with PRP-alone therapy in the treatment of knee osteoarthritis: a systematic review and meta-analysis. J Exp Orthop. 8:1-15 (2021).
- Zou G, Jia W, Zheng M et al. Platelet-rich plasma trigger point injection treatment for chronic achilles insertion tendonitis. Chinese Journal of General Practitioners. 8(12),657-659 (2013).
- Guenoun D, Magalon J, de Torquemada I et al. Treatment of degenerative meniscal tear with intrameniscal injection of platelets rich plasma. Diagn Interv Imaging. 101(3),169-176 (2020).
- Betancourt JP, Murrell WD. Leukocyte-poor platelet-rich plasma to treat degenerative meniscal tear: A case report. J Clin Orthop Trauma. 7(Suppl 1),106–109 (2016).
- Verdonk R, Madry H, Shabshin N et al. The role of meniscal tissue in joint protection in early osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 24,1763–74 (2016).
- Sihvonen R, Paavola M, Malmivaara A et al. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. Engl J Med. 369(26),2515-24 (2013).
- Jianbing Ma, Wenxing Yu, Xiujin Chen et al. Platelet-rich plasma shows beneficial effects for patients with knee osteoarthritis by suppressing inflammatory factors. Exp Ther Med. 15(3),3096–3102 (2018).
- Nie L, Zhao K, Ruan J et al. Effectiveness of Platelet-Rich Plasma in the Treatment of Knee Osteoarthritis: A Meta-analysis of Randomized Controlled Clinical Trials. Orthop J Sports Med. 9 (2021).
- Joint surgery Group. Chinese Orthopedic Association Osteoarthritis diagnosis and treatment guideline. China J Orthop. 38,705-715 (2018).
- McLarnon M, Heron N. Intra-articular platelet-rich plasma injections versus intra-articular corticosteroid injections for symptomatic management of knee osteoarthritis: systematic review and meta-analysis. BMC Musculoskelet Disord. 22,550 (2021).
- Zou Guo-you, Jia Wei-tao, Zheng Min-qian. Autologous platelet-rich plasma intra-articular injection for treatment the knee osteoarthritis: a preliminary study. Chinese Journal of injury repair and wpund healing. 8,482-486 (2013).
- Driban J, Davis JE, Lu B et al. Accelerated Knee Osteoarthritis is Characterized by Destabilizing Meniscal Tears and Pre-Radiographic Structural Disease Burden. Arthritis Rheumatol. 71(7): 1089–1100 (2019).
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref