Research Article - Interventional Cardiology (2015) Volume 7, Issue 1
Clinical impact of the switch from femoral to radial approach for coronary intervention: a single-center experience
- Corresponding Author:
- Adrian Ionescu
Morriston Regional Cardiac Centre
Wales, SA6 6NL, UK
E-mail: Adrian.Ionescu@wales.nhs.uk, dr.o.a@doctors.net.uk
Abstract
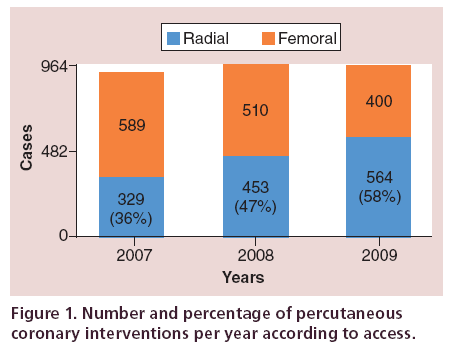
Aim: To evaluate the safety profile during a 3-year transition from default transfemoral access to default transradial access (TRA) for percutaneous coronary interventi ns in a tertiary cardiac center. Methods: Data were collected from electronic databases n all percutaneous coronary interventions from 2007 to 2009. Results: Two th usand eight hundred and forty-five procedures were recorded. TRA increased fr m 36 to 58% of procedures over the study period. Postprocedure blood transfusi n equirements, incidence of hematoma and hospital length of stay were less am ng TRA cases. Fluoroscopy time, procedure time and mortality were similar in both g ups. Access site crossover was higher among TRA cases but not prohibitive. Conclusion: T ansitioning from a default transfemoral access to TRA unit was not associated with an adverse clinical or safety profile.
Keywords
bleeding, coronary intervention, femoral access, fluoroscopy time, hematoma, hospital stay, mortality, radial access, transfusion, transition
There is an increasing interest worldwide in transradial coronary angiography and intervention. The evidence in favor of transradial approach (TRA) for percutaneous coronary intervention (PCI) is accumulating [1,2]; nonetheless radial access is still underutilized in many countries.
In our unit, the TRA was first used in 2006 after the appointment of two ‘defaultradial’ operators. Afterward, the switch toward default TRA was mainly driven by the accumulating evidence of reduced morbidity. The decision to adopt it and the extent to which it was used was left entirely at the discretion of individual operators. Operator’s increasing expertise with the technique and overall clinical experience most likely influenced choice of access thereafter.
There was no formal TRA training program within the department; however, all operators attended at least one transradial catheterization master class at national or international meetings. There was extensive informal tuition and information exchange between peers in the department.
The voluntary switch over to default TRA provided us with the ideal opportunity to study and characterize in retrospect the differences in outcome between TRA and transfemoral access (TFA) for PCI in a tertiary cardiac unit over a 3-year transition period (2007–2009, Figure 1).
Methods
Setting
The study took place at Morriston Regional Cardiac Centre, Swansea, UK, which is a tertiary center serving a population of 1,000,000 and performing approximately 1100 percutaneous interventional procedures per year, with seven operators.
Data collection
Data were collected retrospectively over a 3-year period (2nd January 2007 to 1st December 2009) from a departmental PCI database, electronic patient’s records including electronic discharge summaries and the Welsh demographic database.
The choice of the study period was determined by two factors. Firstly, a new database was introduced in 2007 and hence data from 2006 were not included. Secondly, radial access became our default route in 2009 in at least >50% of cases, therefore data analysis beyond this point would not have addressed our aim.
Arterial access site, sex, age, procedure urgency, use of heparin and/or glycoprotein IIb/IIIa antagonists (Gp 2b/3a), recent thrombolysis, previous PCI, previous coronary artery bypass grafting (CABG) and presence of cardiogenic shock were the core variables collected. Only cases with a full core dataset were retained for analysis. A secondary set of variables, including anonymized operator identity, creatinine and hemoglobin levels, transfusion requirements, hospital outcomes and survival status (in-hospital and 1-year mortality) were also collected.
Outcomes
The main outcome measures were access site crossover, length of stay in the tertiary center excluding pretertiary hospital transfer waits, blood transfusion, hematoma (as a binary variable regardless of size), in-hospital mortality and 1-year mortality.
We examined electronic patient’s records for evidence of peri-procedural bleeding and we collected pre- and postprocedural hemoglobin levels (lowest value within 30 days of PCI) as a surrogate marker for bleeding. We used the HORIZON definition of bleeding specifically reduction in hemoglobin concentration of ≥4g/dl [3]. This definition was used as it did not necessitate a clinical assessment which was not available in the database.
There is no routine assessment of radial artery patency postprocedure in our center therefore the rate of postprocedural radial artery occlusion is not documented before, during or after the transition period.
After completion of data collection 20% of the data (600/2845 cases) were randomly rechecked for quality assurance purposes.
Analysis & statistical methods
All calculations were performed using SPSS 17.0. (IBM, NY, USA); p values of <0.05 were considered significant for all analyses. Continuous variables were expressed as standard deviations and categorical variables as percentages. Continuous variables were compared using the independent sample t-test. Categorical variables were assessed using Chi-square test.
We ran several analyses in order to maximize our understanding of the differences between TRA and TFA PCI during the transition period and to minimize bias in this nonrandomized cohort. Firstly, raw unadjusted data were analyzed using univariate regression, to discern the impact of the variables on the end points. Secondly, approximately a fifth of our patients (520 patients – 260 cases in the radial group and 260 in the femoral group, Delta <5%) were propensity score matched [4] on the following variables: age, sex, operator, and urgency of procedure and history of CABG. We repeated the univariate analyses between the matched groups. Finally, logistic regression and best models using the c-statistics (receiver-operating characteristic curve) on the total study group were used to identify complex relationships among different variables and their impact on the end points. Kaplan-Meier survival curves were generated. A small number of missing values, approximately 10%, outside the core dataset were replaced using multiple imputations. Pooled data, after rounding to the nearest one when appropriate, were used.
Results
Unadjusted data
There were 3188 PCIs during the study period. Only 2845 PCIs (89%) performed in 2660 patients had complete ‘core’ datasets. Out of these, 1346 were performed by TRA and 1499 by TFA. The demographic and clinical characteristics of the patients are presented in Table 1.
| Variable | Total PCIs | TRA (%) | TFA (%) | p-value | |
|---|---|---|---|---|---|
| n | 2845 | 1346 (47.3%) | 1499 (52.7%) | – | |
| Year | |||||
| 2007 | 918 (32%) | 329 | 589 | <0.01 | |
| 2008 | 963 (34%) | 453 | 510 | <0.01 | |
| 2009 | 964 (34%) | 564 | 400 | <0.01 | |
| Age (years) | 63.6 (11) | 63.5 (11) | 63.9 (11) | 0.666 | |
| Female sex | 761 (26%) | 294 (38.6%) | 467 | (61.3%) | <0.01 |
| Procedure urgency | |||||
| Elective | 924 (32%) | 464 | 460 | NS | |
| Urgent | 1468 (51%) | 660 | 808 | NS | |
| Emergency | 449 (17%) | 220 | 229 | NS | |
| Salvage | 4 | 2 | 2 | NS | |
| Clinical syndrome | |||||
| Stable | 933 (32%) | 467 | 466 | NS | |
| ACS | 1508 (53%) | 682 | 826 | NS | |
| Rescue PCI | 173 (6%) | 88 | 85 | NS | |
| Primary PCI | 231 (9%) | 109 | 122 | NS | |
| Prior MI | 569 (20%) | 245 (43%) | 324 (57%) | 0.011 | |
| Prior CABG | 171 (6%) | 39 (22.8%) | 132 (77.2%) | <0.01 | |
| Prior PCI | 422 (14.8%) | 176 (41.8%) | 246 | (58.2%) | 0.013 |
| Recent thrombolysis | 506 (17.8%) | 250 (49.5%) | 256 (50.9%) | 0.16 | |
| Cardiogenic shock | 52 (1.8%) | 16 (30.7%) | 36 (69.2%) | 0.17 | |
| Arterial management | |||||
| TR band | 1342 | N/A | |||
| Angioseal | N/A | 910 | |||
| Manual compression | 4 | 589 | |||
| Angina severity | |||||
| No angina | 635 (22.3%) | 305 | 329 | NS | |
| No limitation on DL | 97 (3.4%) | 111 | 208 | NS | |
| Slight limitation | 520 (18%) | 575 | 1095 | NS | |
| Marked limitation | 378 (13%) | 426 | 804 | NS | |
| Pain at rest | 46 (1.6%) | 57 | 103 | NS | |
| Diabetes mellitus | 413 (14.5%) | 181 (43.8%) | 232 | (56.2%) | 0.69 |
| Serum Creatinine | 92.4 (44) | 90 (44.6) | 94 (44.6) | 0.39 | |
Table 1: Clinical characteristics of the patients.
Adoption of TRA PCI & number of vessels & lesions treated
Radial access was increasingly adopted during the study period (Table 1 & Figure 1). Female sex (10 vs 16.4%, p <0.01), a history of CABG (1.4 vs 4.6%, p <0.01) and cardiogenic shock (0.6 vs 1.8%, p = 0.011) were more prevalent in patients having femoral access. The clinical urgency of the procedure (elective, urgent vs emergency [STEMI cases]) did not influence access route (Table 1). Patients having angioplasty via the femoral approach had more vessels (1.22 vs 1.18, p = 0.03) attempted and a trend toward more lesions (1.41 vs 1.37, p = 0.09), but had lower usage of Gp 2b/3a antagonists (8.7 vs 9.7%, p = 0.003) and received lesser amounts of peri-procedural heparin than those treated via TRA (6100 [SD: 3853] vs 6700 [SD: 3689] units, p <0.01) (Table 2).
| Variable | All | TRA | TFA | p-value |
|---|---|---|---|---|
| Number of vessels attempted | 1.2 | 1.18 | 1.22 | 0.033 |
| Number of lesions attempted | 1.39 | 1.37 | 1.41 | 0.09 |
| Number of stents used | 1.08 | 1.06 | 1.10 | 0.1 |
| Gp2b3a use | 525 (18.5%) | 277 (52.7%) | 248 (47.3%) | 0.003 |
| Heparin (IU) | 6400 | 6700 | 6100 | <0.01 |
| Guide Cathere Size Mode | 6 f | 6 f | 6 f | N/A |
| Mean | 6.05 | 6.01 | 6.1 | <0.01 |
| Screening time (min) | 11.45 | 11.77 | 11.18 | 0.151 |
| Procedure time (min) | 45.84 | 46.76 | 44.97 | 0.64 |
| Hospital stay (days) | 2 | 1.44 | 2.13 | <0.01 |
Table 2: Procedural characteristics.
Procedural characteristics & outcome measures
Access site crossover due to inability to complete the procedure was 3.2% (43/1341 cases) in the radial group and 0.2% (3/1493 cases) in the femoral group (p <0.01). Over the transition period, 0, 6 and 37 radial cases crossed over to TFA in 2007, 2008 and 2009, respectively (p <0.01), reflecting an increase in the number of default radial procedures over time. The commonest cause for radial access failure was arterial spasm (15 cases), followed by tortuosity (11 cases), unable to pass wire (six cases), absent palpable pulse (four cases), arterial dissection (two cases), lack of guide support (two cases), accessory radial artery (one case), unable to cannulate the radial artery (one case) and radial artery perforation (one case). The femoral access failure cases were due to weak palpable pulse, unable to pass a wire and a case of severe spasm. Among radial cases, there was a trend toward more crossover in patients with previous PCI (5.8 vs 2.2%, p = 0.08). Variables such as age, sex and renal failure were not different between the two groups (p = NS).
Fluoroscopy time did not differ between the two groups (radial 11.77 min vs femoral 11.18 min, p = 0.151), neither the procedure time (radial 46.67 min vs femoral 44.97 min, p = 0.64).
There was no difference for in-hospital mortality (0.1 vs 0.4%, p = 0.127) or 1-year mortality (1.4 vs 2.2%, p = 0.061) between the TRA and the TFA approaches, although there was a numerical trend toward fewer deaths among TRA cases (Table 3).
| Outcome measure | Radial PCIs | Femoral PCIs | p-value |
|---|---|---|---|
| Access site crossover | 43 (3.2%) | 3 (0.2%) | <0.01 |
| In-hospital mortality | 4 (0.1%) | 10 (0.4%) | 0.127 |
| One-year mortality | 41 (1.4%) | 63 (2.2%) | 0.061 |
| Transfusion | 21 (0.7%) | 45 (2.3%) | 0.007 |
| Hematoma | 14 (0.5%) | 63 (2.2%) | <0.01 |
Table 3: Unadjusted outcome measures.
Transfusion (0.7 vs 2.3%, p = 0.007) and accesssite hematoma (0.5 vs 2.2%, p <0.01) were lower for TRA even though patients in the radial group had more exposure to Gp 2b/3a antagonists. The incidence of access-site hematoma declined over the study period (Table 4). Pre- and post-PCI hemoglobin levels were available for 1136 procedures. There was a trend toward fewer bleeding cases among TRA than TFA (0.2% [two cases] vs 1.3% [13 cases], p = 0.07).
| Outcome measure | 2007 | 2008 | 2009 | p-value | |
|---|---|---|---|---|---|
| Hematoma | 36 (1.3%) | 28 (1%) | 13 (0.5%) | 0.002 | |
| Transfusion | 20 (0.7%) | 26 | (0.9%) | 33 (1.2%) | 0.261 |
| 1-year mortality | 26 (0.9%) | 37 | (1.3%) | 41 (1.4%) | 0.251 |
| Hospital stay (days) | 2 | 1.76 | 1.87 | 0.330 | |
Table 4: Outcome measures during the transition period.
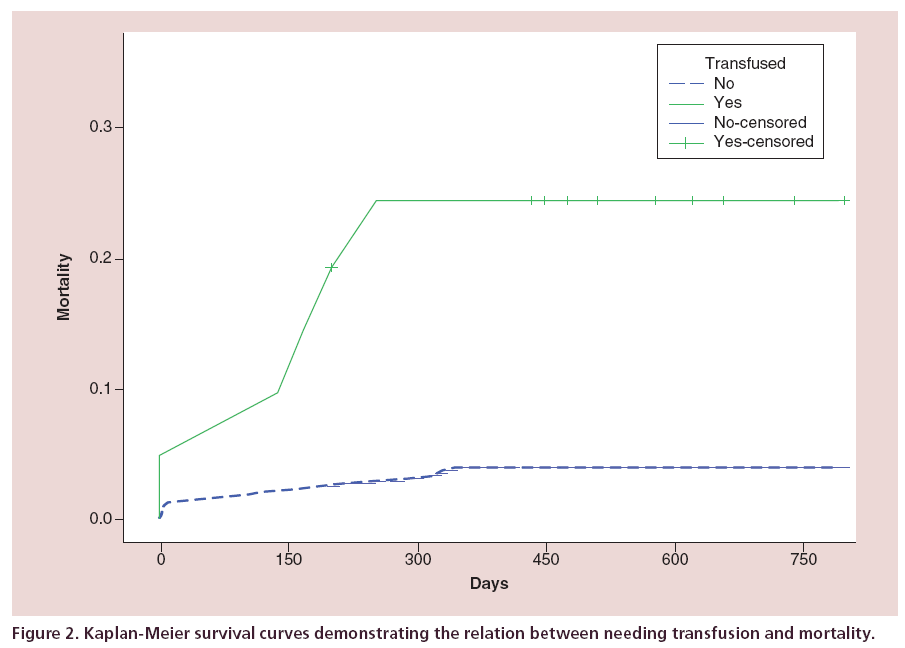
There was a strong association between transfusion and 1-year mortality (unadjusted odds ratio [OR]: 7.19; 95% CI: 4.36–11.86; p <0.01; Kaplan-Meier survival curves, Figure 2).
TFA PCI patients stayed in hospital on average 2.13 (3.7) days; range (0–43), while TRA PCIs patients stayed only 1.44 (2.6) days; range (0–62) (p <0.01). Hospital length of stay was similar in years one, two and three over the transition period (p = 0.33, Table 4).
The major and net adverse clinical events (MACE/ NACE; death, MI, percutaneous revascularisation and bleeding [excluding stroke]) have been summarized in Table 5. As there was no electronic database to identify the incidence of cerebrovascular events, this outcome was excluded from our study.
| MACE/NACE | Radial | Femoral | p-value |
|---|---|---|---|
| One-year mortality | 1.4% | 2.2% | 0.061 |
| MI | 3.7% | 3.6% | 0.49 |
| Any percutaneous revascularization | 5.8% | 6.3% | 0.326 |
| Bleeding | 0.2% | 1.3% | 0.07 |
| Stoke | Unable to comment |
Table 5: MACE and NACE during the study period.
Propensity score matching
In the propensity score matched cohort there was no difference in mortality, need for transfusion or access-site hematoma between TRA and TFA. TRA patients had more exposure to Gp 2b/3a antagonists (3.8 vs 6.9%, p = 0.017). The difference in length of hospital stay became insignificant after propensity score matching (mean hospital stay 1.63 (0–44 (3))) days for both groups (TRA 1.6 (3.2), TFA 1.6 (2.7), range 0–44, p = NS). Crossover from TRA to TFA occurred in six cases (1.2%) and two (0.4%) TFA cases were converted to TRA (p = 0.143).
Logistic regression
Age, cardiogenic shock (adjusted OR: 21.36; 95% CI: 6.48–70.38, relative risk 16; 95% CI: 6.5–39) and red blood cell transfusion (adjusted OR: 7.70; 95% CI: 2.30–25.80, relative risk 6.4; 95% CI: 2.5–16) were the only significant determinants of 1-year mortality.
Gender (OR for a female: 2.7; 95% CI: 1.78–4.14), development of access-site hematoma (OR: 5.4; 95% CI: 2.49–11.7) and serum creatinine above 150 umol/l (OR: 3.3; 95% CI: 1.7–6.7) were the only factors associated with the need for red blood cell transfusion. The transfused group had higher serum creatinine levels (119 vs 87 umol/l, p <0.01).
Discussion
After a slow start, the transradial approach is gaining widespread usage, although the US centers have been sluggish compared with Europe in adopting it. Its proponents invoke the reduced risk of severe bleeding as well as patient comfort as the main reasons for expanding its use. The opponents point to the slow learning curve [5], the potential for longer procedures compared with the femoral approach and to longer fluoroscopy times [6], as arguments for continuing with the time-honored femoral approach.
We sought to study the differences in outcome between TRA and TFA PCI during our departmental transition period toward default radial access.
Bleeding & transfusion requirement
Procedure-related bleeding is a significant predictive risk factor for death following coronary intervention [3]. This makes TRA PCI particularly attractive, in view of its association with reduced bleeding rates. In the National Cardiovascular Data Registry which included 593,094 procedures from more than 600 centers, Rao et al. [7] reported significantly fewer bleeding complications, OR for any bleeding complication was 0.42 (CI: 0.31–0.56) for TRA versus TFA PCI. A posthoc analysis of the RIVAL [8] study also showed that the rate of bleeding was less with radial PCIs.
Blood transfusions have been used as a surrogate marker for bleeding as data are usually readily available and robust. A lower rate of transfusion after transradial PCIs has been reported. Chase et al. [9] and Cantor et al. [10] reported that 1.4 versus 2.8% and 0.9 versus 4.8% of patients needed blood transfusions, radial versus femoral, respectively.
Our data, derived during an unenforced transition from TFA to TRA, show very similar results, with transfusion rates of 0.7% for TRA versus 2.3% for TFA. However, neither transfusion requirements nor the incidence of bleeding were different in the propensity score matched groups.
Length of hospital stay
The current financial environment has focused administrators and physicians minds on cost and savings. Reduced hospital length of stay and reduced financial cost with radial PCIs have been reported previously. Agostoni et al. [5] reported mean hospital stay of 1.8 versus 2.4 days in TRA versus TFA which should translate in lower costs as shown by Roussanov et al. for diagnostic coronary angiography (TRA mean cost $369.5 ± 74.6 vs TFA $446.9 ± 60.2 p <0.001).
Our study demonstrates reduced hospital stay among radial cases even during the switch toward default TRA and it is likely that hospital length of stay has reduced even further as operators have become more experienced with the technique.
Fluoroscopy time
Agostini et al. [5] reported longer fluoroscopy time with TRA than with TFA (8.9 vs 7.8 min, p <0.01). Furthermore, Neil et al. [6] reported longer fluoroscopy time during transition from femoral to default radial access for both diagnostic and interventional cases. However, they also demonstrated a decrease of fluoroscopy time as experience accumulates with TRA. We found similar fluoroscopy times in transradial and transfemoral coronary intervention (11.77 vs 11.18 min, p = NS) during the transition period indicating equivalent efficiency between TRA and TFA during the switch.
Mortality
Although radial access reduces vascular access site complications and need for transfusion, the evidence that radial approach reduces mortality in all PCIs is yet to be provided. One observational study found lower mortality with radial access but with a negligible survival advantage when transfusion requirements were taken into account [9].
A meta-analysis by Agostoni et al. [5] found that radial and femoral approaches yielded similar major cardiac event rates. The RIVAL study [8] showed no statistically significant mortality benefit with the use of the radial approach for the patient population as a whole except in STEMI patients. The RIVAL researchers suggested that a sample size of 17,000 patients would be needed for a randomized study of transradial coronary intervention to demonstrate a survival benefit in all-comers to the catheter laboratory [8].
Our study demonstrated no mortality benefit with TRA. However, it showed no evidence of increased mortality during the transition period from a default TFA to a default TRA PCI.
The disappearance of differences in outcomes after propensity matching is probably related to the relatively small sample size. Moreover, propensity matching excludes patients that are extreme outliers to form more homogenous groups.
Limitations
This is a single-center observational study and our findings cannot be applied to other settings. The data were extrapolated from databases which restricted our baseline variables. Some notable variables such as short- and mid-term radial artery patency, cerebrovascular events and surgical intervention on access site vascular injury or hematomas are not routinely recorded on this database and therefore not included in this study.
There was no information on patients who moved out of region and continued followup in other parts of the country. Also, our center is a tertiary center for seven district general hospitals in South West Wales, a relatively large geographic area. The electronic data linkage among these hospitals is minimal and as a result our data are limited on patients that transferred back to their referring district general hospitals.
Approximately 10% of the cases were not included because they had missing variables. The variables were missing at random suggesting their exclusion did not alter the findings.
Even allowing for all of the above, the results of the study are broadly consistent with the literature which enhances their relevance.
Conclusion
The differences in outcome between TRA and TFA PCI during the introduction of radial access for coronary intervention in a tertiary center are similar. Numerical trends, in patients undergoing TRA PCI, suggested benefits in mortality, rate of bleeding, transfusion requirement and length of hospital stay, which disappeared after propensity score matching. While conclusive randomized control trial data are accumulating, our experience confirms that the transradial approach is at least equivalent to the transfemoral approach in terms of safety and outcomes for percutaneous coronary interventions during the process of transition toward default radial access.
Future perspective
TRA for coronary intervention is becoming the default access globally. Centers that use femoral access as a default are likely to experience pressures to switch over to radial access. Our study paves the way to those following our transition.
Up to 10–20% of patients will still need their procedure performed via the femoral route. Therefore, we should emphasize the need for continued upkeep of skill in femoral access. Transfemoral artery procedures should remain part of training for future cardiac interventionists.
Acknowledgements
We thank O Budger, Swansea University, for his generous help and statistical advice; A Chase and D Smith for their constructive comments; the catheterization lab staff and the cardiophysiology staff for their support; and the pathology lab staff at Morriston hospital for their help with the transfusion data.
Financial and competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Executive summary
Objectives
• Between 2007 and 2009, the radial approach was adopted in our center. We sought to study the impact of the switch from transfemoral approach to trans-radial approach (TRA).
Introduction
• The TRA for percutaneous coronary interventions (PCIs) is now the default in Europe; its uptake is still slow in the USA. Switching to a default TRA for PCIs could be an intricate process.
Methods
• We data mined procedure-related characteristics for all PCIs performed between 2007–2009. Mortality, bleeding, red blood cell transfusion and hospital stay were also assessed.
Results
• We identified 2845 procedures (2084 M [73%], mean age [SD] 63.6 [11] years, range 29–98 years). The radial approach was used in 47% (1346) of procedures, increasing during the study period, from 36 to 58% of procedures (p <0.01 for trend).
• Postprocedural transfusions of red blood cells were required in 66 (2.3%) cases (radial 21 [0.7%], femoral 45 [1.6%] p = 0.007). Hematomas developed in 77 (2.7%) cases (radial 14 [0.5%], femoral 63 [2.2%] p <0.01) with a clear decrease during the study period, from 1.3 to 0.5% (p = 0.002 for trend). There was no difference in fluoroscopy or procedure times between the two groups.
• Age, cardiogenic shock (adjusted odds ratios: 21.36; 95% CI: 6.48–70.38, relative risk 16; 95% CI: 6.5–39) and red blood cell transfusion (adjusted odds ratios: 7.70; 95% CI: 2.30–25.80, relative risk 6.4; 95% CI: 2.5–16) were the only significant determinants of 1-year mortality. Hospital stay was different between the two groups (femoral 2.13 days, radial 1.44 days [p <0.01]).
• We were able to propensity score match 520 cases based on the access (Delta <5%). There was no difference in mortality, need for transfusion, incidence of hematoma or hospital stay between the two groups.
Conclusion
• While further conclusive randomized data are awaited, our experience confirms that the radial approach is at least as safe as the femoral approach during the transition toward default radial access.
References
- De Luca G, Schaffer A, Wirianta J, Suryapranata H. Comprehensive meta-analysis of radial vs femoral approach in primary angioplasty for STEMI. Int. J. Cardiol. 168(3), 2070–2081 (2013).
- Muthusamy P, Busman DK, Davis AT, Wohns DH. Assessment of clinical outcomes related to early discharge after elective percutaneous coronary intervention: COED PCI. Catheter Cardiovasc. Interv. 81(1), 6–13 (2013).
- Mehran R, Rao SV, Bhatt DL et al. Standardized bleeding definitions for cardiovascular clinical trials. Circulation 123(23), 2736–2747 (2011).
- Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav. Res. 46(3), 399–424 (2011).
- Agostoni P, Biondi-Zoccai GG, de Benedictis ML et al. Radial versus femoral approach for percutaneous coronarydiagnostic and interventional procedures: systematicoverview and meta-analysis of randomized trials. J. Am. Coll. Cardiol. 44(2), 349–356 (2004).
- Neill J, Douglas H, Richardson G et al. Comparison ofradiation dose and the effect of operator experience infemoral and radial arterial access for coronary procedures Am. J. Cardiol. 106(7), 936–940 (2010).
- Rao SV, Ou FS, Wang TY et al. Trends in the prevalence and outcomes of radial and femoral approaches to percutaneous coronary intervention: a report from the National Cardiovascular Data Registry. JACC Cardiovasc. Interv. 1(4), 379–386 (2008).
- Jolly SS, Yusuf S, Cairns J et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet 377(9775), 1409–1420 (2011).
- Chase AJ, Fretz EB, Warburton WP et al. Association of the arterial access site at angioplasty with transfusion and mortality: the M.O.R.T.A.L study (Mortality benefit Of Reduced Transfusion after percutaneous coronary intervention via the Arm or Leg). Heart 94(8), 1019–1025 (2008).
- Cantor WJ, Mahaffey KW, Huang Z et al. Bleeding complications in patients with acute coronary syndrome undergoing early invasive management can be reduced with radial access, smaller sheath sizes, and timely sheath removal. Catheter Cardiovasc. Interv. 69(1), 73–83 (2007).