Review Article - Imaging in Medicine (2010) Volume 2, Issue 4
Imaging of running-induced osseous injuries
Timothy G Sanders† and Terry A Sanders1
1 Columbia Podiatry Foot & Ankle Center, Columbia, MO, USA
- *Corresponding Author:
- Timothy G Sanders
Columbia Podiatry Foot & Ankle Center Columbia
MO, USA
Tel.: +1 954 698 9390
Fax: +1 434 295 5265
E-mail: radmantgs@cs.com
Abstract
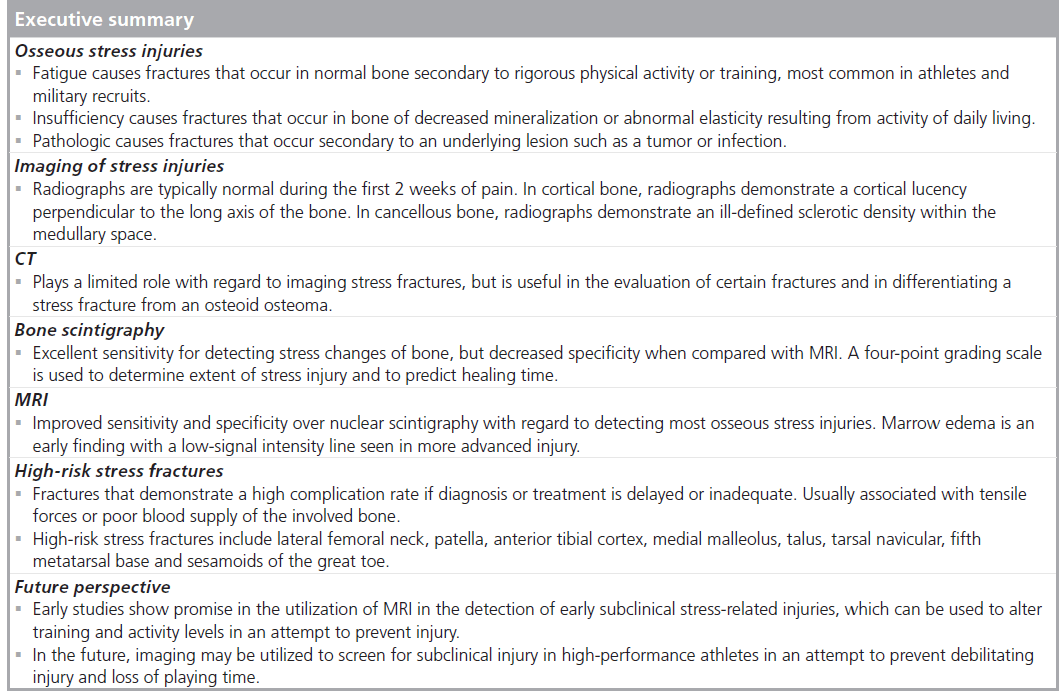
Osseous overuse and stress-related injuries commonly occur in individuals who participate in the sport of running. While the clinical history and physical examination are important first steps in establishing the correct diagnosis, imaging often plays a vital role in confirming the diagnosis and in determining the extent of injury and prognosis for the injured athlete. This article will provide a thorough review of the numerous osseous stress injuries that occur in runners, including a summary of the high-risk stress fractures. Imaging strategies are discussed and the typical radiographic, CT, MRI and nuclear scintigraphic findings are described for each of the various stress-related injuries associated with running.
Keywords
bone scan; CT; MRI; running injury; sports medicine; stress fracture ; stress injury
Running continues to grow in popularity as a sport and is also an important component of the training and conditioning of athletes who participate in numerous other sports including American football, basketball and soccer to name a few. Therefore, it is not surprising that the number of running-associated injuries is on the rise [1]. Many factors can put a runner at risk of injury but the majority of injuries result from overuse, often following a sudden increase in activity level or an abrupt change in the training regimen. While obtaining an accurate clinical history and performing an appropriate physical examination are the most important factors in establishing the correct diagnosis, imaging often plays a vital role in establishing or confirming a suspected diagnosis. Imaging can often differentiate soft tissue from osseous injury, can help guide therapy and aid in determining the prognosis for a specific injury. Here we review the clinical and imaging findings associated with common osseous stress-related injuries that occur in runners.
Osseous injuries
Stress fractures can be categorized as fatigue stress fractures or insufficiency stress fractures [2–4]. Fatigue fractures occur in bones that have normal mineralization and normal elasticity properties and most often occur in the young athletic population or in military recruits, resulting from rigorous physical activity or training. Insufficiency fractures occur in bones that have decreased mineralization and or abnormal elasticity properties and result from the normal activities of daily living. These fractures are more likely to occur in the elderly population, in women or in individuals with predisposing illnesses, such as rheumatoid arthritis or renal disease, or exogenous steroid use [3,5,6]. Hormonal factors, including the menopause or amenorrhea, especially when associated with minimal body fat or anorexia can play a role in stress fractures in females [7,8]. As a result, stress fractures in female athletes are considered by many to be a combination of both fatigue and insufficiency. Insufficiency fractures should be differentiated from pathologic fractures, which occur secondary to an underlying bone lesion such as a tumor, cyst or infection.
Biomechanics of osseous stress injury
There is a broad continuum of stress-related bone injuries that occur as a result of excessive repetitive force placed on a given bone, and these injuries are common in the lower extremities of runners. This repetitive force is a combination of many factors including weight-bearing, muscular contraction as well as bending and torsional forces that are applied to the affected bone. Bone is a dynamic tissue that responds to various stresses placed upon it. When these stresses exceed the bone’s ability to remodel and repair itself, then we see a spectrum of osseous injury that begins with microtrabecular injury and culminates with a complete fracture.
Radiographs
Radiographs are typically normal during the first 2–3 weeks following the onset of pain in a runner who develops an osseous stress injury. Radiographs can remain normal for considerably longer periods of time. When abnormal, the radiographic appearance depends upon the timing and the location of injury. Injuries that involve cortical bone (i.e., the shaft of a long bone) will usually present with a cortical lucency oriented perpendicular to the long axis of the bone (Supplementary Figure 1A, see online www.futuremedicine.com/doi/suppl/10.2217/ iim.10.37). Periosteal new bone formation and cortical thickening are late radiographic findings. When stress changes occur in cancellous bone (i.e., metaphyseal regions of a long bone, femoral neck, and small bones of the foot and ankle), radiographs most often show an illdefined linear area of sclerotic density located within the medullary space of the bone. The area of sclerosis is typically oriented perpendicular to the primary trabeculae of the involved bone (Supplementary Figure 1B) [2,3].
CT scan
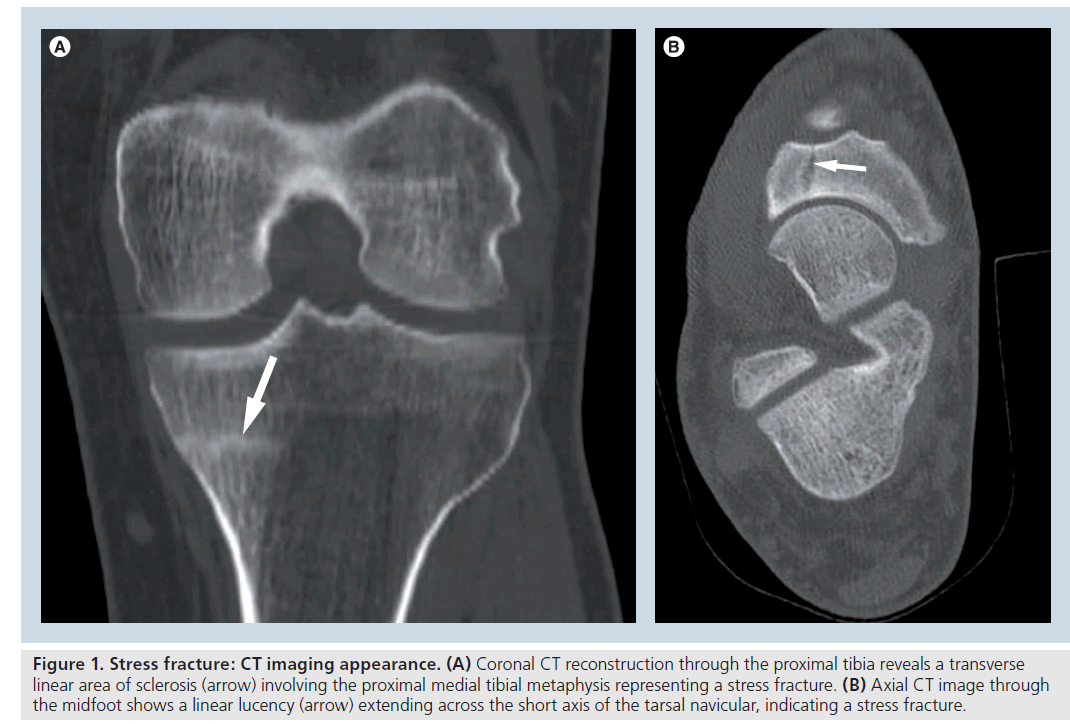
CT imaging only plays a limited role with regard to the evaluation of suspected osseous stress injuries of the lower extremities. However, there are a few specific instances when CT imaging can be of particular help. These include evaluation of a potential longitudinal stress fracture of the tibial shaft, evaluation of the tarsonavicular bone (Figure 1) or of the sesamoids of the great toe, and in detecting the presence of a nidus when attempting to differentiate an osteoid osteoma from a stress injury of the bone (Supplementary Figure 2) [9,10].
Nuclear-medicine bone scan
Nuclear-medicine bone scan demonstrates excellent sensitivity for the detection of osseous stress-related injuries of the lower extremity and has long been considered the gold standard with regard to detecting early stress-related changes of bone. More recently, MRI has supplanted bone scintigraphy as the imaging modality of choice in most instances of suspected stress-related osseous injuries of the lower extremity [11–13]. MRI demonstrates sensitivity equivalent to bone scan for the detection of stress-related injuries and has improved specificity with regard to differentiating stress changes from tumor, infection or other bone lesions and also nicely depicts soft tissue injuries that often accompany or mimic an osseous stress-related abnormality [14].
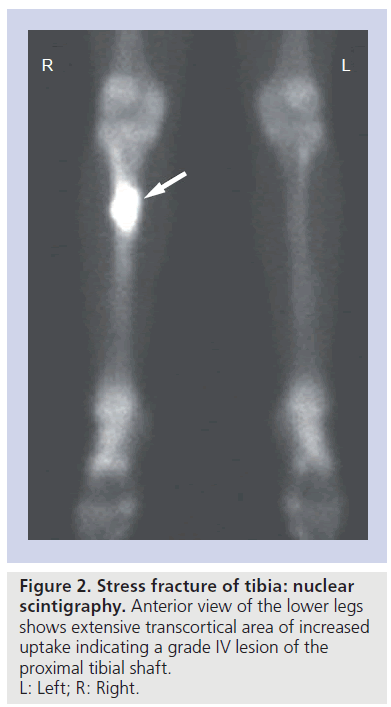
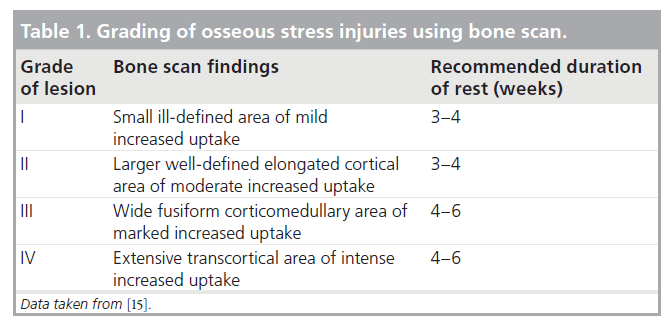
Nuclear-medicine bone scan will detect an area of increased uptake within areas of osseous stress response much earlier than radiographic imaging will demonstrate a detectable abnormality (Figure 2). Repetitive stresses placed on a bone resulting from increased activity level or a change in training regimen will result in increased turnover of bone, and the focal area of increased uptake on the bone scan corresponds to the area of increased osteoblastic activity. A normal bone scan has a high negative predictive value and in the past was thought to exclude the possibility of a stress fracture even in clinically suspected cases [15]. However, more recently, several reports of abnormal MRI examinations in the setting of a normal nuclear-medicine bone scan have demonstrated that MRI provides a higher level of sensitivity in the detection of early osseous stress changes [7,16–20]. In addition, Bryant et al. demonstrated that SPECT imaging can detect early stress-related changes of the femoral neck in the setting of a normal planar bone scan [18]. Zwas et al. developed and later refined a classification of bone scintigraphic findings, grading the extent of stress lesions from mild to severe. The grade of lesion as determined by bone scan is useful in directing therapy (Table 1) and in establishing an appropriate prognosis [15].
When performing a bone scan on a runner with a suspected osseous stress injury, it is recommended that the area of imaging include the entire pelvis and bilateral lower extremities regardless of the symptomatic site, as patients may demonstrate additional asymptomatic lesions in contralateral bones or in additional areas within the ipsilateral lower extremity. The rate of resolution of bone scan abnormality is generally related to the severity of lesion, with most low-grade lesions resolving within the first 4–6 months. Persistent unresolved lesions in most cases are believed to be related to a lack of rest and are generally associated with persistent symptoms. Occasionally patients with persistent activity will show new lesions on subsequent follow-up examinations [15,21].
MRI
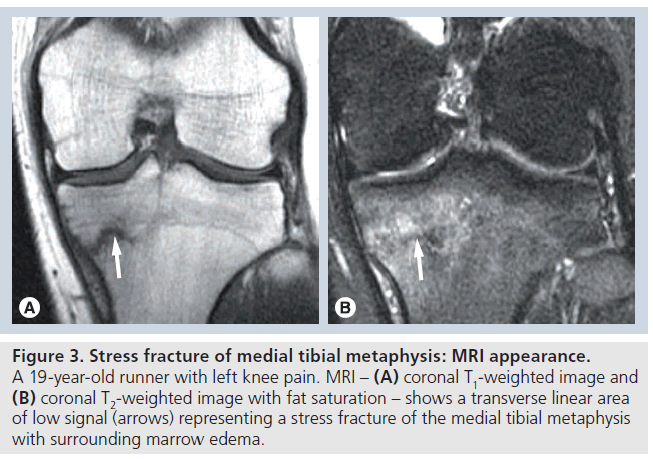
With regard to the detection of osseous stressrelated injuries and stress fractures, MRI has been shown to demonstrate both improved sensitivity and specificity relative to bone scintigraphy [11]. MRI findings typically parallel bone scintigraphic changes. Early findings may include subperiosteal edema with or without adjacent soft tissue edema. Medullary edema, manifested as low T1 and increased T2 signal on short TI inversion recovery or T2 ‑weighted imaging with fat saturation, can also be an early finding. As the extent of osseous stress-related changes progress, marrow edema may become more intense and more extensive with eventual intracortical signal abnormality developing. Magnetic resonance findings of early osseous stress-related injury may be nonspecific and may appear similar to changes of infection, bone contusion or a marrow infiltrative process. However, the correct diagnosis is often made on the basis of the clinical history combined with the typical imaging findings. Early stress fracture will typically appear as an ill-defined low-signal intensity line, seen on all pulse sequences, with surrounding marrow edema. The stress fracture may be intramedullary, but often extends to the cortex of the bone. Visualization of the linear area of low-signal intensity coupled with adjacent marrow edema is highly suggestive of a stress fracture (Figure 3) and, in the proper clinical setting, essentially excludes other diagnostic considerations [16].
Figure 1. Stress fracture: CT imaging appearance. (A) Coronal CT reconstruction through the proximal tibia reveals a transverse linear area of sclerosis (arrow) involving the proximal medial tibial metaphysis representing a stress fracture. (B) Axial CT image through the midfoot shows a linear lucency (arrow) extending across the short axis of the tarsal navicular, indicating a stress fracture.
Pelvis
Both fatigue and insufficiency stress fractures have been reported in various locations of the osseous pelvis. Fatigue fractures most often occur in regions of the pubic rami, typically involving the lateral aspect of the superior pubic ramus or the medial aspect of the inferior pubic ramus. Stress fractures can also occur in the supra-acetabular regions of the pelvis and in the region of the sacrum. Pelvic stress fractures have been reported in runners, military recruits, soccer players and bowlers and, while seen in both males and females, they are most commonly reported in females [7,22].
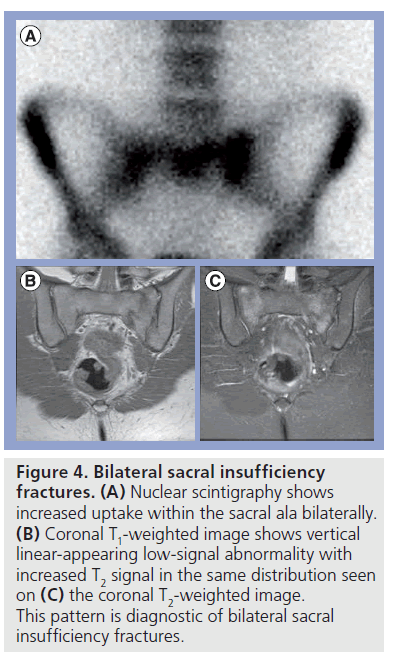
Early osseous stress changes of the pelvis are difficult to detect on radiographs but are easily detected on either MRI or bone scintigraphy. In long-standing cases, radiographs often show an area of ill-defined sclerosis usually vertically oriented in the region of the pubic rami or horizontally oriented in the supra-acetabular region. Bone scintigraphy will show an area of increased uptake while MRI will demonstrate areas of low T1 or bright T2 signal. Once a stress fracture develops, a linear area of low-signal abnormality will be seen on magnetic resonance images surrounded by marrow edema (Supplementary Figure 3). Knowledge of the typical locations of pelvis stress fractures can improve the likelihood of detection. Sacral stress fractures are typically seen as a linear area of low signal surrounded by marrow edema within the sacral ala and are often bilateral in occurrence. With regard to sacral stress fractures, bone scintigraphy has been shown to be nearly 100% sensitive, while MRI is slightly less sensitive, but has better specificity (Figure 4) [2,11]. CT imaging lacks sensitivity, but the presence of a linear lucency surrounded by sclerosis is diagnostic of a stress fracture.
Figure 2. Stress fracture of tibia: nuclear scintigraphy. Anterior view of the lower legs shows extensive transcortical area of increased uptake indicating a grade IV lesion of the proximal tibial shaft. L: Left; R: Right.
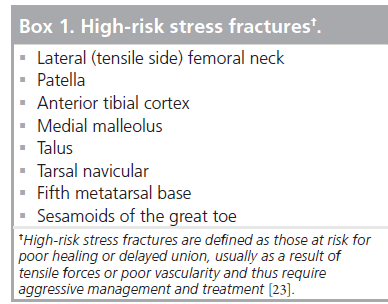
Femur
The femur is the fourth most common location for stress fracture in the running athlete. In a large series of athletes with lower extremity stress fractures, Matheson et al. reported the tibia to be the most common location, accounting for 49% of all stress fractures, with tarsal bones accounting for 25% and the metatarsals 9%. The femur accounted for approximately 7% of stress fractures in this population [5]. Femoral stress fractures can occur in numerous locations including the subchondral region of the femoral head, femoral neck and shaft and occassionally in the region of the distal femoral condyles. Femoral neck stress fractures are considered high-risk fractures with a high rate of complication when the diagnosis is delayed or if the patient is inadequately treated (Box 1) [23].
Femoral head stress fractures
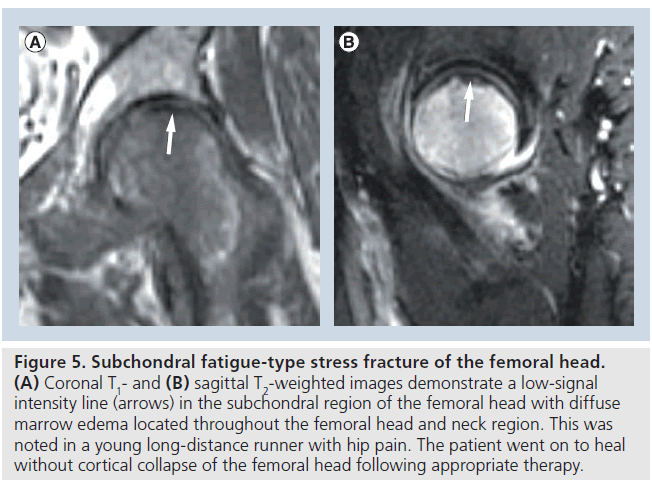
Subchondral stress fracture of the femoral head is an uncommon lesion that has recently been described and in the past was most likely misclassified as either transient osteoporosis or avascular necrosis of the femoral head. Subchondral stress fractures of the femoral head are now a recognized entity separate from avascular necrosis or transient osteoporosis with specific imaging findings. Subchondral insufficiency stress fractures of the femoral head have been reported in the elderly and in postliver transplant patients, while fatigue stress fractures have been reported in the young athletic population and in military recruits [24,25]. These patients present with insidious onset of hip pain that worsens with activity. There is a single report of bilateral femoral head subchondral stress fractures but bilaterality does not appear to be as common as is seen with femoral head avascular necrosis, which is reported in up to 50% of cases [26].
Radiographs are typically normal at the time of presentation. MRI demonstrates an ill-defined low-signal intensity line paralleling the subchondral plate of the femoral head with diffuse marrow edema noted throughout the femoral head (Figure 5). Insufficiencytype subchondral fractures often progress to cortical collapse, leading to secondary osteoarthritis while collapse of the femoral head in fatigue-type subchondral fractures appears to be uncommon [24]. The increased incidence of collapse in insufficiency-type fractures may be associated with inferior quality bone in this subset of elderly patients when compared with the young athletic population. Conservative treatment with nonweight bearing usually leads to resolution of MRI findings and symptoms in the young patient. In patients with hip pain and diffuse subchondral marrow edema on MRI, a thorough search should be made for the presence of a nondisplaced subchondral fracture line paralleling the subchondral plate, which differentiates a subchondral fracture from avascular necrosis or transient osteoporosis [24].
Femoral neck stress fractures
Fatigue stress fractures of the femoral neck most often occur in long-distance runners and in military recruits. Females appear to be more prone to these stress fractures, especially those with the so-called female athlete triad, defined as a female athlete with an eating disorder, amenorrhea and osteoporosis [27–29]. Stress fractures associated with the female athlete triad are considered by many to be a combination of stress and insufficiency-type fractures. The patient complains of an insidious onset of groin pain following a recent increase in activity level or training. The pain is often exacerbated with activity and relieved with rest. Femoral neck stress fractures in athletes (fatigue fractures) usually occur along the medial aspect, basicervical region of the femoral neck involving the compressive trabeculae, while insufficiency fractures of the elderly population occur more commonly along the lateral aspect, subcapital region of the femoral neck involving the tensile trabeculae and present a higher risk for fracture completion [30].
Radiographs will be normal during the early stages of femoral neck stress injury. The earliest findings will be an ill-defined horizontal linear-appearing sclerotic density but this may not be apparent for several weeks following the onset of symptoms (Supplementary Figure 4A). The index of suspicion should be high for femoral neck stress fractures in patients with known risk factors and additional imaging should be ordered early in the evaluation process. If bone scintigraphy is performed, it should be remembered that SPECT imaging is more sensitive than planar bone scintigraphy in the detection of femoral neck stress injury [18]. However, MRI is the preferred imaging modality to assess and grade the extent of stress injury of the femoral neck (Supplementary Figure 4B–4D). The majority of athletes with stress fractures located along the medial side of the femoral neck (compressive trabeculae) can be treated conservatively with rest and nonweight bearing, while elderly patients with lateral- or tensile-sided insufficiency fractures usually require pinning to prevent the catastrophic complication of fracture completion [31,32]. In cases of early detection and imaging, MRI will show marrow edema in the region of the femoral neck. More advanced cases will show an incomplete lowsignal intensity line running perpendicular to the trabeculae of the femoral neck. In the young athlete, the stress fracture is most often seen along the medial aspect, basi-cervical region of the femoral neck, while in the elderly patient the fracture is most often seen laterally in the subcapital region of the femoral neck. In those patients who are appropriately treated, marrow signal changes resolve in 90% of patients within 6 months. Persistent marrow signal greater than 6 months usually indicates a new injury or inadequate rest [33].
Figure 3.Stress fracture of medial tibial metaphysis: MRI appearance. A 19-year-old runner with left knee pain. MRI – (A) coronal T1-weighted image and (B) coronal T2-weighted image with fat saturation – shows a transverse linear area of low signal (arrows) representing a stress fracture of the medial tibial metaphysis with surrounding marrow edema.
Figure 4.>Bilateral sacral insufficiency fractures. (A) Nuclear scintigraphy shows increased uptake within the sacral ala bilaterally. (B) Coronal T1-weighted image shows vertical linear-appearing low-signal abnormality with increased T2 signal in the same distribution seen on (C) the coronal T2-weighted image. This pattern is diagnostic of bilateral sacral insufficiency fractures.
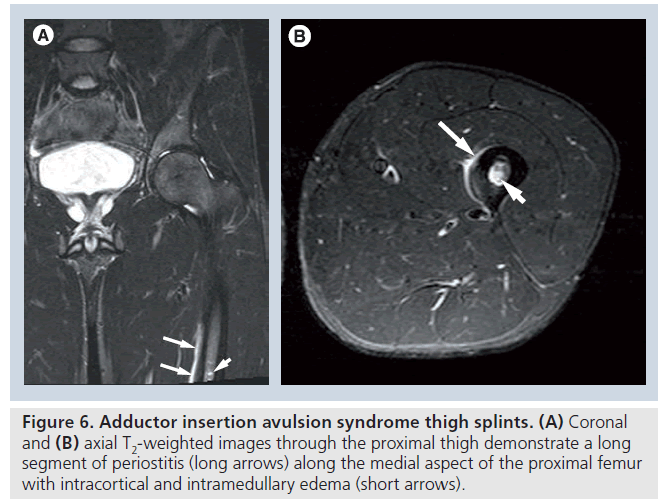
Adductor insertion avulsion syndrome
Adductor insertion avulsion syndrome refers to an overuse injury that results from chronic repetitive traction forces that occur along the medial aspect of the proximal third of the femur at the insertion site of the adductor longus and brevis muscles. The individual typically presents with chronic progressive pain that is vague and difficult to localize but is most often described as involving the groin or proximal medial thigh. The pain is often exacerbated by activity, relieved by rest and is most often reported in female long-distance running or female military recruits, although there are a few reports in male athletes as well. The pathophysiology of adductor insertion avulsion syndrome is similar to that of shin splints and, as a result, this entity is sometimes referred to as thigh splints. The symptoms usually abate with conservative treatment and rest, but if the individual continues the aggravating activity then the early changes of periostitis can progress to a stress fracture of the proximal femoral shaft [34,35].
Figure 5.Subchondral fatigue-type stress fracture of the femoral head. (A) Coronal T1- and (B) sagittal T2-weighted images demonstrate a low-signal intensity line (arrows) in the subchondral region of the femoral head with diffuse marrow edema located throughout the femoral head and neck region. This was noted in a young long-distance runner with hip pain. The patient went on to heal without cortical collapse of the femoral head following appropriate therapy.
Radiographs are typically normal in thigh splints but in advanced cases may demonstrate changes of mild periostitis along the posteromedial aspect of the proximal femoral shaft. Nuclear-medicine bone scan will reveal linear uptake along the proximal medial femoral cortex proximal while in advanced cases, uptake may occur along both the medial and lateral cortex. CT examination will show linear periosteal new bone formation along the posteromedial aspect of the proximal to mid-femur. MRI will show increased T2 signal parallel to the posteromedial cortex of the proximal to midfemur. The length of periostitis can extend as much as half of the length of the femoral shaft. The location of the periostitis in thigh splints is often seen at, or just below, the inferior margin of the field-of-view obtained in a standard hip MRI. As a result, this condition may be missed on a standard MRI of the hip and if adductor insertion avulsion syndrome is suspected clinically, the field-of-view for imaging of the hip should be enlarged to include the proximal third to half of the femur (Figure 6). In advanced cases, abnormal signal may be noted within the medullary space but only rarely within the cortex of the femur at the level of periostitis. The presence of periostitis along the proximal aspect of the femoral shaft should prompt a thorough search for an associated stress fracture (Supplementary Figure 5). Differential diagnosis also includes infection, tumor and osteoid osteoma, which should be easily differentiated in most cases on the basis of clinical presentation and imaging findings [34,35].
Femoral shaft & femoral condyle stress fractures
Femoral shaft stress fractures are uncommon and in some instances may be associated with progression of adductor assertion avulsion stress injury (Supplementary Figure 5) [30]. Stress fractures of the femoral shaft may present with vague groin or proximal thigh pain and there are reports of femoral shaft stress fractures progressing to complete fractures in the setting of continued activity [27]. Distal femoral condyle stress fractures are also uncommon. In long standing cases, radiographs may demonstrate an incomplete fracture line with adjacent periosteal new bone formation and cortical thickening. Early stress changes are best depicted with MRI (Supplementary Figure 6). Stress fractures can also occur in the subchondral bone of the femoral condyles in association with underlying meniscal tears. These stress fractures are typically subchondral in location with extensive surrounding marrow edema. In the past many of these lesions were referred to as spontaneous osteonecrosis but the majority represent true stress or insufficiency fractures. Conservative treatment often results in complete healing without significant sequelae, although some of these lesions may progress to overlying cortical collapse and fragmentation resulting in secondary osteoarthritis of the involved compartment of the knee. MRI typically reveals a low-signal intensity line within the subchondral bone paralleling the cortex of the femoral condyle (Supplementary Figure 7). This entity may be associated with an overlying meniscal tear or may occur as a postsurgical complication following partial meniscectomy.
Patella
Patellar stress fractures appear to be rare, as indicated by their lack of inclusion in two large published series of lower extremity stress fractures in athletes [5,36]. Stress fractures of the patella are typically seen in the young athletic patient but have been reported in a 64‑year-old runner [37,38]. In the young athletic patient, the presence of patellar tendinitis often precedes a stress fracture of the patella [39]. While patellar stress fractures have been reported in runners, they are also reported in weightlifters, basketball players and other athletes. Patients often present with pain localized to the patella and tenderness upon palpation. While rare, there have been case reports of bilateral patellar stress fractures in a marathon runner and in a basketball player [37,40].
Radiographs are typically normal at the time of presentation, and the diagnosis is often delayed until such time as the fracture goes on to completion. At the time of completion, the patient often describes an audible ‘pop’ or ‘cracking’ sensation followed by pain and inability to ambulate [39,41]. Patellar stress fractures are thought to result from the diametric forces of the quadriceps tendon and the patellar tendon. The patella is the largest sesamoid within the body and its unique anatomy within the extensor mechanism results in tensile forces being placed upon the anterior cortex of the patella while the subchondral region of the patella experiences compressive forces. As a result, stress fractures involving the anterior cortex of the patella are at a higher risk for fracture completion. A high index of suspicion is required to make the correct diagnosis prior to fracture completion and imaging with MRI can be beneficial in establishing a timely diagnosis (Supplementary Figure 8). MRI will demonstrate diffuse marrow edema within the patella and the presence of a low-signal intensity transverse line may be identified. Stress fractures typically occur in the transverse plane at the junction of the middle and distal two thirds and fracture completion typically results in displaced fracture fragments. It has also been suggested that symptomatic bipartite patella may be the result of chronic tensile forces across the unfused synchondrosis of the patella [42].
Figure 6.Adductor insertion avulsion syndrome thigh splints. (A) Coronal and (B) axial T2-weighted images through the proximal thigh demonstrate a long segment of periostitis (long arrows) along the medial aspect of the proximal femur with intracortical and intramedullary edema (short arrows).
Tibia
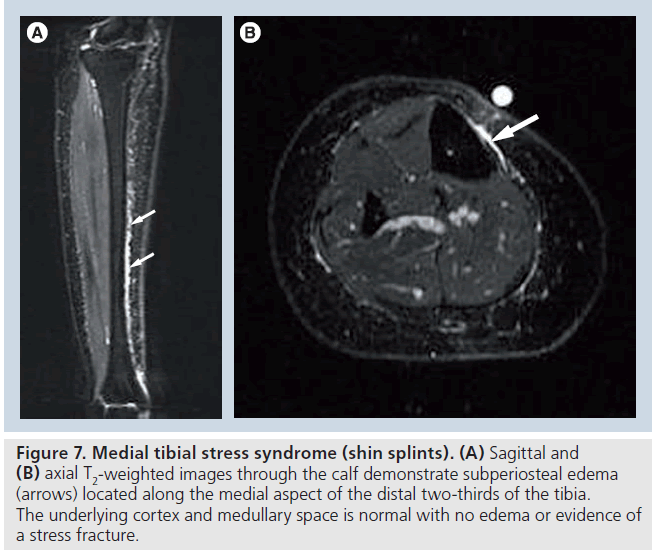
Medial tibial stress syndrome (shin splints)
Medial tibial stress syndrome refers to a condition in which there is stress-related periosteal changes involving the medial aspect of the distal third of the tibia at the origins of the posterior tibialis, soleus and flexor digitorum muscles [43,44]. Athletes report diffuse pain and tenderness located along the posteromedial tibia. The pain is activity related and most often reported late in the season after prolonged training and activity [43]. The individual complains of activity-related pain, relieved with rest. While bone scintigraphy has suggested that this is a clinical entity separate from stress-related changes of the tibia that lead to stress fracture, MRI has demonstrated that medial tibial stress syndrome shin splints is likely to be a stress-related injury that is on a continuum with stress fracture. Medial tibial stress syndrome is thought to represent a periostalgia or possibly a tendonopathy associated with the attachment of the posterior tibialis and soleus muscles [8].
Radiographs are normal in medial tibial stress syndrome; however, bone scintigraphy will reveal longitudinal uptake along the distal third of the tibia, which is diagnostic of shin splints and differs from the more fusiform increased uptake noted with stress fracture. MRI has also been demonstrated to have findings typical of medial tibial stress syndrome and can differentiate shin splints from more severe stress-related changes of the tibia, which can lead to stress fracture. MRI will reveal isolated linear high signal noted along the medial aspect of the tibia indicating subperiosteal edema occasionally associated with minimal soft tissue edema within the adjacent posterior tibialis, soleus and flexor digitorum muscles. However, the tibia is otherwise normal with no cortical or marrow edema and no evidence of a stress fracture with no cortical break or low-signal intensity line noted (Figure 7) [45]. Individuals with medial tibial stress syndrome typically respond to 2–3 weeks of rest with nonsteroidal anti-inflammatories and ice [43,46,47].
Figure 7.Medial tibial stress syndrome (shin splints). (A) Sagittal and (B) axial T2-weighted images through the calf demonstrate subperiosteal edema (arrows) located along the medial aspect of the distal two-thirds of the tibia. The underlying cortex and medullary space is normal with no edema or evidence of a stress fracture.
Proximal tibial metaphysis
Stress fractures involving the proximal medial tibial metaphyseal region appear to be uncommon, but are noted in two patient populations. First, insufficiency stress fractures have been noted in the elderly population associated with internal derangement of the medial compartment of the knee, and second, in the young running athlete there are reports of fatigue-related stress fractures that occur in this region. Stress changes in the proximal medial tibia are most often seen in long-distance runners and appear to be associated with certain intrinsic risk factors, including limb malalignment, hyperpronated foot and cavus deformity [38,48]. While most cases appear to correlate to one of these risk factors, there are reports of long distance runners who develop stress fractures in this location with no reported risk factor other than increased activity level.
Radiographs are often normal early in the course of injury, whereas late findings reveal a sclerotic transverse linear density typically located along the posterior peripheral aspect of the proximal tibial metaphysis. Radiographic findings are usually subtle, even in advanced cases. MRI will demonstrate diffuse marrow edema throughout the medial tibial metaphysis with an ill-defined irregular linear transverse low-signal intensity abnormality that is typically located along the posterior and peripheral aspect of the proximal medial tibial metaphysis. MRI is an excellent tool for identifying the extent of stress fracture and in detecting the presence of stress-related changes long before radiographs show any detectable abnormality [48]. Patients with proximal medial tibial stress fracture can present with a confusing clinical picture and are often suspected of having either internal derangement of the knee or distal pes anserine tendinosis/bursitis. MRI is capable of differentiating between these separate entities (Supplementary Figure 9) [38].
Tibial shaft
The tibial shaft is the most common site for stress fractures in runners and while stress fractures can occur in nearly any location along the shaft of the tibia, they most often occur along the posteromedial cortex in the region of the compressive trabeculae [30,49,50]. Appropriate history and clinical examination is important in establishing the correct diagnosis. Individuals typically complain of insidious onset of pain, worsened with activity and relieved with rest. Pain is usually localized to the area of the stress fracture and history often reveals risk factors such as an abrupt increase in training or components of the female athlete triad. As the stress-related injury progresses, pain becomes more severe, occurring earlier in the course of the activity and persisting longer after cessation of activity. Physical examination will reveal point tenderness over the fracture site and the presence of redness or swelling may be observed [43].
As is typical for most stress fractures, radiographs will be normal during the first 2–3 weeks of symptoms. Radiographic abnormalities will first appear at the site of palpable tenderness. Early radiographic abnormalities include a focal area of fluffy periostitis. Development of an actual stress fracture will eventually result in a subtle transverse linear lucency, and long-term radiographic findings may include a segment of cortical thickening (Supplementary Figure 10A). Nuclear medicine bone scan will demonstrate a focal area of increased uptake and the aforementioned grading system can be used to determine the extent of injury and to aid in directing therapy (Supplementary Figure 10B). Early in the course of injury, MRI will show subtle increased T2 signal on short TI inversion recovery or T2‑weighted images with fat saturation. As the stress response progresses, the marrow signal becomes more diffuse with an abnormal T1‑weighted signal developing. Eventually, a low-signal intensity line will become evident (Supplementary Figure 11).
Two types of mid-tibial shaft fractures deserve special attention. A stress fracture involving the anterior cortex of the middle third of the tibial shaft is particularly problematic (Supplementary Figure 12). These fractures appear to have a higher association with jumping activities rather than running and have been described in activities such as hurdling, basketball and ballet [51–53]. Stress fractures of the anterior tibial cortex are notoriously difficult to detect on conventional radiographs. When abnormal, radiographs will reveal a subtle transverse linear lucency within the anterior cortex, sometimes referred to as the ‘dreaded black line’ [8,43,51]. MRI should be performed early in the evaluation of a suspected anterior tibial cortex lesion. The combination of tensile forces and hypovascularity of this portion of the tibia places these fractures at particular risk for delayed union or nonunion. Avascular necrosis may develop at the site of the fracture. Radiographs and MRI may show sclerotic margins on either side of a persistent transverse fracture involving the anterior tibial cortex, but periosteal new bone formation (callous) is often absent. While most fractures of the compressive side of the tibia respond very well to rest, anterior tibial cortex (tensile) stress fractures often require rest for up to 4–6 months and, if nonunion develops, more aggressive therapy is often required, which may include external electrical stimulation, excision of the fracture followed by bone grafting and intramedullary nailing [23].
The second subset of the tibial shaft stress fracture that deserves special attention is the longitudinal stress fracture (Supplementary Figure 13). This is an unusual tibial stress fracture that rather than extending transverse to the long axis of the tibial shaft extends longitudinally along the long axis of the tibia [54]. The fracture typically involves either the anterior or the posterior cortex and extends several centimeters in length. The fracture is difficult to detect on radiographs, but is easily identified on CT and MRI. A linear area of cortical disruption is visualized on multiple sequential axial sections located along either the anterior or posterior cortex. MRI has the advantage of demonstrating marrow edema and subperiosteal edema that typically extends several centimeters in length paralleling the longitudinal fracture with soft tissue edema often located within the overlying musculature [55]. Those unfamiliar with the longitudinal stress fracture of the tibia can easily misinterpret the long segment of abnormality on either MRI or bone scintigraphy as an aggressive osseous lesion and miss the true nature of this lesion.
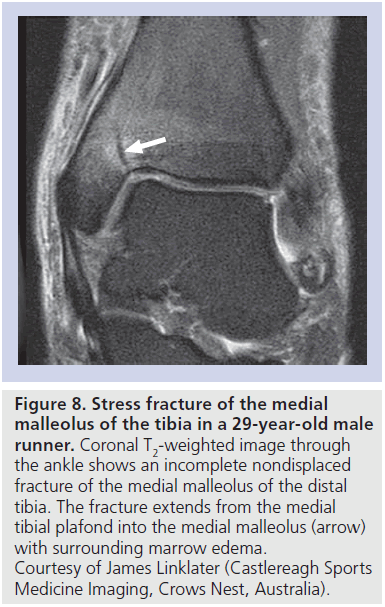
A stress fracture of the medial malleolus is an unusual tibial stress fracture that is most often seen in runners or jumping athletes. Patients present with medial ankle pain that is exacerbated by activity and insidious in onset. The patient is tender to palpation over the medial malleolus. The fracture is typically vertical or obliquely oriented arising at the junction of the medial tibial plafond and the medial malleolus [56]. Radiographs are often normal early in the course of injury. MRI best depicts the area of marrow edema and an obliquely oriented low-signal intensity line extending from the medial tibial plafond into the medial malleolus (Figure 8). This is considered a highrisk injury as the shearing forces across this region of the ankle can lead to fracture completion and nonunion [23]. Long-standing cases or development of nonunion will require fixation with cancellous screws and possible bone grafting [57]. Stress fractures can also occur in the subchondral bone of the distal tibia (Supplementary Figure 14).
Figure 8.Stress fracture of the medial malleolus of the tibia in a 29-year-old male runner. Coronal T2-weighted image through the ankle shows an incomplete nondisplaced fracture of the medial malleolus of the distal tibia. The fracture extends from the medial tibial plafond into the medial malleolus (arrow) with surrounding marrow edema. Courtesy of James Linklater (Castlereagh Sports Medicine Imaging, Crows Nest, Australia).
Fibula
Stress fractures of the fibula are unusual but, when they occur, are most often seen in highend athletes and, in particular, long distance or marathon runners. They may be seen in association with stress fractures of the tibia. Most fibular stress fractures occur in the region of the distal shaft and have radiographic and MRI appearances similar to tibial stress fractures (Supplementary Figure 15).
Tarsal bones
In runners, stress fractures of the tarsal bones are second in frequency only to the tibia and metatarsals [5,58]. Therefore, there should be a high index of suspicion for osseous stress injuries in the runner who presents with hindfoot or ankle pain. The anatomy of the foot and ankle is complex and clinical presentations can overlap between patients who present with osseous changes versus soft tissue overuse injuries. Imaging often plays a vital role in determining the injured structure and the source of pain. While many of the osseous stress injuries at the level of the hindfoot and ankle are treated conservatively, there are a few that are considered high-risk fractures. These include the talus, tarsal navicular and base of the fifth metatarsal, which may require aggressive therapy to prevent significant complications [23]. During the early stages of injury radiographs are usually normal, while MRI often shows nonspecific ill-defined marrow edema. In runners with foot and ankle pain, MRI may demonstrate widespread marrow edema within several bones. Once a stress fracture develops, MRI will show a focal linear area of low-signal abnormality surrounded by extensive marrow edema. A well-documented clinical history and physical examination will help accurately identify an early stress fracture. Knowledge of the typical location of stress fractures in the ankle and hindfoot will also aid in the detection of these lesions on radiographs and MRI.
Stress fractures of the calcaneus usually present with heel pain and can be difficult to differentiate clinically from plantar fasciitis. Therefore, imaging can play an important role in establishing the correct diagnosis. The calcaneus is the largest of the tarsal bones and is composed of a thin rim of cortical bone surrounding cancellous bone, which comprises the majority of the bone. As a result, radiographic imaging will demonstrate the typical appearance of cancellous stress response, which is an ill-defined linear sclerotic density oriented perpendicular to the normal trabeculae (Supplementary Figure 1B). The sclerotic density, which represents endosteal new bone formation in response to the abnormal stress, is typically located in the posterior calcaneal process and is vertically oriented. MRI will typically show diffuse marrow edema adjacent to the stress fracture (Supplementary Figure 16). While the majority of calcaneal stress fractures occur in the posterior process, they can also occur in the middle and anterior portions of the calcaneus [59]. In addition, stress fractures of the calcaneus have been reported in association with posterior subtalar facet coalition probably resulting from abnormal forces placed on the hindfoot as a result of the coalition [60]. Patients with calcaneal stress fractures in the absence of coalition typically respond well to conservative therapy.
Cuboidal stress fractures are less common than calcaneal stress fractures and typically present with lateral foot/ankle pain and may mimic lateral collateral ligament or peroneal tendon pathology. They most commonly occur in military recruits and runners. Stress fractures of the cuboid are difficult to detect on radiographs. The cuboid is composed primarily of cancellous bone and, therefore, when visualized, the stress fracture will appear as a sclerotic density perpendicular to the normal trabeculae. On MRI, marrow edema is the most common finding early in the injury process with an illdefined low-signal intensity line seen within the medullary space once an actual stress fracture develops (Supplementary Figures 17 & 18) [61]. The cuboid, similarly to the calcaneus, responds well to conservative treatment.
Stress fractures of the talus are rare but can occur in various locations throughout the talus, including the lateral talar process, the subchondral region of the talar dome, posterior talar process, talar neck and subchondral region of the talar head (Supplementary Figure 19). Talar stress fractures are considered high risk as they have a propensity to experience delayed or suboptimal healing [23,62]. Subchondral stress fractures may progress to cortical collapse and subsequent osteoarthritis, with this complication reported in roughly half of all patients with talar stress fractures with middle-term followup (Supplementary Figure 20) [63]. Stress fractures of the cuneiforms have also been reported, and appear to have an association with plantar fascia injury, large body habitus and either excessive training or onset of a new training regimen [64].
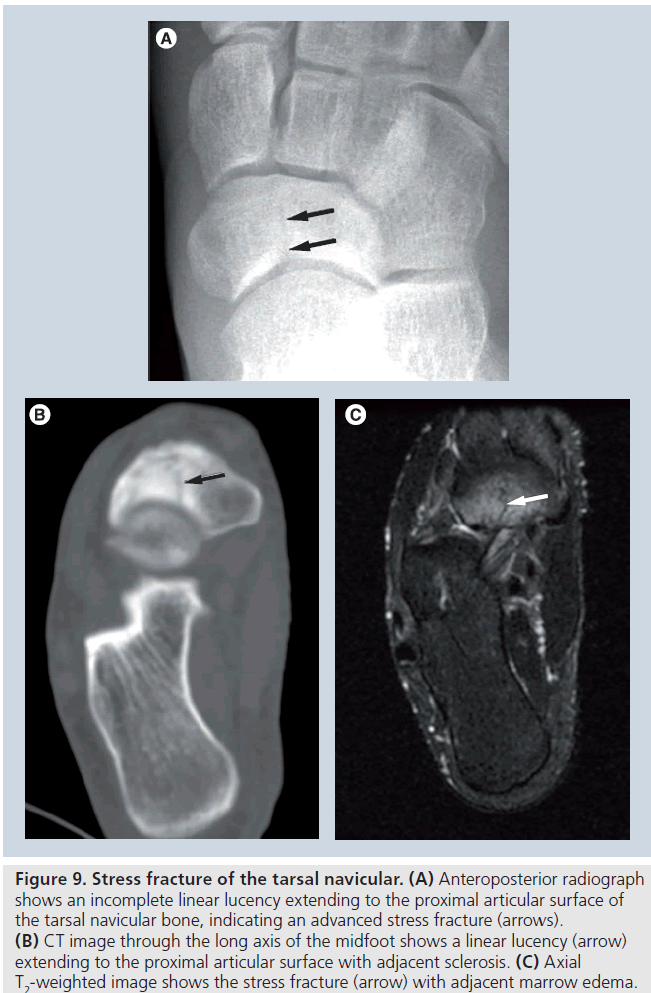
Stress fractures of the tarsal navicular bone were once considered rare, but are now being recognized with increasing frequency and represent a high-risk stress fracture that can result in catastrophic complications when the diagnosis is delayed [65]. These stress fractures occur primarily in long-distance runners and in elite athletes. The signs and symptoms are often nonspecific; this, coupled with the fact that radiographs are typically normal early in the injury process, often leads to a significant delay in diagnosis, many weeks or even months after the onset of symptoms [9,66]. A high degree of clinical suspicion coupled with an appropriate imaging strategy will allow for the earliest possible diagnosis and ensure optimal clinical outcome.
Patients typically present with vague insidious onset of midfoot pain, exacerbated by running. The pain initially improves with rest but, over time, becomes more constant and severe. Point tenderness is often detected overlying the fracture site. Local redness and swelling may occasionally be observed. The fracture is most often located within the central third of the tarsal navicular bone originating at the proximal articular surface. As the fracture progresses, it extends towards the distal articular surface, eventually leading to a complete fracture with displacement of the fracture fragments, which can result in a disabling secondary osteoarthritis of the midfoot, preventing return to preinjury activity level. Risk factors include a short first metatarsal combined with a relatively long second metatarsal. Tarsal navicular stress fractures often occur in conjunction with stress fractures of the second or third metatarsal shaft. Radiographs are typically normal at an early stage, while late findings include a linear lucency located in the proximal aspect of the central third of the navicular bone with or without surrounding sclerosis (Figure 9A). Bone scintigraphy will demonstrate increased uptake within the tarsal navicular bone [67]. CT and MRI are equally beneficial in detecting and determining the extent of the actual stress fracture but MRI may show marrow edema in early cases prior to development of a discrete fracture line (Figure 9B & 9C) [9,68]. Tarsal navicular stress fractures detected early are often initially treated with conservative therapy to include limitation of activity, possibly with cast immobilization and nonweight bearing. Extensive fractures or those that do not respond appropriately to conservative measures may require internal fixation with a compression screw. Cross-sectional imaging will demonstrate complications such as nonunion of the fracture, avascular necrosis of fragments and secondary osteoarthritis (Supplementary Figure 21). Imaging findings on MR and CT often lag many months behind clinical improvement in patients with tarsal navicular stress fractures [9].
Figure 9.Stress fracture of the tarsal navicular. (A) Anteroposterior radiograph shows an incomplete linear lucency extending to the proximal articular surface of the tarsal navicular bone, indicating an advanced stress fracture (arrows). (B) CT image through the long axis of the midfoot shows a linear lucency (arrow) extending to the proximal articular surface with adjacent sclerosis. (C) Axial T2-weighted image shows the stress fracture (arrow) with adjacent marrow edema
Metatarsals
Fractures of the metatarsals are common amongst runners and military recruits with the most common location for the fracture occurring at the mid-shaft or neck of the second or third metatarsal. These fractures are typically transverse in orientation. Stress fractures occurring at the base of the fifth metatarsal have been shown to occur more commonly in basketball players and typically occur approximately 1.5 cm distal to the proximal tip of the fifth metatarsal. These fractures typically begin along the lateral cortex and progress medially until the fracture goes on to completion. Stress fractures at the base of the fifth metatarsal are considered high-risk fractures and often undergo poor or delayed healing secondary to the relative avascularity of this area of bone. Another contributing factor is the pull of the peroneus brevis tendon inserting on the base of the fifth metatarsal, which can place a separating force across the fracture site.
Early radiographs are typically normal, but within a few weeks after onset of symptoms, radiographs may demonstrate a transverse linear lucency. As the fracture progresses, it may become complete with subtle displacement of the fracture fragments. In more chronic injury, fluffy periosteal new bone will be seen surrounding the fracture with eventual cortical remodeling. Bone scans will demonstrate increased uptake at the level of abnormality. MRI has been demonstrated to show marrow edema early in the course of stress changes and it has been suggested that the use of MRI can play a role in prevention of metatarsal stress fractures in collegiate basketball players and other athletes prone to these injuries, thus diagnosing injury early and minimizing time away from the sport (Supplementary Figure 22) [69]. Late findings with MRI will show a transverse low-signal intensity line at the location of the fracture with eventual periosteal new bone formation and adjacent cortical thickening (Supplementary Figure 23). Marrow edema may also be noted in additional locations of the forefoot or midfoot, indicating subclinical areas of early stress injury. Soft tissue edema is often identified within the soft tissues of the forefoot adjacent to the stress fracture. The majority of metatarsal stress fractures are treated with conservative measures of suspension of activity or nonweight bearing casts. Nonunion at the base of the fifth metatarsal will appear on radiographs or CT as a persistent transverse lucency with sclerotic margins on either side of the fracture and nonunion may require internal fixation with bone grafting (Supplementary Figure 24) [2].
Phalanges & sesamoides
Stress fractures of the proximal phalanx of the great toe are rare and appear to be associated with anatomic malalignment of the foot. These stress fractures occur most commonly along the medial aspect of the base of the phalanx near the attachment of the medial collateral ligament of the first metatarso–phalangeal joint and at the attachment site of the abductus tendon. The stresses of these structures are increased in patients with hallux valgus, which results in a bowstringing effect of the extensor hallux longus tendon resulting in increased shearing forces at the medial aspect of the base of the proximal phalanx [70]. These fractures, while rare, appear to occur in exercises that involve sprinting, jumping and standing on ones tip-toes and show a strong association with underlying hallux valgus deformity [70,71]. Radiographs will show an obliquely oriented lucency extending through the medial aspect of the base of the proximal phalanx and often extend to the proximal articular surface. If the fracture progresses to completion, treatment will typically require open reduction and internal fixation with good results reported [70].
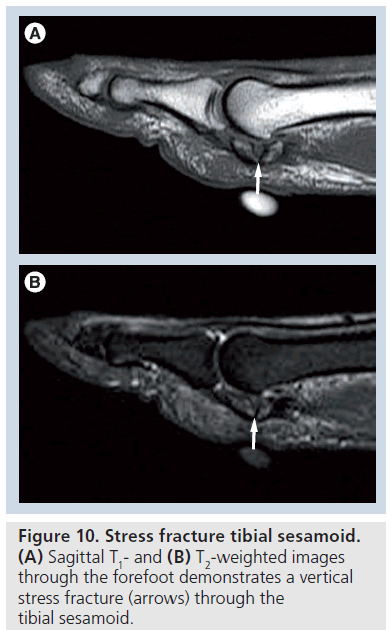
The hallucal sesamoidal complex contains two separate sesamoid bones, the medial (tibial) sesamoid is the larger of the two and is embedded within the medial head of the flexor hallucis brevis tendon and typically directly underlies the first metatarsal head. The lateral (fibular) sesamoid is the smaller of the two sesamoids and is embedded within the lateral head of the flexor hallucis brevis tendon. The unique anatomy of the hallucal sesamoidal complex helps to disperse excessive forces that occur across the first metatarso–phalangeal joint, which can occur during the push-off phase of the gait, thus providing protection to the first metatarsal head. Athletes who are exposed to excessive running, jumping or forced dorsiflexion of the forefoot are at risk of stress fracture of the sesamoids. While either sesamoid can develop a stress fracture, they occur much more commonly within the medial sesamoid, which directly underlies the first metatarsal head, while the lateral position of the fibular sesamoid will allow it to slip between the first and second metatarsal heads during forced dorsiflexion, affording a degree of protection to the fibular sesamoid.
Radiographs may demonstrate a focal linear lucency usually vertically oriented with or without adjacent sclerosis. In chronic cases, the fracture may progress to completion with resultant separation of the fragments. Bone scan will demonstrate focal uptake within the abnormal sesamoid. In the early stress injury, MRI will show isolated edema within the sesamoid (Supplementary Figure 25). More advanced cases will show a low-signal intensity line, vertically oriented with eventual fragmentation and separation of fracture fragments (Figure 10). Sesamoidal stress fractures are considered high risk as they have a tenuous blood supply and can progress to avascular necrosis. Avascular necrosis will appear as fragmentation with increased density within the nonvascularized fragments (Supplementary Figure 26). A bipartiteappearing medial sesamoid can occur in up to 30% of cases and can usually be differentiated on the basis of smooth -well corticated margins of the bipartite sesamoid (Supplementary Figure 27). Bipartite sesamoids usually present bilaterally and are similar in appearance. Therefore, bilateral radiographs may aid in initial evaluation. In questionable cases, nuclear scintigraphy or MRI can be used to evaluate for increased uptake or the presence of marrow edema in abnormal sesamoids [72].
Figure 9.Stress fracture tibial sesamoid. (A) Sagittal T1- and (B) T2-weighted images through the forefoot demonstrates a vertical stress fracture (arrows) through the tibial sesamoid.
Conclusion
Imaging plays a vital role in the evaluation of suspected stress-related osseous injuries in the running athlete. Radiographs are often normal at the time of initial presentation and a high index of suspicion is required to proceed to appropriate imaging using MRI or nuclear scintigraphy. Knowledge of the various stress injuries will aid in the early detection and treatment thus preventing progression to more serious injury in the high-risk stress fractures. Early detection and diagnosis is also important in minimizing recovery time and limiting loss of playing time in various sports that require running.
Future perspective
Early studies show promise in the utilization of MRI in the detection of early subclinical stress- related injuries, which can be used to alter training and activity levels in an attempt to prevent injury. In the future, imaging may be utilized to screen for subclinical injury in highperformance athletes in an attempt to prevent debilitating injury and loss of playing time.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received orpending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Papers of special note have been highlighted as:
* of interest
* of considerable interest
References
- Buist I, Bredeweg SW, Lemmink KA, van Mechelen W, Diercks RL: Predictors of running-related injuries in novice runners enrolled in a systematic program: a prospective cohort study. Am. J. Sports Med. 38(2), 273–280 (2009).
- Umans H, Pavlov H: Stress fractures of the lower extremities. Seminars Roentgen. 29(2), 176–193 (1994).
- Daffner RH: Stress fractures: current concepts. Skelet. Radiol. 2, 221–229 (1978).
- Cooper KL: Insufficiency stress fractures. Curr. Probl. Diagn. Radiol. 23(2), 29–68 (1994).
- Matheson GO, Clement DB, McKenzie DC et al.: Stress fractures in athletes: a study of 320 cases. Am. J. Sports Med. 15(1), 46–58 (1987).
- Wilson ES, Katz FN: Stress fractures: an analysis of 250 consecutive cases. Radiology 92, 481–486 (1969).
- Lapp JM: Pelvic stress fracture: assessment and risk factors. J. Manipulative Physiol. Ther. 23(1), 52–55 (2000).
- Wilder RP, Sethi S: Overuse injuries: tendonopathies, stress fractures, compartment syndrome, and shin splints. Clin. Sports Med. 23, 55–81 (2004).
- Sanders TG, Williams PM, Vawter KW: Stress fracture of the tarsal navicular. Mil. Med. 169, viii–xii (2004).
- Clayer M, Krishnan J, Lee WK, Tamblyn P: Longitudinal stress fracture of the tibia: two cases. Clin. Radiol. 46(6), 401–404 (1992).
- Wall J, Feller JF: Imaging of stress fractures in runners. Clin. Sports Med. 25, 781–802 (2006).
- Bergman AG, Fredericson M. MR imaging of stress reactions, muscle injuries and other overuse injuries in runners. Magn. Reson. Imaging Clin. N. Am. 7(1), 151–174 (1999).
- Saifuddin A, Chalmers AG, Butt WP: Longitudinal stress fractures of the tibia: MRI features in two cases. Clin. Radiol. 49(7), 490–495 (1994). & Discusses the imaging findings of longitudinal stress fractures of the tibia, which can be easily misinterpreted as a different lesion.
- Fayad LM, Kawamoto S, Kamel IR et al.: Distinction of long bone stress fractures from pathologic fractures on cross-sectional imaging: how successful are we? AJR Am. J. Roentgen. 185, 915–924 (2005).
- Zwas ST, Elkanovitch R, Frank G: Interpretation and classification of bone scintigraphic findings in stress fractures. J. Nucl. Med. 28(4), 452–457 (1987). & Discusses the standard bone scintigraphic classification system for stress fractures.
- Gaeta M, Minutoli F, Scribano E et al.: CT and MR imaging findings in athletes with early tibial stress injuries: comparison with bone scintigraphy findings and emphasis on cortical abnormalities. Radiology 235, 553–561 (2005).
- Wen DY, Propeck T, Singh A: Femoral neck stress injury with negative bone scan. Am. J. Board Fam. Pract. 16, 170–174 (2003).
- Bryant LR, Song WS, Banks KP, Bui-Mansfield LT, Bradley YC: Comparison of planar scintigraphy alone and with SPECT for the initial evaluation of femoral neck stress fracture. AJR Am. J. Roentgen. 191, 1010–1015 (2008).
- Bal BS, Sandow T: Bilateral femoral neck fractures with negative bone scans. Orthopedics 19, 974–976 (1996).
- Sterling JC, Webb RF Jr, Meyers MC, Calvo RD: False negative bone scan in a female runner. Med. Sci. Sports Exerc. 25, 179–185 (1993). & Important article that demonstrates the possibility of a false-negative bone scan in stress-related injuries in runners.
- Prather JL, Nusynowitz HA, Snowdy HA, Hughes AD, McCartney WH, Bragg RJ: Scintigraphic findings in stress fractures. J. Bone Joint Surg. Am. 59, 869–874 (1977).
- Huan DW, Kettner NW, Yochum DC, Gree RL: Sacral fatigue fracture in a female runner: a case report. J. Manipulative Physiol. Ther. 30(3), 228–233 (2007).
- Boden BP, Osbahr DC: High-risk stress fractures: evaluation and treatment. J. Am. Acad. Orthop. Surg. 8(6), 344–353 (2000). & Discussion of high-risk stress fractures, imaging and treatment options.
- Lee YK, Yoo JJ, Koo KH et al.: Collapsed subchondral fatigue fracture of the femoral head. Orthop. Clin. N. Am. 40, 259–265 (2008).
- Iwasaki K, Yamamoto T, Nakashima Y et al.: Subchondral insufficiency fracture of the femoral head after liver transplant. Skeletal Radiol. 38(9), 925–928 (2009).
- Sudo A, Hasegawa M, Kato K, Uchida A: Bilateral subchondral insufficiency fracture of the femoral head. Orthopedics 31(4), 399 (2008).
- Farkas TA, Zane RD: Comminuted femur fracture secondary to stress during the Boston marathon. J. Emergency Med. 31(1), 79–82 (2006).
- Griffin LY: Stress fracture: with early diagnosis, rest is curative. J. Musculoskel. Med. 12, 12 (1995).
- DeFranco MJ, Recht M, Schils J, Parker RD: Stress fractures of the femur in athletes. Clin. Sports Med. 25, 89–103 (2006). & Discussion of the female athlete triad.
- Boden BP, Speer KP: Femoral stress fracture. Clin. Sports Med. 16(2), 307–317 (1997).
- Dorne HL, Lander PH: Spontaneous stress fractures of the femoral neck. AJR Am. J. Roentgen. 144, 343–347 (1984).
- Kerr PS, Johnson DP: Displaced femoral neck stress fracture in a marathon runner. Injury 26(7), 491–493 (1995).
- Slocum KA, Gorman JD, Puckett ML, Jones SB: Resolution of abnormal MR signal intensity in patients with stress fractures of the femoral neck. AJR Am. J. Roentgen. 168, 1295–1299 (1997).
- Lawande MA, Sankhe S, Pungavkar SA, Patkar DP: Adductor insertion avulsion syndrome with stress fracture of femoral shaft: MRI findings. 51(Spec No.), B104–B106 (2007). & Discusses the clinical and imaging findings in adductor insertion avulsion syndrome: a little known and often misdiagnosed stress injury.
- Anderson MW, Kaplan PA, Dussault RG: Adductor insertion avulsion syndrome (thigh splints): spectrum of MR imaging features. AJR Am. J. Roentgen. 177, 673–675 (2001).
- Orava S, Puranen J, Ala-Ketol L: Stress fractures caused by physical exercise. Acta Orthop. Scand. 49, 19–27 (1978).
- Carneiro M, Nery CA, Mestriner LA: Bilateral stress fracture of the patellae: a case report. Knee 13, 164–166 (2006).
- Drabicki RR, Greer WJ, DeMeo PJ: Stress fractures around the knee. Clin. Sports Med. 25, 105–115 (2006).
- Crowther MAA, Mandal A, Sarangi PP: Propagation of stress fracture of the patella. Br. J. Sports Med. 39, e6 (2005).
- Tibone JE, Lombardo SJ: Bilateral fracture of the inferior pole of the patellae in a basketball player. Am. J. Sports Med. 9, 215–216 (1981).
- Teitz CC, Harrington RM: Patellar stress fracture. Am. J. Sports Med. 20, 761–765 (1992).
- Ogden JA, McCarthy SM, Joki P: The painful bipartite patella. J. Pediatr. Orthop. 2(3), 263–269 (1982).
- Edwards PH, Wright ML, Hartman JF: A practical approach for the differential diagnosis of the chronic leg pain in the athlete. Am. J. Sports Med. 33, 1241–1249 (2005).
- Spitz DJ, Newberg AH: Imaging of stress fractures in the athlete. Magn. Reson. Imaging Clin. N. Am. 11, 323–339 (2003).
- Aoki Y, Yasuda K, Tohyama H, Ito H, Minami A: Magnetic resonance imaging in stress fracture and shin splints. Clin. Orthop. Relat. Res. 421, 260–267 (2004).
- Moore MP: Shin splints: diagnosis, management, prevention. Postgrad. Med. 83(1), 199–200, 203–205, 208–210 (1988).
- Pell RF, Khanuja HS, Cooley GR: Leg pain in the running athlete. J. Am. Acad. Orthop. Surg. 12, 396–404 (2004).
- Vossinakis IC, Tasker TPB: Stress fracture of the medial tibial condyle. Knee 7, 187–190 (2000).
- Brukner P, Bradshaw C, Khan KM, White S, Crossley K: Stress fractures: a review of 180 cases. Clin. J. Sport Med. 6, 85–89 (1996).
- Iwamoto J, Takeda T: Stress fractures in athletes: review of 196 cases. J. Orthop. Sci. 8, 273–278 (2003).
- Beck BR: Tibial stress injuries: an aetiological review for the purposes of guiding management. Sports Med. 26, 265–279 (1998).
- Schneider HJ, King AY, Bronson JL et al.: Stress injury and developmental changes of lower extremities in ballet dancers. Radiology 113, 627–738 (1974).
- Daffner RH. Anterior tibial striations. AJR Am. J. Roentgen. 143, 651–653 (1984).
- Jeske J, Demos T, Vade A et al.: Longitudinal tibial stress fracture. Orthopedics 19, 66–70 (1996).
- Umans H, Kaye J: Longitudinal stress fractures of the tibia: diagnosis by magnetic resonance imaging. Skelet. Radiol. 25, 319–324 (1996). & Discussion of longitudinal stress fractures of the tibia, a commonly misdiagnosed stress injury.
- Shelbourne KD, Fisher DA, Rettig AC, McCarroll JR: Stress fractures of the medial malleolus. Am. J. Sports Med. 16, 60–63 (1988).
- Reider B, Falconiero R, Yurkofsky J: Nonunion of a medial malleolus stress fracture: a case report. Am. J. Sports Med. 21, 478–481 (1993).
- Yale J: A statistical analysis of 3,657 consecutive fatigue fractures of the distal lower extremities. J. Am. Podiatr. Med. Assoc. 68, 739–748 (1976).
- Sormaala MJ, Niva MH, Kiuru MJ, Mattila VM, Pihlajamaki HK: Stress injuries of the calcaneus detected with magnetic resonance imaging in military recruits. J. Bone Joint Surg. Am. 88(10), 2237–2242 (2006).
- Moe DC, Choi JJ, Davis KW: Posterior subtalar facet coalition with calcaneal stress fracture. AJR Am. J. Roentgen. 186, 259–264 (2006).
- Dodson NB, Dodson EE, Shromoff PJ: Imaging strategies for diagnosing calcaneal and cuboid stress fractures. Clin. Podiatr. Med. Surg. 25, 183–201 (2008).
- Brockwell J, Yeung Y, Griffith JF: Stress fractures of the foot and ankle. Sports Med. Arthrosc. 17(3), 149–159 (2009).
- Sormaala MJ, Niva MH, Kiuru MJ, Mattila VM, Pihlajamaki HK: Outcomes of stress fractures of the talus. Am. J. Sports Med. 34(11), 1809–1814 (2006).
- Bui-Mansfield LT, Thomas WR: Magnetic resonance imaging of stress injury of the cuneiform bones in patients with plantar fascia. J. Comput. Assist. Tomogr. 33(4), 593–596 (2009).
- Jones MH, Amendola AS: Navicular stress fractures. Clin. Sports Med. 25, 151–158 (2006).
- Torg JS, Pavlov H, Cooley LH et al.: Stress fractures of the tarsal navicular. J. Bone Joint Surg. Am. 64, 700–712 (1982).
- Goergen TG, Venn-Watson EA, Rossman DJ, Resnick D, Gerber KH: Tarsal navicular stress fractures in runners. AJR Am. J. Roentgen. 136, 201–203 (1981).
- Kiss ZS, Khan KM, Fuller PJ: Stress fractures of the tarsal navicular bone: CT findings in 55 cases. AJR Am. J. Roentgen. 160, 111–115 (1993).
- Majors N: Role of MRI in prevention of metatarsal stress fractures in collegiate basketball players. AJR Am. J. Roentgen. 186, 255–258 (2006).
- Yokoe K, Kameyama Y: Relationship between stress fractures of the proximal phalanx of the great toe and hallux valgus. Am. J. Sports Med. 32(4), 1032–1034 (2004).
- Shiraishi M, Mizuta H, Kubota K et al.: Stress fracture of the proximal phalanx of the great toe. Foot Ankle 14, 28–34 (1993).
- Sanders TG, Rathur SK: Imaging of painful conditions of the hallucal sesamoidal complex and plantar capsular structures of the first metatarsophalangeal joint. Radiol. Clin. N. Am. 46, 1079–1092 (2008).