Case Report - Clinical Practice (2022) Volume 19, Issue 3
Incarcerated urinary bladder in a rectal prolapse: A case report
- Corresponding Author:
- Ningi AB
Department of Surgery, Abubakar Tafawa-Balewa University, Nigeria
E-mail: ningibala41@gmail.com
Received: 17 January, 2022, Manuscript No. fmcp-22-51761 Editor assigned: 21 January, 2022, PreQC No. fmcp-22-51761 Reviewed: 14 February, 2022, QC No. fmcp-22-51761 Revised: 15 February, 2022, Manuscript No. fmcp-22-51761 Published: 21 February, 2022, DOI. 10.37532/ fmcp.2022.19(2).1871- 1876
Abstract
Rectal prolapse is said to occur if there is a full-thickness intussusception of the rectal wall with external protrusion through the anus. It is a rare surgical presentation with an estimated prevalence of 0.5% worldwide. It is slightly commoner in females and the elderly, and women aged above 50 years have 6 times the risk of rectal prolapse than men. It is also seen in children younger than 4 years, mostly in the infancy stage. Excessive straining during defecation with or without constipation, diarrhea, malnutrition, helminthiasis, and prolonged use of laxatives are the main predisposing factors. It is part of a complex called the Pelvic Organ Prolapse (POP). It may therefore be associated with dysfunction and/or descent of other pelvic organs, e.g., rectoceles, uterine or vaginal vault prolapse, cystocele, and enterocoele. We previously reported a rare case of an incarcerated gravid uterus in rectal prolapse. Literature search, however, did not yield a single report of an incarcerated urinary bladder in rectal prolapse. This may probably be the first reported case in humans. The incarcerated prolapsed urinary bladder and the rectum were reduced via laparotomy, an encircling non-absorbable suture Thiersch procedure done on the anus and a proximal defunctioning colostomy sited because the rectal mucosa has questionable viability. No recurrence of rectal prolapse was recorded and the proximal sigmoid colostomy was reversed 6 weeks after the surgery.
Keywords
Incarcerated urinary bladder, rectal prolapse, sigmoid colostomy, thiersch procedure
Introduction
Although Rectal prolapse is defined as a fullthickness protrusion of the rectum through the anus, it hardly occurs at once. It usually begins with an internal sigmoid-rectal intussusception that can be demonstrated on defecography, followed by external mucosal prolapse only, and a subsequent full-thickness rectal prolapse [1]. Both the full-thickness rectal prolapse and internal sigmoid-rectal mucosal intussusception can occur independently or be associated with prolapse of other pelvic organs [1]. Rectal prolapse has been well studied and the barrage of anatomical and functional abnormalities associated with it is astounding. It is said to be associated with weakness of the levator ani muscle, an abnormally deep sacral curvature, long and redundant sigmoid colonic segment, and a lax anal external sphincter complex [2]. Some degree of loss of integrity of the rectal sacral ligament attachments has also been adduced to [3]. Although it is hardly present as a surgical emergency, it is a significant source of morbidity. Irritation of the prolapsed rectal mucosa results in significant discomfort, per anal mucus discharge, per anal bleeding, fecal incontinence, or constipation [4]. The initial complaint is that of per anal protrusion of the rectal mucosa following defaecation, with spontaneous reduction of the prolapsed mucosa on completion of the stooling. The size of the protruding segment progressively increases with straining and will warrant manual reduction by the patient. Rarely, it may present as Procidentia, with the prolapsed segment unable to be reduced manually [5,6].
The presence of acute urine retention in a patient with rectal prolapse is not common, and the discovery of an incarcerated urinary bladder within the prolapsed rectal segment is even rarer. We report here such a rare incident in a young male patient with a history of rectal prolapse since childhood.
Case Report
A 30-year-old male patient presented at the emergency room of the Abubakar Tafawa- Balewa University Teaching Hospital (ATBUTH), Bauchi State, Nigeria with a 5-day history of sudden per anal protrusion following defaecation and a 3-hour history of acute urinary retention. The per anal protrusion was said to have failed manual reduction by the patient and also several futile attempts at a secondary tier health facility. The patient did not present to us for the per anal protrusion because there was no associated constipation or fecal incontinence. It was the onset of a sudden inability to pass urine with associated painful supra-pubic swelling that prompted the presentation. A history of recurrent protrusion of the rectal wall per anum was obtained. The protrusion started in childhood, reduced spontaneous initially, then required manual reduction 3 years ago. There was a history of recurrent diarrhea immediately after weaning and history of clinically diagnosed pulmonary tuberculosis at 11-year of age. The patient has been managing the condition well until 3 months before presentation when he failed to achieve manual reduction at home. He has had 2 hospital admissions and manual reduction of the prolapsed rectal mass after application of warm packs, parenteral analgesia, and a lubricating gel.
General physical examination revealed a young male patient in obvious painful distress, dehydrated and pale, afebrile, anicteric, cyanosed, with no significant peripheral lymph node enlargement. He had a pulse rate of 108 beats per minute and blood pressure of 100/60 mmHg.
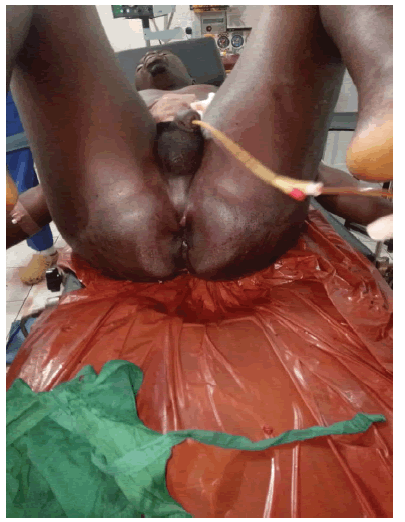
The abdomen was scaphoid, moves with respiration and there are no surgical scars. There was a tender supra-pubic swelling that is dull to percussion, surrounded by zones of resonance. There was a huge reddish mass protruding through the anus with patchy dark areas (FIGURE 1). A digital rectal examination revealed a patulous anus with a lax external sphincter. Urethral catheterization produced concentrated urine and relieved the tender supra-pubic swelling.
An ultrasound scan with a 5 MHz transducer of the per anal mass confirmed a prolapsed rectal segment with an incarcerated segment of the urinary bladder.
The patient was fully resuscitated with Hartman’s solution and maintained on same, alternated with 5% Dextrose in water. Informed consent was obtained for the reduction of the prolapsing complex under regional anesthesia. The initial attempt at manual reduction failed despite the application of warm packs and lubricating gel. General anesthesia was given and a combined abdominal and perineal approach was deployed. A successful reduction was achieved after dis-impacting the incarcerated bladder and the prolapsed rectum was manually reduced (FIGURE 2). An encircling purse-string Thiersch suture was placed around the anus with polyamide 2.0 to retain the reduced rectum in a position (FIGURE 3). A defunctioning divided sigmoid colostomy was sited because of the questionable viability of the reduced rectal complex.
The patient did well postoperatively and was discharged home. The Thiersch suture was removed at 6 weeks and the colostomy was reversed at 12 weeks. No recurrence of the rectal prolapse was noted.
Discussion
Cases of rectal prolapse are rare surgical presentations. A Rectal prolapse commonly contains all the layers of the rectum protruding per anum as a cylindrical, elongated mass or an ovoid mass with pinkish fleshy tissue. The causes of the Prolapse may be varied but, it usually follows urogenital or anorectal disorders, recurrent diarrhea from colitis or proctitis, and chronic constipation from tumors of the colon, rectum, or anus [7]. It is commoner in women above the age of 50 years and the peak age of incidence is the seventh decade in women, whereas the majority of males that develop rectal prolapse are seen at the age of 40 or less. Some have reported an increased predilection in young victims for autism, developmental disorders, and psychiatric comorbidities requiring multiple medications [8]. They were also reported to present with significant symptoms of bowel motility dysfunction, especially, constipation [7]. Our patient reflected the above finding. He is a 30-year old male and the predominant complaint was that of constipation.
Although symptoms at presentation may vary, it is estimated that up to 50% to 75% of patients with rectal prolapse present with fecal incontinence, and 25% to 50% of them will report constipation [9-13]. However, in most surgical units the presentation occurs in stages.
The presentation of incomplete rectal prolapse is that of a huge bulge of a fleshy mass protruding per anum with associated spontaneous reduction after completion of defaecation, then progressing to reduction through manual manipulation. A fraction of these patients has rather a subtler presentation [4,14]. They may present with a complaint of the feeling of rectal fullness, constipation, fecal incontinence, per anal mucous discharge, and anal bleeding. If the condition progresses to a Procidentia, rectal incarceration or even strangulation may occur from sphincteric constriction and intrinsic edema. The presentation here will be that of a huge, painful, irreducible prolapsed rectal mass [1]. Patients with sigmoid-rectal intussusception only may present with acute onset of constipation or colicky abdominal pain. Many may remain asymptomatic, only picked up incidentally on defecography [15]. Our patient presented with an incarcerated external prolapse, hence the main complaints were the painful, immobile, prolapsed rectal tissue, with evidence of patchy mucosal infarction.
The fecal incontinence seen in complete rectal prolapse is said to be a result of disruption of the external anal sphincter mechanism, loss of sphincteric muscle integrity due to excessive stretch from the prolapsed rectum, and the persistent activation of recto-anal inhibitory reflex by the same prolapsed rectal complex [16]. Some reports have indicated the presence of pudendal neuropathy in these patients and it can be demonstrated in about 50% of those presenting with incontinence [17], the pudendal neuropathy is said to lead to denervation-related atrophy of the external sphincter muscles [18]. Despite its preponderance, our patient, however, did not report fecal incontinence.
Constipation is noted to be commoner in those with sigmoid-rectal intussusception, with the intussuspicient sigmoid mucosa occluding the rectal lumen. These patients may also have an associated pelvic floor weakness, and colonic motility disorder [11,12]. Our patient presented with constipation, possibly from combined complete and incomplete rectal prolapse.
Apart from the history of chronic constipation, our patient has a history of chronic cough, was treated for pulmonary Tuberculosis during childhood. Chronic cough and chronic obstructive airway diseases are known to result in chronic episodic increases in abdominal pressure. It has been reported in one case-control study that chronic cough and chronic airway obstruction are associated with an increased risk of pelvic organ prolapse in women <45 years of age (14%) compared to controls (2.4%) [19]. Another important risk factor is the history of recurrent diarrhea following weaning in our patient. Many studies have implicated the loss of Ischio-rectal fat due to malnutrition, chronic constipation, and/or straining during defecation, or due to idiopathic causes in the etiology of rectal prolapse [20-22].
Late presentation as in the index patient was widely reported, especially in an ignorant peasant whose the vicissitude of daily living is his utmost concern. We noted this in our previous report on an incarcerated gravid uterus in a prolapsed rectum [23]. The only diagnostic investigation we were able to do was an Ultra- Sound Scan. It clinched the diagnoses and helped in the surgical decision taken. Previous reports from Nigeria also relied on the same radiological tool [23].
Despite several years of handling cases of rectal prolapse, a consensus treatment has remained elusive. It started with the attempt to restore the altered anatomy to normalcy, up to the gamut of procedures now deployed with variable degrees of success [4]. Although our patient is conversant with manual reduction, this maneuver has been unfruitful for months before the presentation. This may perhaps be the result of the significant size of the incarcerated prolapsed rectum due to edema. Some reports have indicated successful reduction after the application of table sugar. This was related to the hygroscopic property of incarcerated rectal prolapse which absorbs the edema fluid of the swollen rectal tissue [24]. A successful reduction is however an incomplete victory, because, relapse is inevitable following another straining.
Surgery has so far remained the most successful treatment option [4]. The number of surgical procedures deployed for rectal prolapse indicates that none has been considered the gold standard. The surgical options include both open and minimally invasive surgeries and the approaches may be perineal or abdominal, depending on the clinical presentation and the past medical history [4,5]. These may include Thiersch encircling anal suture, rectal mucosal excision, rectal anterior resection with or without rectopexy, rectopexy to the sacral fascia, perineal procto-sigmoidectomy, or posterior sagittal rectopexy in children [25]. Many of the surgical anchorages of the prolapsing rectum are done with the use of synthetic meshes attached to the presacral fascia. The choice of either open or laparoscopic approach or the extent of surgery is dictated by the background medical condition of the patient, the competence of the Surgeon, perhaps, how old is the patient and the presence or absence of fecal incontinence [26]. A Thiersch encircling anal suture was used after a successful reduction in the theatre in this patient. This was chosen because, the patient presented as an emergency with evidence of mild acute kidney injury, it can be done fast and safely, and has been reported to carry fewer complications [27]. It has so far successfully prevented a recurrence, even after the return of normal defecatory function.
Whatever the type of Surgical procedure chosen, the aims should be to reduce the prolapsed rectum and restore the normal sigmoid-rectoanal anatomy, correct troubling morbidities of fecal incontinence or chronic constipation, and as much as possible minimize surgical complications from the procedure [7]. A recurrence rate of 16% to 30% has been reported after most perineal repairs of rectal prolapse, even after perineal resection of the rectum or rectopexy [28-30].
Conclusion
Fecal and urinary incontinence is the most expected in a patient with rectal or even pelvic organ prolapse. The presence of Acute Urinary Retention should always arouse suspicion of urinary bladder incarceration within the prolapsing rectum. A good physical examination and a simple high-resolution ultrasound scan will help to identify this situation. A successful disengagement of the bladder from the prolapsing rectal complex eases subsequent reduction of the prolapse and minimizes the risk of bladder injury where perineal resection of the rectum will be used.
References
- Liliana B, Caitlin WH, Andreas MK, et al. Rectal prolapse: An overview of clinical features, diagnosis, and patient-specific management strategies. J Gastrointest Surg. 18,1059-1069 (2014).
[Google Scholar] [Crossref] - Broden B, Snellman B. Procidentia of the rectum studied with cineradiography: a contribution to the discussion of causative mechanism. Dis Colon Rectum. 11, 330-347 (1968).
[Google Scholar] [Crossref] - Collinson R, Cunningham C, D’Costa H, et al. Rectal intussusception and unexplained fecal incontinence: findings of a proctographic study. Colorectal Dis. 11, 77-83 (2009).
[Google Scholar] [Crossref] - Varma M, Rafferty J, Buie WD, et al. Practice parameters for rectal prolapse. Dis Colon Rectum. 54, 1339-1346 (2011).
[Google Scholar] [Crossref] - Hammond K, Beck DE, Margolin DA, et al. Rectal prolapse: A 10-year experience. Ochsner J. 7, 24-32 (2007).
[Google Scholar] [Crossref] - Goldstein SD, Maxwell PJ. Rectal prolapse. Clin Colon Rectal Surg. 24, 39-45 (2011).
[Google Scholar] [Crossref] - Bordeianou L, Paquette I, Johnsonet E, et al. Clinical practice guidelines for the treatment of rectal prolapse. Dis Colon Rectum. 60, 1121-1131 (2017).
[Google Scholar] [Crossref] - Marceau C, Parc Y, Debroux E, et al. Complete rectal prolapse in young patients: psychiatric disease a risk factor of poor outcome. Colorectal Dis. 7, 360-365 (2005).
[Google Scholar] [Crossref] - Kim DS, Tsang CB, Wong WD, et al. Complete rectal prolapse: evolution of management and results. Dis Colon Rectum. 42, 460-466 (1999).
[Google Scholar] [Crossref] - Madoff RD, Mellgren A. One hundred years of rectal prolapse surgery. Dis Colon Rectum. 42, 441-450 (1999).
[Google Scholar] [Crossref] - Schultz I, Mellgren A, Dolk A, et al. Long-term results and functional outcome after Ripstein rectopexy. Dis Colon Rectum. 43, 35-43 (2000).
[Google Scholar] [Crossref] - Schultz I, Mellgren A, Oberg M, et al. Whole gut transit is prolonged after Ripstein rectopexy. Eur J Surg. 165, 242-247 (1999).
[Google Scholar] [Crossref] - Senagore AJ. Management of rectal prolapse: the role of laparoscopic approaches. Semin Laparosc Surg. 10, 197-202 (2003).
[Google Scholar] [Crossref] - Bordeianou L, Rockwood T, Baxter N, et al. Does incontinence severity correlate with quality of life? Prospective analysis of 502 consecutive patients. Colorectal Dis. 10, 273-279 (2008).
[Google Scholar] [Crossref] - Dvorkin LS, Gladman MA, Epstein J, et al. Rectal intussusception in symptomatic patients is different from that in asymptomatic volunteers. Br J Surg. 92, 866-872 (2005).
[Google Scholar] [Crossref] - Hawkins AT, Olariu AG, Savitt LR, et al. Impact of rising grades of internal rectal intussusception on faecal continence and symptoms of constipation. Dis Colon Rectum. 59, 54-61 (2016).
[Google Scholar] [Crossref] - Glasgow SC, Birnbaum EH, Kodner IJ, et al. Preoperative anal manometry predicts continence after perineal proctectomy for rectal prolapse. Dis Colon Rectum. 49, 1052-1058 (2006).
[Google Scholar] [Crossref] - Snooks SJ, Henry MM, Swash M. Anorectal incontinence and rectal prolapse: differential assessment of the innervation to pubo-rectalis and external anal sphincter muscles. Gut. 26, 470-476 (1985).
[Google Scholar] [Crossref] - Rinne KM, Kirkinen PP. What predisposes young women to genital prolapse? Eur J Obstet Gynecol Reprod Biol. 1999; 84:23-5.
[Google Scholar] [Crossref] - Ashcraft KW, Garred JL, Holder TM, et al. Rectal prolapse: 17-year experience with the posterior repair and suspension. J Pediatr Surg. 25, 992-994 (1990).
[Google Scholar] [Crossref] - Sanaka MR, Ferguson DR, Ulrich S, et al. Polyp associated with rectal prolapse. Gastrointest Endosc. 59, 871-872 (2004).
[Google Scholar] [Crossref] - Rintala RJ, Pakarinen M. Disorders of the anus and rectum, anorectal function. In: O’Neill JA, Coran AG, Fonkalsrud E, Grosfeld JL, editors. Pediatric surgery. 6th ed. Philadelphia: Mosby. 1595-1596 (2006).
- El-Nafaty AU, Obiano SK, Mamman TH, et al. Incarcerated gravid uterus in a rectal prolapse: A case report. Int J Case Rep Images. 8, 473-477 (2017).
[Google Scholar] [Crossref] - Myers JO, Rothenberger DA. Sugar in the reduction of incarcerated prolapsed bowel: report of two cases. Dis Colon Rectum. 34, 416-418 (1991).
[Google Scholar] [Crossref] - Amel Abd EH. Posterior sagittal rectopexy in the treatment of recurrent rectal prolapse in children. Annals of Pediatric Surgery. 7, 101-104 (2011).
[Google Scholar] [Crossref] - Brown AJ, Anderson JH, McKee RF, et al. Strategy for selection of type of operation for rectal prolapse based on clinical criteria. Dis Colon Rectum. 47, 103-107 (2004).
[Google Scholar] [Crossref] - Lee JL, Yang SS, Park IJ, et al. Comparison of abdominal and perineal procedures for complete rectal prolapse: An analysis of 104 patients. Ann Surg Treat Res. 86, 249-255 (2014).
[Google Scholar] [Crossref] - Altomare DF, Binda G, Ganio E, et al. Long-term outcome of Altemeier’s procedure for rectal prolapse. Dis Colon Rectum. 52, 698-703 (2009).
[Google Scholar] [Crossref] - Azimuddin K, Khubchandani IT, Rosen L, et al. Rectal prolapse: a search for the “best” operation. Am Surg. 67, 622-627 (2001).
[Google Scholar] [Crossref] - Pescatori M, Zbar AP. Tailored surgery for internal and external rectal prolapse: functional results of 268 patients operated upon by a single surgeon over 21 years*. Colorectal Dis. 11, 410-419 (2009).
[Google Scholar] [Crossref]