Mini Review - Journal of Experimental Stroke & Translational Medicine (2022) Volume 14, Issue 5
Experimental Stroke: Craniectomy in Acute Ischemic Stroke
Sun Jing*
Department of Neurosurgery, University Hospital Wurzburg, Josef-Schneider, Wurzburg, Germany
Department of Neurosurgery, University Hospital Wurzburg, Josef-Schneider, Wurzburg, Germany
E-mail: jingsun@edu.org
Received: 02-Sep-2022, Manuscript No. JESTM-22-76295; Editor assigned: 05-Sep-2022, PreQC No. JESTM-22-76295 (PQ); Reviewed: 19- Sep-2022, QC No. JESTM-22-76295; Revised: 23-Sep-2022, Manuscript No. JESTM-22-76295 (R); Published: 30-Sep-2022, DOI: 10.37532/ jestm.2022.14(5).106-110
Abstract
Acute occlusion of middle artery (MCA) ends up in severe brain swelling and to a malignant, usually fatal syndrome. The authors summarize the present information regarding such a condition and review the most surgical problems concerned. Decompressive hemicraniectomy keeps being a legitimate choice in accurately designated patients.
Introduction
Massive brain swelling could occur in up to 100% of cerebral anemia strokes. In these patients the clinical presentation sometimes starts with focal signs and progresses with a decline of consciousness till brain-stem dysfunction is clear. Despite optimum medical management this condition could cause death in 70–80% of cases, and people UN agency survive expertise severe neurologic deficits. Owing to the grim prognosis, this condition has been termed “malignant” cerebral infarct [1].
The etiology is that the occlusion of an oversized vessel, primarily the interior artery (ICA) or the center artery (MCA). A shift of the anemia tissue instead of raised intracranial pressure (ICP) is that the possibly liable for the initial decrease in consciousness. many alternative satellite reactions square measure concerned in associate degree inexorable pathogenetic cascade, together with disturbances of microvascular tone, epithelial tissue cell swelling, and activation of platelets, leucocytes, and activity.
In this review, we tend to analyze the most clinical problems with malignant supratentorial cerebral infarct and summarize the key surgical problems unremarkably concerned in its management.
At the onset, the clinical presentation of “malignant” cerebral infarct isn’t a lot of completely different than the other acute cerebrovascular accident within the same distribution, though focal signs and symptoms tend to be severe from the offset. Large brain swelling develops over time [2]. Malignant evolution is a lot of common in younger patients, doubtless because of the shortage of atrophy and less tolerance to accommodate changes in brain volume.
Imaging studies square measure the mainstay for identification of individuals at higher risk for malignant infarct among the cerebrovascular accident population. Brain computerized axial tomography (CT) is habitually performed for initial and later controls. The earliest warning signs for developing malignant infarct embody involvement of a neighborhood larger than five hundredth of the MCA territory associate degreed a pathology extending conjointly to the anterior or posterior artery territories. A midplane shift >10 mm, effacement of subarachnoid areas, and attenuation of corticomedullary differentiation are associated with higher risk of severe deterioration, however they sometimes occur later, once a malignant syndrome is already current [3]. The injection of medium with elaboration of its distribution entails higher diagnostic accuracy of anaemia areas and a good earlier detection of patients at higher risk. A call cerebral introduction of a lot of sixty six is said to a probable malignant evolution.
Magnetic resonance imaging is another useful test, that in cerebrovascular accident are often used for prognostic functions among few hours of clinical onset. Its sensitivity is more than CT and it’s a lot of doubtless to point out changes at earlier time points than CT scan. On diffusion weighted pictures (DWI) associate degree anaemia space of a minimum of a minimum of predicts a colossal cerebral infarct. Moreover, DWI anaemia volumes larger than 210 mL were found associated with 100% mortality in patients while not surgical operation (Table 1).
Exam |
Result |
|---|---|
| Plasmatic S100B protein dosage | >1.03 mcg/L |
| CT scan/perfusion-CT | Area compromised > 50% MCA territory |
| Extension to anterior or posterior territories | |
| Perfusion drop > 66% | |
| MRI/DWI | Ischemic area > 145 mL, even at early stages |
Table 1: Summary of the main instrumental clues to detect ischemic patients at higher risk for a malignant supratentorial (MCA) infarction
Intracranial Pressure (ICP)
The first systematic use of endless ICP watching was traditionally created among patients with brain tumors. This watching was then tested and applied to alternative conditions, and more enhancements in technology and technique contributed to its worldwide diffusion. Though wide accepted as useful gizmo within the management of patients with severe head injuries, the role of ICP watching in patients with massive cerebral infarctions is disputable.
It is simple that at final stages the pressure within the so of patients with massive cerebral infarct is maybe high. Anyway, a pressure increase restricted to the infarcted and directly adjacent areas might happen, resulting in neurologic worsening and even death despite no unfold of intracranial high blood pressure. Undisputed poor prognosis predictors as CT uncial hernia associate degreed anisocoria generally occur while not an overall ICP raise is detected. The measure may additionally be influenced by the device used (solid-state or fluid-filled) additionally as by its location [4].
In patients with cerebral infarct, it’s presently potential to own a transparent estimate of the initial anaemia injury and to early observe the well-known potential clinical evolutions. Observant the clinical standing, in the main by neurologic examination in awake patients and by tomography studies in insensible, ends up in a lot of helpful suggestions regarding the correct management instead of trying to find intracranial high blood pressure, which can conjointly ne’er come back [5]. The latter obviously could occur, however it ought to be avoided instead of measured. during this state of affairs, there aren’t any absolute recommendations for a routine use of intracranial pressure watching, because it are often thought-about a not unhazardous procedure that cannot truly influence the ultimate clinical management. In fact, patients with malignant infarct syndrome have to be compelled to be sharply treated, in spite of any quantitative part we tend to might live.
Surgical choice
Despite commonplace treatment, patients with large cerebral infarct go downhill, sometimes among 24–48 hours from the clinical onset. This usually suggests that somnolence, altered consciousness, motor dysfunctions, high blood pressure, arrhythmia, and within the unlucky cases progressive decline with expanded pupils and metabolic process failure. Osmotherapy, buffers, sedation, mannitol, breathing and a lot of recently physiological condition square measure the medical care treatments which may be applied in patients with clinical worsening because of anemia tissue swelling [6]. Sadly, they represent solely temporary interventions and temporizing measures that simply slow the inexorable development of more deterioration from tissue displacement and brain stem shift.
Surgery conversely is often terribly effective with adequate indications; the affordable operative treatment in large cerebral infarct is decompressive hemicraniectomy. The goal of such removing of a vicinity of the bone vault is to cut back the pressure of the swollen anaemia tissue and to avoid wasting the brain that’s still viable. Many animal studies incontestable the biological effects of this surgical operation [7], because the improvement of the plant tissue introduction and also the reduction of caspase-mediated cell death within the anaemia border zone. To not take into account the surgical choice ends up in uncomprehensible opportunities of undefeated treatment, however on the opposite hand not all the patients with the on top of requisite could very like the intervention.
Surgery
Timing is a vital issue to contemplate once evaluating ischaemic patients for surgery. Surgery cannot resurrect dead neurons. The warning signs we have a tendency to mentioned don’t ought to all occur before the brain surgeon is concerned as a result of this evident brain stem suffering would cause poor prognosis despite any effort. Decompressive hemicraniectomy ought to be performed at intervals at intervals of stroke, before brain stem pathology is patent. The requisite for the surgical indication is a good initial worsening in patients with verified large cerebral infarct, and clinical trials did not demonstrate advantages by prophylactic ultra-early surgery as no variations were found between patients treated at twenty four and forty eight hours from stroke onset. Anyway the potential prevalence of a imaging worsening despite a stable clinical standing keeps being AN unresolved issue for indication to decompress [8].
The second issue that the brain surgeon must contemplate is that the patient prestroke condition, that may be a sensible predictor of the possibility of survive and principally of the standard of life just in case of surgical intervention. Within the obtainable clinical trials the patient age resulted in one in all the foremost reliable outcome indicators. Generally, patients older than sixty years aren’t ideal candidates for surgical decompression, as they possess lower vegetative cell malleability and conjointly oftentimes have additional tube risk factors and comorbidities. Even in young patients with severe high blood pressure, viscus failure, embolism, and alternative analogous unfavorable diseases the hemicraniectomy may result extremely risky and fewer effective [9]. Conversely conjointly in older patients with an honest antecedent condition hemicraniectomy appears somehow to enhance the prognosis. As not unequivocal knowledge result from literature it’s urged to not habitually perform surgical decompression in stroke patients older than sixty years a minimum of in very well-selected cases. The consequences of hemicraniectomy in patients aged over sixty five years are going to be anyway assessed within the current Destiny II trial.
Surgery will be safely performed even when endovenous tissue proteolytic enzyme administration for lysis. The aspect of the stroke doesn’t appear to have an effect on the important standing when surgical decompression, thus it mustn’t influence the selection to control. However, the family ought to learn concerning the probably likelihood for the patient to survive however with severe speech disturbances. Family successively could offer helpful info regarding the patient’s needs.
Decompressive Technique
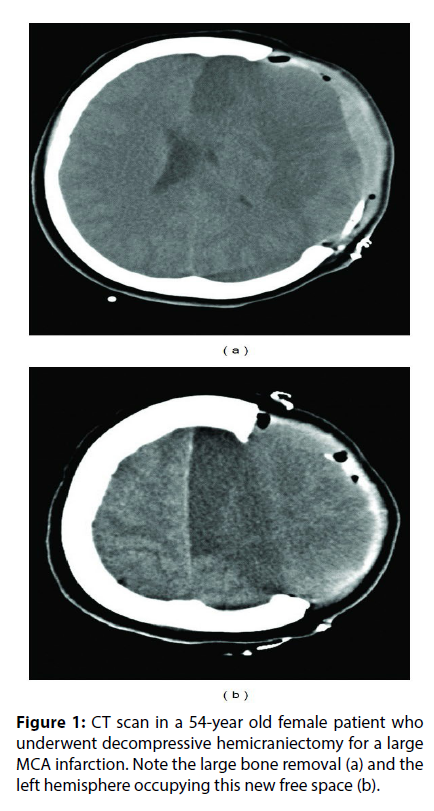
The skin incision will be created as a giant interrogation point or a midplane leaf-spring. Some surgeons advocate surgical procedure of the temporalis muscle and facia to permit a most decompression, however this can be not unremarkably performed. The surgery ought to embody the frontal, parietal, and temporal bones and its anteroposterior length mustn’t be inferior to 12 cm (Figure 1(a)); larger openings up to 14 cm or additional area unit thought to permit a good higher pressure relieve. Specific attention must be paid to decompression of the basal temporal space, because it represents a vital compartment with shut relationship with the brain stem. So as to achieve extra area, the meninges are usually opened moreover. It will then be enlarged with a biological or artificial substitute or left patent, simply lined by styptic material for a quicker closure. The cerebral tissue itself ought to be utterly preserved at surgery for recovery of the not deadly broken areas, which can be not distinguishable from the infarct itself (Figure 1(b)).
Figure 1: CT scan in a 54-year old female patient who underwent decompressive hemicraniectomy for a large MCA infarction. Note the large bone removal (a) and the left hemisphere occupying this new free space (b).
The bone flap will be preserved in an exceedingly connective tissue pocket superjacent the abdomen, however this ends up in partial resorption within the following weeks, longer operation times, and extra risks associated with the extra wound. A sound and presently prevailing various is to store the bone frozen (−80°C) in an exceedingly sterile box. The potential complications of decompressive craniectomy area unit surgical web site infections, hurt troubles and extraaxial fluid collections, hydrocephaly, and also the questionable sinking flap syndrome.
Cranioplasty
Once the clinical standing and imaging area unit compatible, the bone flap will be repositioned to revive structural integrity, defend the brain, and reinstate intracranial pressure. It’s not exceptional that when cranioplasty the patients show some clinical improvement. The necessity to primarily use completely different materials than the autologous bone to hide the bone defect is rare in patients decompressed for cerebrovascular accident. the right temporal order for cranioplasty when hemicraniectomy is debated, and within the literature do articles specific for patients WHO underwent surgery for malignant cerebral infarct not exist [10]. It will anyway be deduced from additional general studies that the bone flap will be sometimes repositioned at intervals five to twelve weeks. Infections and protracted parenchymal rupture through craniectomy essentially need longer waiting times for this second surgical procedure.
The cranioplasty clearly could have complications: infection and extra-axial intumescency formation area unit the foremost common followed by hydrocephaly. Surgical neural structure infarct is fortuitously a rare happening. Sharp brain swelling and late bone organic process area unit potential complications moreover.
Conclusion
Some patients with cerebrovascular accident develop a diffuse and progressive cerebral swelling resulting in a oftentimes fatal condition named malignant cerebral infarct syndrome. It’s vital to find early the cases at higher risk for that, so as to intervene before definitive large brain injury happens. For this purpose each imaging and clinical observations area unit helpful; intracranial pressure watching isn’t indispensable.
Medical treatments often fail in patients with medicine decline for large cerebral infarct, and also the surgical possibility will be in that thought-about. Decompressive hemicraniectomy may be a life-saving procedure that conjointly ends up in higher purposeful outcomes. An outsized unilateral surgery with duraplasty is performed, and also the brain parenchyma is spared. The patients WHO principally like such intervention area unit the younger and antecedently healthier, treated at intervals a slender amount from the clinical deterioration. In any case, the persistence of surgical deficits is that the rule. An entire and honest rationalization of the utility, probably result and limits of the surgical procedure should lean to the relatives of the patient candidate for decompression. Cranioplasty will be sometimes performed at intervals few weeks, once each clinical standing and imaging standing area unit favorable.
The lack of class I evidences about most of the discussed issues is constraining and the need for further studies on medical and surgical effectiveness is undoubted. Anyway at present time the above management flowchart for these patients may be suggested, where the surgical intervention should be considered an extreme but not senseless option once the more suitable cases are selected.
References
- Moulin DE, Lo R, Chiang J et al. Prognosis in middle cerebral artery occlusion. Stroke. 16, 282-284 (1985).
- Wijdicks EFM, Diringer MN. Middle cerebral artery territory infarction and early brain swelling: progression and effect of age on outcome. Mayo Clin Proc. 73, 829-836 (1988).
- Hacke W, Schwab S, Horn M et al. Malignant middle cerebral artery territory infarction: clinical course and prognostic signs. Arch Neurol. 53, 309-315 (1996).
- Frank JI. Large hemispheric infarction, deterioration, and intracranial pressure. Neurology. 45, 1286-1290 (1995).
- Schwab S, Aschoff A, Spranger M et al. The value of intracranial pressure monitoring in acute hemispheric stroke. Neurology. 47, 393-398 (1996).
- Del Zoppo GJ, Mabuchi T. Cerebral microvessel responses to focal ischemia. J Cereb Blood Flow Metab.23, 879-894 (2003).
- Foerch C, Otto B, Singer OC et al. Serum S100B predicts a malignant course of infarction in patients with acute middle cerebral artery occlusion. Stroke. 35, 2160-2164 (2004).
-  Lam WWM, Leung TWH, Chu WCW et al.  Early computed tomography features in extensive middle cerebral artery territory infarct: prediction of survival. J Neurol Neurosurg Psychiatry. 76, 354-357 (2005).
- Hofmeijer J, Algra A, Kappelle LJ et al. Predictors of life-threatening brain edema in middle cerebral artery infarction. Stroke. 25, 176-184 (2008).
- Krieger DW, Demchuk AM, Kasner SE et al. Early clinical and radiological predictors of fatal brain swelling in ischemic stroke. Stroke. 73, 829-836 (1998).
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref