Research Article - Interventional Cardiology (2025)
Multicenter Comparison of AI Deep Learning Reconstruction, Iterative Reconstruction, and Filtered Back Projection for Coronary Artery Calcification Scoring
- Corresponding Author:
- Mark L. Winkler
Department of Radiology, Steinberg Diagnostic Medical Imaging, Las Vegas, Nevada, United States of America,
E-mail: mlwlv@cox.net
Received date: 30-Aug-2025, Manuscript No. FMIC-25-170555; Editor assigned: 01-Sep-2025, PreQC No. FMIC-25-170555 (PQ); Reviewed date: 15-Sep-2025, QC No. FMIC-25-170555; Revised date: 22-Sep-2025, Manuscript No. FMIC-25-170555 (R); Published date: 29-Sep-2025, DOI: 10.37532/1755-5310.2025.17(S28).719
Abstract
Objective: To validate the feasibility of AI Deep Learning Reconstruction for Coronary Artery Calcification Scoring in order to decrease radiation exposure on a 4 cm detector CT scanner. This is the first such validation on devices that are most commonly utilized for this procedure. Methods: Data from 105 consecutive patients referred for Coronary Artery Calcification Scoring (CACS) in 4 centers was reconstructed with Filtered Back Projection (FBP), Iterative Reconstruction (Hybrid-IR), and AI Deep Learning Reconstruction (AI DLR), and analyzed both quantitatively and qualitatively to determine if AI DLR can be routinely used for this purpose. Additional phantom testing was performed to determine if further dose reduction can be accomplished with AI DLR while maintaining or improving image quality compared to current Hybrid IR reconstruction. Results: Quantitively, there was excellent agreement between the three reconstructions (FBP, Hybrid IR and AI DLR) with an interclass coefficient of 0.99. The mean CACS for filtered back projection reconstructions was 111.05. The mean CACS for Hybrid IR was 91.30. The mean CACS for AI Deep Learning Reconstructions was 93.50. Qualitatively, image quality was consistently better with AI DLR than with Hybrid IR at both soft tissue and lung windowing. Based on our phantom experiments, AI DLR allows for dose reduction of at least a 37% without any image quality penalty compared to Hybrid-IR. Conclusion: The use of AI DLR for use in CACS on 4 cm coverage CT scanner has been quantitatively and qualitatively validated for use for the first time. AI DLR produces qualitatively and quantitively better image quality than Hybrid-IR at the same dose level, and produces good agreement in categorization of Agatston scores. In vivo and in vitro evaluations show that AI DLR will allow for an at least a 37% further dose reduction on a 4 cm coverage CT scanner.
Keywords
Coronary artery disease • Risk assessment • Deep learning reconstruction • Iterative reconstruction • Coronary artery calcium scoring • Radiation dose reduction
Introduction
Coronary Artery Calcium Scoring (CACS) is a widely available, low cost, noninvasive imaging test which measures the amount of calcified plaque in the coronary arteries. This score is utilized to assess the risk of coronary artery disease, guide lifestyle modification and therapeutic treatment, and monitor disease progression and response to treatment [1-3]. A patient’s level of CACS may be described by the Agaston score based on a low-dose CT scan of the heart. The Agaston score quantifies the amount of calcified plaque in the coronary arteries. Each calcified plaque is given a score calculated by multiplying the area of the calcified plaque by a scale factor determined by maximum density of the plaque [4,5]. The patient score is a sum of all individual plaque scores.
A score of 0 indicates no identifiable calcified plaque and indicates a very low (less than 5%) risk of significant obstructive CAD. A score of 1-10 indicates minimal calcified plaque and indicates a low (less than 10%) risk of significant obstructive CAD. A score of 11-100 indicates mild calcified plaque and indicates a low to moderate risk of significant obstructive CAD with mild stenosis likely present. A score of 101-400 indicates moderate calcified plaque and indicates a moderate to high risk of significant obstructive CAD with nonobstructive and obstructive disease likely present. A score of over 400 indicates severe diffuse calcified plaque and indicates a high risk of CAD with at least one significant obstruction (greater than 90%) likely present [6]. CACS may be associated with a significant radiation dose, ranging from 0.8 to 10.5mSv [7]. Such radiation doses have been associated with the risks of subsequent tumors [8-11] and therefore minimization of dose is of paramount importance.
The CACS CT test may be reconstructed with a variety of methods. Hybrid-IR has been proven to provide lower doses [12- 17] and higher image quality [18,19] than earlier FBP methods. A previous study with a phantom and human subjects scanned with a wide area detector scanner (16 cm) found that DLR significantly reduced image noise but produced no significant differences in measured calcium volumes. In this study quantification of coronary artery calcium was equivalent between FBP, Hybrid-IR and AI-DLR, with AI-DLR having the lowest bias in measured calcium volumes [20]. This study attempts to determine if DLR can supplant Hybrid-IR to then allow for further dose reduction and improved safety, as suggested in prior studies [21], on nonwide area detector CT scanner.
Materials and Methods
105 consecutive patients referred for CACS in 4 outpatient centers between March 3, 2024, and June 18, 2024, were studied as part of our institution’s routine quality improvement process. There were 57 males and 48 females. CACS studies were performed on CT scanners with 80 row, 4 cm detectors (Prime SP, Canon Medical Systems [93 patients] and Serve SP, Canon Medical Systems [12 patients]). Studies were cardiac gated with a step and shoot technique at a rotation time of 0.35s. Tube voltage was 120 kV for all studies. Data was acquired at 0.5mm slice thickness and reconstruction at a 3mm slice thickness.
Automated exposure control was set to a standard deviation of the noise target of 45 (SD=45) based on the Hybrid-IR model at a 3mm reconstructed slice thickness. This standard deviation level was selected from our prior clinical testing as the level at which non-obese (BMI under 30 kg/m2) patients would be exposed to a dose under 1 mSv for their CACS exam.
Scanning was performed from 1.5 cm above the coronary arteries to 1.5 cm below the left ventricle. Determination of the scan range was assisted by an optical patient positioning system and a low dose 3D localizing scan. Data was reconstructed utilizing three methods: Filtered Back Projection, Hybrid-IR (AIDR, Standard Level), and AI Deep Learning Reconstruction (AiCE, Standard Level). Dose was calculated as the product of Dose Length Product multiplied by the Chest k factor of 0.014 as specified by American Association of Physicists in Medicine report of January 2008 [22]. Quantitative and qualitative CACS was performed by two experienced cardiac imagers with a combined total of 41 years of cardiac imaging experience. A Vitrea workstation (Vitrea Advanced Visualization, Canon Medical Systems) was used to generate the agaston scores.
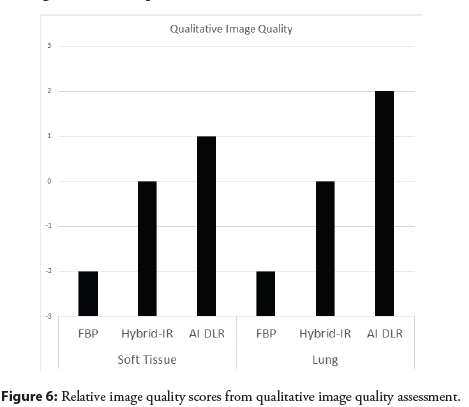
A qualitative image quality assessment of reconstruction algorithms was done using a soft tissue (L40, W350) and lung (L-650, W1600) window settings. The relative change in image quality was done using a ± 3 scale, with 0 being no clinical diagnostic difference, ± 1 being mild clinical diagnostic difference, ± 2 being moderate clinical diagnostic difference, and ± 3 being significant clinical diagnostic difference with the Hybrid-IR image quality set as the reference level of zero.
Phantom scans to evaluate the effects of the reconstruction algorithm on radiation dose and image noise were performed using a Ccatphan 500 phantom (Phantom Laboratory, Salem, NY, USA). To evaluate the dose reduction that could be achieved by changing the reconstruction method for a fixed noise target, scans were performed with noise targets ranging from SD=10 to SD=60. The phantom was scanned and scan doses recorded with Hybrid-IR set as the reconstruction method and repeated with AI DLR set as the reconstruction method.
To quantitively evaluate the noise levels produced by each reconstruction method, images from all scans were reconstructed with FBP, Hybrid-IR and AI DLR. Image noise was measured at the central three slices of the uniformity section of the phantom, using a circular ROI approximately 100 cm2 in size at the center of the image. These measurements provide a quantitative assessment of noise of each reconstruction method at a fixed scan dose, as well as indicators of potential dose reductions at fixed levels of image noise.
Since the data did not follow a normal gaussian distribution the interclass coefficient measure was used to evaluate the agreement between the three different reconstructions. The Fleiss Kappa statistic (κ) was calculated to evaluate the agreement of AI-DLR and FBP with the standard of care reconstruction (Hybrid-IR) [23].
Results
Quantitative
Patient ages ranged from 27 to 77 with a mean age of 55.7 years. Body Mass Indices (BMI) ranged from 16.7 to 39.5 with a mean of 27.5 kg/m2.
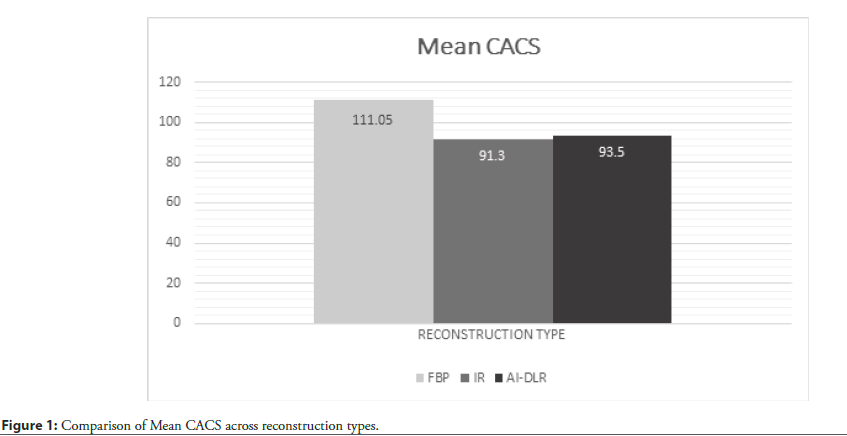
The mean CACS for filtered back projection reconstructions was 111.05. The mean CACS for Hybrid-IR was 91.30. The mean CACS for AI deep learning reconstructions was 93.50 (Figure 1).
All reconstructions FBP, Hybrid-IR and AI-DLR were tested for normality and had D values of 0.3573, 0.3681 and 0.3610 and P<0.0001 which rejects normality of this data. Therefore, an interclass correlation coefficient, which describes the degrees of consistency among measurements, was calculated and found to be 0.99 for the average measures for all 3 reconstructions. This indicates excellent agreement between measurements obtained using the 3 reconstruction methods.
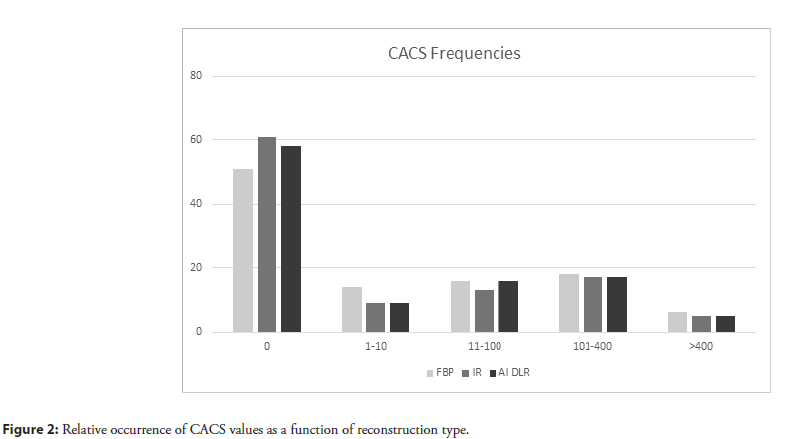
Figure 2 shows the distribution of CACS in each of the risk categories. No coronary calcification (score 0) was seen for 51 patients with FBP, 61 patients with Hybrid-IR, and 58 patients with AI DLR (Figure 2). The kappa statistic (κ) between those patients who were in the CACS category of 0 for AI DLR and Hybrid-IR was 0.94 ± 0.03 while the κ between Hybrid IR and FBP was 0.81 ± 0.05. The two reconstructions (AI DLR and FBP) show strong agreement with Hybrid for those patients with zero calcium.
Minimal coronary calcification (score 1-10) was seen for 14 patients with FBP, 9 patients with Hybrid-IR, and 9 patients with AI DLR. The kappa statistic (κ) for AI DL and Hybrid IR was 0.64 ± 0.14 while, the κ between Hybrid IR and FBP was only 0.27 ± 0.14.
Mild coronary calcification (score 11-100) was seen for 16 patients with FBP, 13 patients with Hybrid-IR, and 16 patients with AI DLR. The kappa statistic (κ) for those patients in the mild coronary calcification category between AI DLR and Hybrid-IR was 0.80 ± 0.09, which is a strong agreement while κ between Hybrid IR and FBP was 0.72 ± 0.1.
Moderate coronary calcification (score 101-400) was seen for 18 patients with FBP, 17 patients with Hybrid-IR, and 17 patients with AI DLR. The kappa statistic (κ) for those patients in the moderate coronary calcification category between AI DLR and Hybrid-IR was 0.92 ± 0.05, which is still strong agreement while κ between Hybrid IR and FBP was 0.90 ± 0.06.
Severe coronary calcification (score over 400) was seen for 6 patients with FBP, 5 patients with Hybrid-IR, and 5 patients with AI DLR. The kappa statistic (κ between AI DLR and Hybrid-IR was 1.0 ± 0.0, which is strong agreement while the κ between Hybrid IR and FBP was 0.9 ± 0.09.
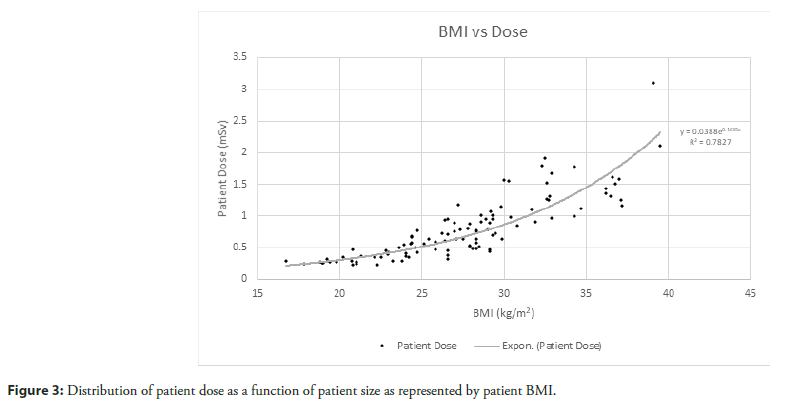
Patient dose was exponentially related to BMI by linear regression analysis and is demonstrated graphically in Figure 3 with a Pearson correlation coefficient of 0.7282 indicating a moderately strong correlation. The dose range was from 0.225 mSv to 3.10 mSv with a mean dose of 0.795 mSv.
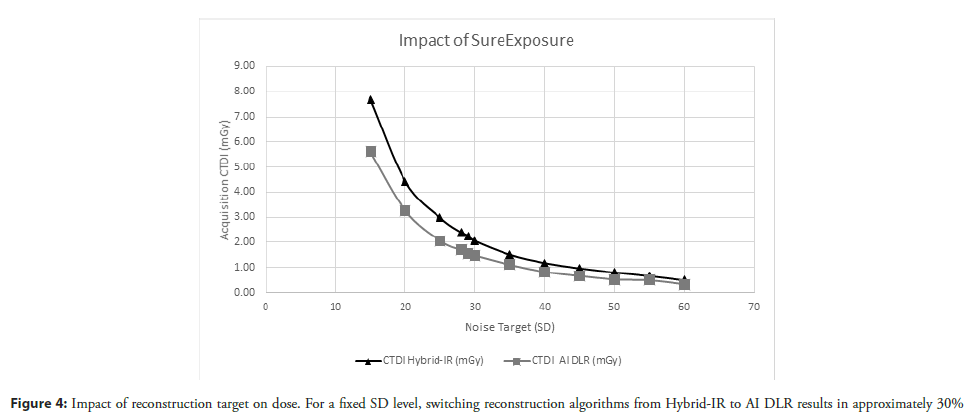
Phantom measurements showed a reduction in CTDI of approximately 30% when the target reconstruction method was changed from Hybrid-IR to AI DLR, but with a fixed noise target (SD). These results are depicted in Figure 4 and Table 1. Table 1 tabulates the CTDI for scans of the Catphan phantom as the noise target was increased when the scan protocol was setup with Hybrid-IR and repeated with AI DLR as the reconstruction. From this table the dose for a noise target of 45 (SD=45) which is our clinical protocol, will reduce the dose by 32% simply by switching the reconstruction being utilized to AI DLR.
| Noise Target (SD) | CTDI Hybrid-IR (mGy) | CTDI AI DLR (mGy) | Reduction in Dose |
|---|---|---|---|
| 15 | 7.68 | 5.61 | 27% |
| 20 | 4.41 | 3.26 | 26% |
| 25 | 2.97 | 2.06 | 31% |
| 28 | 2.39 | 1.69 | 29% |
| 29 | 2.27 | 1.54 | 32% |
| 30 | 2.06 | 1.48 | 28% |
| 35 | 1.51 | 1.11 | 26% |
| 40 | 1.18 | 0.82 | 31% |
| 45 | 0.97 | 0.66 | 32% |
| 50 | 0.80 | 0.52 | 35% |
| 55 | 0.66 | 0.49 | 26% |
| 60 | 0.49 | 0.33 | 33% |
Table 1: Dose reduction achieved between Hybrid-IR and AI DLR reconstructions.
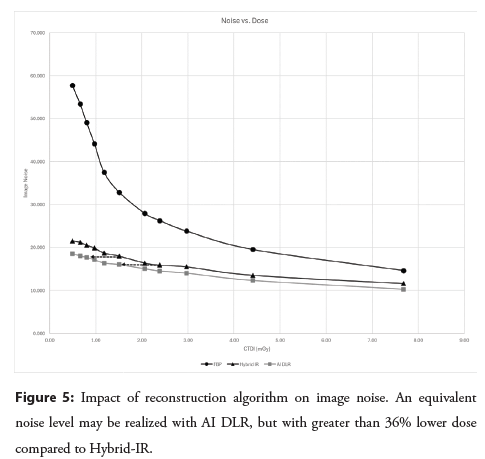
Noise measurements in phantom images were also used to determine the level of dose reduction possible with AI DLR to maintain similar noise levels as Hybrid-IR. Figure 5 shows the effect of the image of reconstruction algorithm on image noise and indicates a dose reduction of at least a 37% would lead no degradation in AI DLR image noise compared to Hybrid IR AI DLR yield lower noise levels compared to FBP or Hybrid-IR.
To maintain the noise level attained with Hybrid-IR at a noise target level of 45 (SD=45), a higher noise target (SD=70) may be used, and this would lead to a dose reduction of approximately 44%. Dashed arrows in Figure 5 illustrate the opportunity for dose reduction. In our phantom experiments, with noise target set at SD=28, a CTDI of 2.4 mGy is administered and noise with Hybrid-IR measures 15.9. To maintain approximately the same noise level with AI DLR, noise target would need to be set to SD=35 and a CDTI of 1.5 mGy would be administered. At this dose level, the noise in the AI-DLR image was measured to be 16.1.
Similarly, with noise target set at SD=35, a CTDI of 1.5 mGy is administered and noise with Hybrid-IR measures 18.0. To maintain approximately the same noise level with AI DLR, noise target would need to be set to SD=55 and a CDTI of 0.66 mGy would be administered. At this dose level, the noise in the AI-DLR image was measured to be 18.1. These results indicate a dose reduction of between 37% and 56% could be implemented without any noise penalty in the AI DLR images.
Qualitative
Qualitative image quality differences were consistent across all patients (Figure 6). The AI DLR image quality was mildly improved (+1 total difference) at soft tissue contrast and moderately improved (+2 total difference) at lung contrast compared with the Hybrid-IR. The Hybrid-IR image quality was moderately improved (+2 total difference) at soft tissue contrast and moderately (+2 total difference) at lung contrast compared with the FBP. The AI DLR was significantly improved (+3 total difference) at soft tissue contrast and even more significantly improved (+4 total difference) at lung contrast compared with the FBP.
Discussion
The results of this study quantitatively and qualitatively validated the use of AI Deep Learning Reconstruction for Coronary Artery Calcification Scoring and established that CACS can be consistently and robustly performed with AI DLR. Such validation results have yet to be reported for a 4 cm detector CT.
The CACS results with DLR show no statistically significant difference in Agaston values from those produced with those of a previously validated Hybrid-IR technique. However, they are generally marginally higher with AI DLR (mean 93.50) than with Hybrid-IR (mean 91.50). Possible reason for the differences between AI DLR and FBP is the lower noise in AI DLR removes a positive bias in CACS measurements caused by noise, while the improved spatial resolution improves the density measurements of small segments of calcium. These results are consistent with those previously reported.
There are two phenomena at play when AI DLR is used in the imaging of calcifications, and especially areas of small calcium deposits. AI DLR images are sharper, so there is less calcium blooming and smaller calcium deposits are detected more robustly. Secondarily, image noise is lower and as a result systematic biases in measurements are reduced. We believe the higher noise with FBP leads to more false positive and hence fewer cases classified as CACS=0 with FBP compared to Hybrid-IR and AI DLR. Additionally, we believe the increased spatial resolution of AI-DLR is responsible for more tiny calcifications being detected, explaining the slightly fewer CAC=0 cases compared to Hybrid-IR.
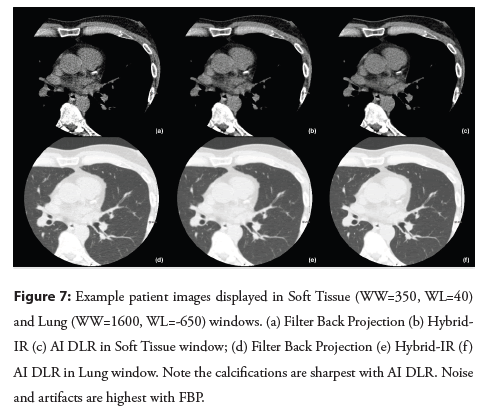
This is supported by qualitative image analysis where individual calcifications may appear sharper and denser on AI DLR and FBP than on Hybrid-IR (Figure 7). It should also be noted that the FBP images have significantly worse clinical diagnostic quality than the AI DLR images and would not be advised for routine clinical use at either soft tissue or lung contrast settings. This is noted in the kappa agreement statistic for minimal calcium classification, which indicates only fair agreement (κ=0.27 ± 0.14) between the Hybrid IR and FBP reconstructions.
Figure 7: Example patient images displayed in Soft Tissue (WW=350, WL=40) and Lung (WW=1600, WL=-650) windows. (a) Filter Back Projection (b) Hybrid- IR (c) AI DLR in Soft Tissue window; (d) Filter Back Projection (e) Hybrid-IR (f ) AI DLR in Lung window. Note the calcifications are sharpest with AI DLR. Noise and artifacts are highest with FBP.
In general, there is substantial or near perfect agreement between all the AI DLR reconstructions and the Hybrid-IR reconstructions which is the current standard of care. Patients with minimal calcium classification, did show substantial agreement with κ=0.64 ± 0.14. Lower measurements of calcium are more susceptible to noise in the measurements. It should be noted that interscan variability exists in CACS measurements. A number of factors including the choice of scanner can affect interscan variability, and the level of agreement in our study is less than variability that could be expected in general [24].
As reported in the results, patient dose was exponentially related to BMI Figure 3. This is consistent with previously studies investigating automated exposure control behavior [25].
AI DLR allows further dose reduction beyond the 1 mSv threshold set in this study for non-obese patients. Utilizing automated exposure control noise targets based on an AI DLR model rather than on Hybrid-IR model will allow for dose reductions of approximately 36% with improved image quality [26]. Further dose reduction can then be accomplished by utilizing a higher standard deviation of the noise (above 45) as the AI DLR image quality was improved compared with the Hybrid-IR image quality.
In conclusion, further dose reduction can be accomplished while maintaining image quality at or better than at current Hybrid-IR levels. We will target a dose reduction of at least a 37% for all patients. Accepting a linear, no threshold model of radiation risk [27, 28] this we expect a similar reduction of radiation risk for all patients.
Conclusion
AI DLR has been quantitatively and qualitatively validated for use in CACS on 4 cm coverage CT scanner. AI DLR produces qualitatively better image quality than HYBRID-IR at the same dose level, while producing good agreement in categorization with agatston scores. AI DLR will allow for at least a 37% further dose reduction on a 4 cm coverage CT scanner.
References
- Ayoub M, Tajti P, Ferenc M, et al. Feasibility and outcome of the Rotapro system in treating severely calcified coronary lesions: The Rotapro study. Cardiol J. 30(4):526-533 (2023).
[CrossRef] [Google Scholar] [PubMed]
- Mankerious N, Richardt G, Allali A, et al. Lower revascularization rates after high-speed rotational atherectomy compared to modified balloons in calcified coronary lesions: 5-year outcomes of the randomized PREPARE-CALC trial. Clin Res Cardiol. 113(7):1051-1059 (2024).
[CrossRef] [Google Scholar] [PubMed]
- Sakakura K, Ito Y, Shibata Y, et al. Clinical expert consensus document on rotational atherectomy from the Japanese association of cardiovascular intervention and therapeutics: Update 2023. Cardiovasc Interv Ther. 38(2):141-162 (2023).
[CrossRef] [Google Scholar] [PubMed]
- Sharma SK, Tomey MI, Teirstein PS, et al. North American expert review of rotational atherectomy. Circ Cardiovasc Interv. 12(5):e007448 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Iannopollo G, Gallo F, Mangieri A, et al. Tips and tricks for rotational atherectomy. J Invasive Cardiol. 31(12):E376-E383 (2019).
[Google Scholar] [PubMed]
- Kaneko U, Kashima Y, Sugie T, et al. Rotablator driveshaft fracture due to significant proximal tortuosity and enlargement causing massive coronary perforation. Korean Circ J. 50:1048-1050 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Kaneko U, Kashima Y, Sugie T, et al. Fracture of rotational atherectomy burr: Pre‐fracture signs, mechanisms, and management strategies. Catheter Cardiovasc Interv. 105(7):1608-1615 (2025).
[CrossRef] [Google Scholar] [PubMed]
- Tomasiewicz B, Kubler P, Zimoch W, et al. Acute angulation and sequential lesion increase the risk of rotational atherectomy failure. Circ J. 85(6):867-76 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Morita Y, Kashima Y, Yasuda Y, et al. Burr entrapment in a percutaneous coronary intervention during rotational atherectomy: An experience with 3195 cases. J Invasive Cardiol. 35(10): (2023).
[Google Scholar] [PubMed]
- Derbas LA, Iskandar MH, Kavinsky LJ, et al. Utility of guide extension catheter for rotational atherectomy through a LIMA graft. JACC Cardiovasc Interv. 15(1):e1-e2 (2022).
[CrossRef] [Google Scholar] [PubMed]
- Kaneko U, Kashima Y, Kuramitsu S, et al. The DELIVER Technique: Deep engagement of guide or ChiLd-guIde Catheter for Burr DeliVEry and rotational atherectomy. JACC Case Rep. 30(5):103177 (2025).
[CrossRef] [Google Scholar] [PubMed]
- Garbo R, Iannaccone M, Werner GS, et al. Utility of guiding catheter extensions for recanalization of chronic total occlusions: A EuroCTO club expert panel report. JACC Cardiovasc Interv. 16(15):1833-1844 (2023).
[CrossRef] [Google Scholar] [PubMed]
- Ali M, Yagoub H, Ibrahim A, et al. Anchor-balloon technique to facilitate stent delivery via the GuideLiner catheter in percutaneous coronary intervention. Future Cardiol. 14(4):291-299 (2018).
[CrossRef] [Google Scholar] [PubMed]
- Patel T, Shah S, Pancholy S, et al. Balloon‐assisted tracking: A must‐know technique to overcome difficult anatomy during transradial approach. Catheter Cardiovasc Interv. 83(2):211-220 (2014).
[CrossRef] [Google Scholar] [PubMed]
- Elbarouni B, Moussa M, Kass M, et al. GuideLiner Balloon Assisted Tracking (GBAT): A new addition to the interventional toolbox. Case Rep Cardiol. 2016(1):6715630 (2016).
[CrossRef] [Google Scholar] [PubMed]
- Kato T, Fujino M, Takagi K, et al. The rotational atherectomy with a guide extension catheter for calcified and tortuous lesions in left anterior descending artery: A case report. BMC Cardiovasc Disord. 21:1-4 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Costanzo P, Aznaouridis K, Hoye A, et al. GuideLiner-facilitated rotational atherectomy in calcified right coronary artery: the "child" makes the difference. JACC Cardiovasc Interv. 9:e47-e48 (2016).
- Pawłowski T, Modzelewski P, Stachura M, et al. Guiding catheter extension compatibility for high speed rotational atherectomy. Postepy Kardiol Interwencyjnej. 17(2):210-213 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Kobayashi N, Yamawaki M, Hirano K, et al. Use of the orbital atherectomy system backed up with the guide-extension catheter for a severely tortuous calcified coronary lesion. SAGE Open Med Case Rep. 8:2050313X20921081 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Kawamura Y, Yoshimachi F, Murotani N, et al. Coronary orbital atherectomy using a five-French guiding catheter. Cardiovasc Interv Ther. 37(3):498-505. (2022).
[CrossRef] [Google Scholar] [PubMed]
- Nakamura M, Kuriyama N, Tanaka Y, et al. Dual-Prep registry: Atherectomy devices and intravascUlAr lithotripsy for the PREParation of heavily calcified coronary lesions registry. Cardiovasc Interv Ther. 40(3):553-564 (2025).
[CrossRef] [Google Scholar] [PubMed]