Research Article - Interventional Cardiology (2024)
Cardiac arrest outcome in septic shock: A national emergency department database study (2016-2018)
- Corresponding Author:
- Tanveer Mir
Department of Internal Medicine, Baptist Medical Center, Alabama, USA,
E-mail: Gr6723@wayne.edu
Received date: 02-Sep-2024, Manuscript No. FMIC-24-147092; Editor assigned: 05-Sep-2024, PreQC No. FMIC-24-147092 (PQ); Reviewed date: 19-Sep-2024, QC No. FMIC-24-147092; Revised date: 26-Sep-2024, Manuscript No. FMIC-24-147092 (R); Published date: 03-Octg-2024, DOI: 10.37532/1755-5310.2024. 16(S24).625
Abstract
Objective: To study the predictors and morality of cardiac arrest patients presenting to the emergency department who had septic shock.
Background: Literature regarding outcomes of cardiac arrest in patients with septic shock is limited.
Methods: Data from the National Emergency Department Sample (NEDS) that constitutes 20% sample of hospital-owned emergency departments in the United States was analyzed for the septic shock related visits from 2016-2018. Septic shock was defined by the ICD codes.
Results: Out of 1,375,507 adult septic shock patients (mean age 67.09 ± 15.6 years, 48.8% females), cardiac arrest occurred in 112,598 (8.2%) of the patients. Among cardiac arrest patients, 82,595 (73.4%) died till discharge. In multivariable-adjusted logistic regression age >65 years (OR=2.2), prior percutaneous coronary intervention (OR 1.2), prior-coronary artery bypass graft (OR=1.26) and peripheral vascular disease (OR=1.3) were associated with mortality and coronary interventions (OR=0.3), shockable rhythm R=0.8), congestive heart failure (OR=0.6) were not associated with mortality (p<0.001). The results were consistent after propensity matching. However, the trend for coronary interventions was steady over study years. Cardiac arrest patients had a longer hospital stay and cardiac arrhythmias had a significant association with longer hospital stay. Cardiac arrest prevalence and survival trends were steady over the study years, 2016-2018.
Conclusion: Cardiac arrest complicated septic shock significantly with high mortality. Coronary interventions were associated with improved survival rates. More research is needed to improve mortality associated with cardiac arrest in patients with septic shock.
Keywords
Cardiac arrest • Septic shock • Survival • Outcomes • National emergency database sample
Introduction
The yearly burden of sepsis on the United States health care system is high with 1.7 million hospitalizations yearly [1]. High proportion of such patients have a septic shock with significant mortality rates. The mortality rates from sepsis have been reported as high as 16%-25% [2,3]. Septic shock defined as hypotension with organ dysfunction secondary to sepsis is associated with higher rates of cardiac arrest and hence mortality. Despite the improvement in the health care system over the last decade the mortality from septic shock are high with rates up to 40% [4]. Survival rates from in-hospital cardiac arrest are low with reported rates of up to 25% [5]. Severe sepsis has a very strong negative association with survival from cardiac arrest [6].
Sepsis as a predictor of cardiac arrest has been evaluated by multiple studies evaluating the in-hospital cardiac arrest [6-8]. Limited data is available regarding the mortality outcomes in patients with sepsis [2,9]. However, to our knowledge, no previous studies are available which has evaluated mortality predictors for cardiac arrest in septic shock patients.
Data regarding the trend, outcomes and predictors of cardiac arrest in patients with septic shock could provide information for improving health care and policymaking for these patients. Currently, very limited knowledge is available regarding cardiac arrest outcomes in patients with septic shock. Therefore, we aimed to examine the national trend, predictorsand mortality outcomes of septic shock patients who had cardiac arrest for the years 2016- 2018 in the national emergency department sample database.
Materials and Methods
Study population and design
An observational cohort study of patients that had septic shock and had a cardiac arrest during the years 2016-2018 in the National Emergency Department Sample (NEDS) database was performed. The National Emergency Department Sample constitutes an approximately 20% sample of hospital-owned emergency departments in the United States [10]. Using a stratified, random sampling design, a sample of hospital-owned emergency departments from the United States participating in both the State Inpatient Databases (SID) and the State Emergency Department Databases (SEDD) was selectedand 100% of the emergency departments visits from the selected hospital-owned emergency departments were retained. Hospitals were included in the NEDS based on geographic region (northeast, mid-west, west, or south), location (urban or rural), teaching status (teaching or non-teaching), ownership (public, private not-for-profit, private for-profit) and Trauma Center Designation. A total of 950 emergency departments are included in NEDS. From each selected emergency departments, all visits were included, which amounted to more than 33 million unweighted visits each year. Patients with age <18 years were excluded at the time of data extraction from the National Emergency Department Sample database. The study was exempt from institutional review board evaluation however it was performed according to the ethical criteria set up by Healthcare Cost and Utilization Project (HCUP) [10].
Study definitions
Septic shock was defined with the International Classification of Diseases, Tenth edition, (ICD-10) code “R65.21”. We identified 1,375,507 adult septic shock patients which included 112,598 cardiac arrests with a national estimate of 8.2%. We generated cardiac arrest using ICD-10 codes I46.2, I46.8, I46.9, I971.21, I977.11, O291.11, O291.12, O291.19, O04.86and O07.36.
Patient and hospital characteristics
Baseline patient demographic characteristics (age, sexand insurance payer) were extracted. Diagnostic codes were used to identify hypertension, diabetes mellitus, obesity, congestive heart failure, cerebrovascular disease, Peripheral Vascular Disease (PVD), Chronic Obstructive Pulmonary Disease (COPD), malignancy, renal failure, liver dysfunction, atrial fibrillation, prior history of stroke, hyperlipidemia, smoking, prior percutaneous coronary intervention, prior coronary artery bypass grafting, cardiogenic shock, using ICD 10 codes. Elixhauser comorbidity index codes were also used to generate the comorbidities [11]. Coronary interventions were defined by ICD-10 Procedural Classification System (PCS) codes and Current Procedure Terminology codes (CPT). The interventions included coronary angiography, percutaneous coronary interventionand coronary artery bypass grafting.
Outcomes
The primary outcome of our study was mortality from cardiac arrest in patients with septic shock. Other outcomes calculated were predictors for mortality in patients who had cardiac arrest.
Statistical methods
Categorical variables were expressed as weighted values along with percentages and continuous variables were expressed as mean ± standard deviation if the variable was not skewed and as median with 25th and 75th percentiles. Descriptive statistics were performed for demographics and comorbidities which were stratified by cardiac arrest and without cardiac arrest septic shock. We used survey procedure “svy” to calculate Pearson’s chi-square test for categorical variables and t-test for the continuous variables. A propensity matching was done using “Coarsened Exact Matching in Stata” for the comorbidities and there was a significant effect from any of the variables [12]. We then computed the Odds Ratio (OR) with 95% Confidence Interval (CI) for the association with mortality from cardiac arrest in multivariable-adjusted logistic regression model 1 adjusted for age 40-50 years, age 51-65 years, age >65 years, hyperkalemia, hypertension, diabetes mellitus, hyperlipidemia, obesity, liver dysfunction, prior-percutaneous coronary intervention, stroke history, sex, coagulopathy, smoking, congestive heart failure, hypothyroidism, Peripheral Vascular Disease (PVD), Chronic Obstructive Pulmonary Disease (COPD), malignancy, renal failure, atrial fibrillation, ventricular tachycardia/fibrillation, coronary interventionsand insurance status. Subgroup analyses of mortality was performed for patients in whom coronary interventions were performed. The proportions were compared using the Chi-square test.
We then computed the Incidence Rate Ratios (IRR) with 95% Confidence Interval (CI) for length of hospital stay in a multivariable-adjusted poison regression model 1 adjusted for age 40-50 years, age 51-65 years, age >65 years, hyperkalemia, hypertension, diabetes mellitus, hyperlipidemia, obesity, liver dysfunction, prior-percutaneous coronary intervention, stroke history, gender, coagulopathy, smoking, congestive heart failure, hypothyroidism, Peripheral Vascular Disease (PVD), Chronic Obstructive Pulmonary Disease (COPD), cardiogenic shock, renal failure, atrial fibrillation, ventricular tachycardia/fibrillation, coronary interventionsand insurance status.
We also evaluated yearly trends in mortality as well as the number of cardiac arrests diagnosed among septic shock patients. Coronary intervention yearly trend was calculated over the study years, 2016- 2018. The significance for trends was reported as a linear trend p-value. All analyses were weighted analyses. Statistical analysis was performed using STATA version 16.1 (College Station, Texas). All p values were 2 sided, with a significance threshold of p<0.05.
Results
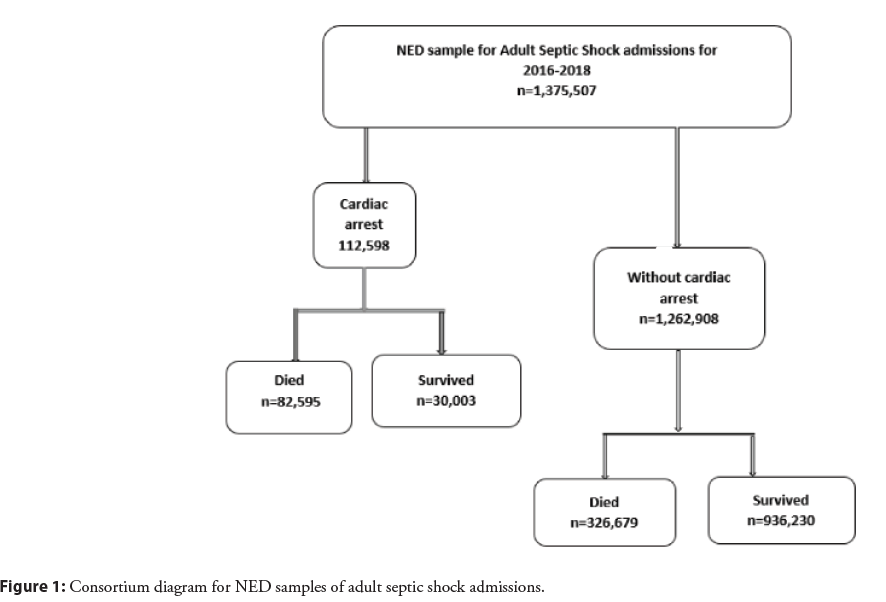
A total of 1,375,507 adult septic shock (mean age 67.09 ± 15.6 years, 48.8% females) patients were included in this analysis from the national emergency database for the years 2016-2018. Cardiac arrest occurred in 112,598 (8.2%) (Figure 1). Baseline characteristics of the patients with a diagnosis of septic shock with and without cardiac arrest are given in Table 1. Cardiac arrest patients had higher prevalence of diabetes, hypertension, renal failure, liver diseases, peripheral vascular disease, congestive heart failure, hyperkalemia, cardiogenic shock on presentation and patients without cardiac arrest had higher prevalence of chronic obstructive pulmonary disease, hypothyroidismand obesity. STEMI was diagnosed in 17,959 (15.9%) patients and NSTEMI was diagnosed in 12,436 (11%) patients among cardiac arrest patients.
| Cardiac Arrest | |||
|---|---|---|---|
| Variables | Present | Absent | p-value |
| (n=112,598) | (n=1,262,908) | ||
| Age (Mean) | 71.02 ± 13.54 | 66.67 ± 15.71 | |
| Age 40-50years | 14,040 (12.5%) | 148,002 (11.7%) | 0.0008 |
| Age 51-65 years | 54,702 (48.6%) | 583,708 (46.2%) | <0.001 |
| Age >65 years | 33,929 (30.1%) | 421,654 (33.4%) | <0.001 |
| Female | 51,300 (45.6 %) | 614,009 (48.6%) | <0.001 |
| Primary payor | |||
| Medicare | 72,949 (64.9%) | 845,206 (67%) | <0.001 |
| Medicaid | 16,298 (14.5%) | 167,133 (13.2%) | <0.001 |
| Private Insurance | 15,816 (14.1%) | 186,229 (14.8%) | <0.001 |
| Self-payment | 4,791 (4.26%) | 35,574 (2.82%) | <0.001 |
| Hypertension | 72,761 (64.6%) | 806,656 (63.9%) | <0.001 |
| Diabetes | 43,494 (38.6%) | 457,514 (36.2%) | <0.001 |
| Stroke history | 8,340 (7.41%) | 99,956 (7.91%) | 0.006 |
| Prior MI | 6,138 (5.45%) | 71,241 (5.64%) | 0.22 |
| Prior CABG | 5,292 (4.7%) | 59,449 (4.71%) | 0.95 |
| Smoker | 15,087 (13.4%) | 170,630 (13.5%) | 0.65 |
| Obesity | 15,573 (13.8%) | 188,245 (14.9%) | <0.001 |
| COPD | 31,292 (27.8 %) | 368,394 (29.2%) | <0.001 |
| Liver disease | 29,819 (26.5%) | 212,384 (16.8%) | <0.001 |
| Atrial fibrillation | 16,115 (14.3%) | 205,928 (16.3%) | <0.001 |
| VtVf | 18,117 (16.1%) | 48,217 (3.82%) | <0.001 |
| Cardiac shock | 7,977 (7.08%) | 44,318 (3.51%) | <0.001 |
| Congestive heart failure | 43,724 (38.8%) | 433,589 (34.3 %) | <0.001 |
| Hyperlipidemia | 28,545 (25.4 %) | 361,543 (28.6%) | <0.001 |
| Peripheral vascular disorders | 13,230 (11.7 %) | 138,971 (11%) | <0.001 |
| Hypothyroidism | 12,544 (11.1%) | 193,337 (15.3%) | <0.001 |
| Renal failure | 39,089 (34.7%) | 390,562 (30.9%) | <0.001 |
| Prior PCI | 4,553 (4.04 %) | 55,346 (4.38%) | 0.01 |
| Coagulopathy | 33,399 (29.7%) | 319,575 (25.3%) | <0.001 |
| Fluid and electrolyte disorders | 89,906 (78.9%) | 955,761 (75.7%) | <0.001 |
| Hyperkalemia | 24,150 (21.4%) | 178,402 (14.1%) | <0.001 |
| Hospice | 26,677 (23.7%) | 231,567 (18.3%) | <0.001 |
| DNR | 43,735 (38.8 %) | 360,458 (28.5%) | <0.001 |
Abbreviations: VtVf: Ventricular tachycardia and Ventricular fibrillation; Prior MI: Prior Myocardial Infarction; COPD: Chronic Obstructive Pulmonary Disease; DNR: Do Not Resuscitate.
Table 1: Baseline characteristics of cardiac arrest and without cardiac arrest septic shock patient population.
Figure 1: Consortium diagram for NED samples of adult septic shock admissions.
Cardiac interventions
Coronary angiography was performed in a small proportion of cardiac arrest patients (n=4,756, 4.2%). Out of these, percutaneous coronary interventions were performed in 963 (3.21%) of patients who survived and 703 (0.8%) who died among cardiac arrest patients. Drug eluting stent was used in 819 (2.73%) of patients who survived and 545 (0.6%) who died from cardiac arrest. Bare metal stent was used in 135 (0.5%) patients of cardiac arrest who survived and 143 (0.17%) of patients of cardiac arrest who did not survive. Coronary artery bypass grafting was done in 153 (0.5%) of cardiac arrest patient who survived and 82 (0.1%) of cardiac arrest patients who died. In multivariable logistic regression model adjusted for model M1 cardiac intervention was less associated with mortality (OR=0.31, 95% CI 0.27, 0.35) among cardiac arrest patients.
Mortality from cardiac arrest
Out of 112,598 patients who had cardiac arrest (82,595,73.4%) of patients died till discharge. Among the patients discharged alive, majority were discharged to skilled nursing homes (18,873,63%). The mortality rates among cardiac arrest patients who had coronary interventions were better (2,249,43.7%) than cardiac arrest patients who did not have cardiac intervention (80,347,74.8%). Significant number of cardiac arrest patients were evaluated by palliative care (26,677,23.7%) and a do-not-resuscitate code status was assigned to (43,735,38.8%) of the cardiac arrest patients.
Cardiac interventions
Coronary angiography was performed in a small proportion of cardiac arrest patients (n=4,756, 4.2%). Out of these, percutaneous coronary interventions were performed in 963 (3.21%) of patients who survived and 703 (0.8%) who died among cardiac arrest patients. Drug eluting stent was used in 819 (2.73%) of patients who survived and 545 (0.6%) who died from cardiac arrest. Bare metal stent was used in 135 (0.5%) patients of cardiac arrest who survived and 143 (0.17%) of patients of cardiac arrest who did not survive. Coronary artery bypass grafting was done in 153 (0.5%) of cardiac arrest patient who survived and 82 (0.1%) of cardiac arrest patients who died. In multivariable logistic regression model adjusted for model M1 cardiac intervention was less associated with mortality (OR=0.31, 95% CI 0.27, 0.35) among cardiac arrest patients.
Mortality from cardiac arrest
Out of 112,598 patients who had cardiac arrest (82,595,73.4%) of patients died till discharge. Among the patients discharged alive, majority were discharged to skilled nursing homes (18,873,63%). The mortality rates among cardiac arrest patients who had coronary interventions were better (2,249,43.7%) than cardiac arrest patients who did not have cardiac intervention (80,347,74.8%). Significant number of cardiac arrest patients were evaluated by palliative care (26,677,23.7%) and a do-not-resuscitate code status was assigned to (43,735,38.8%) of the cardiac arrest patients.
Predictors for cardiac arrest and propensity analysis
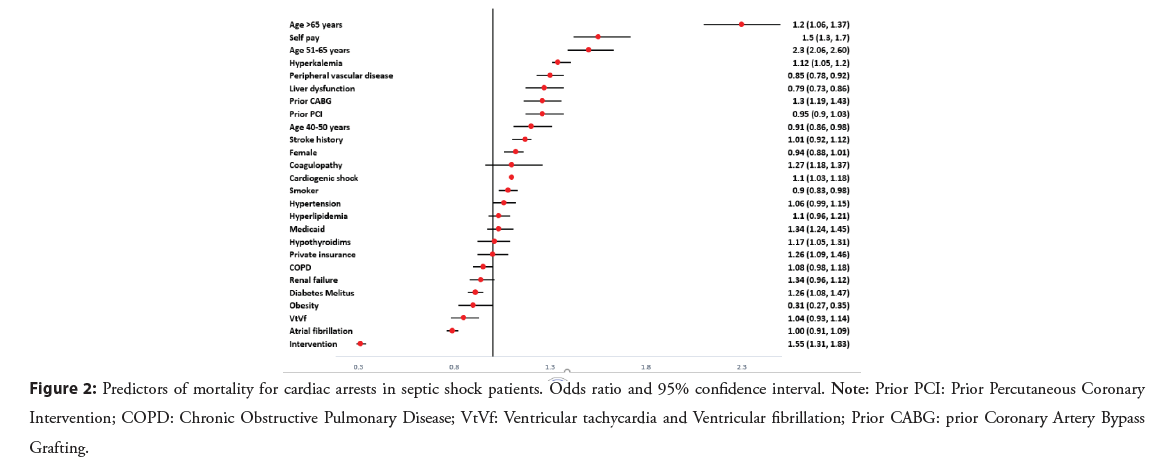
In multivariable-adjusted logistic regression model 1 elderly age, female gender, peripheral vascular disease, liver dysfunction, history of stroke, prior coronary artery bypass grafting, prior percutaneous coronary intervention was associated with mortality and atrial fibrillation, ventricular tachycardias/fibrillation, congestive heart failure, obesity was not associated with mortality (Figure 2). Coronary interventions including PCI, coronary artery bypass graftingand coronary angiography were strong predictors of survival (OR=0.3, p<0.001). Propensity matching analysis was done to balance the baseline characteristics for any confounding effects. There was no confounding effect from any of the variables (Table S1).
Figure 2: Predictors of mortality for cardiac arrests in septic shock patients. Odds ratio and 95% confidence interval. Note: Prior PCI: Prior Percutaneous Coronary Intervention; COPD: Chronic Obstructive Pulmonary Disease; VtVf: Ventricular tachycardia and Ventricular fibrillation; Prior CABG: prior Coronary Artery Bypass Grafting.
Trend of cardiac arrest and mortality from cardiac arrest
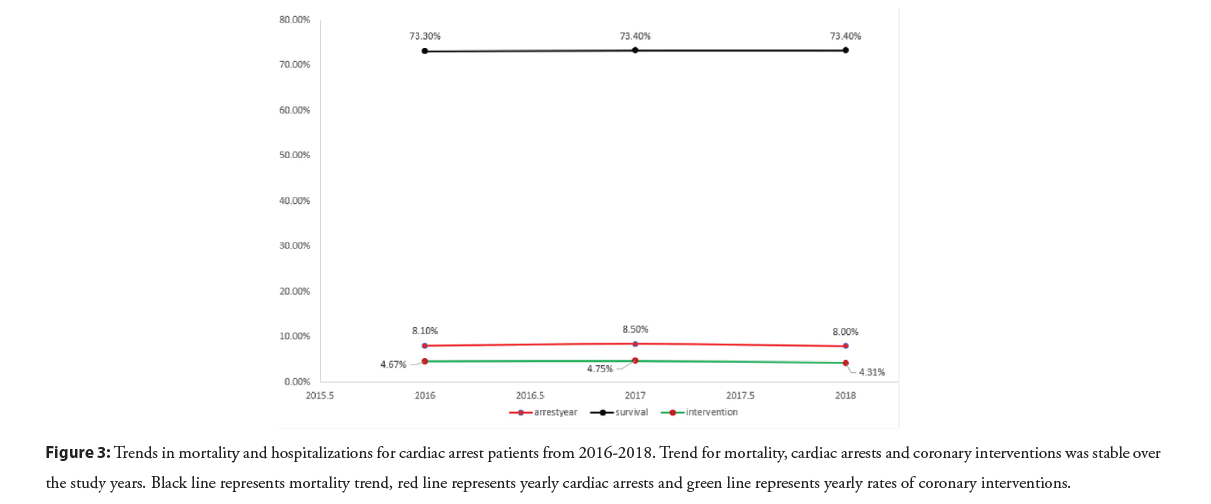
The mortality trend from cardiac arrest in septic shock was steady over the study years, 2016-2018 (linear p trend 0.3). The trend for cardiac arrest from septic shock was stable over the study years (linear p trend 0.8). The proportion of patients that underwent coronary interventions remained steady over the study years (linear p trend 0.4) (Figure 3).
Figure 3: Trends in mortality and hospitalizations for cardiac arrest patients from 2016-2018. Trend for mortality, cardiac arrests and coronary interventions was stable over the study years. Black line represents mortality trend, red line represents yearly cardiac arrests and green line represents yearly rates of coronary interventions.
Length of stay and predictors for the length of stay
Patients who were discharged alive post-cardiac arrest was higher than patients without cardiac arrest among septic shock patients. Among the predictors ventricular tachycardia/fibrillation (IRR=2.4, p<0.001), congestive heart failure (IRR=1.59, p<0.001), coagulopathy (IRR=1.59, p<0.001), coronary interventions (IRR=2.2, p<0.001) were associated with prolonged hospital stay and prior CABG (IRR=0.64, p<0.001), prior PCI (IRR=0.7, p=0.01), female gender (IRR=0.8, p=0.002) were less likely associated with length of hospital stay (Figure S1).
Discussion
This is the first study to evaluate the outcome of cardiac arrest in septic shock patients. One in every 12 patients admitted to the emergency department with septic shock had a cardiac arrest. Patients who had cardiac arrest were younger and predominantly males compared to septic shock patients without cardiac arrest. The mortality rate in patients with cardiac arrest was 73.4%. More interventions were done in patients with cardiac arrest than the septic shock patient who did not have a cardiac arrest. Coronary interventions were strongly associated with survival outcomes among cardiac arrest patients. Prior coronary intervention history was strongly associated with mortality from cardiac arrest. The cardiac arrest trend was steady over the study years. The mortality trend and coronary intervention rates in patients with cardiac arrest was steady over the study years, which is concerning. The majority of alive discharge disposition was to skilled nursing. A significant number of patients went to hospice or had a code status of do-not-resuscitate post-cardiac arrest.
Survival outcomes from cardiac arrest are very poor. A study from the national emergency database for the years 2006-2014 has reported a mortality rate of 71.3% [13]. A study from The Guidelines (GWTG)-Resuscitation registry on 48,841 cardiac arrest patients, for the years 2007-2010, a mortality rate of 78.8% was reported [6]. We observed a mortality rate of 73.4% in patients of cardiac arrest among the septic shock patient population. The overall mortality rate in the septic shock patients was 29.8%, which is better than the previously reported rate of 40% [4]. Interestingly, the mortality rates among the cardiac arrest with septic shock patients improved to 43.7% with coronary interventions including percutaneous coronary intervention, coronary angiographyand coronary artery bypass grafting. The significant survival benefits secondary to coronary interventions seen in the cardiac arrest patient population is a novel finding of our study. We observed the rates of coronary interventions trend was steady over the study years. This would suggest improvement in rates of coronary interventions for better survival outcomes.
Prior history of coronary artery interventions was a strong predictor for cardiac arrest mortality in patients with septic shock.
Peripheral arterial disease, a coronary artery disease equivalent, was associated with cardiac arrest mortality in patients with septic shock. Since septic shock is a hypercoagulable state, it might precipitate acute myocardial infarction in patients who had prior coronary interventions [14]. Patients with septic shock may have acute cardiac ischemia which may be over looked due to septic shock. The hyperadrenergic state could be the reason for worsening myocardial ischemia and mortality associated with cardiac arrest in this patient group. Hyperadrenergic state has been reported to cause sudden death in patients with prior history of myocardial infarction [15]. This would suggest more research to identify myocardial ischemia in patients with prior history of coronary intervention, possibly with ultrasound for regional wall motion abnormalities or troponin trends.
Interestingly, we observed less association of ventricular tachycardia/fibrillation and atrial fibrillation with mortality from cardiac arrest in patients with septic shock, likely secondary to being shockable rhythm. In contrary, previous studies had reported more association of morality with ventricular arrhythmias in patients with severe sepsis [9].
There was a significant difference in length of stay among alive patients. Cardiac arrest patients had higher length of hospital stay than patients without cardiac arrest. Cardiac arrhythmias, younger ageand heart failure had a significant association with prolonged length of hospital stay. A significant number of patients had a disposition to skilled nursing care.
Our study has several implications. Firstly, one in every 12 patients with septic shock develops cardiac arrest and only 1 in every 4 cardiac arrest patients survive. The high mortality rates in such patients were modifiable with coronary interventions. The mortality benefits would suggest improvement in rates of coronary interventions in such high-risk patients. Secondly, a higher association of mortality from cardiac arrest in septic shock patients with prior history of myocardial infarction would suggest better screening procedures to identify any possible myocardial infarction in these critically ill patients. Thirdly, despite the improvements in health care set up, the mortality trend in cardiac arrest patients remained stable over the study years, 2016-2018. This would suggest more research to better understand the cardiac arrest and hence improve survival.
Our study has several limitations. First, this is a retrospective, observational studyand inference regarding causation should be made with caution. Also, we relied on reported ICD-10 codes to identify diagnoses to perform our analysis. The national emergency database is an administrative database that could be subject to inaccurate coding and underreporting of comorbid diagnoses. There is also an absence of important information related to patients’ physical examination, medicationsand laboratory results. We could not do a subgroup analysis based on delays in resuscitation, time to cardiovascular interventionsand duration of cardiopulmonary resuscitation, medications which has a direct relation with outcomes of cardiac arrest. However, NEDS and the codes used in this study have been applied in multiple clinical studies and can be considered a highly reliable databaseand giving the large cohort analyzed this minimizes the study limitation.
Conclusion
Patients with septic shock had a high prevalence rate of 8.2%. The mortality rates among the septic shock patients who had cardiac arrest were high, 73.4%. Coronary interventions had a significant survival benefits among patients who had a cardiac arrest. However, the rates of coronary interventions were steady over the study years which suggest improvement of the rates of interventions. Prior history of myocardial infarction had a strong association with cardiac arrest mortality and hence suggests more research into screening methods for myocardial ischemia in the critically ill septic shock patients.
References
- Rhee C, Dantes R, Epstein L, et al. Incidence and trends of sepsis in US hospitals using clinical vs. claims data, 2009-2014. JAMA. 318:1241-1249 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Moskowitz A, Omar Y, Chase M, et al. Reasons for death in patients with sepsis and septic shock. J Crit Care. 38:284-288 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Knoop ST, Skrede S, Langeland N, et al. Epidemiology and impact on all-cause mortality of sepsis in Norwegian hospitals: a national retrospective study. PLoS One. 12:e0187990 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Vincent J-L, Jones G, David S, et al. Frequency and mortality of septic shock in Europe and North America: A systematic review and meta-analysis. Crit Care. 23(1):196 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Andersen LW, Holmberg MJ, Berg KM, et al. In-hospital cardiac arrest: A review. JAMA. 321:1200-1210 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Chan PS, Berg RA, Spertus JA, et al. Risk-standardizing survival for in-hospital cardiac arrest to facilitate hospital comparisons. J Am Coll Cardiol. 62:601-609 (2013).
[CrossRef] [Google Scholar] [PubMed]
- Nadkarni VM, Larkin GL, Peberdy MA, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 295:50-57 (2006).
- Larkin GL, Copes WS, Nathanson BH, et al. Pre-resuscitation factors associated with mortality in 49,130 cases of in-hospital cardiac arrest: A report from the national registry for cardiopulmonary resuscitation. Resuscitation. 81:302-311 (2010).
[CrossRef] [Google Scholar] [PubMed]
- Shahreyar M, Fahhoum R, Akinseye O, et al. Severe sepsis and cardiac arrhythmias. Ann Transl Med. 6:6 (2018).
[CrossRef] [Google Scholar] [PubMed]
- Agency for Healthcare Research and Quality. 2014 introduction to the NEDS. Healthcare Cost and Utilization Project (HCUP). (2019).
- Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 8-27 (1998).
[CrossRef] [Google Scholar] [PubMed]
- Blackwell M, Iacus S, King G et al. Cem: Coarsened exact matching in Stata. The Stata Journal. 9:524-546 (2009).
- Ravindran R, Kwok CS, Wong CW, et al. Cardiac arrest and related mortality in emergency departments in the United States: Analysis of the nationwide emergency department sample. Resuscitation. 157:166-173 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Gonano C, Sitzwohl C, Meitner E, et al. Four-day antithrombin therapy does not seem to attenuate hypercoagulability in patients suffering from sepsis. Crit Care. 10:R160 (2006).
[CrossRef] [Google Scholar] [PubMed]
- Schwartz PJ, Motolese M, Pollavini G, et al. Prevention of sudden cardiac death after a first myocardial infarction by pharmacologic or surgical antiadrenergic interventions. J Cardiovasc Electrophysiol. 3:2-16 (1992).