Review Article - Interventional Cardiology (2010) Volume 2, Issue 2
Percutaneous mitral valve repair: an overview of new interventional therapies and associated outcomes
- Corresponding Author:
- Timothy Watson
Green Lane Cardiovascular Service, Auckland City Hospital Park Road, Auckland, New Zealand
Tel:+1 847 570 2250
Fax:+1 847 570 1865
E-mail:tfeldman@northshore.org
Abstract
Keywords
mitral regurgitation, mitral valve repair, structural intervention, valve disease
The discussion regarding outcomes of percutaneous mitral valve repair occurs in the context of a completely novel field of development. The first patients treated with any of the current devices used for catheter-based mitral valve repair therapy underwent implantation in July 2003. It is remarkable that there are any substantial outcome data in the field at this point. The available data will be considered in terms of acute results and early trial experience; and, for percutaneous leaflet repair, we will also consider data from the last several years.
Catheter-based mitral valve repair techniques parallel the approaches that have been used for surgical mitral valve repair for several decades. The first surgical concepts to develop parallels in catheter-based therapy include mitral annuloplasty via either the coronary sinus or directly from retrograde left ventricular access, and leaflet repair using the edge-toedge approach. Most of the percutaneous repair devices for mitral regurgitation (MR) have been modeled on existing surgical approaches. The various percutaneous approaches use the basic concepts of surgical repair, although usually in a novel manner. The majority of surgical mitral repair procedures involve the implantation of an annuloplasty ring. A variety of percutaneous annuloplasty devices have been developed. The basic concept of diminishing the mitral circumferences, and compressing the septal– lateral dimension, is common to this class of devices. A variety of approaches, including leaflet resection, sliding annuloplasty and chordal reimplantation or neochordal instruction have been employed.
All of these percutaneous approaches have been used with enough acute success to demonstrate proof-of-concept. The greatest amount of experience has developed with the Evalve MitraClip® system [1–5]. While leaflet repair may have seemed the most difficult development pathway before any procedures were actually performed, the MitraClip device is the only percutaneous valve therapy at the time of writing to have completed enrollment and 1‑year followup in a pivotal randomized trial in comparison with surgical mitral valve repair. Coronary sinus annuloplasty has been accomplished with several devices. Proof-of-concept has been clear from their ability to reduce MR dramatically in some subjects. The major coronary sinus devices with experience in application in patients include the Viacor Percutaneous Transvenous Mitral Annuloplasty (PTMA®) system (Viacor, MA, USA), the Cardiac Dimensions Carillon™ (Cardiac Dimensions, WA, USA) and the Edwards Monarc™ (Edwards Lifesciences Corp., CA, USA). These devices share a common use of coronary sinus access to encircle the mitral annulus in order to achieve both diminished annular circumference and a decrease in the septal–lateral dimension. The mechanism of action and construction of each of the devices is novel, and thus some of their advantages and limitations are device specific. Future directions include catheter-based chordal repair and percutaneous mitral valve replacement.
Evalve MitraClip® system
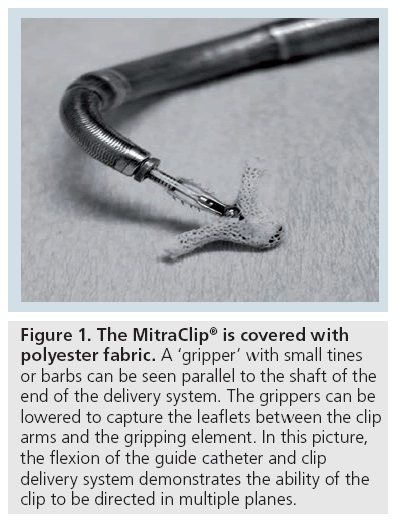
The MitraClip system utilizes a clip with a coaxial catheter system. The tip of the outer guide catheter is delivered to the left atrium utilizing a standard trans-septal approach. The guide catheter is 24-French proximally, and tapers to 22-French at the point where it crosses the atrial septum. A clip delivery system, with a clip attached to its distal end, is passed through the guide catheter (Figure 1). This system is steerable using a two-knob coaxial system that permits medial–lateral and anterior–posterior steering. The clip delivery system is advanced through the guide catheter into the left atrium, and positioned so that the clip is over the mitral valve and the origin of the regurgitant jet. The two arms have an opened span of approximately 2 cm when opened in the grasping position. The width of the clip is 4 mm. Leaflet tissue is secured between the closed arms and each side of the gripper, and the clip is then closed and locked. The procedure is performed under general anesthesia using fluoroscopy and transesophageal echocardiographic guidance. The importance of procedural echocardiographic guidance for this procedure cannot be overemphasized. While most angiographic procedures are fluoroscopically guided, transesophageal echocardiographic guidance is the primary modality for performing this procedure.
Figure 1: The MitraClip® is covered with polyester fabric. A ‘gripper’ with small tines or barbs can be seen parallel to the shaft of the end of the delivery system. The grippers can be lowered to capture the leaflets between the clip arms and the gripping element. In this picture, the flexion of the guide catheter and clip delivery system demonstrates the ability of the clip to be directed in multiple planes.
The guide is positioned in the mid-left atrium, deaired and flushed. The clip delivery system is introduced into the guide catheter, and the clip is advanced into the left atrial chamber. The clip is moved in iterations until it is centered over the mitral orifice. The arms of the clip are opened and oriented perpendicular to the long axis of the leaflet edges, and then the clip is advanced into the left ventricle just below the mitral leaflet edges. The clip is pulled back until the mitral leaflets are captured. The clip is partially closed. At this point, achievement of a double orifice mitral valve, leaflet insertion into the closed clip arms and the degree of MR can be assessed using Doppler echocardiography. Next, the clip is closed incrementally under real time echocardiography to optimize the reduction of MR. If necessary, the clip can be opened, the mitral leaflets released and the clip repositioned. After adequate reduction of MR is achieved, the clip is released from the clip delivery system. A second clip may be placed if needed. Approximately 40% of patients require a second clip. Patients were treated with aspirin 325 mg daily for 6 months, and clopidogrel 75 mg daily for 30 days unless they were already on warfarin.
Leaflet repair with the Evalve MitraClip®
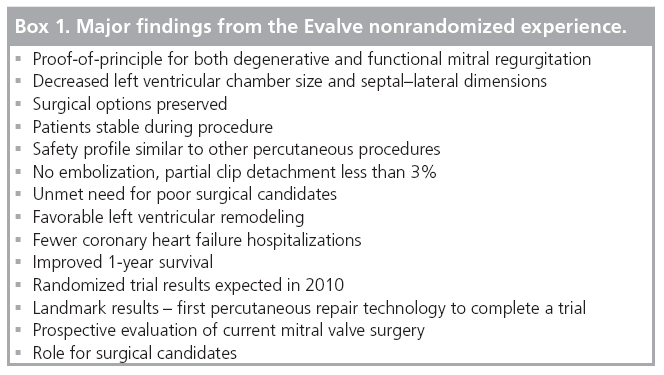
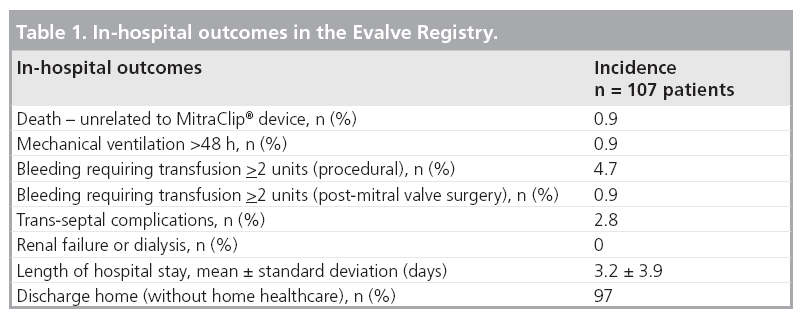
The major findings in the Evalve trial series – the Endovascular Valve Edge-to-Edge Repair (EVEREST) trials – demonstrate proofof- principal for reduction of MR for both degenerative and functional etiologies of MR (Box 1). Several major points are clear based on the experience gained in the Evalve nonrandomized patients [3,4]. Decreased left ventricular chamber size and septal–lateral dimensions have been found in high-risk patients and those with initially dilated ventricles. Surgical options are preserved. Patients can undergo surgical repair following attempted clip procedures when no clip is placed, as well as after placement of a clip with recurrent MR [6]. Successful surgical repair has been performed up to several years after a clip was placed. Patients are stable during procedure and there have not been any problems with hypotension or arrhythmias during procedures that may last up to several hours. The safety profile is similar to other percutaneous procedures, with transfusion from vascular access representing the most frequent acute problem (Table 1). No clip embolization has occurred. Partial clip detachment with loss of capture of a single leaflet is the main procedural problem, with an incidence of less than 3%. The procedure clearly fills an unmet need for poor surgical candidates. In these higher surgical risk cases, favorable left ventricular remodeling, fewer congestive heart failure hospitalizations and improved 1‑year survival compared with matched controls has been observed. The results of the MitraClip system are closely related to the selection criteria of enrolled subjects, thus the proportion of eligible patients from the broad pool of the MR population remains to be determined.
The randomized trial data will be available over the next several months. This is the first percutaneous valve technology to complete a randomized trial. It will also be the first prospective evaluation of current mitral valve surgery using core laboratories to evaluate results. The randomized trial will define the role of this new therapy for typical surgical candidates.
Patient selection
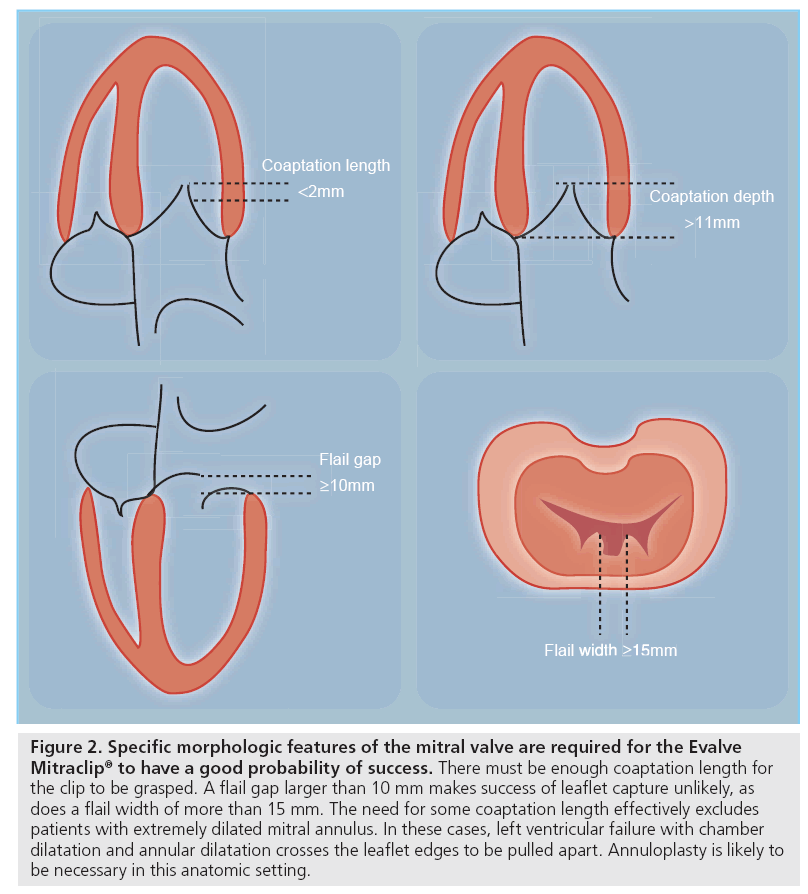
Selection of patients for percutaneous mitral repair is clearly related to candidacy for surgical repair. Percutaneous repair patients might be excellent surgical candidates but they may prefer a less morbid, although less established, percutaneous approach. Percutaneous therapy might have a better role in patients for whom medical therapy has been the alternative to surgical therapy, either because the risk for surgery has been too high, or where the MR has not been severe enough to warrant surgery. The primary concerns are the risk–benefits of percutaneous therapy itself, with the realization that surgical backup may not be an option for the high-risk patient if things go wrong or a good result is not achieved. Finally, percutaneous repair may be a reasonable option in patients who are candidates for surgical repair, but in whom surgical risk and morbidity are high; as long as experience with percutaneous therapy remains of limited duration, elderly patients or patients with limited life expectancy may fall into the this latter group. Anatomic features also play an important role in patient selection (Figure 2). Specific leaflet morphologic features are required for therapy with the MitraClip to be likely to succeed. Importantly, these anatomic features are independent of the etiology of MR, with both functional and degenerative etiologies having successful outcomes in the Evalve registry experience. After successful initial treatment, the 3-year freedom from need for additional surgery has been approximately 80%.
Figure 2: Specific morphologic features of the mitral valve are required for the Evalve Mitraclip® to have a good probability of success. There must be enough coaptation length for the clip to be grasped. A flail gap larger than 10 mm makes success of leaflet capture unlikely, as does a flail width of more than 15 mm. The need for some coaptation length effectively excludes patients with extremely dilated mitral annulus. In these cases, left ventricular failure with chamber dilatation and annular dilatation crosses the leaflet edges to be pulled apart. Annuloplasty is likely to be necessary in this anatomic setting.
Coronary sinus annuloplasty
The primary indication for coronary sinus devices is for treatment of functional MR arising from annular dilatation or deformation. The parallel course of the coronary sinus and the mitral annulus have led to a variety of device concepts to utilize this pathway to encircle and constrain the coronary sinus. The obvious advantage of this approach is the simplicity of access via the venous system and the ability to deliver a device in the beating heart. The fundamental assumption is that the coronary sinus encircles the mitral annulus to a great enough degree to allow for circumferential cinching and diminution of the mitral orifice [7–9]. The degree to which the coronary sinus parallels the mitral annulus is critical. The main concept of coronary sinus annuloplasty is improving mitral leaflet coaptation in functional MR. Numerous studies involving primarily computed tomography approaches have demonstrated significant variability in the degree to which the coronary sinus does in fact parallel the mitral annulus. Angulation of the coronary sinus may move it away from the mitral annulus in many patients. The typical distance is approximately 1 cm. In addition, the coronary sinus resides in a fat pad, and the potential for energy applied by a coronary sinus device to dissipate over time is a theoretical consideration.
The most important anatomic finding in both the computed tomography studies of coronary sinus anatomy and in the practical experience with this category of devices, is the fact that the coronary sinus crosses over the circumflex trunk or a branch of the circumflex coronary artery in somewhere between two thirds and three quarters of patients [7–9]. The degree to which coronary compression might limit patients’ selection is an important consideration. Some cases of myocardial infarction and coronary compression have occurred in the early device experience with this category of devices, and the need to screen patients carefully for this anatomic relationship has had an important impact on the utilization of this class of device therapy. Implant rates for this group of devices have been limited to approximately two in every three of patients owing to either circumflex compression or challenging coronary sinus anatomy. Increasingly careful patient selection using preprocedure computed tomographic angiograms may be helpful.
There are three devices with some human implant experience utilizing the coronary sinus route. These include the Edwards Monarc, Cardiac Dimensions Carillon and the Viacor PTMA systems [10–24]. The Edwards Monarc device is comprised of self-expanding stents at either end of a spring-like bridge element. The distal stent is implanted via jugular venous access in the anterior interventricular vein, and the proximal stent is implanted in the coronary sinus ostium. The spring element is held in an open, elongated configuration by bioabsorbable material in the interstices of the spring. This degrades over a period of several weeks, allowing the sling to contract, placing tension on the coronary sinus. Thus, the diminution of MR does not occur at the time of implantation and the degree of MR reduction cannot be known until at least several weeks have passed. The experience with this device in Phase I trials has clearly demonstrated that MR can be diminished. A majority of patients have a decrease in one grade of MR severity, and greater reductions are possible. Clinical improvement has been demonstrated in those patients with improved MR. Several patients have had myocardial infarction from coronary compression, and this has led to a careful screening approach with CT angiography to demonstrate the relationship of the coronary sinus and to the coronary arteries prior to treatment.
Another important finding with the Monarc device was the degree to which the coronary sinus geometry imposes important stress on coronary sinus devices. In the first generation of the Monarc device, three out of five patients experienced fracture of the bridge element attachment to stent after several months. A redesign to make the connections of the bridge to the stent more robust led to better durability, but several fractures occurred months after implantation in the second-generation device. The third generation device is in testing.
The Viacor PTMA system uses a novel approach to deliver compression to the septal lateral dimension of the mitral orifice. A trilumen plastic cannula is placed via subclavian venous puncture and used to access the coronary sinus. Nitinol rods of varying stiffness can be passed into the cannula to compress the lateral aspect of the mitral annulus through the coronary sinus, leading to compression of the regurgitant mitral orifice. Clear proof-of-principle has been demonstrated with patients showing sustained compression of the mitral annulus for over 1 year. The approach has required significant development to create a family of Nitinol rods that will create adequate compression of the coronary sinus. Among the advantages of this approach is the ability to remove rods if the efficacy of the device is insufficient, or over a period of many months or even potentially years, to replace rods with rods of greater stiffness if the degree of MR worsens. The Phase I trial has been carried out in a small number of patients, and ongoing experience and larger Phase I trials are anticipated. As was the case with the Monarc device, metal fatigue with fracture of the nitinol rods occurred in the first generation of the Viacor PTMA device. Redesign appears to have improved this limitation significantly. The fact that the Viacor system mostly engages the lateral aspect of the coronary sinus should, in theory, lead to less of an issue with coronary compression, although the circumflex branches may still interfere with the mechanism of this device. The Viacor device is unique in that rather than encircling the mitral annulus, the major force is to compress the septal lateral dimension. Thus, the reduction of the regurgitant orifice occurs without cinching of the annular circumference.
The Cardiac Dimensions Carillon device has had investigational use in several nonrandomized studies. This device is also implanted via jugular access for the coronary sinus with anchors for the distal coronary sinus and coronary sinus ostium connected by a rigid nickel titanium bridge element. The mechanism of tension on the coronary sinus circumference is applied by directly pulling back on the catheter after the distal anchor is placed, tensioning the coronary sinus so that when the proximal anchor is delivered, the tension is maintained.
The first generation of Carillon had difficulty with anchoring – a redesign solved this problem. Several instances of metal fatigue with fracture of the attachment of the bridge element to one of the anchors had also occurred with the Carillon. A review of all safety data by the Data and Safety Monitoring Board for the trials confirmed that there was no link between wireform break and adverse events. Interestingly, the efficacy data showed improved or maintained reductions in MR with broken wireforms. Since preclinical histology data demonstrate that the process of device endothelialization is apparent at 1 month, it is possible that maintenance of clinical efficacy is due to encapsulation of the device within the venous endothelium. Study of the cine images from both studies was used to model the observed geometric displacements in mechanical fatigue testing systems. A new fatigue test replicated the wireform fracture observed in the clinical setting. The testing has led to implementation of a device modification with improved wireform fatigue characteristics.
The device can be placed with direct angiographic control of the relationship of the circumflex artery to the coronary sinus. Thus, when coronary compression is observed, the device may be repositioned to relieve coronary sinus encroachment, or it can be removed. The advantage of the complete removability of the device allows for decision-making regarding placement to occur during the cardiac catheterization procedure. The reported experience in the Amadeus trial has demonstrated that efficacy may be achieved with the device. In a cohort of 48 patients, 30 were implanted with the device. Reasons for not receiving the device were problems with coronary sinus access, insufficient reduction of the MR acutely or coronary artery compromise. Most of the patients had between 20 and 30% reductions and quantitative measures of MR. Importantly, the 6-minwalk test distance improved significantly in this group, as did the quality of life measured by standard cardiomyopathy questionnaire methods. A more recent experience with 20 implanted patients amplified these results, demonstrating improved measures of MR, left ventricular dimension, quality of life and 6-min-walk test duration. Broadly, for the class of coronary sinus devices, coronary compression is an important limiting factor, and generally must be assessed both before and during device implantation. MR reduction is in the range of a 1+ decrease in the majority of patients, with a significant number of patients having 2+ reductions. Experiences with three of the coronary sinus annuloplasty devices, approximately two-thirds of intended patients underwent device implantation. The observation that 138 out of 216 attempted implants to date have been successful is important: 11 out of 31 attempted implants have been successful for the PTMA device; 59 out of 72 implants for the Monarc device; and 66 out of 119 for the Carillon device [25], the main reason for a failed attempt being patient anatomy. The progress in this area has been steady, and at this point the target population appears to be patients with heart failure due to MR as an alternative to medical therapy, rather than as a device approach that might be compared in head-to-head trials with surgical mitral valve repair or replacement.
Direct annuloplasty
Direct annuloplasty approaches, also primarily indicated for treating functional MR arising from annular dilatation or deformation, have been modeled after suture annuloplasty [17]. Suture annuloplasty was one of the first ever mitral repair techniques described in the late 1950s, and has since been employed successfully in several surgical series. Circumferential sutures are placed around the mitral annulus and tethered together in a manner analogous to the drawstring of scrub pants. Two efforts to create tethering of the mitral annulus by direct device implantation have moved forward in preclinical and first-inman experiences. Mitralign, Inc. (MA, USA) has developed a system that involves retrograde transaortic access to the left ventricle with placement of a guide catheter between the papillary muscles and into the space directly beneath the mid-posterior mitral leaflet. The guide catheter is in close proximity to the annulus. Radiofrequency wires are used to drive through the mitral annulus and into the left atrium. Four pledgets are anchored on the left atrial side of the annulus and connected with a drawstring that can be used to plicate the annulus. The initial device designed involves a three-arm delivery catheter – the ‘Trident’ – and further refinements in the device have utilized a ‘Bident’ delivery system to place two pairs of pledgets in the annulus and achieve a greater portion of the annular circumference that can be tethered. The various components of the procedure have been successfully employed in first-in-man studies. The second system to use a direct annuloplasty approach is from the guided delivery systems. Nine to 12 nitinol clips are placed in the mitral annulus connecting a string that is tethered to cinch the annulus and decrease the mitral circumference.
This system is being used for intraoperative implants and early clinical trials are under development. Both of these approaches avoid compression of the circumflex vessels because they are intra- rather than extra-cardiac in terms of the delivery of force. They have the additional advantage of encircling the greater part of the mitral circumference with the potential for greater reductions in MR that might be achieved by coronary sinus methods.
Comparisons with surgical methods
To date, only one trial of the Evalve device has been randomized, with a comparison of the device to surgical mitral valve repair or replacement. Retrospective comparisons of these devices to established surgical techniques are not possible, especially since the treated populations with percutaneous therapies differ substantially from surgical historical controls. There have never been controlled trials of surgical approaches, and nonrandomized propensity matched evaluations of surgical therapy for mitral valve repair for ischemic and heart failure-related functional MR have not clearly demonstrated benefits for surgical therapy [26,27]. Thus, the development of percutaneous therapies will continue with the careful scrutiny of prospective trials. The use of core laboratories for evaluation of echocardiographic inclusion criteria for therapy, and events committees for the adjudicator outcomes for these trials will provide clear guidance for the development of percutaneous therapies moving forward.
From many of these novel therapies, comparisons will be made with medical therapy rather than with surgery. Annuloplasty devices are likely to be employed in heart failure patients currently rarely treated with surgery for MR. The importance of residual MR after percutaneous therapy will be defined by clinical outcomes. While 2+ residual MR has been observed after some Evalve procedures, decreased left ventricular chamber dimensions after 1 year suggest the impact of MR reduction is significant. The degree to which residual MR impacts late outcome with percutaneous therapies will become clear with long-term follow-up.
Conclusion
Percutaneous mitral repair technologies are developing steadily. Leaf let repair with the MitraClip has progressed farthest, having completed a substantial registry experience and a randomized clinical trial. The proof-of-principal for both degenerative and functional MR has been demonstrated with the MitraClip. Indirect annuloplasty via the coronary sinus is developing more slowly. The challenges of device stability and device fracture in the coronary sinus, and the potential for compression of the circumflex coronary artery are being addressed. Direct annuloplasty methods may overcome some of the limitations of coronary sinus annuloplasty, but are only at the first-in-man stage. Percutaneous mitral valve replacement is on the far horizon.
Future perspective
A variety of novel devices are on the far horizon of development [28–33]. One recent concept that was applied in a surgical cohort and in several percutaneous cases was the Myocor Coapsys system. This device utilized a tether passed through the left ventricle to compress both the left ventricular chamber and the septal–lateral dimension of the mitral annulus. This is the first mitral annuloplasty device to address both the annulus and the dilated left ventricle. The ventricle is the genesis of MR in functional MR, and standard surgical annuloplasty and percutaneous annuloplasty do not address this fundamental problem. The Myocor device demonstrated promise in the early surgical experience, but the company ran out of funding in the global financial crisis and no longer exists. Hopefully, this line of therapy will eventually continue to develop. Chordal replacement of another novel concept, which is being developed for a beating heart surgical approach, used transapical access. The potential to use catheter methods to repair or replace chordae tendineae is an exciting future avenue for further study.
Mitral valve replacement is also under development using percutaneous approaches. In comparison with the aortic valve, the mitral valve orifice is much larger, and the challenges of fixation of the prosthesis are significantly greater. One limitation that is favorable for the mitral field is that access can be transvenous and transseptal, which places less demand on the development of a low-profile device than would arterial delivery. The potential to completely eliminate MR using valve replacement may develop into an attractive option for patients who are currently treated surgically or who might be at high risk for surgery.
Financial & competing interests disclosure
The author has no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties. No writing assistance was utilized in the production of this manuscript.
Executive summary
▪ Catheter-based mitral valve repair techniques parallel the approaches that have been used for surgical mitral valve repair for several decades.
▪ Leaflet repair and annuloplasty are the major catheter approaches to mitral repair.
▪ All the percutaneous devices for mitral vale repair are still investigational.
Evalve MitraClip® system
▪ The clip is moved in the left atrium until it is centered over the mitral orifice and used to grasp the leaflets to create a double orifice.
▪ Trial experience to date demonstrate proof-of-principal for reduction of mitral regurgitation (MR) for both degenerative and functional etiologies of MR.
▪ Randomized trial data compared with conventional surgery will be available over the next several months.
▪ This is the first percutaneous valve technology to complete a randomized trial.
Coronary sinus annuloplasty
▪ The parallel course of the coronary sinus and the mitral annulus have led to a variety of device concepts to utilize this pathway to encircle and constrain the coronary sinus.
▪ The coronary sinus crosses over the circumflex trunk or a branch of the circumflex coronary artery in two-thirds to three-quarters of patients, which limits the application of this technology.
▪ The primary indication for coronary sinus devices is for treatment of functional MR arising from annular dilatation or deformation associated with heart failure.
▪ These devices may be an alternative to medical therapy for coronary heart failure.
Direct annuloplasty
▪ Direct annuloplasty approaches are also primarily indicated for treating functional MR arising from annular dilatation or deformation.
▪ Circumferential anchors are placed around the mitral annulus and tethered together.
▪ Compared with coronary sinus annuloplasty, direct annuloplasty has the advantage of encircling a greater part of the mitral circumference and not overlapping the circumflex coronary artery.
Comparisons with surgical methods
▪ To date, only one trial of the Evalve device has been randomized, with a comparison of a device to surgical mitral valve repair or replacement.
▪ Retrospective comparisons of these devices to established surgical techniques are not possible, especially since the treated populations with percutaneous therapies differ substantially from surgical historical controls.
▪ From many of these novel therapies, comparisons will be made with medical therapy rather than with surgery.
Future perspective
▪ All of the percutaneous MR therapies are undergoing clinical trial evaluation.
▪ Novel approaches such as chordal replacement and percutaneous mitral valve replacement are on the horizon.
References
Papers of special note have been highlighted as:
▪ of interest
- Alfieri O, Maisano F, De Bonis M et al.: The double-orifice technique in mitral valve repair: a simple solution for complex problems. J. Thorac. Cardiovasc. Surg. 122(4), 674–681 (2001).
- Maisano F, Caldarola A, Blasio A, De Bonis M, La Canna G, Alfieri O: Midterm results of edge-to-edge mitral valve repair without annuloplasty. J. Thorac. Cardiovasc. Surg. 126, 1987–1997 (2003).
- Feldman T, Kar S, Rinaldi M et al.: Percutaneous mitral repair with the MitraClip® system: safety and didterm durability in the initial EVEREST cohort. J. Am. Coll. Cardiol. 54, 686–694 (2009).
- Feldman T, Wasserman HS, Herrmann HC et al.: Percutaneous mitral valve repair using the edge-to-edge technique: six-month results of the EVEREST Phase I clinical trial. J. Am. Coll. Cardiol. 46(11), 2134–2134 (2005).
- Silvestry S, Rodriguez L, Herrmann H et al.: Echocardiographic guidance and assessment of percutaneous repair for MR with the Evalve MitraClip: lessons learned from EVEREST I. J. Am. Soc. Echo. 20, 1131–1140 (2007).
- Dang NC, Aboodi MS, Sakaguchi T et al.: Surgical revision after percutaneous mitral valve repair with a clip: initial multi-center experience. Ann. Thor. Surg. 80(6), 2338–2342 (2005).
- Choure A, Garcia M, Hesse B et al.: In vivo analysis of the anatomical relationship of coronary sinus to mitral annulus and left circumflex coronary artery using cardiac multidetector computed tomography: implications for percutaneous coronary sinus mitral annuloplasty. J. Am. Coll. Cardiol. 48, 1938–1945 (2006).
- Tops L, Van de Veire N, Schuifj J et al.: Noninvasive evaluation of coronary sinus anatomy and its relation to the mitral valve annulus: implications for percutaneous mitral annuloplasty. Circulation 115, 1426–1432 (2007).
- Goitein O, Lacomis J, Gorcsan J III, Schwartzman D: Left ventricular pacing lead implantation: potential utility of multimodal image integration. Heart Rhythm 3, 91–94 (2006).
- Lansac E, Di Centa I, Attar NA, Messika-Zeitoun D, Raffoul R, Vahanian A: Percutaneous mitral annuloplasty through the coronary sinus: an anatomical point of view. J. Thorac. Cardiovasc. Surg. 8, 376–381 (2007).
- Webb JG, Harnek J, Munt BI et al.: Percutaneous transvenous mitral annuloplasty; initial human experience with device implantation in the coronary sinus. Circulation 113, 851–855 (2006).
- Kuck K, Webb JG, Harnek J et al.: Percutaneous treatment of functional mitral regurgitation: interim evolution study results with the Monarc system. Am. J. Cardiol. 100, L58 (2007).
- Dubreuil O, Basmadjian A, Ducharme A et al.: Percutaneous mitral valve annuloplasty for ischemic mitral regurgitation: first in man experience with a temporary implant. Catheter Cardiovasc. Interv. 69, 1053–1061 (2007).
- Feldman T: Percutaneous mitral annuloplasty: not always a cinch. Catheter Cardiovasc. Interv. 69, 1062–1063 (2007).
- Byrne MJ, Kaye DM, Mathis M et al.: Percutaneous mitral annular reduction provides continued benefit in an ovine model of dilated cardiomyopathy. Circulation 110, 3088–3092 (2004).
- Maniu CV, Patel JB, Reuter DG et al.: Acute and chronic reduction of functional mitral regurgitation in experimental heart failure by percutaneous mitral annuloplasty. J. Am. Coll. Cardiol. 44, 1652–1661 (2004).
- Nagy ZL, Peterffy A: Mitral annuloplasty with a suture technique. Eur. J. Cardiothorac. Surg. 18(6), 739–741 (2000).
- Heuser RR, Witzel T, Dickens D, Takeda PA: Percutaneous treatment for mitral regurgitation: the QuantumCor system. J. Interv. Cardiol. 21, 178–182 (2008).
- Schofer J, Siminiak T, Haude M et al.: Percutaneous mitral annuloplasty for functional mitral regurgitation: results of the AMADEUS trial. Circulation 120, 326–333 (2009).
- Sack S, Kahlert P, Bilodeau L et al.: Percutaneous transvenous mitral annuloplasty: initial human experience with a novel coronary sinus implant device. Circ. Cardiovasc. Interv. 2, 277–284 (2009).
- Daimon M, Gillinov A, Liddicoat J et al.: Dynamic change in mitral annular area and motion during percutaneous mitral annuloplasty for ischemic mitral regurgitation: preliminary animal study with real-time 3-dimensional echocardiography. J. Am. Soc. Echocardiogr. 20: 381–388 (2007).
- Dubreuil O, Basmadjian A, Ducharme A et al.: Percutaneous mitral valve annuloplasty for ischemic mitral regurgitation: first in man experience with a temporary implant. Catheter Cardiovasc. Interv. 69, 1053–1061 (2007).
- Webb J, Harnek J, Munt B et al.: Percutaneous transvenous mitral annuloplasty: initial human experience with device implantation in the coronary sinus. Circulation 113, 851–855 (2006).
- Tubler T: Initial experience with the cardiac dimensions device (CARILLON). Presented at: The Catheter Interventions in Congenital and Structural Heart Disease, 99th International Workshop. Frankfurt, Germany, 8–10 June, 2005.
- Feldman T: The Epidemiology and Treatment Patterns of Patients with Mitral Regurgitation. Presented at: Transcatheter Cardiovascular Therapeutics (TCT 2009) 21st Annual Scientific Symposium. San Francisco, CA, USA, 21–25 September, 2009.
- Wu AH, Aaronson AD, Bolling SF, Pagani FD, Welch K, Koelling TM: Impact of mitral annuloplasty on mortality risk with MR and LV systolic dysfunction. J. Am. Coll. Cardiol. 45, 381–387 (2005).
- Mihaljevic T, Lam BK, Rajeswaran J et al.: Impact of mitral valve annuloplasty combined with revascularization in patients with functional ischemic mitral regurgitation J. Am. Coll. Cardiol. 49, 2191–2201 (2007).
- Grossi EA, Goldberg JD, LaPietra A et al.: Ischemic mitral valve reconstruction and replacement: comparison of long-term survival and complications. J. Thorac. Cardiovasc. Surg. 122(6), 1107–1124 (2001).
- Grossi E, Woo Y, Schwartz C et al.: Comparison of coapsys annuloplasty and internal reduction mitral annuloplasty in the randomized treatment of functional ischemic mitral regurgitation: impact on the left ventricle. J. Thorac. Cardiovasc. Surg. 131, 1095–1098 (2006).
- Grossi EA, Saunders PC, Woo YJ et al.: Intraoperative effects of the coapsys annuloplasty system in a randomized evaluation (RESTOR-MV) of functional ischemic mitral regurgitation. Ann. Thorac. Surg. 80(5), 1706–1711 (2005).
- Pedersen WR, Block PC, Feldman TE: The iCoapsys Repair System for the percutaneous treatment of functional mitral insufficiency. Eurointervention 1(Suppl. A), A44–A48 (2006).
- Pedersen WR, Block P, Leon M et al.: iCoapsys mitral valve repair system: Percutaneous implantation in an animal model. Catheter Cardiovasc. Interv. 72, 125–131 (2008).
- Rogers JH, Macoviak JA, David A et al.: Percutaneous septal sinus shortening: a novel procedure for the treatment of functional mitral regurgitation. Circulation 113, 2329–2334 (2006).
▪ Details the results of the initial human experience with the Evalve MitraClip®.
▪ Review of the echo assessment and procedure guidance for the Evalve procedure.
▪ Details the relationship between the coronary sinus and the circumflex coronary artery; important for understanding the limitations of coronary sinus annuloplasty.
▪ Provides an understanding of coronary sinus annuloplasty.