Research Article - Diabetes Management (2022) Volume 12, Issue 2
Association of diabetes and crestal bone loss in dental implant placement
- Corresponding Author:
- Subhasree R
Department of Implantology,
Saveetha Dental College and Hospitals,
Saveetha Institute of Medical and Technical Sciences,
Saveetha University,
Chennai,
India
E-mail: Subhashreer.sdc@saveetha.com
Received: 01-Feb-2022, Manuscript No. FMDM-22-47105; Editor assigned: 03-Feb-2022, PreQC No. FMDM-22-47105 (PQ); Reviewed: 17-Feb-2022, QC No. FMDM-22-45585; Revised: 21-Feb-2022, Manuscript No. FMDM-22-47105 (R); Published: 28-Feb-2022, DOI: 10.37532/1758-1907.2022.12(2).307-312
Abstract
Aim: This study aimed to determine the association of diabetes and crestal bone loss in dental implant placement.
Background: Diabetes mellitus is a critical disease from the standpoint of dental implant therapy. It is well-known that chronic hyperglycemic state impairs periodontal structure and functions, which may directly impact the integrity of the periodontium and hence the placement of the dental implant.
Methods: A total of 155 patients were subjected to dental implant placement between April 2020 to March 2021. The data was collected from the patient management system. The data was collected, and the analysis was done using SPSS by IBM version 23.
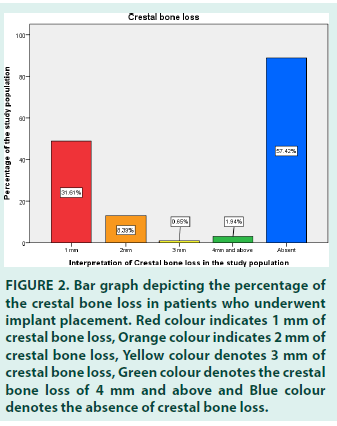
Results: Out of the 155 patients who underwent implant placement, 57.42% of the patients did not have any crestal bone loss, 31.61% of the patients had a crestal bone loss of 1 mm, 8.39% of them had about 2 mm crestal bone loss, 1.94% of them had crestal bone loss of 4 mm and above, and 0.65% of them had 3 mm crestal bone loss. Out of 155 patients, 98.1% patients have no history of diabetes.
Conclusion: Out of the patients who had crestal bone loss, the highest prevalent cresta bone loss was 1 mm. Diabetes was not associated with significant crestal bone loss.
Keywords
diabetes; implant placement; crestal bone loss; osteoclastic activity; bone density; innovation
Introduction
Diabetes mellitus, a chronic illness, was once thought to be a contraindication to dental implant therapy. It has been linked to several comorbidities, including increased susceptibility to infection, slowed wound healing, and oral abscess [1]. Diabetes mellitus, as previously stated, is a metabolic condition that affects the body’s glucose processing. Type 2 diabetes mellitus is a disease in which the body’s insulin levels are insufficient to provide energy to living cells, and it affects nearly every region of the body [2].
Condition defined by chronic hyperglycemia, which causes cells to not absorb glucose due to insulin dysfunction [3].
When it comes to dental implant placement, diabetes is the most deadly disease. This is especially true for people with poorly controlled diabetes, as diabetic patients with well-controlled diabetes have fewer problems [4]. Type 2 diabetes appears to alter the structure and function of collagen, which could directly impact periodontal tissue integrity [5]. Collagen and extracellular matrix formation, maturation, and maintenance are all harmed by chronic hyperglycemia [6]. In hyperglycemia, numerous proteins and matrix components undergo nonenzymatic glycosylation, resulting in accumulating glycation end-products (AGEs). The formation of AGEs occurs at normal glucose levels as well, but in hyperglycemic environments, AGE formation is excessive [7-9].
Factors influencing successful implant therapy for patients with type 2 diabetes mellitus remain unclear, particularly due to limited information available on the influence of glycemic control on implant success [10]. Although the clinical and radiological results of submerged and non- submerged dental implants in non-diabetic patients have been comprehensively explored, evidence on peri-implant outcomes in well- controlled and poorly-controlled type 2 diabetes mellitus is scarce and contentious [11].
In people who have diabetes under control, a dental implant and diabetes may not be a bad combination for a better outcome. Dental implants may be a viable option for replacing missing teeth in diabetic patients with a well-controlled glycemic index. Patients with uncontrolled diabetes may have trouble undergoing implant surgery and have a higher risk of infection following the procedure. It is widely recognized that diabetic patients are more likely than non-diabetic patients to suffer difficulties following implant surgery; consequently, a limited and conservative surgical treatment is recommended. Recent findings show that dental implants may also be successfully placed in poorly controlled diabetic patients with similar success rates as seen in well-controlled diabetic individuals. The study aimed to determine the association between diabetes and crestal bone loss in dental implant placement. Our team has extensive knowledge and research experience that has translated into high-quality publications.
Methodology
It is a single centered retrospective study conducted at Saveetha dental college and hospitals, Chennai. A total of 155 patients who underwent implant placement, predominantly South Indians, were included in the study. Ethical clearance was obtained from the scientific review board. The study was conducted from April 2020 to March 2021. Validation of the study was done by undergraduates, postgraduates and all faculty members of Saveetha dental college.
Data collection was done by using patient management software which has all patients’ records. It is a recording system of all patients of all data related to patients’ medical and dental history and treatment done in Saveetha dental college. The collected data were tabulated under the following parameters-name, age, gender, site, history of diabetes and crestal bone loss. The main variables include the history of diabetes and crestal bone loss.
The data analysis was performed using SPSS software (version 23). The chi-square test and Pearson correlation were done. The chi-square test was used to compare the data and checked for the distributions at 0.05 level of significance for the effect of statistical significance.
Results and Discussion
The data collected from the digital archives was tabulated, imported to SPSS, and descriptive statistics were performed. Out of 155 patients, 60.65% of the study population ranged from 31 to 50 years, 20% of them was from the age group of 18 to 30 years and 19.35% of them were above 50 years. Of the study population, 69.03% of the patients were males, and 30.97% were females.
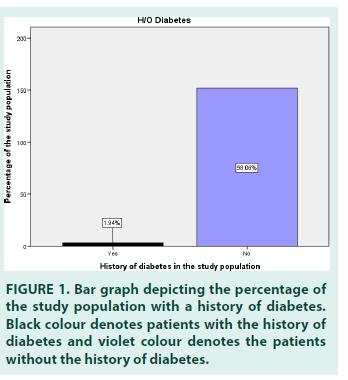
The site of the implant placement was categorized into four groups, namely, Quadrant 1, Quadrant 2, Quadrant 3 and Quadrant 4. 33.55% of the patients had the implant placement in Quadrant 4, 32.26% in Quadrant 3, 19.35% in Quadrant 2 and 14.84% in Quadrant 1. 98.06% of the 155 patients who had implants placed had no history of diabetes, whereas 1.94% had a history of diabetes (FIGURE 1). Out of the patients who underwent implant placement, 57.42% of the patients did not have any crestal bone loss, 31.61% of the patients had a crestal bone loss of 1 mm, 8.39% of them had about 2 mm crestal bone loss, 1.94% of them had crestal bone loss of 4 mm and above, and 0.65% of them had 3 mm crestal bone loss (FIGURE 2).
Figure 2: Bar graph depicting the percentage of the crestal bone loss in patients who underwent implant placement. Red colour indicates 1 mm of crestal bone loss, Orange colour indicates 2 mm of crestal bone loss, Yellow colour denotes 3 mm of crestal bone loss, Green colour denotes the crestal bone loss of 4 mm and above and Blue colour denotes the absence of crestal bone loss.
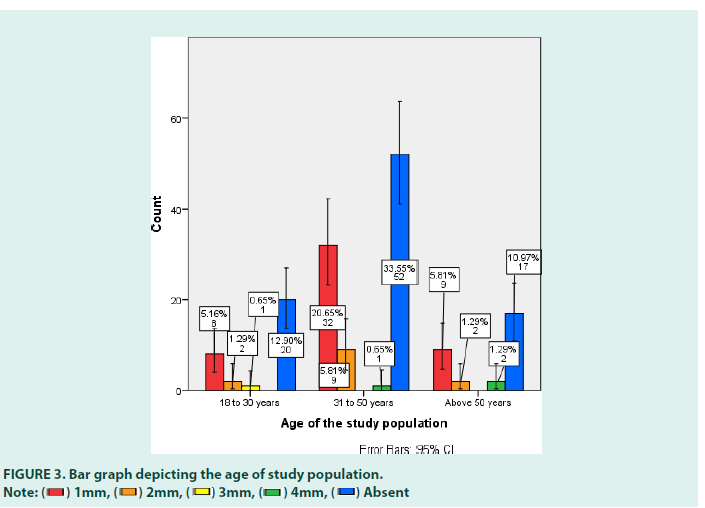
The crosstabs were done between the age and the crestal bone loss. 42.66% of patients belonged to the age group of 31 to 50 yrs, out of which 33.55% of them did not have any crestal bone loss, 20.65% of them had a crestal bone loss of 1 mm, 5.81% of them had a crestal bone loss of 2 mm and 0.65% of them had a crestal bone loss of 4 mm and above. 20.6% of the patients belonged to the age group of 18 to 30 yrs, out of which 12.90% of them did not have crestal bone loss, 5.16% had 1 mm, 1.29% had 2 mm, and 0.65% had 3 mm crestal bone loss. 19.36% of the patients were above 50 yrs, out of which 10.97% did not have crestal bone loss, 5.81% had 1 mm, 1.29% had 2 mm and 3 mm of crestal bone loss each (FIGURE 3). The p-value was 0.000, which is statistically significant. A study by Sanjan Devi states that crestal bone loss increases due to the systemic complications that increase with age. The more the number of medical complications, the more is crestal bone loss and slows the healing rate.
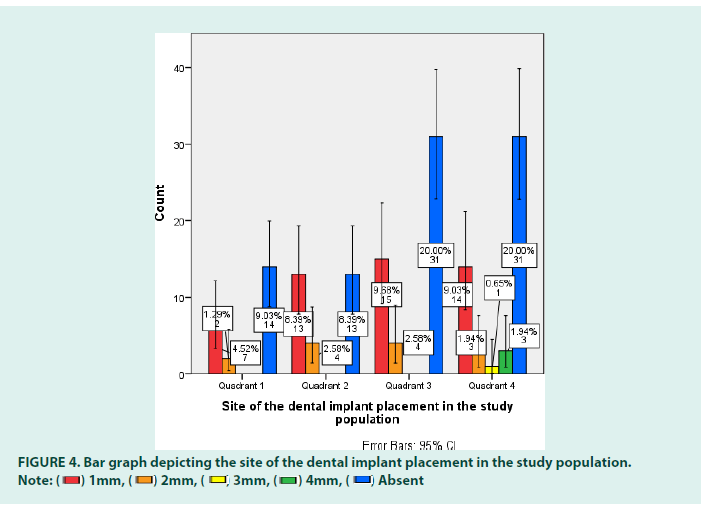
An association was done between the site of the implant placement and crestal bone loss. 33.56% of the patients had an implant placement in quadrant 4, out of which 20% had no crestal bone loss, 9.03% had 1 mm, 1.94% had 2 mm and 4 mm and above each, and 0.65% had crestal bone loss of 3 mm. 20.65% of patients had an implant placement in quadrant 3, out of which 9.68% of them had 1 mm crestal bone loss, 8.39% patients did not have crestal bone loss, and 2.58% had a crestal bone loss of 2 mm. 19.36% of the patients had undergone implant placement in quadrant 2, out of which 8.39% of them do not have crestal bone loss, 8.39% had 1 mm, and 2.58% had 2 mm of crestal bone loss. 14.84% of the patients had the implant placement done in quadrant 1, out of which 9.03% did not have crestal bone loss, 4.52% had 1 mm, and 1.29% had 2 mm crestal bone loss (FIGURE 4). The p-value was found to be 0.000, which is statistically significant.
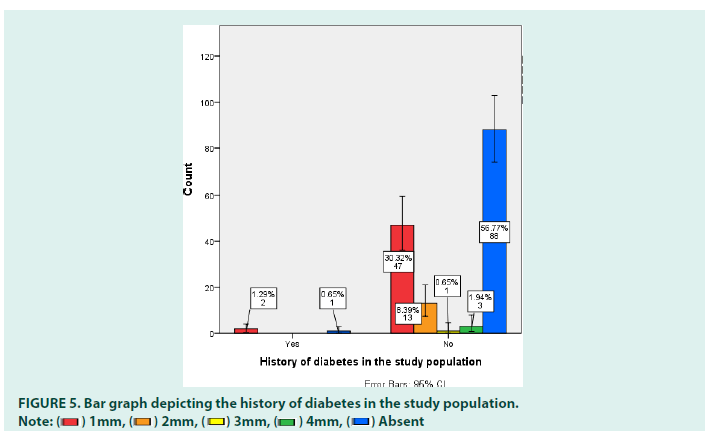
The crosstabs were done between the history of diabetes and crestal bone loss. 1.94% of the patients had a history of diabetes, out of which 1.29% of the patients had 1 mm of crestal bone loss, and 0.65% had no crestal bone loss. 98.07% of the patients did not have a history of diabetes, out of which 56.77% of the patients had no crestal bone loss, 30.32% had 1 mm, 8.39% had 2 mm, and 1.94% had 4 mm and above, and 0.65% had 3 mm of crestal bone loss (FIGURE 5). The p-value was found to be 0.00, which is statistically significant. A study given by Zahrani states those patients with poorly controlled type 2 diabetes present the worse peri-implant bone outcome than patients with well-controlled diabetes. In the present study, the patients with a history of diabetes were very few but had a minimal amount of crestal bone loss. This study is consensus with the present study. For this reason, control and maintenance of glycemic levels should be a key element in the overall care of patients with T2DM. They could play an essential role in ensuring the success of implant therapy.
A study by Nurul Husniyah states that diabetic patients recorded the highest prevalence of bone loss compared to other medically compromised patients. A significant association was found between crestal bone loss and diabetic patients (p<0.05). Patients whose diseases were under control with medication were also observed to have bone loss. Overall, the prevalence of crestal bone loss seems to be higher in diabetic patients compared to other medically compromised patients. There appears to be a definite correlation between diabetes and crestal bone loss.
Dental implant placement in the jaws is impacted by several local factors, including periodontal diseases, the quantity and distribution of dental implants in the arch, occlusion, and bite forces, in addition to systemic considerations. Several studies have shown the importance of local and systemic factors in the long-term success of dental implants; little is known about the factors that influence implant stability following abutment connection and occlusal loading. Thus, the claim that dental implant placement in people with osteoporosis may be contraindicated is based on the assumption that these illnesses may influence the human jaws in the same way that they affect other skeleton elements. Furthermore, there may be changes in the healing kinetics and routes of bone healing and remodeling between long and short bones.
However, no conclusive research has shown that osteoporosis enhances the failure rates of dental implants or the prevalence of peri-implantitis. It is a single centered study with a limited sample size.
Conclusion
This research would help as one of the guides for further research on the association between history of diabetes and crestal bone loss with a larger sample size from the above article it can be concluded that diabetes was not associated with significant crestal bone loss and is lesser when compared to non-diabetic patients. And out of the patients who had crestal bone loss, the highest prevalent crestal bone loss was 1 mm. Out of the patients who had a history of diabetes, most of the patients had a crestal bone loss of only 1 mm.
Acknowledgements
The authors sincerely acknowledge the Medical record department faculties in helping and sorting out datas pertinent to this study.
Conflict of Interest
None to declare
Source of Funding
The present project is funded by Saveetha Institute of Medical and Technical Sciences, Saveetha Dental College and Hospitals, Saveetha University and Rakshith private limited.
References
- Association AD. American Diabetes Association. Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 34(1): S62-S69 (2011).
- Turkyilmaz I. One-Year Clinical Outcome of Dental Implants Placed in Patients With Type 2 Diabetes Mellitus: A Case Series. Implant Dent. 19(2): 323–329 (2010).
- Lee JS, Tolomeo PG, Miller EJ. Effects of Glycemic Control in Patients with Type II Diabetes Mellitus on Dental Implant Survival. J Oral Maxillofac Surg. 74(9): e56 (2016).
- Oates TW Jr, Galloway P, Alexander P, et al. The Effects Of Elevated Hemoglobin A(1c) In Patients With Type 2 Diabetes Mellitus On Dental Implants: Survival and stability at one year. J Am Dent Assoc. 145(12):1218–26 (2014).
- Lee jy, choi yy, choi y, et al. Efficacy Of Non-Surgical Treatment Accompanied by Professional Toothbrushing in the Treatment of Chronic Periodontitis in Patients with Type 2 Diabetes Mellitus: A Randomized Controlled Clinical Trial. J Periodontal Implant Sci. 50(2): 83 (2020).
- Anner R, Grossmann Y, Anner Y, et al. Smoking, Diabetes Mellitus, Periodontitis, and Supportive Periodontal Treatment as Factors Associated with Dental Implant Survival: A long-term retrospective evaluation of patients followed for up to 10 years. Implant Dent. 19(1):57–64 (2010).
- Erbasar GNH, Hocaoğlu TP, Erbasar RC. Risk Factors Associated with Short Dental Implant Success: A Long-Term Retrospective Evaluation of Patients Followed up for up to 9 years. Braz Oral Res. 33(2):77-79 (2019).
- Lee J-B, Shin H-J, Kim D-Y, et al. Evaluation of prognosis related to compliance with supportive periodontal treatment in patients with chronic periodontitis: A clinical retrospective study. J Periodontal Implant Sci. 49(2):76-89 (2019).
- Becker ST, Beck-Broichsitter BE, Rossmann CM, et al. Long-term Survival of Straumann Dental Implants with TPS Surfaces: A Retrospective Study with a Follow-up of 12 to 23 Years. Clin Implant Dent Relat Res. 18(3):480-488 (2016).
- Kazuhiro K. Potentially Risk Factors of Remaining Tooth Extraction in Long Term Cases of Implant Therapy- Retrospective study in 10 Years Follow up Patients. Int J Implant Dent. 9(2):70-76 (2017).
- Adler L. Success, Survival and Complications: A 9-15 Years retrospective longitudinal follow up of dental implant therapy. J Oral Rehabil. 47(1):67-77 (2020).