Research Article - Interventional Cardiology (2025) Volume 17, Issue 3
Coronary ectasia presenting with acute coronary syndrome, its predictors and outcomes.
- Corresponding Author:
- Samir Rafla
Department of Cardiology, Alexandria University, Alexandria, Egypt
E-mail: smrafla@yahoo.com
Received date: 01-May-2025, Manuscript No. FMIC-25-166226; Editor assigned: 03-May-2025, PreQC No. FMIC-25-166226 (PQ); Reviewed date: 17-May-2025, QC No. FMIC-25-166226; Revised date: 24-May-2025, Manuscript No. FMIC-25-166226 (R); Published date: 31-May-2025, DOI: 10.37532/1755- 5310.2025.17(3).996
Abstract
Aim: The study aimed to assess the predictors and outcomes of coronary ectasia in patients presented with acute coronary syndromes.
Methods: 280 patients met our inclusion and exclusion criteria as ectatic Coronary Artery Disease (CAE) presented with Acute Coronary Syndrome (ACS) (group 1), and another 280 random patients as a control group without coronary ectasia presented with ACS (group 2). CAE was defined as the dilatation of a coronary segment with a diameter 1.5 times higher than normal adjacent segments. PCI procedures are detailed in the paper. Follow-up was for one year in all and two years in half the patients.
Results: CAE group 1 was compared to ACS. Patients without ectasia (group 2). Males were 93% vs. 71% in the two groups, respectively: hypertension (61% vs. 57%), dyslipidemia (21% vs. 28%), type 2 diabetes (26% vs. 36%), and ejection fraction more than 35% was present in 57 vs. 58%. Medical management only in 32% vs. 16% in the two groups. PCI was done in 42% vs. 76% in the two groups. CABG was done in 20 cases (7%) and 19 of the control group (7%).
Conclusion: The incidence of coronary ectasia is 4.9% among ACS patients. Mortality was 8.2% vs. 2.8% (P<0.005) in the two groups. Predictors of mortality: Male sex (0.010), previous ACS (0.021), and presentation with STEMI (0.018). Thrombus aspiration was done in 26% with no significant effect on hospital outcome. Most of the cases underwent balloon dilatation, 111 patients (94%), with no significant effect on hospital outcome.
Keywords
Coronary artery ectasia . Percutaneous coronary intervention . Coronary artery disease . Acute coronary syndrome . Antithrombotic therapy
Abbreviations
ACS: Acute Coronary Syndromes; AMI: Acute Myocardial Infarction; CABG: Coronary Artery Bypass Grafting; CAD: Coronary Artery Disease; CAE: Coronary Artery Ectasia; CS: Cardiogenic Shock; CSF: Coronary Slow Flow; IDDM: Insulin-Dependent Diabetes Mellitus; IVUS: Intravascular Ultrasound; LCX: Left Circumflex Arteries; LAD: Left Anterior Descending; MACE: Major Adverse Cardiac Event; MI: Myocardial Infarction; MMP: Matrix Metalloproteinase; MR: Mitral Incompetence; PCI: Primary Percutaneous Coronary Intervention; RCA: Right
Coronary Artery; STEMI: ST-Segment Elevation Myocardial Infarction; TFC: TIMI Frame Count method; TVR: Target Vessel Revascularization; UA: Unstable Angina.
Introduction
Coronary Artery Ectasia (CAE) or coronary artery aneurysm is the aneurysmal dilatation of coronary artery. It is defined as a dilatation with a diameter of 1.5 times the adjacent normal coronary artery based on CASS registry [1-4]. Its prevalence ranges from 1.2%-4.9% with male to female ratio of 3:1 [5]. The prevalence of CAE and comorbidities in the various studies are summarized in Table 1. It is commonly classified based on the shape and the extent of involvement of coronary arteries.
| Study | Total no. of cases | Cases of ecta- sia | Prevalence of CAE | HTN | DM | Hyperlipide- mia | Coexistent CAD |
|---|---|---|---|---|---|---|---|
| Swaye PS, et al. [4] | 20067 | 978 | 4.90% | N/A | N/A | N/A | N/A |
| Hartnell G, et al. [5] | 4993 | 70 | 1.40% | N/A | N/A | N/A | N/A |
| Harikrishnan S, et al. [25] | 3200 | 144 | 4.50% | 45.40% | 27.20% | 90.90% | 84.7% (122 of 144 Cases) |
| Gunes Y, et al. [26] | 8812 | 122 | 1.38% | 47.50% | 16.40% | 54.90% | 59% |
| Lam, et al. [24] | 8641 | 104 | 1.20% | 58% | 31% | 63% | 82% |
| Mohammed Atiq Almansori, et al. [27] | 1115 | 67 | 6% | 64% | 59% | 59% | N/A |
N/A: Not Available
Table 1: Prevalence of CAE and comorbidities [17].
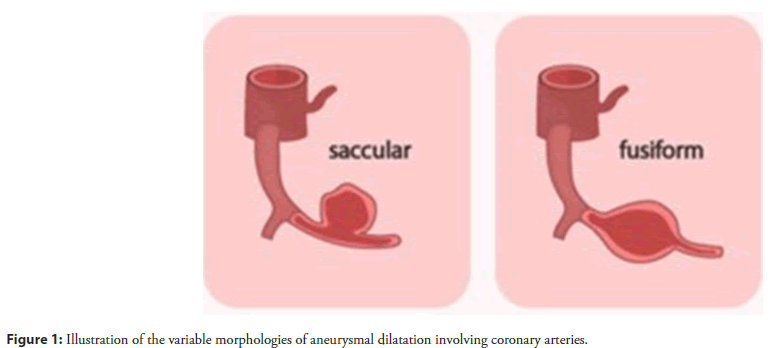
Classification based on shape
Saccular-transverse diameter is greater than the longitudinal dimension. Fusiform-transverse diameter less than the longitudinal dimension. Markis, et al. has classified CAE into four types (Table 2) [6].
| Causes | Frequency |
|---|---|
| Rare Congenital: Frequently associated with other cardiac abnormalities such as bicuspid aortic valve, aortic root dilatation, ventricular septal defect or pulmonary stenosis. Acquired |
|
| 1. Atherosclerosis | 50% |
| 2. Kawasaki disease and congenital causes | 17% |
| 3. Mycotic and infectious septic emboli including syphilis and borreliosis | 11% |
| 4. Connective tissue diseases and Marfan's syndrome | <10% |
| 5. Arteritis, e.g., polyarteritis nodosa, Takayasu's disease, systemic lupus erythematosus | <10% |
| 6. Iatrogenic, e.g., PTCA, stents, directional coronary atherectomy, angioplasty, and laser angioplasty | Rare |
| 7. Primary cardiac lymphoma | Rare |
Table 2: Causes of Coronary Artery ectasia [17].
The proximal and middle segments of the RCA are the most common sites for CAE (68%) followed by the proximal LAD (60%) and the LCx (50%). Coronary artery ectasia of the left main is rare and occurs in only 0.1% of the population. Figure 1 shows the coronary artery ectasia on a coronary angiogram.
Hypothesis of remodeling: Coronary ectasia likely represents an exaggerated form of expansive vascular remodeling (i.e. excessive expansive remodeling) in response to atherosclerotic plaque growth. A variety of factors described below affect the enzymatic degradation of the extracellular matrix of the media which appears to be a fundamental pathologic process.
Proteolytic enzymes such as cysteine proteinases (e.g. cathepsins K; L; and S) and serine proteinases (e.g. neutrophil elastase; plasminogen activators; plasmin; chymase. and tryptase) also play an important role in the pathogenesis of coronary ectasia.
Role of various factors: Elevated homocysteine levels may facilitate the degradation of the medial arterial layer by inducing serine proteinase activity in arterial smooth muscle cells; as well as by activating MMP. Hyperinsulinemia may exacerbate the remodeling process in the setting of coronary atherosclerosis by stimulating the proliferation and migration of vascular smooth muscle cells from the arterial media and interfering with extracellular matrix production.
Diagnosis: The Gold standard in diagnosing coronary ectasia is coronary angiogram. IVUS is available for evaluation of luminal extension and vessel wall pathologies and also for identification of normal arterial segments adjacent to stenotic lesions; which are often falsely characterized as aneurysms by conventional angiography.
Distortions in flow and washout are common in CAE; and are clearly associated with the severity of ectasia. Angiographic signs of turbulent and stagnant flow include delayed antegrade contrast filling; a segmental back flow (milking phenomenon) and local deposition of contrast in the dilated coronary segment (stasis).
Coronary slow flow: The presence of aneurysmal segments produces sluggish and turbulent blood flow. This is associated with an increased incidence of typical exercise induced angina pectoris and myocardial infarction; regardless of the severity of co-existing stenotic lesions [7-10].
Patients
Study population: All patients were studied with ACS with ectatic CAD in Alexandria main university hospital and International Cardiac Center (ICC; Alexandria) from January 2016 till December 2018 retrospectively and from January 2019 till June 2019 prospectively.
The patients with ectatic CAD were compared to control group without coronary ectasia. Demographic features; angiographic results and clinical events were compared.
Exclusion criteria
1. Patients with a previous history of CABG or treated with emergent CABG.
2. Patients with inconclusive clinical data from hospital files and computer records.
3. Patients with cardiogenic shock.
All patients gave written informed consent to the study protocol that was approved by the institutional ethical review board.
Materials and Methods
All the patients with ectatic coronary artery disease were subjected to thorough history taking with special emphasis on:
Clinical data of the patients
1. Clinical presentation of acute coronary syndrome either STEMI; NSTEMI or unstable angina.
2. Demographic features and clinical characteristics of the patients according to age; sex; DM (insulin dependent or non-insulin dependent); HTN; smoking; dyslipidemia; family history of CAD; previous ACS and previous coronary interventions.
3. Initial drug history and medications including antiplatelet; anticoagulants; statin; beta blockers and others (Table 3).
| Control | Cases | (p) | |
|---|---|---|---|
| Previous ACS | 10(3.5%) | 22(7.8%) | p=0.029* |
| Previous PCI | 79(28%) | 18(6.4%) | p=0.527 |
| STEMI | 88(31%) | 79(28%) | p=0.406 |
| Non STEMI | 65(23%) | 57(21%) | p=0.413 |
| UA | 127(46%) | 143(51%) | p=0.176 |
| ECG | 151(54%) | 164(58%) | p=0.268 |
| MR | 40(14%) | 76(27%) | p<0.001* |
| RWMA | 115(41%) | 116(41%) | p=0.932 |
| EF ≤ 35 >35 (mean ± SD) | 8 | 10 | P=NS |
| 272 (57 ± 8.9) | 270 (58.3 ± 9.6) | p=0.087 |
Table 3: Comparing cases and controls regarding presentation, echocardiography, and ECG of the study population.
Standard 12 leads ECG
Transthoracic echocardiography with special emphasis on ejection fraction; RWMA and degree of mitral valve regurgitation [11-15].
Coronary angiography
• All patients underwent coronary angiography after informed consent forms were obtained. Angiography procedures were performed using standard technique.
• Angiograms were analyzed by two independent and experienced intervention cardiologists and Syntax score were calculated.
• Diagnosis of ectatic coronary artery and classification according to the extent of involvement (type 1; 2; 3 and 4) and presence of aneurysm.
• Coronary ectasia was defined as the dilatation of a coronary segment with a diameter of 1.5 times higher than normal adjacent segments. Decision about the ectatic coronary artery was made by visual assessment.
• Number of ectatic vessels
• TIMI flow before coronary intervention in ectatic and non ectatic vessels.
• Thrombus burden was evaluated according to the TIMI thrombus scoring. The TIMI score 4 was defined as highgrade thrombus burden.
• Decision of medical treatment; PCI or CABG.
PCI procedure
a) Radial vs. femoral access.
b) Guiding catheter 6F or 7F.
c) Guiding wire either hydrophilic or non-hydrophilic.
d) Thrombus aspiration or not.
e) Balloon predilatation or not.
f ) Type of stents either DES or covered stents (number of stents used; diameter and length).
g) Intracoronary Glycoprotein IIb/IIIa inhibitor was used or not.
h) TIMI flow and myocardial blush grade post procedure.
i) Single vs. multi vessel PCI.
j) At the same setting vs staged PCI as regard the same vessel and time lapse in-between.
In-hospital outcome according to: Death; MI; stroke; bleeding; arrhythmia; heart failure; target vessel revascularization or non-target vessel revascularization. Intermediate outcome with minimum follow up 6 months up to 3 years. All data were acquired retrospectively and prospectively. Demographic features and clinical characteristics of the patients as well as data regarding revascularization and recurrent events were obtained from hospital records. Mortality information at 1 year were obtained from phone calls; national records in addition to those found in the hospital record system. Although in-hospital outcomes were obtained from hospital records; long-term clinical data were documented by review of hospital records; telephone interviews; and outpatient visits (Table 4).
| Control | Cases | (p) | |
|---|---|---|---|
| Medical | 42(15%) | 90(32%) | p<0.001* |
| PCI | 215(76%) | 118(42%) | p<0.001* |
| CABG | 19(7%) | 20(7%) | p=0.868 |
| *Statistically significant by Chi-square test, p<0.05 | |||
Table 4: Comparing cases and controls regarding management.
Results
Demographic and clinical data of the study population. Among 7000 patients with ACS; 280 patients (4%) met our inclusion and exclusion criteria as ectatic coronary artery disease presented with acute coronary syndrome; and another 280 random patients as a control group without coronary ectasia presented with ACS were studied and included in the final analysis.
The majority of cases were male (262 male; 93%) in the ectatic group and (201 male; 71%) in the control group; which is statistically significant (p<001). The mean age was 58.1 ± 10.9 in the cases and 57 ± 10.0 in the control group.
Hypertension was present in 173 cases (61%) and 184 (65%) in the control patients. 161 of the cases were smokers (57%); and 114 (40%) were in the control group; which is statistically significant (p<001).
Fifty-nine of the cases were dyslipidemic (21%) but 79 were in the control group (28%); which is statistically significant (p=0.05). IDDM was present only in 8 cases (2.8%) and 28 of the control group (9%); while 75 of the experimental group were non-IDDM (26%) versus 109 in the control group (38%); which is statistically significant (p=0.002) for the control group.
Twenty-one of the cases had renal impairment (7.5%) and nine patients in the control group (3.2%) which is statistically significant (p=0.24).
Family history was present in 3 patients of the ectatic group (1.07%) but 2 patients (0.71%) in the control group.
Acute coronary syndrome presentation; echocardiography; and ECG of the study population (Table 5).
| Death | MI | CVS | Bleeding | Arrhythmia | HF | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | |
| No Stent | 14 | 0 | 11 | 3 | 14 | 0 | 14 | 0 | ||||
| Stent | 101 | 2 | 95 | 7 | 95 | 7 | 100 | 2 | ||||
| P value | FEP=1 | FEP=0.1 | FEP=0.5 | FEP=1 | ||||||||
| FEP: Fisher exact significance | ||||||||||||
Table 5: Comparing patients with stents and patients without stents regarding hospital outcomes.
Twenty-two of the cases had a previous ACS (7.8%) and 10 patients in the control group (3.5%); which is statistically significant (p=0.029). Previous PCI was found only in 18 cases (6.4%) but more frequently encountered in 79 patents of the control group (28%). Seventy-nine of the cases (28%) presented with STEMI; 57 patients (21%) with NSTEMI; and 143 patients with unstable angina (51%).
In the control group; 88 patients (31%) presented with STEMI; 65 patients (23%) with NSTEMI; and 127 (46%) with unstable angina. ST segment and T wave changes were encountered in 164 cases (58%) and 151 (54%) in the control group. Echocardiography revealed mild or more than mild mitral valve regurgitation in 76 cases (27%) and 40 patients in the control group (14%); which is statistically significant (P<0.001). RWMA was in 116 cases (41%); and 115 in the control group (41%). The mean EF was 58.3 ± 9.6% in cases and 57 ± 8.9% in the control group.
Management of the study population: (Table 6).
| Death | MI | CVS | Bleeding | Arrhythmia | HF | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | |
| No Stent | 13 | 1 | 11 | 2 | 12 | 1 | 13 | 0 | ||||
| Stent | 91 | 10 | 91 | 1 | 92 | 0 | 90 | 2 | ||||
| P value | FEP=1 | FEP=.04* | FEP=0.1 | FEP=1 | ||||||||
FEP: Fisher exact significance
Table 6: Comparing patients with stents and patients without stents regarding intermediate outcomes.
Ninety cases (32%) were managed medically; but 42 (15%) in the control group; which is statistically significant (p<0.001).
PCI was done in 118 cases (42%) but in 215 of the control group (76%); (p<0.001). CABG was done in 20 cases (7%) and in 19 patients of the control group (7%). Comparing parameters with in-hospital outcomes in the ectatic group undergoing PCI. One hundred and eighteen patients with ectatic CAD presented with ACS underwent PCI.
Most of the cases had a low syntax score: 115 patients (97%) and 3 patients with an intermediate syntax score (3%); with no statistically significant effect on hospital outcome among the 2 groups. Regarding the anatomy of ectatic vessels; RCA was present in 70 patients (41%); LAD in 59 patients (35%); LCx in 34 patients (20%); OM in 3 patients; and LM in 2 patients; with no statistically significant effect on in-hospital outcome between different vessels. Regarding the type of ectasia; type 1 was found in 22 patients (18%); type 2 in 14 patients (11%); type 3 in 32 patients (27%) and type 4 in 50 patients (42%). Aneurysm was found in 27 patients (23%); there was no statistically significant effect on in-hospital outcome between different types.
TIMI flow before PCI was zero in 34 patients (29%); TIMI 1 in 10 patients (8%); TIMI 2 in 27 patients (23%); and TIMI 3 in 47 patients (40%) were statistically significant effects on in-hospital bleeding (MCP=0.011).
Thrombus aspiration was done in 31 patients (26%) with no statistically significant effect on hospital outcomes. Most of the cases underwent balloon dilatation; 111 patients (94%) with no statistically significant effect on in-hospital outcome.
TIMI 0 flow post-PCI occurred only in one patient (0.8%); TIMI 1 in 2 patients (1.7%); TIMI 2 in 13 patients (11%). and TIMI 3 in 102 patients (86%) with no statistically significant effect on hospital outcomes.
Myocardial blush grade after PCI was zero in one patient (0.8%); grade 1 in 2 patients (1.7%); and grade 2 in 13 patients (11%). and grade 3 in 102 patients (86%) with no statistically significant effect on in-hospital outcomes.
A GPIIb/IIIa inhibitor was used in 45 patients (38%) with no statistically significant effect on hospital outcomes. The TIMI score ranges from zero to 5; with a median of 0.5 and a statistically significant effect on an incidence of in-hospital bleeding (p=0.01) (Table 7).
| Death | MI | CVS | Bleeding | Non TVR | HF | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | |
| No Anticoagulant | 114 | 2 | 105 | 10 | 108 | 7 | 113 | 2 | ||||
| Anticoagulant | 2 | 0 | 2 | 0 | 2 | 0 | 2 | 0 | ||||
| P value | FEP=1 | FEP=1 | FEP=1 | FEP=1 | ||||||||
Table 7: Comparing patients on anticoagulants regarding hospital outcomes.
Stent diameter ranges from 2.75 to 4.5 mm with a median of 4 mm; with a statistically significant effect on the incidence of in-hospital arrhythmia (p=0.03) and heart failure (p=0.02). Comparing parameters with intermediate outcomes in the ectatic group undergoing PCI. One hundred and eighteen patients with ectatic CAD presented with ACS underwent PCI. Most of the cases had a low syntax score: 115 patients (97%) and 3 patients with an intermediate syntax score (3%); which had a statistically significant effect on non-TVR in the intermediate outcome (FEP=0.03) to intermediate syntax score. Regarding the anatomy of ectatic vessels; RCA was encountered in 70 patients (41%); LAD in 59 patients (35%); LCx in 34 patients (20%); OM in 3 patients; and LM in 2 patients with a statistically significant effect on mortality in the intermediate outcome; which was higher in patients with ectatic LCX (FEP=0.039) among the other vessels. Regarding the type of ectasia; type 1 was found in 22 patients (18%); type 2 in 14 patients (11%); type 3 in 32 patients (27%) and type 4 in 50 patients (42%). Aneurysm was found in 27 patients (23%); with no statistically significant effect on the intermediate outcome between different types. TIMI 0 flow before PCI was encountered in 34 patients (29%); TIMI 1 in 10 patients (8%); TIMI 2 in 27 patients (23%); and TIMI 3 in 47 patients (40%); with no statistically significant effect on intermediate outcome among the different groups. Thrombus aspiration was done in 31 patients (26%) with no statistically significant effect on intermediate outcomes. Most of the cases underwent balloon dilatation; 111 patients (94%) with no statistically significant effect on the intermediate outcome. TIMI flow after PCI was zero in 1 patient (0.8%); TIMI 1 in 2 patients (1.7%); TIMI 2 in 13 patients (11%); and TIMI 3 in 102 patients (86%) with a statistically significant effect on CVS as an intermediate outcome in patients with TIMI zero (MCP=0.006) (Table 8).
| Death | MI | CVS | TVR | Non TVR | HF | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | |
| No Anticoagulant | 102 | 12 | 101 | 2 | 103 | 0 | 100 | 3 | 101 | 2 | 101 | 2 |
| Anticoagulant | 2 | 0 | 1 | 1 | 1 | 1 | 2 | 0 | 2 | 0 | 2 | 0 |
| P value | FEP=1 | FEP=0.057 | FEP=0.019* | FEP=1 | FEP=1 | FEP=1 | ||||||
Table 8: Comparing patients on anticoagulants regarding intermediate outcomes.
Myocardial blush grade after PCI was zero in one patient (0.8%); grade 1 in 2 patients (1.7%); grade 2 in 13 patients (11%); and grade 3 in 102 patients (86%) with a statistically significant effect on the incidence of CVS as an intermediate outcome in patients with MBG zero (MCP=0.006). A GPIIb/IIIa inhibitor was used in 45 patients (38%) with no statistically significant effect on the intermediate outcome. The TIMI score ranges from zero to 5; with a median of 0.5; with a statistically significant effect on the incidence of myocardial infarction as an intermediate outcome in patients with a higher TIMI score (P=0.03). Stent diameter ranges from 2.75 to 4.5 mm with a median 4 mm with no statistically significant effect on the intermediate outcome. Most of the patients underwent stent deployment during PCI 102 (87%) but 14 patients underwent balloon dilatation only without stenting (13%) with no statistically significant effect on hospital outcome. But there was a statistically significant effect on the incidence of myocardial infarction as an intermediate outcome in patients who underwent balloon dilatation only without stenting (FEP=0.04). NOACs was used in only 2 patients (1.7%) with no statistically significant effect on hospital outcome. But increased incidence of CVS in intermediate outcome (FEP=0.019). Comparing patients on anticoagulants regarding hospital and intermediate outcomes NOACs was used in only 2 patients (1.7%) with no statistically significant effect on hospital outcome. But increased incidence of CVS in intermediate outcome (FEP=0.019). In hospital mortality has been witnessed in 3 ectatic patients (1.07%) but only in 2 patients of the control group (0.71%). Bleeding occurred in 19 patients of the ectatic group (6.78%) and 20 patients of the control group (7.14%). Arrhythmia occurred in 19 patients of the first group (6.78%) but in 18 patients of the control group (6.42%). Six patients of the ectatic group developed acute heart failure (2.14%) and 9 patients of the control group (3.21%). TVR was indicated to one patient with coronary artery ectasia due to instent thrombosis and none of the control group.
Regarding follow-up of the cases patients with ectatic CAD showed a higher mortality (23 patients, 8.2%) versus only 8 patients of the control group (2.8%); which is statistically significant (p=0.005). Seven patients of the ectatic group developed myocardial infarction (2.5%); and 3 patients of the control group (1%) CVS occurred in one patient with ectatic CAD (0.35%) but not in the control group. Bleeding was encountered only in one patient of the first group (0.35%) but none of the control group. None of the patients with ectatic CAD was found to have any arrhythmia (0%); on the other hand arrhythmia occurred in 2 patients of the control group (0.8%). Three patients of the first group developed heart failure (1%) and none of the control group. TVR was indicated to six patients with ectatic CAD (2.14%) and three patients in the control group (1%). Non-TVR was indicated for 4 patients of the first group (1.4%) but only for two patients of the control group (0.7%). Antiplatelets and anticoagulants of the study population (Table 9).
| Control | Cases | (p) | |
|---|---|---|---|
| Death | 8(2.8%) | 23(8.2%) | p=0.005* |
| MI | 3(1%) | 7(2.5%) | p=0.171 |
| CVS | 0(0%) | 1(0.4%) | FEP=0.48 |
| Bleeding | 0(0%) | 1(0.4%) | P=0.303 |
| Arrhythmia | 2(0.8%) | 0(0%) | FEP=0.499 |
| HF | 0(0%) | 3(1%) | FEP=0.114 |
| TVR | 3(1%) | 6(2.1%) | FEP=0.327 |
| Non TVR | 2(0.7%) | 4(1.4%) | FEP=0.438 |
*Statistically significant by Chi square test, p<0.05; FEP: Fisher Exact significance
Table 9: Comparing cases and controls regarding intermediate outcome.
Clopidogrel was used as an antiplatelet in 193 patients with ectatic CAD (69%) and in 218 patients in the control group (77%). Ticagrelor was prescribed as an antiplatelet drug in 80 ectatic patients (29%) but in 62 patients of the control group (22%). Warfarin was used in 5 patients of the ectatic group (1.7%) and 3 patients of the control group (1%). NOACs was used only in 4 patients of the first group (1.4%) but none of the control group. Predictors of mortality as in hospital outcome (Table 10). In the multivariate logistic regression model; male sex (0.010); previous ACS (0.021); and presentation with STEMI (0.018) were found as independent predictors of in-hospital mortality; p=0.01*. Predictors of mortality as an intermediate outcome. In the multivariate logistic regression model; the ectatic group (0.005) and presentation with STEMI (0.001) were found to be independent predictors of mortality as an indeterminate outcome. In a multivariate logistic regression model; stent diameter (p=0.005) and also thrombus aspiration were significant predictors (p=0.047) of in-hospital MACE. Predictors of MACE as an intermediate outcome. The logistic regression model predicting intermediate outcome is not statistically significant (p=0.217) (Figure 2).
| Control | Cases | (p) | |
|---|---|---|---|
| Clopidogrel (Plavix) | 218(77%) | 193(69%) | p=0.024* |
| Ticagrelor (brilique) | 62(22%) | 80(29%) | p=0.072 |
| OAC | 3(1%) | 5(1.7%) | FEP=0.503 |
| NOAC | 0(0%) | 4(1.4%) | FEP=0.061 |
*Statistically significant by Chi square test, p<0.05; FEP: Fisher Exact significance
Table 10: Comparing cases and controls regarding antiplatelets and anticoagulants.
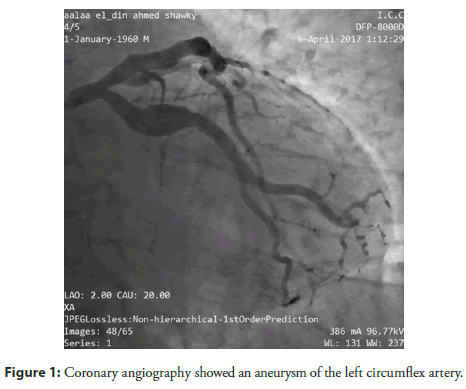
Figure 2: Coronary angiography showed an aneurysm of the left circumflex artery.
Case no. 14
52-year-old male patient HTN and smoker presented with NSTEMI
Coronary angiography showed an aneurysm of the left circumflex artery.
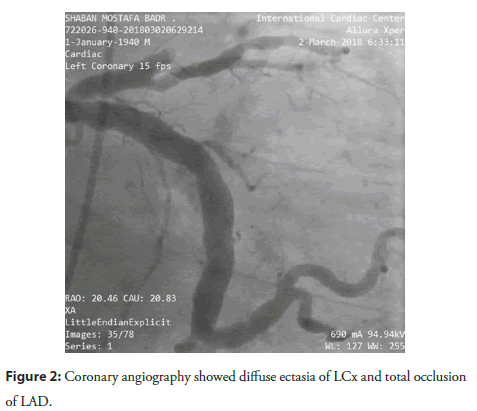
Case no. 180
45-year-old male smoker presented with unstable angina.
Coronary angiography showed diffuse ectasia of LCx and total occlusion of LAD. PPCI was done in LAD with one DES (Figure 3).
Figure 3: Coronary angiography showed diffuse ectasia of LCx and total occlusion of LAD.
Discussion
Although CAE is associated with abnormal vessel dilatation; disturbed coronary flow; and enhanced thrombogenicity; its association with cardiac events has not been fully characterized. CAE is generally defined according to the ratio of the size of the ectatic segment to that of the adjacent normal reference segment. (4; 9) Kruger, et al. developed another definition of CAE that used the mean size of each coronary segment in an age and sex-matched cohort without heart disease as a reference value [16,17].
In our study; the conventional definition of CAE was applied. Consequently; we identified CAE in 4% of the patients with ACS in the same period; which was within the range of the previously reported prevalence (0.9%-5.3%) [18].
The presence of CAE in the culprit vessel has been previously analyzed in studies with smaller sample sizes: Yip, et al. [15] found CAE in the culprit vessel in 2.6% of a cohort of 924 patients; whereas in another study consisting of 643 patients with myocardial infarction; the frequency of CAE was 4.8%. The results of the present study confirm a previous series and reported a frequency of CAE (irrespective of location) of 3.6% and 3.2% when considering the presence of CAE in the culprit vessel.
In our study; male gender; renal impairment; dyslipidemia; and smoking were independently associated with ectatic IRA. Male predominance of more than 90% resembles prior findings [19]. Male gender; dyslipidemia; renal impairment; and smoking were demonstrated to be associated with higher inflammatory levels [20,21]. Higher C-reactive protein and interleukin levels were found in patients with smoking and dyslipidemia. Smoking was also shown to be associated with coronary artery calcification; which also plays a role in the process of CAE formation. We think these findings could explain the link between dyslipidemia; renal impairment; smoking; and CAE. However; the differences in age and family history did not reach statistical significance in our study.
In our study; previous ACS were found more in CAE; which may be related to more risk factors associated with CAD. While the majority of patients in our study with ACS with CAE presented with unstable angina; less than half of them eventually underwent PCI (42%); the remaining half were managed medically or referred to elective CABG.
In our study; there was no significant difference between CAE and control regarding hospital MACE. But male sex; previous ACS; and presentation with STEMI are independent predictors of hospital mortality.
In our study; we found that CAE and STEMI presentation are independent predictors of mortality as intermediate outcomes. A large thrombus burden and a low initial TIMI flow were observed in patients with CAE; which is consistent with previous studies. Although thrombus aspiration and glycoprotein IIb/IIIa inhibitors have been frequently used in patients with AMI and CAE. The occurrence of no-reflow or distal embolization is very frequent [22,23]. We observed a non-significantly higher frequency of final TIMI flow<3 in patients with CAE compared to non-CAE patients. Proper selection of the stent According to the size and extent of CAE; it is critical to reduce the risk of stent thrombosis and stent migration.
In patients with AMI; we observed that the presence of CAE was associated with increased mortality at 3-4 year follow-up. Compared to patients without CAE.
The difference in acute stent thrombosis was also nonsignificant in our study. Karabulut, et al. found no difference in no-reflow rates in ectatic and non-ectatic coronary arteries after primary PCI in 26 patients with STEMI. They suggested that the higher rate of early application of antiaggregant such as acetylsalicylic acid; clopidogrel; and glycoprotein 2b/3a antagonists may have contributed to these results. As expected; no-reflow rates were significantly higher in our study despite higher thrombectomy rates among patients with ectatic IRA. However; this difference did not yield any change in in-hospital and 1-year outcomes.
In our study; we did not find any difference in the in-hospital outcomes of 14 patients with only balloon angioplasty but an increased rate of recurrent MI with follow-up. However; given that this was a very limited sample size; we are not able to make definitive suggestions about treatment strategies.
Regarding the angiographic features of the equation In CAD patients in our study; RCA was present in the majority of the cases; this higher predisposition of the RCA to develop CAE as compared to the other coronary arteries has been previously described; but the underlying pathophysiology remains unknown. In addition; multivessel CAE is infrequent and has been described in only 25% of patients with CAE.
But there is a statistically significant effect on mortality in the intermediate outcome; which was higher in patients with ectatic LCX (FEP=0.039) among the other vessels; which may be explained by the presence of multivessel CAD with higher MACE compared with single vessel disease.
Most of the cases had a low syntax score with no statistically significant effect on hospital outcome among the 2 groups but had a statistically significant effect on non-TVR in intermediate outcome to intermediate syntax score; which also may be explained by the fact that a higher syntax score was associated with multi-vessel than single-vessel disease; with an increased rate of revascularization [24].
To our knowledge; only one prior study has assessed the relationship of the grade of CAE with clinical outcomes. Zhang, et al. studied 512 CAE patients (76 with isolated CAE and the rest with CAE+CAD) in a Chinese population. Each patient was graded according to the Markis classification; and the mean follow-up was 34.6 months. Most patients (371/512) had low-grade CAE (Markis 3/4). The study found no significant difference in major adverse cardiac event rate in the various CAE groups. This is similar to our study where we found no significant and independent association of high-grade CAE as compared to low-grade CAE for risk of ACS and mortality.
The proportion of patients with high-grade CAE was significantly lower in the study by Zhang, et al. (27.5%) as compared to Gunasekaran, et al. [25] (48%); which could potentially explain the higher incidence of ACS on follow-up in Gunasekaran, et al. This is also similar to a recent study from India; where 49.4% had high-grade CAE.
There is not much convincing data regarding the prognosis and outcomes in patients with ectatic IRA. Although most of the previous research was not designed to compare STEMI patients with ectatic IRA to a control group; our findings regarding in-hospital and long-term mortality rates were consistent with previous findings. Moreover; we also found similar revascularization rates during 3-year follow-up among our population.
In our study; TIMI flow before PCI was zero in 29% of cases; with an increased risk of in-hospital bleeding as more use of anticoagulation and GP IIb/IIIa inhibitors. But increased risk of CVS (one patient) as an intermediate outcome with more use of NOACs as TIMI flow and MBG was zero post-PCI.
Both postmortem studies and several case reports describe instances of acute MI in CAE patients with acute thrombotic occlusion at the ectatic segments without occlusive CAD [26,27]. Thus; it has been suggested that use of anticoagulants may help reduce the risk of MI in these patients.
Conclusion
The incidence of coronary ectasia is 4.9% among acute coronary syndrome patients. Comparing the ectatic group vs. the non-ectatic; respectively mortality was 8.2% vs. 2.8% (P<.005). Male incidence: 93% vs. 71%; P<0.001. Hypertension was present in 61% vs. 65% P=NS. Smokers 57% vs. 114 40% (p <001). Dyslipidemic (21%) vs. (28%) (p=0.05). Diabetes type II: (26%) versus (38%) (p=0.002). Renal impairment (7.5%) vs. (3.2%) (p=0.24). Acute coronary syndrome presentation: Previous ACS (7.8% vs. (3.5%); (p=0.029). Previous PCI (6.4%) vs. (28%). (28%) presented with STEMI; (21%) with NSTEMI; and unstable angina (51%). In the control group; 31% presented with STEMI; 23% with NSTEMI; and 46% with unstable angina. ST segment and T wave changes were encountered in (58%) vs. (54%) in the control group.
Echocardiography: Mitral valve regurgitation in 76 cases (27%) vs. 40 patients in the control group (14%) (P<.001). RWMA was in 41% and 115 in the control group (41%). The mean EF was 58.3 ± 9.6% vs. 57 ± 8.9% in the control group. Management of the study population: medical management (32% vs. 15%) in the control group (p<.001). PCI was done in (42%) vs. (76%) (p<.001). CABG was done in (7%) vs. (7%).
In hospital outcomes: One hundred and eighteen patients with ectatic CAD presented with ACS underwent PCI. Most of the cases had a low syntax score: 115 patients (97%) and 3 patients with an intermediate syntax score (3%); with no statistically significant effect on hospital outcome among the 2 groups. Regarding the anatomy of ectatic vessels; ectasia was present in RCA in 41%; 35% in LAD; 20% in LCx; 3 patients in OM; and 2 patients in LM; with no statistically significant effect on hospital outcome between different vessels. Regarding the type of ectasia (ectasia or aneurysm); there was no statistically significant effect on hospital outcomes between different types. TIMI flow before PCI was zero in 29%; TIMI 1 in 8%; TIMI 2 in 23%; and TIMI 3 in 40%; with a statistically significant effect on in-hospital bleeding (0.011).
Thrombus aspiration was done in 26% with no statistically significant effect on hospital outcome. Most of the cases underwent balloon dilatation; 111 patients (94%); with no statistically significant effect on hospital outcome.
A GPIIb/IIIa inhibitor was used in 45 patients (38%); with no statistically significant effect on hospital outcome. Comparing patients on anticoagulants regarding hospital and intermediate outcomes. NOACs were used in only 2 patients (1.7%) with no statistically significant effect on hospital outcome. But increased incidence of CVS in intermediate outcome (FEP=0.019). In hospital mortality has been witnessed in 3 ectatic patients (1.07%); but only in 2 patients of the control group (0.71%). Bleeding occurred in 19 patients of the ectatic group (6.78%) and 20 patients of the control group (7.14%). Regarding follow-up of the cases; patients with ectatic CAD showed a higher mortality (23 patients; 8.2%) versus only 8 patients of the control group (2.8%) (p=0.005). Predictors of mortality as in hospital outcome: male sex (0.010); previous ACS (0.021); and presentation with STEMI (0.018) were found as independent predictors of inhospital mortality.
Declarations
This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration. The ethics department of our faculty of medicine approved the study protocol in 2019. Informed Consent: Written informed consent was taken from all patients.
Consent for Publication
All authors agree to publication.
Availability of data and material: The master chart and patients’ files are available on request with Dr. EA.
Conflict of Interest
Financial Disclosure or Funding: The study was done without any financial support from any agent.
Authors' Contributions
Samir Rafla: Wrote the paper and submitted it; Amr Zaki: Idea and design of the work; the main catheterizer; Mohamed Sadaka: Main catheterizer; Elsayed Abdelaaty: This is the doctoral thesis of Dr. Elsayed Abdelaaty; he collected the data and wrote the thesis.
Acknowledgement
We thank all residents and technicians who helped in the catheterization of patients.
Authors' information (optional).
Samir Rafla: CV Emeritus professor of cardiology at Alexandria University and assessor (grader) in the National Council for the Promotion of Professors in Cardiology. Fellow of the American College of Cardiology (FACC) Emeritus Fellow; European Society of Cardiology (FESC). Fellow Heart Rhythm Society (FHRS) Member; Heart Rhythm Society EHRA Senior Member; Egyptian Society of Cardiology Google Scholar publications>100.
References
- Puymirat E, Simon T, Cayla G, et al. Acute myocardial infarction: Changes in patient characteristics, management, and 6-month outcomes over a period of 20 years in the FAST-MI program (French Registry of Acute ST-Elevation or Non-ST-Elevation Myocardial Infarction) 1995 to 2015. Circulation. 136(20):1908-1919 (2014).
- Jaffe AS. Third universal definition of myocardial infarction. Glob Heart. 46(1-2):1-4 (2013).
- Panju AA, Hemmelgarn BR, Guyatt GH, et al. The rational clinical examination. Is this patient having a myocardial infarction? JAMA. 280:1256-1263 (1998).
- Swaye PS, Fisher LD, Litwin P, et al. Aneurysmal coronary artery disease. Circulation. 67(1):134-138 (1983).
- Hartnell GG, Parnell BM, Pridie RB, et al. Coronary artery ectasia. Its prevalence and clinical significance in 4993 patients. Br Heart J. 54(4):392-395 (1985).
- Markis JE, Joffe CD, Cohn PF, et al. Clinical significance of coronary arterial ectasia. Am J Cardiol. 37(2):217-222 (1976).
- Elahi MM, Dhannapuneni RV, Keal R, et al. Giant left main coronary artery aneurysm with mitral regurgitation. Heart. 90(12):1430 (2004).
- Kawsara A, Núñez Gil IJ, Alqahtani F, et al. Management of coronary artery aneurysms. JACC Cardiovasc Interv. 11(13):1211-1223 (2018).
- Devabhaktuni S, Mercedes A, Diep J, et al. Coronary artery ectasia-a review of current literature. Curr Cardiol Rev. 12(4):318-323 (2016).
- Roberts WC. Natural history, clinical consequences, and morphologic features of coronary arterial aneurysms in adults. Am J Cardiol. 108(6):814-821 (2011).
- Antoniadis AP, Chatzizisis YS, Giannoglou GD, et al. Pathogenetic mechanisms of coronary ectasia. Int J Cardiol. 130(3):335-343 (2008).
- Mavrogeni S. Coronary artery ectasia: From diagnosis to treatment. Hellenic J Cardiol. 51(2):158-63 (2010).
- Khedr A, Neupane B, Proskuriakova E, et al. Pharmacologic management of coronary artery ectasia. Cureus. 13(9):e17832 (2021).
- Ipek G, Gungor B, Karatas MB, et al. Risk factors and outcomes in patients with ectatic infarctârelated artery who underwent primary percutaneous coronary intervention after ST elevated myocardial infarction. Catheter Cardiovasc Interv. 88(5):748-753 (2016).
- Yip HK, Chen MC, Wu CJ, et al. Clinical features and outcome of coronary artery aneurysm in patients with acute myocardial infarction undergoing a primary percutaneous coronary intervention. Cardiology. 98(3):132-140 (2002).
- Krüger D, Stierle U, Herrmann G, et al. Exercise-induced myocardial ischemia in isolated coronary artery ectasias and aneurysms (“dilated coronaropathy”). J Am Coll Cardiol. 34(5):1461-1470 (1999).
- Demopoulos VP, Olympios CD, Fakiolas CN, et al. The natural history of aneurysmal coronary artery disease. Heart. 78(2):136-141 (1997).
- Giannoglou GD, Antoniadis AP, Chatzizisis YS, et al. Prevalence of ectasia in human coronary arteries in patients in northern Greece referred for coronary angiography. Am J Cardiol. 98(3):314-318 (2006).
- Fujii T, Sakai K, Kimura M, et al. Coronary flow improvement following unsuccessful primary percutaneous coronary intervention in ST-elevation myocardial infarction with diffuse ectatic coronary artery. Eur Heart J Acute Cardiovasc Care. 6(7):623-631 (2017).
- Harrison DG, Guzik TJ, Lob HE, et al. Inflammation, immunity, and hypertension. Hypertension. 57(2):132-140 (2011).
- McEvoy JW, Blaha MJ, DeFilippis AP, et al. Cigarette smoking and cardiovascular events: Role of inflammation and subclinical atherosclerosis from the MultiEthnic study of atherosclerosis. Arterioscler Thromb Vasc Biol. 35(3):700-709 (2015).
- Pauletto P, Rattazzi M. Inflammation and hypertension: The search for a link. Nephrol Dial Transplant. 21(4):850-853 (2006).
- Zhang Y, Huang QJ, Li XL, et al. Prognostic value of coronary artery stenoses, markis class, and ectasia ratio in patients with coronary artery ectasia. Cardiology. 131(4):251-259 (2015).
- Karabulut A, Cakmak M, Uzunlar B. Association between preinfarction angina and coronary artery ectasia in the acute myocardial infarction. Acta Cardiologica. 66(4):509-514 (2011).
- Harikrishnan S, Sunder KR, Tharakan J, et al. Coronary artery ectasia: Angiographic, clinical profile and follow-up. Indian Heart J. 52(5):547-553 (2000).
- Gunasekaran P, Stanojevic D, Drees T, et al. Prognostic significance, angiographic characteristics and impact of antithrombotic and anticoagulant therapy on outcomes in high versus low grade coronary artery ectasia: A longâterm followâup study. Catheter Cardiovasc Interv. 93(7):1219-1227 (2019).
- Furugen M, Takagawa Y. Staged interventional management of a massive thrombus related to coronary artery ectasia in acute coronary syndrome. Cardiovasc Interv Ther. 27(1):57-61 (2012).