Case Report - International Journal of Clinical Rheumatology (2019) Volume 14, Issue 6
Polyarteritis nodosa and renal vein thrombosis: A case report and review of the literature
- Corresponding Author:
- Francesco Bozzao
Department of Medicine
Azienda Sanitaria Universitaria Integrata and University of Trieste (ASUITs)
Strada di Fiume 449, 34149, Trieste, Italy
E-mail: francesco.bozzao@gmail.com
Abstract
Renal Vein Thrombosis (RVT) is rare and usually complicates nephrotic syndrome and renal malignancies. We report the case of a 48-year-old woman, who was diagnosed with polyarteritis nodosa (PAN) and RVT, which was incidentally detected during diagnostic workup. Venous thromboembolism (VTE) can complicate the active phases of several vasculitides. Our review of the literature suggests that the risk of VTE in PAN is lower than that in other vasculitides, although it remains higher during the active disease. Our case reminds clinicians that VTE can be a rare manifestation of PAN.
Keywords
polyarteritis nodosa • renal vein thrombosis • venous thromboembolism • vasculitis
List of Abbreviations
RVT: Renal Vein Thrombosis; HBV: Hepatitis B Virus; DNA: deoxyribonucleic acid; ANCA: AntiNeutrophil Citoplasmic Antibodies; CT: Computed Tomography; PAN: Polyarteritis Nodosa; VTE: Venous Thromboembolism; AKI: Acute Kidney Injury; AAV: ANCA-Associated Vasculitides; BD: Behçet's Disease; GPA: Granulomatosis with Polyangiitis; MPA: Microscopic Polyangiitis; EGPA: Eosinophilic Granulomatosis with Polyangiitis; H&E: Hematoxylin and Eosin
Introduction
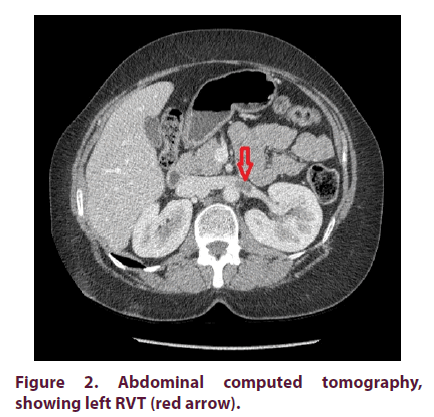
Renal Vein Thrombosis (RVT) is a rare medical condition occurring most commonly in adults with nephrotic syndrome and renal cell carcinoma [1]. Additional causes include trauma, oral contraceptives, dehydration, inherited thrombophilia’s or extra renal compression of the renal vein. Although RVT can present with symptoms of renal infarction, including flank pain or hematuria, it remains most often asymptomatic and carries a risk of pulmonary embolism [2]. It can also be incidentally discovered by imaging studies, as in our case. Here, we described a 48-year old woman with signs and symptoms suggestive of vasculitis of medium-sized vessels, in which a left RVT was detected by Computed Tomography (CT), performed to exclude an occult malignancy.
Therapy of RVT depends upon the renal function, since patients with Acute Kidney Injury (AKI) require thrombolysis with or without thrombectomy, and the others are generally treated using anticoagulants [2]. There are some exceptions, such as that described in our case report.
Case presentation
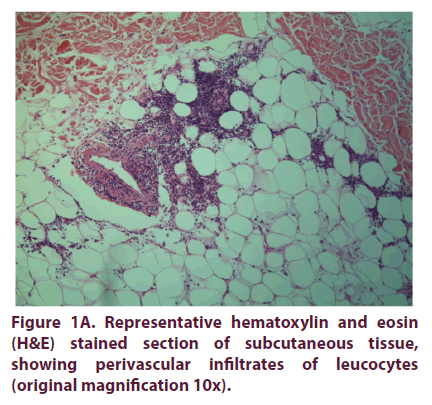
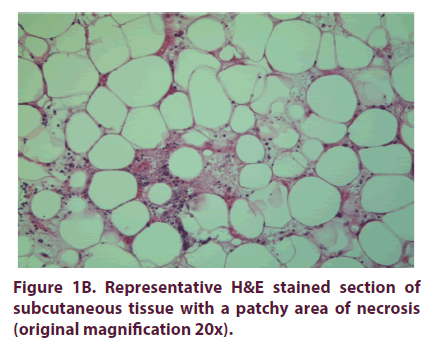
A 48-year-old woman presented to our Department with a three-month history of painful nodules on the thorax and the upper limbs, recurrent fever and headache, persistent myalgia, unintentional weight loss of 6 kg and high levels of diastolic blood pressure (150/110 mmHg). Physical examination revealed livaedo reticularis on the lower limbs, while the painful nodules were suggestive of erythema nodosum. C-reactive protein and erythrocyte sedimentation rate were elevated; a past hepatitis B with undetectable levels of serum HBV DNA was also detected. Anti-Neutrophil Cytoplasmic Antibodies (ANCA), antinuclear antibodies and cryoglobulins were all negative. Skin biopsy revealed a necrotizing vasculitis of mediumsized and small vessels and perivascular lymphogranulocytic infiltrates (Figure 1a and 1b). To exclude a paraneoplastic vasculitis, a total-body CT was performed, which revealed a left RVT (Figure 2). Screening tests for inherited or acquired forms of thrombophilias, antiphospholipid antibodies and lupus anticoagulant were all negative. AKI and nephrotic syndrome were also excluded.
Given the American College of Rheumatology classification criteria [3], polyarteritis nodosa (PAN) associated with RVT was diagnosed and the patient received steroids (Prednisone 1 mg/kg/day) with a gradual tapering schedule, low-molecular-weight heparin (100 units/kg twice daily), and Azathioprine (100 mg/day), then substituted with Methotrexate (20 mg/ week) because of gastric intolerance. At the CT performed two months later, RVT was no longer present and heparin therapy was discontinued. In the following five months the patient did not experience a relapse and steroids were stopped.
Discussion
PAN is a necrotizing vasculitis involving medium-sized and small arteries without glomerulonephritis or vasculitis in arterioles, capillaries and venules [4]. ANCA are typically negative. While most cases are considered idiopathic, a minority is associated with hepatitis B or other infections. Vascular inflammation is usually segmental and predominates in branching points. Vascular occlusion can occur because of thrombosis, intimal hyperplasia or fibrosis of the vessel wall, while severe wall injury can cause microaneurysms [5].
VTE is a recognized complication of several vasculitides, especially during periods of active disease [6]. This is certainly true for Behçet's Disease (BD), in which up to 40% of patients develop vascular involvement, mostly venous in origin, with the most common sites being deep vein thrombosis in the extremities and superficial thrombophlebitis [7]. Anti-Neutrophil Cytoplasmic Antibody (ANCA) associated vasculitides (AAV) are also associated with VTE. As emerged during the Wegener's granulomatosis (now renamed granulomatosis with polyangiitis, GPA) Etanercept trial, the incidence of VTE in patients with GPA was seven times higher than that of systemic lupus erythematosus and similar to that of patients with recurrent VTE [8]. An increased risk of VTE was also demonstrated in microscopic polyangiitis (MPA) and Eosinophilic Granulomatosis with Poly Angiitis (EGPA) [9].
Association between PAN and VTE is questionable. First evidence comes from case reports, describing patients with thrombosis and PAN, especially when antiphospholipid antibodies were present [10]. Subsequently, a retrospective study based on the French Vasculitis Study Group cohort reviewed the risk of VTE among 1130 patients with AAV (GPA, MPA, EGPA) and PAN during 50 months of median follow-up [9]. The frequency of VTE among the 285 patients with PAN was 2.5% and was significantly lower as compared to that of patients with AAV (0.58 versus 1.84 per 100 person-year, respectively), but higher than that of the general population (0.3 per 100 person-year in the Swedish population). Furthermore, as in AAV, VTE occurred mainly during periods of high disease activity of PAN. Other large population-based studies come to different conclusions. Ramagopalan et al analyzed retrospectively three databases of patients with immunemediated diseases, which were hospitalized in England between 1968 and 2008 [11]. The reference cohort was constituted by hospitalized patients with other diagnoses, mainly minor medical conditions. In all three datasets, an elevated risk of VTE was found for 13 immunemediated diseases, including PAN. That was also confirmed in a large Swedish study by Zöller et al. which investigated the risk of PE among hospitalized patients with 33 immunemediated diseases between 1964 and 2008 [12]. It should be noted, however, both Ramagopalan and Zöller could not distinguish between the current definition of PAN and that used before 1994, in which MPA was considered a variant of PAN. Furthermore, these studies are conducted in hospitalized patients, which are likely not only to have a higher disease activity but also more comorbidities.
Management of vasculitis-associated VTE is challenging since no prospective randomized controlled trials have ever been conducted and most of the evidence comes from retrospective studies in patients with BD. According to the 2018 European League Against Rheumatism (EULAR) recommendations, glucocorticoids and immunosuppressant’s are generally used, while anticoagulants tend to be discouraged, owing to the lower efficacy in preventing BD-associated VTE and the risk of hemorrhage from pulmonary artery aneurysms, which are relatively common in BD [13]. However, anticoagulants seem to reduce the incidence of post-thrombotic syndrome in BD and certain immunosuppressant’s might cause a paradoxical risk of thrombosis through various effects on thrombogenesis [14,15]. Given this, our patient was treated both with immunosuppressive therapy and three-month anticoagulant therapy with heparin.
Conclusion
Despite the declining incidence in various countries, PAN remains a condition not to be forgotten, given the potentially catastrophic consequences in case of delayed diagnosis and treatment. VTE may be a manifestation of this disease, although it seems to occur more rarely than in other vasculitides. Regarding the management of vasculitis-associated VTE, evidence is still lacking and this issue will need to be assessed in prospective randomized controlled trials.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Informed consent for publication of this case report, and any accompanying images, was obtained from the patient.
Competing interests
The authors declare that they have no competing interests.
Funding support
We declare no financial support.
Availability of data and materials
This is a case report of a single patient, to protect privacy and respect confidentiality; none of the raw data has been made available in any public repository. The original reports, laboratory studies, imaging studies and outpatient clinic records are retained as per normal procedure within the medical records of our institution.
Authors' contributions
FB examined the patient and contributed to manuscript conception, preparation, and editing. SB, MR, MD and FF examined the patient and contributed to manuscript conception, preparation and editing. DR performed pathological readings.
References
- Wysokinski WE, Gosk-Bierska I, Greene El et al. Clinical characteristics and long-term follow-up of patients with renal vein thrombosis. Am. J. Kidney. Dis. 51(2), 224–232 (2008).
- Asghar M, Ahmed K, Shan SS et al. Renal vein thrombosis. Eur. J. Endovasc. Surg. 34(2), 217–223 (2007)
- Lightfoot RW Jr, Michel BA, Bloch DA et al. The American College of Rheumatology 1990 criteria for the classification of polyarteritis nodosa. Arthritis. Rheum. 33(8), 1088–1093 (1990).
- Jennette JC, Falk RJ, Bacon PA et al. 2012 Revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis. Rheum. 65(1), 1–11 (2013).
- De Virgilio A, Grego A, Magliulo G et al. Polyarteritis nodosa: A contemporary overview. Autoimm. Rev. 15(6), 564–570 (2016).
- Katz Ob, Brenner B, Horowitz Na. Thrombosis in vasculitic disorders- clinical manifestations, pathogenesis and management. Thromb. Res. 136(3), 504–512 (2015).
- Emmi G, Bettiol A, Silvestri E et al. Vascular Behçet's syndrome: An uptodate. Int. Emerg. Med. 14(5), 645–652 (2019).
- Merkel PA, Lo GH, Holbrook JT et al. Brief communication: high incidence of venous thrombotic events among patients with Wegener granulomatosis: The Wegener's Clinical Occurence of Thrombosis (WeCLOT) Study. Ann. Int. Med. 142(8), 620–626 (2005).
- Allenbach Y, Seror R, Pagnoux C et al. High frequency of venous thromboembolic events in Churg-Strauss syndrome, Wegener's granulomatosis and microscopic polyangiitis but not polyarteritis nodosa: a systematic retrospective study on 1130 patients. Ann. Rheum. Dis. 68(4), 564–567 (2009).
- Han Bk, Inaganti K, Fahmi S et al. Polyarteritis nodosa complicated by catastrophic antiphospholipid syndrome. J. Clin. Rheumatol. 10(4), 210–213 (2004).
- Ramagopalan SV, Wotton CJ, Handel AE et al. Risk of venous thromboembolism in people admitted to hospital with selected immune-mediated diseases: record-linkage study. BMC. Med. 9(1) (2011).
- Zoller B, Li X, Sundquist J et al. Risk of pulmonary embolism in patients with autoimmune disorders: a nation-wide follow-up study from Sweden. Lancet. 379(9812), 244–249 (2012).
- Hatemi G, Christensen R, Bang D et al. 2018 update of the EULAR recommendations for the management of Behçet's disease. Ann. Rheum. Dis. 77(6), 808–818 (2018).
- Silvestri E, Scalera A, Emmi G et al. Thrombosis in Autoimmune Diseases: A Role for Immunosuppressive Treatments? Semin. Thromb. Hemost. 42(6), 650–661 (2016).
- Sonmez He, Armagan B, Ayan G et al. Polyarteritis nodosa: lessons from 25 years of experience. Clin. Exp. Rheumatol. 117(2), 52–56 (2019).