Mini Review - Journal of Pharmaceutical Toxicology (2023) Volume 6, Issue 3
Exploring the Future of Drug Therapies: Advancements and Challenges
Sara Richard*
Bioengineering Department, IQS, Ramon Lull University, Via Augusta 390, Barcelona 08017, Spain
- *Corresponding Author:
- Sara Richard
Bioengineering Department, IQS, Ramon Lull University, Via Augusta 390, Barcelona 08017, Spain
E-mail: richardsara@gmail.com
Abstract
Psychedelic substances have long been associated with counterculture movements and recreational use. However, recent scientific research has unveiled their potential therapeutic benefits in the field of mental health treatment. The reemergence of psychedelic-assisted therapy has sparked significant interest among researchers, healthcare professionals, and the general public. This article delves into the groundbreaking advancements in the field, shedding light on the transformative potential of psychedelic-assisted therapy for various mental health conditions. Psychedelic-assisted therapy involves the careful administration of psychedelic substances, such as psilocybin (found in magic mushrooms) or MDMA (commonly known as ecstasy), in conjunction with therapy sessions. These substances are known to induce altered states of consciousness that can facilitate deep introspection and emotional processing. When combined with therapeutic support, they offer a unique opportunity for individuals to explore and address the root causes of their mental health issues.
Keywords
Diagnostic test • Covid-19 • Clinical trial • Pharmacology
Introduction
Clinical trials investigating the efficacy of psychedelic-assisted therapy have shown promising results in treating depression and anxiety disorders. For example, studies have reported significant reductions in depressive symptoms and improved emotional well-being in patients with treatment-resistant depression. Similarly, individuals struggling with anxiety disorders, including post-traumatic stress disorder (PTSD), have experienced significant symptom relief and enhanced quality of life after undergoing psychedelic-assisted therapy. Addiction is a complex condition that often involves deep-rooted psychological and emotional factors. Psychedelic-assisted therapy has shown potential in treating substance abuse disorders by helping individuals gain new insights and perspectives on their addictive behaviors. Research indicates that psychedelics can facilitate profound spiritual experiences and increase one’s sense of connectedness, which can play a crucial role in breaking the cycle of addiction [1-3].
Scientists are actively investigating the neurological and psychological mechanisms underlying the therapeutic effects of psychedelics. Recent studies using neuroimaging techniques have revealed how these substances modulate brain activity, promoting increased connectivity between different brain regions and facilitating neuroplasticity. Additionally, psychedelics may enhance emotional receptivity and facilitate the reprocessing of traumatic memories, leading to profound healing experiences. The resurgence of psychedelic-assisted therapy also brings forth important ethical considerations and legal implications balancing patient safety, access to treatment and rigorous scientific standards is paramount to fully harnessing the potential of psychedelic-assisted therapy [4,5].
Material and Methods
Psychedelic-assisted therapy represents a paradigm shift in the field of mental health treatment. With mounting scientific evidence supporting their efficacy, psychedelics are increasingly being recognized as powerful tools for healing and personal growth. While there are still many questions to be answered and challenges to overcome, the transformative potential of psychedelic-assisted therapy offers a glimmer of hope for individuals grappling with mental health conditions that have been resistant to traditional treatments. In recent years, the field of drug therapy has witnessed remarkable advancements, revolutionizing the way we approach various diseases and medical conditions. From breakthrough treatments for cancer to innovative approaches in mental health, the pharmaceutical industry has been at the forefront of medical innovation. This article delves into the future of drug therapies, highlighting the latest developments, potential benefits, and challenges that lie ahead.
Advancements in genomics and molecular biology have paved the way for precision medicine, an approach that tailors drug therapies to an individual’s unique genetic makeup. By identifying specific genetic markers and utilizing targeted therapies, precision medicine offers the promise of enhanced treatment efficacy, reduced side effects, and improved patient outcomes. This section explores the potential of precision medicine across various fields, including oncology, cardiovascular diseases, and rare genetic disorders. Immunotherapy has emerged as a groundbreaking approach in cancer treatment, utilizing the body’s immune system to combat tumors. This section discusses the latest developments in immunotherapies, such as checkpoint inhibitors, CAR-T cell therapies, and cancer vaccines. It highlights their potential to revolutionize cancer treatment and improve long-term survival rates.
Results
The re-emergence of psychedelic-assisted therapies has garnered significant attention in recent years. Clinical trials and research studies have demonstrated the potential of substances like psilocybin and MDMA in treating mental health conditions such as depression, anxiety, and posttraumatic stress disorder (PTSD). This section explores the promising results, ongoing research, and the regulatory challenges that need to be addressed for wider acceptance and integration of these therapies. Drug repurposing, also known as drug repositioning, involves identifying new therapeutic applications for existing drugs. This cost-effective strategy bypasses the lengthy drug development process and allows for the potential discovery of treatments for different diseases. This section discusses the advantages, limitations, and recent success stories in drug repurposing, highlighting its potential to rapidly address unmet medical needs.
As drug therapies advance, new challenges arise.
This section explores the regulatory hurdles faced by innovative therapies, including precision medicine and psychedelic-assisted therapies. It also delves into the ethical considerations surrounding access, affordability, and the equitable distribution of these novel treatments. The future of drug therapies holds immense promise, with advancements in precision medicine, immunotherapy, psychedelic-assisted therapies, and drug repurposing pushing the boundaries of medical innovation. While challenges in regulation and ethics remain, continued research, collaboration, and a patientcentered approach can pave the way for a new era of personalized, effective, and accessible drug treatments, ultimately transforming the landscape of healthcare.
In recent years, there has been a resurgence of interest in the therapeutic potential of psychedelic substances such as psilocybin, MDMA, and LSD. These substances, which were once associated with counterculture movements of the 1960s, are now being studied and recognized for their potential in revolutionizing mental health treatment. This article explores the growing field of psychedelic-assisted therapies and the significant impact they may have on addressing various mental health disorders. Over the past decade, there has been a notable shift in scientific and medical communities towards exploring the therapeutic benefits of psychedelics. The lifting of prohibitions and the recognition of their potential have paved the way for rigorous clinical trials and research studies. This section delves into the renaissance of psychedelic research and highlights some of the groundbreaking studies that have emerged in recent years.
Discussion
Psychedelic-assisted therapies involve the controlled administration of psychedelic substances in conjunction with psychotherapy sessions. This section explains the mechanism of action of these substances and how they can influence brain activity and neural pathways. It also explores the therapeutic potential of psychedelics for conditions such as depression, post-traumatic stress disorder (PTSD), anxiety disorders, and addiction. Numerous clinical trials are currently underway to investigate the safety and efficacy of psychedelic-assisted therapies. This section provides an overview of some of the ongoing studies and highlights the preliminary results that have shown promise. It discusses the use of psilocybin for treatment-resistant depression, MDMA-assisted therapy for PTSD, and other groundbreaking trials that are pushing the boundaries of mental health treatment [6-8].
As psychedelic-assisted therapies gain recognition, it becomes crucial to address safety concerns and legal considerations. This section examines the safety profile of psychedelic substances when administered in controlled settings and the measures in place to minimize potential risks. It also explores the evolving legal landscape surrounding psychedelic research and the efforts to navigate regulatory frameworks. The potential impact of psychedelic-assisted therapies on mental health treatment is vast. This section discusses the future prospects of these therapies and their integration into mainstream healthcare systems. It explores the challenges that lie ahead, including stigma, accessibility, and ensuring equitable access to these potentially life-changing treatments. Psychedelic-assisted therapies represent a paradigm shift in mental health treatment. While further research is needed, the growing body of evidence suggests that these therapies have the potential to transform the lives of individuals suffering from various mental health disorders. As attitudes and regulations continue to evolve, psychedelic-assisted therapies may become an integral part of a comprehensive approach to mental healthcare, offering hope and healing to those in need [9-11].
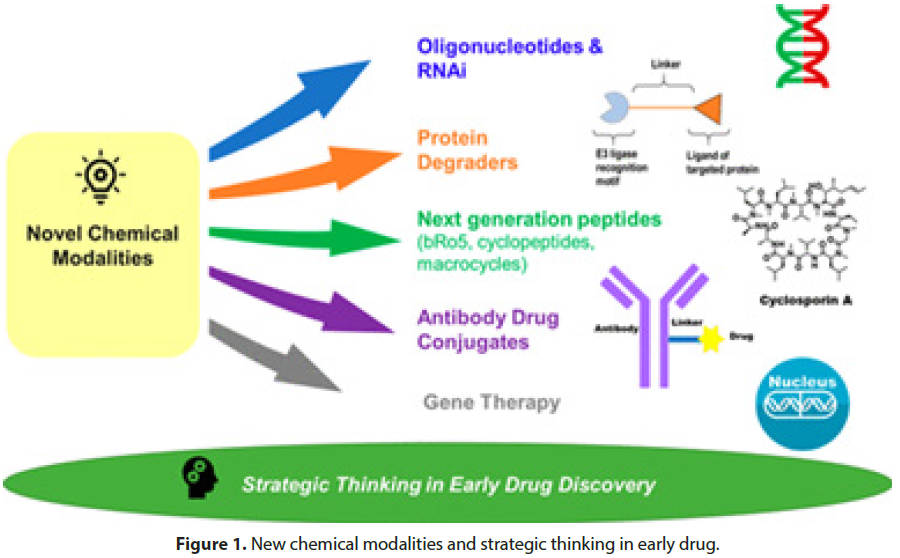
Drug addiction continues to be a pressing issue worldwide, affecting individuals and communities across various socioeconomic backgrounds. The complexities surrounding drug abuse, ranging from the factors contributing to addiction to the consequences it has on public health, necessitate a comprehensive understanding of the problem. This article aims to shed light on the challenges associated with drug addiction and explore promising strategies being implemented to combat this pervasive issue. The emergence of synthetic drugs, such as fentanyl and bath salts, has created new challenges in the battle against drug addiction. This section delves into the potency and risks associated with synthetic substances, highlighting the need for increased awareness and effective regulatory measures to address this evolving threat. Young people are particularly vulnerable to the lure of drugs, and preventing substance abuse among this demographic is crucial for building healthier communities. This segment discusses the factors contributing to youth drug addiction, including peer pressure and socioeconomic influences, and presents preventive measures and intervention strategies aimed at breaking the cycle (Figure 1).
In recent years, technology has played a significant role in transforming addiction recovery approaches. From mobile applications to virtual support networks, technology-based interventions have shown promise in providing accessible and personalized support for individuals seeking recovery. This section explores the integration of technology into addiction treatment and recovery programs, highlighting its potential benefits and limitations. Traditional drug policies have often focused on punitive measures rather than harm reduction. However, an alternative approach is gaining momentum— harm reduction strategies. This part examines the principles and effectiveness of harm reduction practices, such as needle exchange programs and supervised consumption sites, and discusses their potential impact on public health and society [12-14].
Stigma remains a significant barrier to individuals seeking help for their addiction. This section highlights the detrimental effects of stigma and explores initiatives that aim to reduce the associated shame and discrimination. By fostering an environment of compassion and understanding, society can encourage more individuals to seek treatment and support for their substance use disorders. Addressing drug addiction requires a multifaceted approach that encompasses prevention, treatment, recovery support, and policy reform. By understanding the challenges posed by synthetic drugs, targeting youth substance abuse, leveraging technology for recovery, adopting harm reduction strategies, and combating stigma, progress can be made in the battle against drug addiction. With continued research, collaboration, and a focus on evidence-based practices, we can strive towards a future where individuals and communities are empowered to overcome the grip of addiction.
In recent years, there has been a resurgence of interest in the therapeutic potential of psychedelic substances such as psilocybin, LSD, and MDMA. These substances, once associated with counterculture movements of the 1960s, are now being studied for their profound effects on mental health disorders. The growing body of research suggests that psychedelic-assisted therapy could herald a paradigm shift in the field of mental health treatment. Over the past decade, there has been a renewed interest in studying the therapeutic benefits of psychedelics. After a long hiatus due to legal restrictions and societal stigma, researchers are once again exploring the potential of these substances to alleviate symptoms of conditions like depression, anxiety, PTSD, and addiction. The article delves into the history of psychedelic research, highlighting key studies and the factors that have led to its revival [15-18].
Psychedelic substances work by interacting with serotonin receptors in the brain, leading to altered states of consciousness and profound subjective experiences. Recent neuroimaging studies have shed light on the neural mechanisms underlying the therapeutic effects of psychedelics, suggesting that they promote neuroplasticity and facilitate emotional processing. This section explains the neurochemical and psychological processes involved in psychedelic-assisted therapy. Numerous clinical trials have demonstrated the potential of psychedelics in the treatment of mental health disorders. For instance, studies have shown that psilocybin-assisted therapy can reduce symptoms of depression and anxiety in cancer patients, while MDMA-assisted therapy has shown promise in treating PTSD. This section summarizes some of the most notable clinical trials and their outcomes. While the research on psychedelic-assisted therapy is promising, there are still significant challenges and ethical considerations to address [19,20].
Conclusion
The article discusses issues such as standardization of treatment protocols, ensuring participant safety, navigating legal and regulatory frameworks, and managing the potential risks and adverse effects associated with psychedelic use. Looking ahead, the article explores the potential future implications of psychedelicassisted therapy. It discusses ongoing research, the role of psychedelic integration therapy, and the possibilities of personalized medicine in this emerging field. Additionally, it examines the potential impact on mental health care systems and the challenges of integrating these therapies into mainstream healthcare practices. Psychedelicassisted therapy represents a groundbreaking approach to mental health treatment, offering new hope for individuals suffering from various mental health disorders. While there are still hurdles to overcome, the research and clinical trials conducted thus far provide compelling evidence for the potential of psychedelics to revolutionize the field of mental health care. As society continues to evolve its understanding and acceptance of these substances, the integration of psychedelic-assisted therapy into mainstream medicine may offer a promising path forward for improved mental well-being.
Acknowledgement
None
Conflict of Interest
None
References
- Ogurtsova K, Fernandes JD, Huang Y et al. IDF Diabetes Atlas Global estimates for the prevalence of diabetes. Diabetes Res Clin Pract. 128, 40-50 (2017).
- Zhou Z, Mahdi A, Tratsiakovich Y et al. Erythrocytes From Patients With Type 2 Diabetes Induce Endothelial Dysfunction Via Arginase I. J Am Coll Cardiol. 72, 769-780 (2018).
- Sprague RS, Stephenson AH, EA Bowles et al. Reduced expression of Gi in erythrocytes of humans with type 2 diabetes is associated with impairment of both cAMP generation and ATP release. Diabetes. 55, 3588-3593.
- Blaslov K, Kruljac I, Mirošević G et al. The prognostic value of red blood cell characteristics on diabetic retinopathy development and progression in type 2 diabetes mellitus. Clin Hemorheol Microcirc. 71, 475-481 (2019).
- Venerando B, Fiorilli A, Croci G et al. Acidic and neutral sialidase in the erythrocyte membrane of type 2 diabetic patients. Blood. 99,1064-1070 (2002).
- Kadiyala R, Peter R, Okosieme OE et al. Thyroid dysfunction in patients with diabetes: clinical implications and screening strategies. Int J Clin Pract. 64, 1130-1139 (2010).
- Clark A, Jones LC, de Koning E et al. Decreased insulin secretion in type 2 diabetes: a problem of cellular mass or function. Diabetes. 50, 169-171 (2001).
- DeFronzo RA. Pathogenesis of type 2 diabetes: metabolic and molecular implications for identifying diabetes genes. Diabetes Reviews. 5, 177-269 (1997).
- Peppa M, Betsi G, Dimitriadis G et al. Lipid abnormalities and cardio metabolic risk in patients with overt and subclinical thyroid disease. J Lipids. 9,575-580 (2011).
- Cettour-Rose P, Theander-Carrillo C, Asensio C et al. Hypothyroidism in rats decreases peripheral glucose utilisation, a defect partially corrected by central leptin infusion. Diabetologia. 48,624-633 (2005).
- Dessein PH, Joffe BI, Stanwix AE et al. Subclinical hypothyroidism is associated with insulin resistance in rheumatoid arthritis. Thyroid. 14, 443-446 (2004).
- Warren KA, Bahrani H, Fox JE et al. NSAIDs in combination therapy for the treatment of chronic pseudophakic cystoid macular edema. Retina. 30, 260-266 (2010).
- Schoenberger SD, Miller DM, Petersen MR et al. Nepafenac for epiretinal membrane surgery. Ophthalmol. 118,1482-1482 (2011).
- Friedman DS, O’Colmain BJ, Munoz B et al. Prevalence of age-related macular degeneration in the United States. Arch Ophthalmol. 122, 564-572 (2004).
- Maloney SC, Fernandes BF, Castiglione E et al. Expression of cyclooxygenase-2 in choroidal neovascular membranes from age-related macular degeneration patients. Retina. 29, 176-180 (2009).
- Hu W, Criswell MH, Ottlecz A et al. Oral administration of lumiracoxib reduces choroidal neovascular membrane development in the rat laser-trauma model. Retina. 25,1054-1064 (2005).
- Chen E, Benz MS, Fish MH et al. Use of nepafenac (Nevanac) in combination with intravitreal anti-VEGF agents in the treatment of recalcitrant exudative macular degeneration requiring monthly injections. Clin Ophthalmol. 4, 1249-1252 (2010).
- Gomi F, Sawa M, Tsujikawa M et al. Topical bromfenac as an adjunctive treatment with intravitreal ranibizumab for exudative age-related macular degeneration. Retina. 32, 1804-1810 (2012).
- Zhou J, Wang S, Xia X et al. Role of intravitreal inflammatory cytokines and angiogenic factors in proliferative diabetic retinopathy. Curr Eye Res. 37, 416-420 (2012).
- Harris R, Beebe-Donk J, Namboodiri KK et al. Inverse association of non-steroidal anti-inflammatory drugs and malignant melanoma among women. Oncol Rep. 8, 655-657 (2001).
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at