Research Article - Diabetes Management (2025) Volume 15, Issue 1
Glucose control in older adults with diabetes following intra-articular and epidural triamcinolone acetonide injections
- Corresponding Author:
- Connie Valdez
Department of Pharmacy and Pharmaceutical Sciences, Skaggs School of Pharmacy and Pharmaceutical Sciences, University of Colorado, 12850 East Montview Blvd., C-238, Aurora, United States
E-mail: Connie.Valdez@cuanschutz.edu
Received: 02-Sep-2025, Manuscript No. FMDM-25-170606; Editor assigned: 05-Sep-2025, PreQC No. FMDM-25-170606 (PQ); Reviewed: 19-Sep-2025, QC No. FMDM-25-170606; Revised: 01-Oct-2025, Manuscript No. FMDM-25-170606 (R); Published: 28-Oct-2025, DOI: 10.37532/1758-1907.2025.15(1).689-694.
Abstract
Corticosteroid injections are widely used as part of a multimodal approach to manage pain in various areas of the body. These injections are often considered prior to resorting to more invasive options such as surgery and joint replacement. Common indications for corticosteroid injections include osteoarthritis, shoulder pain, and lumbar spine pain. Corticosteroid injections are typically administered Intra-Articular (IA) or epidural, and include agents such as methylprednisolone acetate, and triamcinolone acetonide, which is available as Immediate-Release (TA-IR) and Extended-Release (ER). Of these agents, TA-IR is the most studied and widely available and will be the primary focus of this review. Epidural and IA triamcinolone are absorbed both locally and systemically and have prolonged clearance compared to intravenous triamcinolone. Since metabolic abnormalities, including hyperglycemia, are common with corticosteroids, patients with diabetes who receive IA and epidural corticosteroid injections could be at higher risk of glucose excursions compared to patients without diabetes. The duration and extent of this risk, however, is not well described and needs to be further examined to help delineate the risks of corticosteroid injections in patients with diabetes.
Keywords
Hyperglycemia, Immediate release, Extended release, Lumbar spine pain
Introduction
The influence of triamcinolone injections on blood glucose can be highly variable. Factors that contribute to this variability include triamcinolone dose, formulation (extended release (ER) vs. Immediate Release (IR)), injection location, degree of baseline diabetes control and requirement for insulin [1].
Objective
The objective of this review is to evaluate recent literature, describing the use of IA and epidural triamcinolone injections for pain management and the effects on blood glucose control when used in patients with type-2 diabetes. This review will compare various doses and the impact of the ER versus IR formulations of injectable triamcinolone on blood glucose control. The purpose of this review is to provide clinicians with a summary of safety information to assist in predicting injectable steroid-mediated glucose excursions in patients with type-2 diabetes. This review may be useful to guide selection of TA injection dose and formulation that exerts adequate analgesia while minimizing excessive hyperglycemia in patients with type-2 diabetes [2].
Materials and Methods
Search strategy and study selection
In September 2024, a literature search was conducted using PubMed, Ovid Medline, Embase, Cochrane Library, and CINAHL. The following keywords were included: “triamcinolone”, “diabetes”, “hyperglycemia”, “intra-articular injection”, “epidural injection”, “continuous glucose monitor”, “glucocorticoid” and “knee, osteoarthritis”. Within PubMed, Medical Subject Headings (MeSH) terms and directly searching the above keywords separated by “AND” were included in the search. For all databases, the keywords were searched within the titles, abstract, and text. Titles were initially screened, then abstracts were reviewed. Duplicate articles were excluded from the final analysis.
Study designs included for initial review were randomized, controlled trials, prospective and retrospective cohort studies, case-control studies, and case reports. Full manuscripts of eligible articles were accessed and reviewed. Articles were selected for analysis based on the following inclusion criteria:
1. Study evaluated the effect of intra-articular or epidural triamcinolone acetonide.
2. Participants of the study had type-2 diabetes and were on average at least 60 years of age.
3. Endpoints of the study evaluated numerical changes in glucose.
Articles were excluded based on the following criteria, if the study used: (1) A corticosteroid other than triamcinolone acetonide or (2) Intravenous triamcinolone was administered.
Data extraction and analysis
A literature analysis was completed on all included articles, appraising study design, inclusion and exclusion criteria, number of participants, statistically significant results and clinical relevance [3].
Results
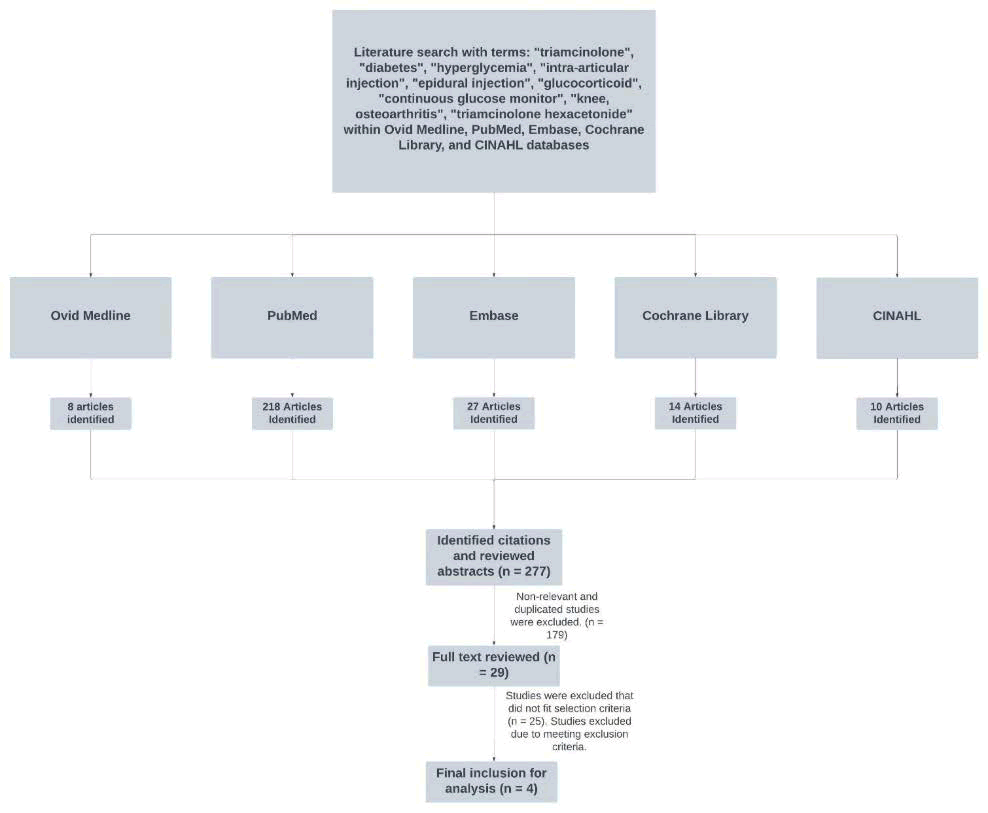
A total of 277 articles were initially screened, 29 full text manuscripts met inclusion criteria, of which 25 were excluded for being non-primary literature (n=2), evaluating knee IA or epidural corticosteroid but not reporting data for TA alone (n=9), evaluated injection sites other than knee or epidural sites (n=5), or articles not reporting glucose levels (n=9). Ultimately, 4 studies met criteria for the final review (FIGURE 1). TABLE 1 contains the citation, study design, mean age, injection site, diabetes characterization, triamcinolone formulation and dose [4].
FIGURE 1: Literature search process.
| Study design | N | Mean age | Injection site | Diabetes characterization | Triamcinolone dose and formulation |
| Prospective study | 7 | 61 years +/- 4.4 | Epidural | Controlled T2DM (HbA1C <7%) managed with hypoglycemic agents or insulin. | TA-IR 40 mg |
| Double-blind, randomized, parallel-group, phase 2 study | 33 | 61 years (46-83) | Knee | HbA1C 6.5-9.0% 1-2 oral hypoglycemic agents on stable doses for at least 2 months | Triamcinolone ER: 32 mg compared to Triamcinolone IR: 40 mg |
| Post-hoc analysis of Russell et al. 2018 study | 33 | 61 years (46-83) | Knee | HbA1C 6.5-9.0% 1-2 oral hypoglycemic agents on stable doses for at least 2 months | Triamcinolone ER: 32 mg compared to Triamcinolone IR: 40 mg |
| Prospective observational study | 100 | TA-IR 40 mg: 68 years (60-78) TA-IR 20 mg: 69 years (63-75) | Epidural | Active therapy with record of HbA1C obtained within one month of enrollment | TA-IR 40 mg compared to TA-IR 20 mg |
TABLE 1. Summary of included studies.
Intra-articular injections of the knee
In a double-blind, randomized, prospective study, Russell and colleagues evaluated glucose excursions following IA knee injections of TAER 32 mg compared to TA-IR 40 mg using Continuous Glucose Monitoring (CGM) for patients with Type 2 Diabetes Mellitus (T2DM) and knee osteoarthritis. The Glucose Management Indicator (GMI) is a percentage value that is generated by CGM devices to give an estimation of glucose control over time. The authors compared average daily CGM Glucose (CGMG) from baseline (days -3 to -1) to posttreatment period (days 1-3) for TA-ER and TA-IR groups. The average daily CGMG was significantly lower in the TA-ER group versus the TA-IR group (14.7 vs. 33.9; LSM (95% CI) difference of -19.2 mg/dL (-38, -0.4) P=0.0452). The TA-ER had a CGMG increase of 8.2 mg/ dL from baseline to post-injection periods (P= 0.6665) while TA-IR had an increase of 37.1 mg/dL from baseline to post injection periods (P=0.0354). The TA-IR group had a significant increase in average daily CGMG during baseline to post-injection period, while TA-ER did not. Mean average hourly CGMG levels were also reported by the authors. Participants who received TA-IR experienced a greater time above target range (70-180 mg/dL) than TA-ER, 49.9% vs. 34.5%, respectively [5,6].
Spitzer et al. performed a post-hoc analysis of the same study, which expanded on the CGM data and analyzed the full ambulatory glucose profile. The CGM results showed that participants who received TA-IR injections in their knee had less time in range with their desired glucose ranges (70-180 mg/dL) than those who received TA-ER injections (time in range 48% vs. 62%, P=0.123) during the first three days. As expected, those who received TA-IR 40 mg experienced significantly more time with severe hyperglycemia >250 mg/dL compared to TA-ER (26% versus 12%, P=0.047). Time in range for days 4 through 14 were reported as follows: Percent time within severe hyperglycemia (>250 mg/dL) was 11% for both TA-ER and TA-IR groups; percent time within hyperglycemia (>180 mg/dL-250 mg/dL), 18% for TA-IR and 26% for TA-ER; and percent time within target range (>70 mg/ dL-180 mg/dL), 48% for TA-IR and 62% for TA-ER. However, P values were not reported for this data. The Glucose Management Indicator (GMI) of the TA-IR group was not significantly higher compared to the TA-ER group (7.5 versus 7.1 P=0.3241). The authors also evaluated glucose levels over time (up to a maximum of 360 hours after injection) and found median time to a glucose value of 250 for TA-ER was 44 hours, while TA-IR was 6 hours (P=0.003).
Epidural injections
In a prospective observational study, Kim and colleagues analyzed the glucose effects of two different doses of epidural TA-IR in 100 patients with diabetes. Specifically, the authors compared epidural TA-IR 20 mg versus epidural TA-IR 40 mg and evaluated the effect on mean Fasting Plasma Glucose (FPG) and mean Post-Prandial Glucose (PPG) over a 14-day period using Self- Monitoring of Blood Glucose (SMBG). During the first two days, participants who received 40 mg TA-IR experienced significantly higher FPG compared to the 20 mg TA-IR group. In the TA-IR 40 mg group, the average increase in FPG compared to baseline was 50 mg/dL (Day 1) P<0.001; 25 mg/dL (Day 2) P<0.001; and 12 mg/dL (Day 3) P=0.01. In the TA-IR 20 mg group, the average increase in FPG compared to baseline was 15 mg/dL (Day 1) P<0.001; 5 mg/ dL (Day 2) P=0.0053; and no increase or -1 mg/ dL (Day 3) P=0.669.10
Similarly, participants who received TA-IR 40 mg experienced significantly higher average PPG compared to the TA-IR 20 mg group. The average PPG of TA-IR 40 mg group across days 1-3: Day of injection +110 (P<0.001); Day 1 +88 mg/dL (P<0.001); Day 2 +66 mg/ dL (P<0.001); Day 3 +19 mg/dL (P<0.001). Average PPG of TA-IR 20 mg group across days 1-3: Day of injection +59 mg/dL (P<0.001); Day 1 +50 mg/dL (P<0.001); Day 2 +37 mg/ dL (P<0.001); Day 3 +9 mg/dL (P=0.023). Average PPG returned to baseline after 5 days for the 40 mg group and after 4 days for the 20 mg group. In another study, however, Moon and colleagues found no significant increases in mean FPG after receiving TA-IR 40 mg: Day 1 +13.5 mg/dL (P=0.41); Day 2 -1 mg/dL (P=0.85); Day 3 -0.2 mg/dL (P=0.49). Disadvantages of this study were the small number of patients with diabetes, 7 participants, and analyzing FBG using laboratory readings [7].
Discussion
Assessing glucose excursions is a major focus of ensuring safe use of IA or epidural TA in patients with diabetes. However, it is also important for clinicians to consider the dose-response relationship for analgesia. The overarching goal of therapy is to optimize pain control while minimizing glucose excursions. This discussion synthesizes recommendations, integrating the reviewed literature evaluating the effects of triamcinolone on blood glucose with considerations for optimal pain control. Given that both IR and ER formulations can impact glucose control, careful selection of formulation and dose, along with blood glucose monitoring, is essential for patients with T2DM receiving TA injections [8].
These studies all evaluated the effects of TA-IR and TA-ER in patients with variable diabetes control. Russell and Spitzer evaluated patients with variable glucose control (6.5%-9% on stable doses of hypoglycemic agents) and found prominent elevations in glucose during their studies. Kim and colleagues demonstrated that even patients with well-controlled diabetes had significant elevations in average FPG and PPG. However, the study population in Moon and colleagues had well controlled diabetes with HbA1c<7% and resulted in no significant elevations in mean FPG.
While epidural and IA TA have potential for significant glucose excursions in patients with relatively stable glucose control, it is important to acknowledge the lack of data of epidural and IA TA in patients with poorly controlled T2DM. It can be hypothesized that a patient with poorly controlled T2DM who is treated with TA (epidural or IA) may be at a higher risk of hyperglycemic events than a patient with well controlled T2DM. This subject matter is complicated by the altered pharmacokinetic profile of the older adult population as there have been reported cases of hyperglycemic emergencies following injected corticosteroid [9,10].
In a recent retrospective cohort study, the authors analyzed the incidence of Diabetic Ketoacidosis (DKA) and hyperglycemic hyperosmolar syndrome 30 days after receiving an injected corticosteroid. One 60-year-old woman in this study received 80 mg triamcinolone into the knee joint and experienced DKA afterwards. This case highlights the risk of high-dose triamcinolone into the knee joint, especially in patients with burden of uncontrolled diabetes and comorbidities [11].
Advantages of TA-ER
Compared to TA-IR, TA-ER was associated with lower glucose excursions from post-injection day 1 to 3, as well as days 4 to 14 with a lower FBG and PPBG. These data show TA-ER may potentially have better glucose tolerability in patients with diabetes when compared to TA-IR. However, limited data exists regarding glucose excursions following IA knee injections beyond the first few weeks. This review highlights how FPG and PPG are significantly increased after administration of injectable TA. Additionally, Russell and colleagues demonstrated the value of CGM monitoring for patients receiving injectable TA, as this helps predict trends and may provide helpful guidance on treatment options for TA-associated hyperglycemia.
Comparison of 40 mg TA-IR injections in the knee (IA) and epidural sites
There is a lack of data between the glucose effects of 40 mg TA-IR in varying administration sites across the body. Russell and colleagues reported daily average CGMG, whereas Kim and colleagues reported fingerstick FPG and PPG values, with the currently published literature, it is difficult to compare the numerical outcome of glucose excursions of 40 mg TA-IR in the IA and epidural injections sites. However, between both studies, glucose metrics remained significantly elevated for three days in both the epidural and IA injection sites. This finding suggests that return to baseline may be similar between these injection sites. There may be value in future studies to evaluate glucose effects of TA-IR doses in different injection sites.
Epidural TA-IR dosing
Currently, TA-ER is only approved for knee osteoarthritis. For epidural TA-IR, evidence suggests significant glucose excursions are associated with higher doses compared to lower doses. As described above, Kim and colleagues showed that both average FPG and PPG were significantly higher with administration of 40 mg TA-IR when compared to 20 mg TA-IR.
Conclusion
Triamcinolone is a commonly used corticosteroid for musculoskeletal pain of the back and knee. Given the high prevalence of type-2 diabetes in patients who have musculoskeletal pain, hyperglycemic complications due to systemic absorption of triamcinolone are a concern. Clinicians should consider optimizing pain control while mitigating glucose excursions by understanding how the pharmacodynamic effects of triamcinolone are variable based on formulation and dose. Higher doses of TA-IR appear associated with more severe glucose excursions, compared to modest doses. Additionally, TA-ER may be preferred due to producing less glucose increase compared to TA-IR. Although cost may play a role in corticosteroid choice, utilizing TA-ER may offer improved glucose profiles after knee injections. Additional studies are needed to further evaluate triamcinolone injections in other locations CGM data would be beneficial to evaluate glucose excursions. These findings will guide clinicians on optimal dosing and formulation to treat pain while minimizing corticosteroid-induced glucose excursions.
Conflict of Interest
Each author has fulfilled the criteria for authorship, reviewed and approved the paper, and attest to the integrity of the work.
None of the authors have any conflicts of interest or financial interests related to the work.
References
- Cato RK. Indications and usefulness of common injections for nontraumatic orthopedic complaints. Med Clin North Am. 100, 1077-1088 (2016).
[Crossref] [Google Scholar] [PubMed]
- Stout A, Friedly J, Standaert CJ. Systemic absorption and side effects of locally injected glucocorticoids. PM R. 11, 409-419 (2019).
[Crossref] [Google Scholar] [PubMed]
- Kim N, Schroeder J, Hoffler CE, et al. Elevated hemoglobin A1C levels correlate with blood glucose elevation in diabetic patients following local corticosteroid injection in the hand: A prospective study. Plast Reconstr Surg. 136, 474e-479e (2015).
[Crossref] [Google Scholar] [PubMed]
- Habib GS, Miari W. The effect of intra-articular triamcinolone preparations on blood glucose levels in diabetic patients: A controlled study. J Clin Rheumatol. 17, 302-305 (2011).
[Crossref] [Google Scholar] [PubMed]
- Lekic N, Patel AA, Friend ME, et al. A prospective study on the effect of corticosteroid injection dosage for hand disorders in non-insulin dependent diabetics. Bull Hosp Jt Dis (2013). 76, 198-202 (2018).
[Google Scholar] [PubMed]
- Stepan JG, London DA, Boyer MI, et al. Blood glucose levels in diabetic patients following corticosteroid injections into the hand and wrist. J Hand Surg Am. 39, 706-712 (2014).
[Crossref] [Google Scholar] [PubMed]
- Moon HJ, Choi KH, Lee SI, et al. Changes in blood glucose and cortisol levels after epidural or shoulder intra-articular glucocorticoid injections in diabetic or nondiabetic patients. Am J Phys Med Rehabil. 93, 372–378 (2014).
[Crossref] [Google Scholar] [PubMed]
- Russell SJ, Sala R, Conaghan PG, et al. Triamcinolone acetonide extended-release in patients with osteoarthritis and type 2 diabetes: A randomized, phase 2 study. Rheumatology (Oxford). 57, 2235-2241 (2018).
[Crossref] [Google Scholar] [PubMed]
- Spitzer AI, Rodbard HW, Iqbal SU, et al. Extended-release versus immediate-release triamcinolone acetonide in patients who have knee osteoarthritis and type 2 diabetes mellitus. J Arthroplasty. 39, S218-S223.e1 (2024).
[Crossref] [Google Scholar] [PubMed]
- Kim WH, Sim WS, Shin BS, et al. Effects of two different doses of epidural steroid on blood glucose levels and pain control in patients with diabetes mellitus. Pain Physician. 16, 557-568 (2013).
[Google Scholar] [PubMed]
- Sytsma TT, Greenlund LS, Fischer KM, et al. Impact of intra-articular corticosteroid injection on glycemic control: A population-based cohort study. Clin Diabetes. 42, 96–103 (2024).
[Crossref] [Google Scholar] [PubMed]