Research Article - Clinical Practice (2022) Volume 19, Issue 2
Assessing the prevalence and risk factors of anemia in women of reproductive age attending primary health care in Afghanistan’s Provinces of Kabul, Nangarhar, and Herat
- Corresponding Author:
- Mamosai Zewar
Ph.D. Scholar, Jodhpur School of Public Health
Maulana Azad University, India
E-mail: mamosai18@hotmail.com
Received: 28 February, 2022, Manuscript No. M-56150 Editor assigned: 05 March, 2022, PreQC No. P-56150 Reviewed: 20 March, 2022, QC No. Q-56150 Revised: 23 March, 2022, Manuscript No. R-56150 Published: 27 March, 2022, DOI. 10.37532/fmcp.2022.19(2).1907-1919
Abstract
Background: Anemia is one of the most significant consequences of dietary deficiencies in the world. Over 25% of the global population is afflicted. In the world, anemia affects 41.84% of pregnant women and nearly 30.2% of non-pregnant women. Anemia causes can be broadly classified into three major groups: nutritional deficiencies, infectious diseases, and genetic hemoglobin disorders. The most common cause of anemia in developing countries is nutritional anemia. The paper describes factors associated with anemia in reproductive-age women at Kabul, Herat, and Ningrahar primary health care centers, where many patients come from Paghman, Zendajan, and Sangar Sary districts. A low-income slum in Afghanistan. Objective: The objective was to identify how prevalent anemia is and what risk factors contribute to it. Method: a cross-sectional quantitative study among 385 Women of Reproductive Age (WRA) based face to face interviews. Result: The mean Hb level was 52.1% (95% CI:50.7-53.4). In multivariate analysis, anemia was significantly associated with age group, family income, nutritional habits, drinking tea with food, use of iron tablets, irregular menstruation, birth spacing, and history of anemia. Conclusion: Policymakers must develop appropriate practical and context-based policies and initiatives to better address anemia in women during their reproductive years.
Keywords
Anemia, nutrition, WRA, iron supplementation, hemoglobin, epidemiology, risk factors, Afghanistan regions, PHC
Introduction
Anemia is defined as a condition in which the blood has low quantities of hemoglobin and has a low number of functioning red blood cells [1]. It is the world’s 2nd leading factor of disability [2] and one of the most consequential global public health concerns; about 1.62 billion people in the world have anemia [3]. 30.2% of women of reproductive age (15-49) are anaemic in nature, which means around 496 million [4], 38% of pregnant women, 32 million pregnant women, and 43% of children, accounting for 273 million, are anaemic in nature. 68 million people all over the world live with a disability due to anemia [1,5]. Anemia has unfavorable health implications for human capital economics, resulting in a loss of billions of dollars per year [3]. Women are facing more serious consequences and implications than men. It has been shown to be more concerning among women of reproductive age. Women of Reproductive Age (WRA) experience significant effects, including reduced work capacity, lost productivity, poor intellectual performance [2,6], cognitive impairment, and poor health outcomes as a result of poor immunity, which increases infection susceptibility and maternal mortality [7,8]. Anemia is more prevalent, especially in low-income countries, due to nutritional deficiency during pregnancy and infancy, and it has long-term consequences for brain health [9-12] Indeed, among nutritional anemia, the most prevalent cause of anemia is iron-deficiency anemia. About half of the anemia caused in the world is because of iron deficiency. That means 50% of anemia cases are because of iron deficiency all over the world [13,14]. Africa and Asia are the two continents that are most severely affected by anemia and have the highest prevalence of anemia [11]. Based on an estimate, the prevalence of anemia among reproductiveage women in eastern Africa was 34.85%. While a lower range of anemia in women was reported at 19.23% in Rwanda, a higher range was explored at 53.98% in Mozambique [15]. Similarly, among reproductive-age women in 7 South and Southeast Asian countries, the prevalence of anemia was 52.5%, while the lowest range was 22.7% in Timor-Leste and the highest was 63% in the Maldives [16]. Age, education, marital status, parity, current pregnancy status, lactation, interpregnancy interval, place of residence, wealth, use of modern contraceptives, occupation, socioeconomic, literacy level, status, family size, and BMI were frequently recommended as epidemiological factors for developing anemia in females aged 15-49 years [4,17-27].
Anemia’s public health significance in a population is determined by population prevalence. For the afflicted population, 4.9 percent of anemia cases are not a public health problem; 5.0%-19.9% are mild public health concerns; 20.0%-39.9% are moderate public health concerns, and 40% or more of anemia cases are severe public health concerns and emergencies.
Although anemia has been admitted as a public health issue for many years, a slight progress has been made and the prevalence of anemia globally remains insufferably high (WHO, 2004). The World Health Organization, in its draft on “Anaemia Policy Brief ” in its WHA Global Nutrition Targets 2025, has specified the target to bring down the prevalence of anemia to 50% by 2025, but the current efforts and more than that, the COVID-19 pandemic and the increasing trend of the poverty line, especially in conflict and developing countries, have shown it to be a mammoth task.
Anemia prevalence estimates in twenty-three low-income countries range from 41.9% to 61.8%, indicating a critical condition. A more than 40% prevalence of anemia has been declared as a health emergency by the WHO. In addition, anemia affects more than 40% of people in six middle-income countries, ranging from 40.6% to 51.1%. While highincome countries are not in the midst of a health emergency, interestingly, several HIC nations still seem to have anemia prevalence rates ranging from 20% to 35%. Additionally, if observed, WHO estimates that the lowest prevalence of anemia in LIC is 23.5%-39% (just one Rawanda recorded 16.6%), in MIC nations it varies from 10.6% to 37.7% (in Guatemala it was reported at 7.4%), and in HIC regions it is 8.5%-19%. Afghanistan is one of the nations on the list of countries with health emergencies and a serious public health burden among women of reproductive age in Afghanistan. Steve AG, et al. provides information on the prevalence of anemia in Afghanistan. Approximately, 60.5% of children under the age of 5 are anaemic, more than 40% of women who are of reproductive age are anaemic, and 44% of pregnant women are anaemic in this country. Also, 24% of women of reproductive age suffer from iron deficiency in Afghanistan. As mentioned above, anemia is a major public health problem among women of reproductive age (15-49) in the country. Still, the risk factors are unknown, and no comprehensive study has been conducted to determine the prevalence of anemia among women attending primary health care centers in Afghanistan, where there is insufficient data on anemia risk factors. This study aims to determine the prevalence and risk factors of anemia among women of reproductive age (15- 49 years) attending primary health care in three major provinces of Afghanistan. According to the Basic Packages of Health Service (BPHS, 2005), the Primary Health Care (PHC) facilities in the Afghan health system are health posts, basic health centers, comprehensive health centers, and district hospitals. There are seven components in the BPHS package: control of communicable diseases, mental health, child health and immunization, maternal and newborn health, nutrition, disability, and the provision of essential drugs. In the component of mother and newborn, ANC, delivery care, PNC, family planning, and care of the newborn are included. In addition to components of public nutrition, micronutrient supplementation and clinical malnutrition are included. Detection and treatment of anemia are included in primary health care’s basic health services. However, there has not been any research conducted to know the existing gaps in the health system or the prevalence of anemia among women attending primary health care centers, so the risk factor remains unknown. We hypothesized that the prevalence of anemia in women of reproductive age in three provinces of Afghanistan is high and that different factors are associated with the development of anemia. Besides that, those are the largest provinces with large rural settings, where internally displaced families were shifted from neighboring provinces because of climate change and insecurity, as well as immigrants who came back to the country, mostly living in those cities. The study’s findings will help policymakers and program planners make better judgments on effective intervention strategies to address this serious public health concern and actually achieve the plan.
Methodology
â Study sitting
Afghanistan is a land-locked country with a high incidence of natural hazards such as earthquakes, floods, landslides, and droughts. Such shocks potentially force people to leave their usual places of residence and lead to their displacement, either temporarily or permanently, depending on their impact. Subsequently, a high proportion of the Afghan population suffers from extreme poverty. Most of the returnees have shifted from Iran and Pakistan and were internally displaced due to conflict in unsecured areas; they are accommodated in the nearest provinces to the border (Herat, Nangarhar) and center (Kabul) of Afghanistan. Kabul, Herat, and Nangarhar provinces have been faced with the burden of migratory populations from outside the country as well as IDPs.
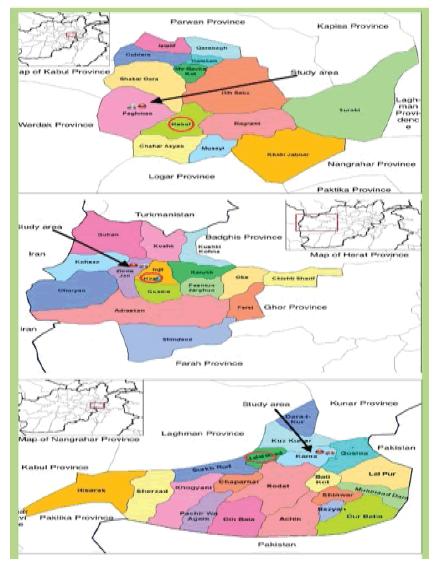
The study was conducted in the center, east and west provinces of Afghanistan; Paghman CHC is in Kabul province, Sangar Sray Kamala CHC is in Nangarhar Province, and Zenda Jan CHC is located in Herat Province. These three are the largest of the provinces in Afghanistan (FIGURE 1).
â Sample size and Design
A quantity analysis using a cross-sectional study of 385 women aged 15 to 49 years was conducted for primary research, and anemia was diagnosed by measuring hemoglobin below 12 g/dL.
The objective: is to study the prevalence and socio-demographic and other factors of anemia among women attending primary health care in three provinces of Afghanistan, which reflected the problem of the country
â Sampling and Data collection method
The questionnaire was designed by validating and appropriating questions from a descriptiveanalytic prospective cross-sectional study. The questionnaire enumerates the socio-demographic and reproductive history (age, family size, marital status, menstrual cycle, education level, livelihood, dietary habits, socioeconomic status, etc.) of the study contestant; the questionnaire was pretested in the region that has comparable characteristics.
In two stages, a probability-based simple random sampling technique was used for sample selection. At the first stage, a random sample was randomly selected from the health facilities, and at the second stage, a random sample was randomly selected from the study subjects. Data were analyzed using the SPSS version V.20.
The independent variables were demographic and socioeconomic conditions (age, education, literacy, family size, number of children in the household, occupation, and family income), food and nutrition conditions, and women’s health conditions (menstruation, number of pregnancies, history of miscarriages, etc.). The variables were obtained by descriptive statistics such as frequency, percentage, mean, and standard deviation analysis using SPSS version 20. The Chi-square test and Odds Ratio (OR) with corresponding 95% Confidence Intervals (CI) were computed to determine the association between independent and dependent variables. A logistic regression analysis was used to examine the factors associated with anemia and to identify characteristics that predict anemia in women of reproductive age in a significant and independent way.
â Ethical consideration
The study protocol for the research to be carried out was approved by the board of studies and passed by the ethical committee of the institution, Public Health Afghanistan as well as the authorities of Maulana Azad University in Jodhpur, India. Privacy and confidentiality were upheld. Formal permission was obtained from the participants before starting the interview.
We followed all the rules and regulations of the Afghan government as well as the Maulana Azad University in Jodhpur, India.
â The description of characteristics
The descriptive of sociodemographic characteristics, dietary habits, and reproductive of WRA were shown in the study in December 2018 (TABLE 1).
| 1. Descriptive of socio-demographic characteristics of WRA in the study | 2. Descriptive of women’s reproductive history and history of anemia | ||||
|---|---|---|---|---|---|
| Marital status (N=386) | N | % | Pregnancy (N=386) | N | % |
| Single | 8 | 2.1 | Yes | 286 | 74.1 |
| Married | 378 | 97.9 | No | 100 | 25.9 |
| Distribution of age group by year (N=386) | Menstruation (N=386) | n | % | ||
| 15-19 | 52 | 13.5 | Regular | 233 | 60.4 |
| 20-29 | 205 | 53.1 | Irregular | 153 | 39.6 |
| 30-39 | 120 | 31.1 | The interval between two menstruation (N=386) | n | % |
| 40-49 | 9 | 2.3 | Less than 28 day | 201 | 52.1 |
| Average Age (Mean+SD) | 26.25+6.14 | More than 28 day | 185 | 47.9 | |
| Level of education (N=386) | Duration of menstruation (N=386) | n | % | ||
| Illiterate | 184 | 47.7 | 1-5 day | 181 | 46.9 |
| Can read and Write | 92 | 23.8 | 6-10 day | 205 | 53.1 |
| Primary school | 52 | 13.5 | History of abortion (N=357) | n | % |
| Intermediate school | 32 | 8.3 | Yes | 50 | 14 |
| High school | 21 | 5.4 | No | 307 | 86 |
| Higher education | 5 | 1.3 | Birth spacing (N=317) | n | % |
| Occupation (N=386) | <2 years | 92 | 29 | ||
| Housewife | 339 | 87.8 | ≥ 2 years | 225 | 71 |
| Employed | 47 | 12.2 | Use of contraceptive method (N=334) | n | % |
| Family income (n=386) | Yes | 184 | 55.1 | ||
| Less than 5000 | 198 | 51.3 | No | 150 | 44.9 |
| 5000-10000 | 139 | 36 | Which kind of contraceptive (N=182) | n | % |
| 11000-20000 | 42 | 10.9 | Oral tablet | 94 | 51.65 |
| 21000-30000 | 7 | 1.8 | Injection | 74 | 40.66 |
| Husband/Father Occupation (N=382) | IUD | 14 | 7.7 | ||
| Govt. employee | 66 | 17.3 | How long have you used this method of contraceptive (N=184) | n | % |
| Private employee | 74 | 19.4 | Less than 2 years | 39 | 21.2 |
| Former | 76 | 19.9 | Equal and more than 2 years | 145 | 78.8 |
| Daily wage | 145 | 38 | History of anemia (N=246 ) | n | % |
| Jobless | 21 | 5.5 | Yes | 91 | 37 |
| Location by province (N=386) | No | 155 | 63 | ||
| Kabul (Paghman CHC) | 129 | 33.4 | Family history of anemia (N=246) | n | % |
| Nangrahar (Sangarsaray CHC) | 128 | 33.2 | Yes | 85 | 34.6 |
| Herat (Zenda Jan CHC) | 129 | 33.4 | No | 161 | 65.4 |
| Family members (N=386) | 3. Description of dietary habits among WRA in the study | ||||
| 1-4 members | 70 | 18.1 | Use of meat per month (N=386) | N | % |
| 5 7 members | 125 | 32.4 | I or two times per month | 263 | 68.1 |
| 8+ members | 191 | 49.5 | 1-2 times per week | 102 | 26.4 |
| Average Family members (Mean+SD) | 8.2+2.6 | 3/more than three times in a week | 21 | 5.4 | |
| Number of children (N=367) | Use of beans per week (N=386) | ||||
| 1-3 Child | 265 | 72.2 | I or two times per month | 173 | 44.8 |
| 4/more than four | 102 | 27.8 | Two times a week | 186 | 48.2 |
| Average Amount of children <Mean+ SD) | 2.6+2. l | Three or four times a week | 27 | 7 | |
| Use of fruits per week (N=386) | |||||
| Two times a week | 206 | 53.4 | |||
| I or four times in a week | 148 | 38.3 | |||
| one rime in a day | 32 | 8.2 | |||
| Use of dairy (milk, yogurt) (N=386) | |||||
| Daily | 93 | 24.1 | |||
| Weekly | 259 | 67.1 | |||
| Don't use | 34 | 8.8 | |||
| Use of tea alon2 with foods (N=386) | |||||
| Yes | 153 | 39.6 | |||
| No | 233 | 60.4 | |||
| Current use of iron tablet (N=386) | |||||
| Yes | 128 | 33.2 | |||
| No | 258 | 66.8 | |||
TABLE 1. Show descriptive of socio-demographic characteristics of WRA in the study, descriptive of women the reproductive history and history of anemia, and descriptive of dietary habits among WRA in the study.
â Prevalence of anemia and associations
Level of Hemoglobin: The mean hemoglobin (Hb) level across the sample, adjusted for altitude and capillary blood sample [28] was 11.36 g/dl (SD:1.39), and the overall prevalence of anemia was 52.1% (95% CI:50.7-53.4). Most cases were mild anemia, with a prevalence of 20.7% (95% CI:19-18.8); 29% (95% CI:28-30%) was moderate anemia, and 6.6% (95% CI:5-7) was severe anemia. While the level of hemoglobin of more than 12 gm/dl was 47.9%.
â Age
The majority of women were anemic at the age of 20-29 years old (53.7%); women at the age of 30-39 (33.3%); at the age of 15-19 (10%) and at the age of 40-49 (3%) had a prevalence of anemia age had an association with anemia (p=0.02).
â Marital status
Anemia among married WRA was 98.5% and among the unmarried was 1.5%.
â Pregnant and non-pregnant
75.6% of pregnant women and 24.4% of nonpregnant women were anemic
â Level of education
The majority of anemic women were illiterate; 43.8% of illiterate women had anemia compared to 1.5% of higher-educated women
â Women occupation
Anemia among women of reproductive age with no occupation was 87.6%, while it was 12.4% with occupation.
â Husband or Father occupation
Most women whose husbands had an income from their daily wages (self-employed) were anemic (44.7%), and among farmer husbands’ wives’ anemia was 21%, among private employee husbands it was 15.6%, among government employees it was 14.1% and among jobless housewives’ anemia was 4.5%. It has strong associations with anemia (p=0.01).
â Household income
A majority (57.7%) of women had anemia with a household income of under 5000 Afghani and 31.1% of women had a household income of under 10000-50000 Afghani, 11000-20000 Afghani 8% and 21000-30000 3% of WRA had anemia with strong association(p=0.03).
*1$=100 Afs
â Family size and number of children
Anemia was more than half (50.2%) among women in the study who had 8 or more than 8 family members: 29% among women with 5-7 family members and 20.4% among women with 1-4 family members.
Women with 1-4 children had anemia at a rate of 70.3%, while women with 4 or more children had anemia at a rate of 29.7%.
â Location
A high prevalence of anemia was found (40.8%) in Nangarhar province, 32% in Herat province, and 26.9% in Kabul province.
â Dietary habits
74.6% of anemic women used meat less than twice per month, and 20.4% of them used it less than twice per week (p=0.01). 50.2% of anemic women consume beans twice a week, while 43.8% consume beans twice a month. Fruit is consumed by 57.2% of anemic women twice a week, 37.8% one to four times a week, and 5% once a day (p=0.01). 73.1% of anemic women use dairy per week and 21.9% of anemic women use dairy per day. 54.7% of anemic women use tea along with food, and 45.3% of anemic women don’t drink tea (p=0.001).
â Iron supplementation
Anemia among women was (71.6%) who did not use iron tablets, and 28.4% of anemic women used iron tablets (p=0.04).
â Menstruation
While 67.7% of anemic women had irregular menstruation (p=0.001). Mensuration intervals of less than 28 days had 54.2% prevalence, although more than 28 days had 45.8% anemia (p=0.01). 76.1% of the menstruating women were anemic if they had had 6-10 days of mensuration bleeding. while the women’s 1-5- day menstruation duration was 23.9% anemic (p=0.001).
â Birth spacing and history of abortion
Women with 2 or less than 2 years of birth spacing had a higher prevalence of anemia than those women who had less than 2 years of birth spacing (p=0.02). Women with a history of abortion had 12.1% anemia.
â Contraceptive methods
Anemia was observed in a relatively higher 52.5% among participants who were using any contraceptive methods, while 47.5% was observed among non-users. Similarly, women using oral pales were more anemic, with 47.3 and 45.2% anemia found among injectable contraceptive methods, while among IUD users it was only 7.6%. Participants with 2 years or more than 2 years of use of any contraceptive method had 81.7% anemia, and 18.3% of those who had used it for less than two years had anemia.
â Women and her family history of anemia
62.8% of women had anemia with a history of anemia and 48% of women were anemic without a history of anemia (p=0.02). Comparing, women with a family history of anemia were less anemic at 32.5% as compared to those who had no family history of anemia (67.4%).
Risk factor of anemia (Multi-Variate logistic regression): Compared to women in the poor category (5000-10,000 family income and 11000-20,000 family income), they were 1.71 and 2.30 times more likely to have anemia (OR: 1.71, 95% CI:1.10-26.64, p=0.01 and OR:2.30, 95% CI:1.16-4.55, p=0.01) than women in the rich category (21000=30,000 family income). Women’s husbands or fathers with daily wages were 0.46 times as likely to have anemia (OR:0.46, 95% CI:0.25-083, p=0.0.01) than women in the other categories of husband or father occupations. Women who reported using meat 1-2 times per week were 1.97 times more likely to have anemia (OR:1.97, 95% CI:1.24-3.14, p=0.004) than those who ate 3 or more times per week. In addition, women who consumed fruits once a day, twice in a week were 2.78 times more likely to have anemia (OR: 2.78, 95% CI:1.25-6.16, p=0.012) than those who consumed fruits four times a week. Women who were drinking tea along with food were 0.25 times as likely to have anemia (OR:0.25, 95% CI:0.16-0.38, p-value<0.001) as compared to women who were not drinking tea while eating food. Compared to women who were not using iron tablets, those who were using iron tablets were 1.57 times more likely to have anemia (OR:1.57, 95% CI:1.02- 2.41, p=0.03). As compared with women with irregular menstruation, women with regular menstruation were 0.48 times as likely to have anemia (OR:0.48, 95% CI:0.02-0.08, p-value<0.001). Women with less than a 28-day interval between menstruation were 1.69 more likely to have anemia (OR:1.69, 95% CI:1.13- 2.54, p=0.01) than women with more than a 28- day interval between menstruation, 0.69 times as likely to have anemia. Those who had a 6-10- day duration of menstruation were 0.38 times more likely to have anemia (OR:0.38, 95% CI:0.26-0.71, p=0.001) than those who had a 1-5-day duration of menstruation. Compared to women who had more than 2 years of birth spacing, women who had less than 2 years of birth spacing were 1.79 times as likely to have anemia (OR:1.79, 95% CI:1.09-2.92, p=0.02). Additionally, compared to women who had no history of anemia, women with a history of anemia were 0.55 times as likely to have anemia (OR:0.55, 95% CI:1.26-0.11, p<0.001).
Discussion
The objectives of this study are to identify the prevalence and background characteristics of WRA in Afghanistan with anemia and to therefore identify associated risk factors. According to the study analysis, a significant proportion of WRA had anemia in both pregnant and non-pregnant women. The prevalence of anemia among WRA in Afghanistan was 52.1%. Afghanistan’s anemia prevalence was nearly equal to that of many other Sub-Saharan African countries [29] and South and Southeast Asia [16]. It is considered a severe public health problem according to WHO criteria. The prevalence of anemia was similar to other relevant studies conducted by WRA in Afghanistan. In addition, according to WHO estimates, the prevalence of anemia in WRA in Afghanistan increased between the years 2000 and 2019 and varied across population subgroups. In this study, it was found to vary with age, marital status, pregnancy, level of education, women’s occupation, husband or father’s occupation, economic status (family income), province of residence, family size, number of children, and the type of contraceptive method used, as well as nutrition status (using meat, fruits, beans, and dairy products), using tea with the meal, usage of iron tablets, history of anemia, family history of anemia, mensural problems, abortions, use and types of contraceptive methods. The etiology of anemia is complex, and successful anemia reduction efforts must identify the major contributing factors, then develop and implement an evidence-based package of interventions in order to achieve effective results. Evidence suggests that iron deficiency anemia is one of the most prevalent causes of anemia. Chronic low iron intakes, poor bioavailability of iron sources, or high requirements such as during periods of increased iron need due to rapid body growth during early childhood, adolescence, and pregnancy, or excess iron loss due to hookworm infection, bleeding disorders, or heavy menstrual blood loss, all contribute to iron deficiency. The most prevalent causes of iron deficiency are nutritional, which are the outcome of inadequate micronutrient intake in the regular diet; poor absorption due to low bioavailability or excessive absorption inhibitors in the diet; increased robust requirements (for example, during periods of rapid growth such as infancy and adolescence, or during pregnancy) and increased losses. In addition, causes and contributors to iron deficiency include high iron demands owing to rapid growth in blood, muscle, and other tissues (early childhood, adolescence, pregnancy, lactation). Even in places with increased nutritional diversity, food and nutrition security, and usage of animalsource foods, it is difficult to meet high iron needs. Similarly, non-nutritional causes of or contributors to anemia include factors associated with anemia, particularly in women, including poverty, obesity, low education level, household wealth, cultural norms, lack of empowerment, rural living, inadequate health care, nutrition knowledge, health policies, limited access to health care, inadequate maternal and childcare, and vulnerability of women and children (early onset of childbearing, high parity, and short birth spacing) [1]. According to the study, the prevalence of anemia among pregnant women (75.6%) is comparable to that of non-pregnant women of reproductive age (24.4%). The prevalence is also higher than in several other studies inside the country [5]. Furthermore, 30.4% of Ethiopian women had anemia [30], 44.8% of Sierra Leone women had anemia [31], and 39.5% of Tanzanian women had anemia [32]. In this study, 20-29-year-old women were at a higher risk of anemia than the prevalence of women aged 30-39, and among those, 15-19 was in the third category. This is also coherent with previous reports on Afghanistan. Obstetric and maternal characteristics are known to be important determinants of anemia. Pregnant mothers from the primary study regions of the country had a higher prevalence of anemia during pregnancy than non-pregnant women. A study in Bangladesh [33] among women attending ANC in a government hospital reported the high prevalence of anemia in pregnant women. India also reported that pregnant women develop a high prevalence of anemia. A community-based study in Ethiopia shows the high prevalence of anemia in pregnant women. In our study, women from the Nangarhar region had a high level of prevalence, while those from the Kabul and Herat regions had a lower level of prevalence. Those regions with a high prevalence of anemia have something in common; they are located in the eastern part of the country and are endemic to malaria. Individuals who drank tea with their meals had a high prevalence of anemia. Another study found that drinking tea with meals is the main factor associated with unacceptably high levels of anemia in women of reproductive age. Anemia occurred more among illiterate women and those with no occupation and lower household income. In Bangladesh, illiterate women were more anemic than literate women [34]. Poor category women were more likely to have anemia and it was higher among women whose husbands had an income from their daily wages (self-employed). Similar findings were observed in Rwanda, Ethiopia, and Pakistan, where poor and undernourished women were more likely to have anemia [24,35,36].
Anemia is a complex problem in which nutrition and socioeconomic status interact. Improved economic status has been associated with better nutrition [37], decreased infection morbidity [36], higher access to health care, and other favorable living conditions [37,38] all of which influence anemia. Undernourished women are more likely to suffer from iron deficiency. The most common underlying causes of anemia and malnutrition are usually linked to low socioeconomic status [39,40]. In order to minimize the prevalence of anemia, interventions that seek to economically empower women should be addressed. Furthermore, malnutrition treatment programs must include iron supplements as a component of their intervention packages. High-level anemia occurs in married women. As a result, slaw has emerged among Jordanian women [25]. Higher morbidity due to anemia in this population subgroup occurred because of poor socioeconomic status and overcrowding [41]. In Eastern Africa, high parity and large household size were associated with a higher prevalence of anemia [15]. Similarly, anemia was more than half (50.2%) prevalent among women who had 8 or more than 8 family members and more than 4 children. In Bangladesh, women with more than seven children were anemic [34]. Most of the women (71.6%) who did not use iron tablets were anemic. Iron supplementation and food fortification are considered the best strategies to reduce women’s anemia. Addressing iron deficiency would require both iron supplementation programs targeted at women and adolescent girls, as well as populationbased solutions such as flour fortification. Other initiatives, such as dietary supplements and agrocultural support, that can have a higher impact with fewer adverse effects are also required. Iron supplementation for one to three months resulted in greater increases in hemoglobin and ferritin than either shorter or longer periods. Symptomatic fatigue is eliminated with iron supplementation [42]. Anemia was more prevalent among women who had irregular or more days of menstruation. Women with 2 or less than 2 years of birth spacing had a higher prevalence of anemia. Kammaruzaman M. et al. reported the high percentages of anemia among those who had current amenorrhea and those who were not using contraception. It was prevalent among those with a history of abortion, using any contraceptive method, using oral pales and injectable contraceptive methods, among participants with 2 years or more than 2 years of use of any contraceptive method, and among women with a history of anemia [15]. They also suggest that there is a prevalence of anemia among women who are living in households with a size of 6 or more than 6, with no use of contraceptives, and residing in rural areas. Various types of anemia are related to glitches in the genes of the family. So, it is proven that there is an association between women and a family history of anemia and anemia.
â Associations of anemia with variables
In our study, twelve factors were found to be significantly associated with anemia in our sample: 1) age group, 2) husband and father’s occupation, 3) family incomes, 4) meat consumption, 5) fruit consumption, 6) drinking tea with food, 7) use of iron tablets, 8) irregular menstruation, 9) intervals between menstruation (p=0.01), 10) duration of menstruation, 11) birth spacing and 12) history of anemia. The findings are supported by a study in Kyrgyzstan [43]. Anemic women for following improper dietary habits such as avoiding food during pregnancy, craving for non-food substances, and inadequate women’s dietary diversity. The nutritional status of iron is determined by consuming sufficient amounts of iron in the diet or taking iron supplements [44] Several studies have shown that iron supplementation has a positive impact on improving hemoglobin levels in women of reproductive age [45-47] which is similar to our study. Addis Alene et al. reported that iron supplementation during pregnancy, the trimester of current pregnancy, of pregnancies, wealth quintile, and MUAC are significantly associated with anemia. It is recommended to improve the ANCs that have been taken in government hospitals. As pregnancy is a critical stage for a woman, we highly recommend that people take extra care apart from the treatment they receive from the hospital so that they can prevent the life-threatening risk of anemia. Anemia associated with married women between the ages of 20 and 29 needs further research, to better understand the possible links between marital status, age, and anemia status. Zegeye B et al. found the prevalence of anemia and its associated factors among married women in 19 sub-Saharan African nations. This report supported our study findings on marital status and age [34,48]. 20-29-year-old women, particularly married women, may suffer from one of several un-researched health issues. Younger maternal age has been implicated in the development of postpartum anemia because this age group tends to have incomplete growth, less utilization of prenatal and postnatal services, and psychological factors [49]. Understanding the health requirements of this vulnerable group should be given special attention and consideration. National governments and other stakeholders working on women’s health must work together to improve married women’s economic empowerment, promote family planning services, and collaborate with religious leaders to reduce the burden of anemia among women. Toheed R et al., which is correlated with our findings, describe a highly significant association with abnormally heavy menstrual bleeding, irregular menstruation, and dysmenorrhea [50]. Having frequent births with less than 2 years of spacing is among the key predictors of anemia in Afghanistan. This is also consistent with other studies [27] that showed limiting births or using family planning to control frequent birth rates and birth spacing is a key contributing factor to the prevention of anemia during pregnancy. Sharma JB and Shankar M revealed that anemic women should adopt an effective contraceptive method and not conceive for at least two years to allow their iron stores to recover. Interestingly, in our primary study, individuals who had used any contraceptive method for two years or more had a greater incidence of anemia than those who had used it for less than two years. In this study association between contraceptive users and anemia was found. There is a need for further study to find an association between anemia and contraceptive use.
â Risk factors of anemia in women reproductive age
In total, eleven risk factors for anemia among women of reproductive age were found in the multivariate logistic regression analysis: 1) nutritional status; meat consumption; 2) consumption of fruits and vegetables 3) Consuming tea with foods 4) gross family income, 5) the occupations of the husband and father, 6) current use of iron tablets, 7) irregular menstruation, 8) intervals between menstruation, 9) duration of menstruation, 10) birth spacing, and 11) history of anemia.
Women in the poor category of family income were 2.30 times more likely to be at risk of anemia than women in the rich category. In WRA, similar risk factors for anemia occurred in Cambodia (1.38), India (1.15), Maldives (1.61), Myanmar (1.18), and Bangladesh (1.35) times at risk of anemia [16]. Iron deficiency anemia is a risk factor for maternal mortality; about 115, 000 maternal mortalities and 59, 000 perinatal mortalities happen due to iron deficiency worldwide. Those women who had 3-5 pregnancies were 1.95 times more likely to be anemic. Scott Poe and Mary Cogswell also signified the findings that with the increasing severity of anemia, the risk of preterm birth is rising. Similarly, the risk of anemia increases with decreasing Hb levels. At the same time, women who experienced less birth spacing and had the experience of frequent pregnancy were also found to have a 1.79 times higher risk of developing anemia (OR: 1.79, 95% CI: 1.09-2.92, p=0.02). This is most likely because women have not yet restored essential minerals, particularly iron and folic acid, that were decreased during the previous pregnancy. Women who were drinking tea along with food were 0.25 times as likely to have anemia (OR:0.25). In Ethiopia, it was shown that consuming tea or coffee immediately after food (AOR: 3.58) was associated with significant risk. Using meat 1-2 times per week was 1.97 times more likely to have anemia (OR:1.97) and twice a week was 2.78 times more likely to have anemia (OR:2.78). In an Ethiopian study, they showed a higher risk of anemia among fewer meat users. Dietary iron absorption from the body’s gut is dependent on physiological requirements and is likely to be limited by bioavailability or quantity [51]. Whether iron deficiency and anemia among middle and lowincome people are primarily a result of dietary insufficiency remains to be seen. Anemia and low hemoglobin levels are important risk factors for women’s health and nutrition status. Symptoms of anemia with the flow of menses It is clearly revealed that women who have very high menstrual blood flow also have high symptoms of anemia. During menstrual bleeding, about 100 mg-150 mg of iron can be lost [32]. Hormonal contraceptives may have an effect directly or indirectly on iron loss among women. In Tanzania [32] indicated that hormonal contraceptive use was significantly associated with a decreased risk of anemia and iron deficiency among non-pregnant women. The effect is perhaps because of a decrease in the flow of menstrual bleed. Pregnant women who do not take iron supplementation during pregnancy are 1.54 times more likely to develop anemia. Anemia may further deteriorate during pregnancy in response to the increased physiologic demands of gestation, thereby increasing the risk of adverse pregnancy outcomes. Due to the increase of substantially Demond of gestation during pregnancy; thus, anemia perhaps further deteriorates and increased the risk of adverse effects of pregnancy [29]. Beard reported that sufficient iron is essential for immune function. The presence of iron is crucial in body tissues for cellular respiration and other reductionoxidation enzyme systems; it has special critical metabolic functions in the brain, muscle, and red cells. WHO guidelines recommend universal iron and folic acid supplementation for pregnant women where anemia is highly prevalent. Ezzati et al. reported a statement on severe anemia and delivery death: Evidence of circulatory decompensation is visible at 6.0 g/ dl. At rest, women suffer from dyspnea and higher cardiac output. The increased stress of childbirth can cause maternal death at this point. With a hemoglobin content of 4.0 g/dl, maternal mortality from anemic heart failure is likely without appropriate treatment. Even just a 100 mL blood loss can cause vascular shock and death. Population surveys among pregnant and non-pregnant women illustrate a strong linear correlation in the Hb values of these women. The difference between Hb values in non-pregnant and non-pregnant conditions is nearly constant (range: 1.34 gm/dl-1.339 gm/ dl). The Hb cut-off range for anemia is also lower in pregnancy. The WHO cut-off is 1 gm/ dl lower in pregnancy. Although the physiologic hemodilution in mid-pregnancy reduces the Hb concentration by 1.5 gm/dl, obtained in field surveys. Hence, we can expect the prevalence of anemia among pregnant women to be about equal among pregnant and non-pregnant women. For this reason, pregnant women are more iron-deficient than non-pregnant women. A better understanding of anemia based on biological, socio-demographic, nutritional, and reproductive history will help us to design strategies and interventions to better address anemia during the reproductive cycle in Afghanistan’s provinces. As a result, the risk of unfavorable maternal and fetal outcomes related to anemia will be reduced. Moreover, it will also help us identify the prevalence of anemia and predict the causes related to it. Consequently, the findings of this research have the potential to benefit the general population by improving our understanding of what factors contribute to anemia and what can be done to improve the health of Afghan women of reproductive age, particularly in the three provinces that have been understudied [52]. The findings of this study will assist policymakers in developing appropriate policies and initiatives and taking the appropriate action accordingly by designing suitable approaches to better address the specific type of anemia in women in the Provence of Afghanistan. Effective efforts for preventing and controlling anemia should focus on women in urban and rural regions who have little or no education, do not use contraception during pregnancy, and have dietary issues.
Conclusion
Thus, this study concluded that routine iron supplementation in women of reproductive age and early commencement of prenatal clinic attendance could lower the prevalence of anemia in women. As a result, women are advised to consume iron-rich foods on a regular basis in order to prevent the prevalence of iron deficiency (anemia) during their reproductive age, especially during pregnancy. In fact, educating girls can help to reduce anemia in communities. A strategy plans to make it mandatory for flour importer merchants to import all ironfortified flour. Furthermore, strict steps should be implemented to minimize the risk factors for anemia in women by distributing information to the media and public.
Acknowledgment
I would like to thank my supervisor for valuable suggestions that improved the final form of this paper.
Conflict of Interest
There is no conflict of interest in this study.
References
- World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. World Health Organization. (2011).
- Balarajan Y, Ramakrishnan U, Ozaltin E, et al. Anemia in low-income and middle-income countries. Lancet. 378, 2123-2135 (2011).
- World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. World Health Organization. (2016).
- Bezerra AGN, Leal VS, de Lira PIC, et al. Anemia and associated factors in women at reproductive age in a Brazilian Northeastern municipality. Rev Bras Epidemiol. 21: e180001 (2018).
- Flores-Martinez A, Zanello G, Shankar B, et al. Reducing anemia prevalence in Afghanistan: Socioeconomic correlates and the particular role of agricultural assets. PLoS One. 11, e0156878 (2016).
- Jimenez K, Kulnigg-Dabsch S, Gasche C. Management of Iron Deficiency Anemia. Gastroenterol Hepatol (N Y). 11, 241-250 (2015).
- World Health Organization. Global Nutrition Targets 2025: Anemia Policy Brief Geneva. WHO. (2014).
- Haas JD, Brownlie T. Iron deficiency and reduced work capacity, a critical review of the research to determine a causal relationship. J Nutr. 131, 676S-90S (2001).
- Hare D, Ayton S, Bush A, et al. A delicate balance: Iron metabolism and diseases of the brain. Front Aging Neurosci. 5, 34 (2013).
- Burke RM, Leon JS, Suchdev PS, et al. Identification, prevention, and treatment of iron deficiency during the first 1000 days. Nutrients. 6, 4093-4114 (2014)
- Pala K, Dundar N. Prevalence & risk factors of anemia among women of reproductive age in Bursa, Turkey. Indian J Med Res.128, 282-286 (2008).
- Al-Alimi AA, Bashanfer S, Morish MA, et al. Prevalence of iron deficiency anemia among university students in hodeida province, Yemen. Anemia. 2018, 1-7 (2018).
- World Health Organization. Iron deficiency anemia. assessment, prevention, and control. A guide for programme managers. 47-62 (2001).
- McLean E, Cogswell M, Egli I, et al. Worldwide prevalence of anemia, WHO vitamin and mineral nutrition information system, 1993-2005. Public Health Nutr. 12, 444-454 (2009).
- Teshale AB, Tesema GA, Worku MG, et al. Anemia and its associated factors among women of reproductive age in eastern Africa: A multilevel mixed effects generalized linear model. PLoS One. 15, e0238957 (2020).
- Sunuwar DR, Singh DR, Chaudhary NK, et al. Prevalence and factors associated with anemia among women of reproductive age in seven South and Southeast Asian countries. PLoS One. 15, e0236449 (2020).
- World Health Organization. Global nutrition monitoring framework: Operational guidance for tracking progress in meeting targets for 2025. (2017).
- Lover AA, Hartman M, Chia KS, et al. Demographic and spatial predictors of Anemia in women of reproductive age in timor-leste: implications for health program prioritization. PLoS One. 9, e91252 (2014).
- Habyarimana F, Zewotir T, Ramroop S, et al. Prevalence and Risk Factors Associated with Anemia among Women of Childbearing Age in Rwanda. Afr J Reprod Health. 24, 141-151 (2020 ( .
- Lakew Y, Biadgilign S, Haile D, et al. Anaemia prevalence and associated factors among lactating mothers in Ethiopia. BMJ open. 5, e006001 (2015).
- Liyew AM, Kebede SA, Agegnehu CD, et al. Spatiotemporal patterns of anemia among lactating mothers in Ethiopia. PLoS One. 15, e0237147 (2020).
- Win HH, Ko MK. Geographical disparities and determinants of anaemia among women of reproductive age in Myanmar: analysis of the 2015-2016 Myanmar Demographic and Health Survey. WHO South East Asia J Public Health. 7, 107-113(2018).
- Kordas K, Centeno ZYF, Pachon H, et al. Being overweight or obese is associated with lower prevalence of anemia among Colombian women of reproductive age. J Nutr. 143, 175-181 (2013).
- Gebremedhin S, Enquselassie F. Correlates of anemia among women of reproductive age in Ethiopia: evidence from Ethiopian DHS 2005. Ethiop J Heal Dev. 25, 22-30 (2011).
- Arabyat RM, Arabyat G, Al-Taani G, et al. Prevalence and risk factors of anemias among ever-married women in Jordan. East Mediterr Health J. 24, 543-552 (2019).
- Obse N, Mossie A, Gobena T, et al. Magnitude of anemia and associated risk factors among pregnant women attending antenatal care in Shalla Woreda, West Arsi Zone, Oromia Region, Ethiopia. Ethiop J Health Sci. 23, 165-173 (2013).
- Alemu T, Umet M. Raeproductive and obstetric factors are key predictors of maternal anemia during pregnancy in Ethiopia. Anemia. 649815. (2015):
- Kevin M, Mei Z, Grummer-Strawn L, et al. Hemoglobin adjustments to define anemias. Trop Med Int Health. 13, 1267-1271 (2008).
- Stevens GA, Finucane MM, De-Regil LM, et al. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995-2011: a systematic analysis of population-representative data. Lancet Glob Health. 1, e16-25 (2013).
- Haidar J. Prevalence of anaemia, deficiencies of iron and folic acid and their determinants in Ethiopian women. J Health Popul Nutr. 28, 359-368 (2010).
- Wirth JP, Woodruff BA, Engle-Stone R, et al. Predictors of anemia in women of reproductive age: Biomarkers Reflecting Inflammation and Nutritional Determinants of Anemia (BRINDA) project. Am J Clin Nutr. 106, 416S-427S (2017).
- Haile ZT, Kingori C, Teweldeberhan AK, et al. The relationship between history of hormonal contraceptive use and iron status among women in Tanzania: A population-based study. Sex Reprod Healthc. 13, 97-102 (2017).
- Azhar BS, Islam M, Karim M. Prevalence of anemia and associated risk factors among pregnant women attending antenatal care in Bangladesh: A cross-sectional study. Primary Health Care Res Develop. 22, E61 (2021).
- Kamruzzaman, Rabbani MG, Saw A, et al. Differentials in the prevalence of anemia among non-pregnant, ever-married women in Bangladesh: multilevel logistic regression analysis of data from the 2011 Bangladesh Demographic and Health Survey. BMC Women's Health. 15, 54 (2015).
- Hakizimana D, Nisingizwe MP, Logan J, et al. Identifying risk factors of anemia among women of reproductive age in Rwanda-a cross-sectional study using secondary data from the Rwanda demographic and health survey 2014/2015. BMC Public Health. 19, 1662 (2019).
- Soofi S, Khan GN, Sadiq K, et al. Prevalence and possible factors associated with anemias, and vitamin B 12 and folate deficiencies in women of reproductive age in Pakistan: analysis of national-level secondary survey data. BMJ Open. 7, e018007. (2017):
- Apouey BH. Health policies and the relationships between socioeconomic status, access to health care, and health. Isr J Health Policy Res. 2, 1-2 (2013).
- Arpey NC, Gaglioti AH, Rosenbaum ME, et al., How socioeconomic status affects patient perceptions of health care: a qualitative study. J Prim Care Community Health. 8, 169-175 (2017).
- Kassebaum NJ, GBD 2013 Anemia Collaborators. The global burden of Anemia. Hematol Oncol Clin North Am. 30, 247-308 (2016).
- Mawani M, Ali SA, Bano G, et al. Iron deficiency anemia among women of reproductive age, an important public health problem. Repro Sys Sex Dis Current Res. 5(3): 1-6 (2016).
- Bellizzi S, Ali MM. Effect of oral contraception on anemia in 12 low and middle-income countries. Contraception. 97, 236-242 (2018).
- Low MS, Speedy J, Styles CE, et al. Daily iron supplementation for improving anaemia, iron status and health in menstruating women. Cochrane Database Syst Rev. 4, CD009747 (2016).
- Otunchieva A, Smanalieva J, Ploeger A. Dietary quality of women of reproductive age in low-income settings: a cross-sectional study in Kyrgyzstan. Nutrients. 2022, 14(2), 289
- Sharma JB, Shankar M. Anemia in Pregnancy. JIMSA. 23, 253-260 (2010).
- Iqbal S, Ekmekcioglu C. Maternal and neonatal outcomes related to Iron supplementation or iron status; the journal of Maternal-Fetal and Neoborn. related to iron supplementation or iron status: a summary of meta-analyses. J Matern Fetal Neonatal Med. 32, 1528-1540 (2019).
- Wang Z, Sun J, Wang L, et al. Effect of iron supplementation on iron deficiency anemia of childbearing age women in Shanghai. Wei Sheng Yan Jiu. 41, 51-55 (2012).
- Zegeye B, Anyiam FE, Ahinkorah BO, et al. Prevalence of anemia and its associated factors among married women in 19 sub-Saharan African countries. Arch Public Health. (2021) 79:214
- Dey S, Goswami S, Goswami M. Prevalence of anemias in women of reproductive age in Meghalaya: A logistic regression analysis. Turkish J Med Sci. 40, 783-789 (2010).
- Bhagwan D, Kumar A, Rao CR, et al. Prevalence of Anaemia among Postnatal Mothers in Coastal Karnataka. J Clin Diagn Res. 10, LC17-LC20 (2016).
- Toheed R, Ayub TB, Ali HS, et al. Prevalence of menstrual dysfunction and its comparative correlation with anaemia. JRMC. 21, 157-160 (2017).
- Ecker O, Weinberger K, Qaim M, et al. Patterns and determinants of dietary micronutrient deficiencies in rural areas of East Africa. African J Agri Res Eco. 4, 1750194 (2010).
- Ezzati M, Lopez AD, Rodgers A, et al. Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors. World Health Organization, Geneva, Switzerland. 3, 2248 (2004).